Abstract
Background:
Women having their first birth have a higher risk of episiotomies. Therefore, the study of the procedure in this group of at risk women will assist in solving some of its associated controversies.
Aim:
The aim was to determine the prevalence, predictors, and outcomes of episiotomy among primigravid women in Enugu, Nigeria.
Materials and Methods:
The study was a retrospective cross-sectional review of labor ward records of women that had their first delivery at the University of Nigeria Teaching Hospital (UNTH) Enugu, over a 5-year of April 204 to March 2009. Only women that had a vaginal delivery were included in the study. Mann–Whitney U-test (continuous data) and Chi-square test (categorical data) were used for data analysis.
Results:
Prevalence of episiotomy in the study was 62.1% (411/662). The episiotomy rate for booked women (65.6%, 376/573) was significantly higher than that of unbooked women (39.3%, 35/89), (prevalence ratio = 1.67 [95% confidence interval: 1.28, 2.17]). The birth weights of babies delivered in the episiotomy group (median = 3.2 kg [interquartile range (IQR): 2.9-3.5]) was statistically higher than those of women who did not receive episiotomy (median, 3.1 kg [IQR: 2.7-3.4]), (Z = -3.415, P = 0.001). Proportion of newborns with low 1st min Apgar scores in the episiotomy group (21.7%, 89/411) was significantly lower than the no episiotomy group (15.1%, 38/251) (P = 0.04).
Conclusion:
Prevalence of episiotomy among women that had their first births in the UNTH, Enugu was high, and the predictors included booked status of women, higher gestational age at delivery, and larger neonatal birth weight. More efforts should be made to reduce episiotomy rate in the hospital.
Keywords: Episiotomy, Nullipara, Outcomes, Predictors, Primigravidae, University of Nigeria teaching hospital-Enugu
Introduction
Episiotomy is an intentional surgical incision made on the perineum with the aim of enlarging the introitus during childbirth.[1,2] There are essentially two types thus: Midline, and mediolateral episiotomies; and each has its advantages and drawbacks.[3] Furthermore, it is recommended that the choice of episiotomy technique should be the one which the care giver is most familiar with.[2] The procedure is usually administered for several reasons including to prevent severe perineal laceration/tear in the parturient, especially in the primigravidae;[4] and was first reported in the 18th century.[5] Although episiotomy has become one of the most commonly performed surgical procedures in the world, it was introduced without strong scientific evidence of its effectiveness.[2,6,7] Therefore, despite many years of its practice, the operation has remained controversial.[4] The reported rates of the procedure around the world ranges from as low as 9.7% in Sweden to 100% in Taiwan.[8] In some settings such as Argentina, episiotomy is routine for almost all women having their first delivery.[9] In Nigeria, a report from Zaria,[10] showed an episiotomy rate of 35.6% following all vaginal deliveries and 88.5% in primigravidae; while in Enugu, the rate was 40.4% for women of all parities and 76.2% in primigravidae.[4] Another recent report from Calabar, Nigeria showed a comparatively low episiotomy rate of 20.1% among all women that had a vaginal delivery; there was no stratification into parity groups.[11]
The suggested maternal benefits of episiotomy are the reduction in the likelihood of third degree perineal tears, the preservation of the muscle relaxation of the pelvic floor and perineum leading to improved sexual function, and reduced risk of fecal and urinary incontinence, as well as ease of repair and better healing than laceration because it is a straight and clean incision.[2,5] For the neonate, it is suggested that episiotomy reduces prolonged second stage in some cases of rigid perineum which could lead to fetal asphyxia, cranial trauma, cerebral hemorrhage and mental retardation; it may also reduce the possibility of fetal shoulder dystocia.[2] Conversely, the possible adverse effects of episiotomy include the iatrogenic cutting of the anal sphincter or rectum especially in midline episiotomies or unavoidable extension of the incision, the unsatisfactory anatomic results such as skin tags, asymmetry or excessive narrowing of the intriotus, vaginal prolapse, rectovaginal fistula and fistula-in-ano, increased blood loss and hematoma, pain and edema in the episiotomy region, infection and dehiscence, and sexual dysfunction.[2,12]
Primigravidae or women having their first delivery (nulliparous women) have a higher risk of episiotomies,[10] and a regular audit of the surgical procedure in this at risk group will assist in resolving the above issues. This study, therefore, aimed at determining the episiotomy rate in this vulnerable group as well as highlights the possible predictors and outcomes.
Materials and Methods
This was a retrospective cross-sectional study of all parturients with live births at the University of Nigeria Teaching Hospital (UNTH) Enugu, over a 5-year period of April 2004 to March 2009. The UNTH, Enugu is a teaching hospital owned by the Federal government of Nigeria. It is the pioneer tertiary health facility in South-eastern Nigeria, and it is currently located in Ituku-Ozalla, at the outskirt of Enugu city. The labor ward attends to an average delivery of over 700 births/year.[13] The policy on the use of episiotomy at the study center is restrictive, and the mediolateral technique is recommended when indicated using standard procedure.[1,3] Enugu State is in the South-east geopolitical zone of Nigeria, and its capital city is Enugu. Residents of the State are predominantly Igbos, and the majority of the existing 17 Local Government Areas of the State is rural.[14] Further details of the study area and UNTH Enugu, Nigeria have been described.[13]
All women who had their first delivery (primipara) within the study period were eligible for the study. Exclusion criteria included delivery by cesarean section, twin delivery, instrumental vaginal delivery such as vacuum delivery, vaginal breech delivery. The primary outcome measure was the prevalence of episiotomy in primiparous women at the study center; therefore, based on episiotomy rate in primipara of 76.2% from a previous report,[4] the sample population used in the study was adequate to determine the primary measure at a confidence level of 95% and error margin of 5%.
Eligible women were identified from the labor ward register, and appropriate data retrieved from their labor ward records. Information sought for included, mother's age, booking status, presence of episiotomy, estimated blood loss (EBL), Apgar scores at 1st min, birth weight, and the presence of perineal lacerations. Statistical Packaging for Social Sciences (SPSS) Software version 13.0. (SPSS Inc. Chicago, Illinois, USA) was used for data analyses. P < 0.05 was considered to be significant. Sample population was further stratified into two groups – episiotomy recipients, and no-episiotomy recipients; and the following secondary outcome measures were compared between the two groups – booking status, EBL, gestational age at delivery, neonatal birth weight and Apgar score, perineal laceration. Normality of continuous data was assessed with Kolmogorov–Smirnov test – all continuous data such as gestational age at delivery and the EBL, for each of the two strata of women, were nonnormally distributed (P < 0.05). Nonparametric (Mann–Whitney U) test was used to compare the associations between continuous data, while cross-tabulation (Chi-square test) was used for categorical data. Results were presented using simple percentages and tables. Associations between variables were shown using P values, prevalence ratios (PRs) and confidence intervals (CI).
For the purpose of the study, primiparous mother was defined as a woman who had her first childbirth, irrespective of the neonatal outcome, after carrying a pregnancy for at least 28 weeks (≥28 weeks). For clarity and uniformity of reporting, primigravidae as used in the study's discussion represents both primigravidae and nullipara. Perineal laceration or tear is a rent of varying degrees (first to fourth) involving the perineum of a women during vaginal birth.[3] There were no ethical issues; ethical approval was got from the Ethics committee of the study center.
Results
A total of 662 nulliparous women who had a vaginal delivery within the study period was eligible for the study. The mean age of the women was 27.3 (4.3) years; the most frequent age group of women was 20-29 years (67.0%, 442/660), while the least was 40 years and above (0.5%, 3/660). Twenty-three (3.5%) women were less than 20 years while the remaining 192 (29.0%) women were within 30-39 years. A majority (86.6%, 573/662) of women had their antenatal care at the study center (booked women).
Four hundred and eleven women had episiotomy which gave an episiotomy prevalence of 62.1%. All (100.0%) episiotomies were mediolateral. The episiotomy rate for booked women was 65.6% (376/573), while that of women referred during labor (unbooked women) was 39.3% (35/89). The observed difference was statistically significant (PR = 1.67 [95% CI: 1.28, 2.17]). The women's age distribution was similar for the episiotomy (median = 27 [interquartile range (IQR): 24-30]) and no episiotomy groups (median = 27 [IQR: 25-30]), (Z = −1.132, P = 0.26). Episiotomy rate among women of less than 30 years (64.3%, 299/465) was not statistically different from that of women that were 30 years and above (56.9%, 111/195), (PR = 1.13 [95% CI: 0.98, 1.30]). On the other hand, the distribution of gestational age at delivery for the episiotomy group (median = 39 [IQR = 37-40 weeks]) differed significantly from that of the no-episiotomy group (median = 39 [IQR = 38-40 weeks]), (Z = −3.747, P < 0.001).
With respect to maternal and neonatal outcomes, the birth weights of babies delivered in the episiotomy group (median = 3.2 kg [IQR: 2.9-3.5]) was statistically higher than those of women who did not receive episiotomy (median, 3.1 kg [IQR: 2.7-3.4]), (Z = −3.415, P = 0.001). No woman in the episiotomy group sustained additional perineal lacerations unlike in the no-episiotomy group where 35.5% (89/251) of women sustained perineal lacerations. There was no data on the degree of lacerations.
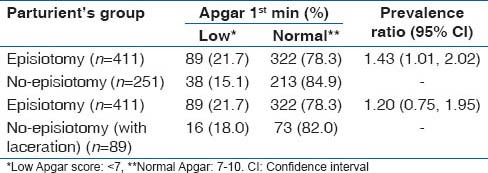
Furthermore, 21.7% (89/411) of newborn in the episiotomy group had low Apgar scores (<7) at 1st min as against 15.1% (38/251) in the no-episiotomy group. The difference was statistically significant (PR = 1.43 [95% CI: 1.01, 2.02]) [Table 1]. Similarly, the EBL during delivery varied significantly between the two groups (P = 0.03); however, when allowed for women with intact perineum (no-episiotomy without lacerations), the observed difference became non-significant (P > 0.05). Details of the association between EBL and women's episiotomy exposure groups are shown in Table 1.
Table 1.
Estimated blood loss and neonatal birth weight (episiotomy vs. no-episiotomy)
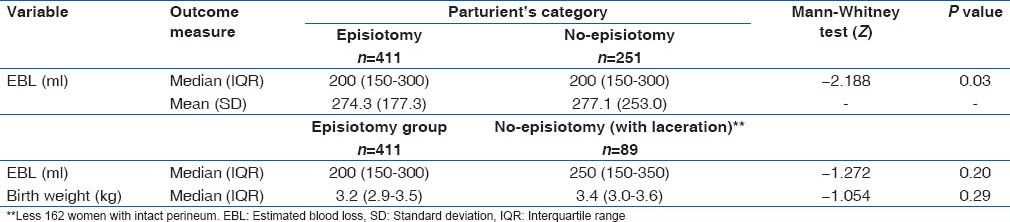
Tables 1 and 2 show that the episiotomy group did not differ from the no-episiotomy women that had perineal lacerations with respect to EBL, rate of low Apgar at 1st min, and neonatal birth weight.
Table 2.
Neonatal Apgar scores (episiotomy vs. no-episiotomy)
Discussion
Regular audit of clinical practices are necessary to identify gaps and develop strategies to improve outcome. This study reviewed the rate and predictors of episiotomy in the most at risk group – primigravidae/nullipara.[10] The episiotomy rate (62.1%) in this study was lower than the 76.2% earlier report from a study involving the study center, which may suggest a moderate reduction probably due to the increased emphasis on the restrictive use of episiotomy at the institution in line with evidence based recommendations.[2,15] Though the episiotomy rate was similar to the 62.2% observed among primigravida in a related study from South-West Nigeria,[16] it is still far higher than 10% recommended by the World Health Organization,[17] which calls for continuous retraining of labor ward staff especially the midwives who usually conduct most of the deliveries.[11] Other suggested ways to reduce episiotomy rate that may be applicable in our environment include perineal massage, use of certain birthing positions (e.g. hands and knees), and labor support.[18] Unfortunately, labor support which is an accessible and very effective maternal health intervention, is not practiced at the study center despite the fact that mothers desire it.[13] Furthermore, the episiotomy rate in this study is also lower than 88.5% and 77.1% among primigravida in Zaria, Northern Nigeria,[10] and Port-Harcourt Southern, Nigeria[19] respectively, which may suggest a more restrictive use at the study center. Though labor in unbooked women are usually more complicated than booked women,[20] this study showed that the risk of having an episiotomy among booked women was about 2 times higher than that of unbooked women – it is likely that accoucheurs were too cautious while conducting the delivery of booked women thus reducing their threshold for the administration of episiotomy for the group. Unlike the earlier study of all women that had vaginal delivery,[4] age of women did not appear to be a predictor of episiotomy in primigravida as shown in this study. Episiotomy is indicated in the second stage of labor when the perineum threatens to tear, and it may be assumed that the threat to tear has a direct relationship to the stretch ability of the perineum, which informed the development of a childbirth Trainer device currently associated with a reduction in episiotomy rates.[21] The device is an inflatable vaginal dilator used by primigravida during the last 2-3 weeks of pregnancy for daily home practice with the aim of stretching their perineum before labor so as to prevent perineal trauma during delivery.[21] That no woman in the episiotomy group had, perineal laceration may validate the judgments of the accoucheurs at the study center about the perception of “about to tear” perineum in primigravidae. Furthermore, this study identified higher gestational age at delivery, and birth weight as significant factors that increased the risk of episiotomy in primigravid women and the reasons may not be farfetched since fetal weight increased with gestational age, and larger weight of the newborn may increase the perceived threat of perineal tear.
There was a significant difference in the distribution of EBL between women who received episiotomy and those who did not. However, when women with intact perineum were excluded from the no-episiotomy group, the observed EBL difference became non-significant which suggests that the additional blood loss from women with intact perineum was responsible for the observed significant difference [Table 1]. This observation contrasts the findings of an earlier study from the center in 2002 that reported more blood loss among women who had an episiotomy when compared with women that had perineal laceration.[4] The explanation for this disparity is not clear, however, the inconsistent pattern of inaccuracies associated with visual estimation of blood,[22] which is the method used at the study center, may be a factor. Simulation exercises using predetermined quantity of blood volume on materials that simulate clinical scenarios, may improve the accuracy of visual EBL estimation in the labor room of the hospital.
The risk of developing birth asphyxia measured by low Apgar scores was marginally higher among the episiotomy group when compared to the no-episiotomy women [Table 1]. The reasons for this cannot be conclusively drawn from this study because of effects of possible confounders such as duration of labor, duration of the second state of labor, and oxytocin augmentation. However, there is the possibility of delays in delivery that might be associated with the process of administering episiotomies in this center. Clinical experience shows that preparations for the process of administering episiotomies in the hospital, including local analgesia administration and the interval before its effect, may sometimes introduce delays. Nevertheless, this explanation remains within the realm of speculation - a well-designed prospective comparative study may assist in addressing the issue of delay of delivery due to process of episiotomy administration. This study was not designed to collect data on 5 min Apgar scores because we felt that 1 min score was a better indicator of the impact of labor events including episiotomy on the newborn.[23]
In this study, perineal lacerations were observed only among women who did not receive an episiotomy. This was despite the finding that women who received episiotomy had significantly larger babies than those who did not receive an episiotomy. This observation may support the suggestion that episiotomy may be protective against unintended lacerations.[1]
The limitations of the study include the retrospective nature of the study with its inherent limitations and weaknesses for instance, data on social status of parturients, including education status and occupation, were difficult to retrieve because of inadequate record keeping. Furthermore, as discussed for EBL, measurement errors cannot be ruled out for all variables reported in the study, however, their effects on the study's estimates were likely to be minimal and nondirectional. The retrospective nature also limited the scope of the study as the late complications of episiotomy could not studied. Finally, multivariate analyses would have ruled out the effect of confounders identified above if data were available. There is a need to monitor the acquisition and recording of relevant data in the labor ward of the hospital.
The main strength of the study is that the study population was from a tertiary university hospital of a developing country. It highlighted the progress of the pioneer teaching hospital in South-east Nigeria that attends over 700 births/year, in implementing restrictive episiotomy administration for the most vulnerable population, as well as the possible predictors to episiotomy in the group. The study findings should raise useful questions on the use of episiotomy in primigrada as well as stimulate interest in prospective research on the subject matter.
Conclusion
Episiotomy rate among primigravida in the UNTH, Enugu was high, and the predictors included booked status of women, higher gestational age at delivery, and larger neonatal birth weight. Furthermore, episiotomy appeared to protect against perineal lacerations, and it was associated with lower 1st min Apgar scores when compared with primigravidae who did not receive an episiotomy. More efforts should be made to reduce episiotomy rate in the hospital.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Ekwempu CC. Maternal injuries. In: Agboola A, editor. Textbook of Obstetrics and Gynaecology for Medical Students. 2nd ed. Ibadan: Heinemann Educational Book Plc; 2006. pp. 477–80. [Google Scholar]
- 2.Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;1:CD000081. doi: 10.1002/14651858.CD000081.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baskett TF, Calder AA, Arulkumaran S. 11th ed. Edinburgh: Elsevier Ltd; 2007. Munro Kerr's Operative Obstetrics. [Google Scholar]
- 4.Onah HE, Akani CI. Rates and predictors of episiotomy in Nigerian women. Trop J Obstet Gynaecol. 2004;21:44–5. [Google Scholar]
- 5.Ould F. Vol. 1741. London: J Buckland; A Treatise of Midwifery; pp. 145–6. Cited in Joshi A, Acharya R. Perineal outcome after restrictive use of episiotomy in primi-gravidas. JNMA J Nepal Med Assoc 2009;48:269-72. [PubMed] [Google Scholar]
- 6.Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap LC, Wenstrom KD. 22nd ed. New York: McGraw Hills; 2005. Williams Obstetrics. [Google Scholar]
- 7.Lede RL, Belizán JM, Carroli G. Is routine use of episiotomy justified? Am J Obstet Gynecol. 1996;174:1399–402. doi: 10.1016/s0002-9378(96)70579-3. [DOI] [PubMed] [Google Scholar]
- 8.Graham ID, Carroli G, Davies C, Medves JM. Episiotomy rates around the world: An update. Birth. 2005;32:219–23. doi: 10.1111/j.0730-7659.2005.00373.x. [DOI] [PubMed] [Google Scholar]
- 9.Lede R, Moreno M, Belizan JM. Reflexiones acerca de la indicacion rutinaria de la episiotomia. Sinopsis Obstet Ginecol. 1991;38:161–6. Cited in Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;1:CD000081. [Google Scholar]
- 10.Sule ST, Shittu SO. Puerperal complications of episiotomies at Ahmadu Bello University Teaching Hospital, Zaria, Nigeria. East Afr Med J. 2003;80:351–6. doi: 10.4314/eamj.v80i7.8717. [DOI] [PubMed] [Google Scholar]
- 11.Inyang-Etoh CE, Umoiyoho AJ. The practice of episiotomy in a university teaching hospital in Nigeria. Int J Med Biomed Res. 2012;1:68–72. [Google Scholar]
- 12.Homsi R, Daikoku NH, Littlejohn J, Wheeless CR., Jr Episiotomy: Risks of dehiscence and rectovaginal fistula. Obstet Gynecol Surv. 1994;49:803–8. [PubMed] [Google Scholar]
- 13.Dim CC, Ikeme AC, Ezegwui HU, Nwagha UI. Labor support: An overlooked maternal health need in Enugu, South-Eastern Nigeria. J Matern Fetal Neonatal Med. 2011;24:471–4. doi: 10.3109/14767058.2010.501121. [DOI] [PubMed] [Google Scholar]
- 14.Ministry of Human Developments and Poverty and Reduction Enugu State; 2004; Enugu state SEED Enugu State of Nigeria, Poverty Reduction Strategy/State Economic Empowerment and Development Strategy (PRS/SEEDS) 2004-2009. [Google Scholar]
- 15.National Collaborating Centre for Women's and Children's Health. London: RCOG Press; 2007. Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. [PubMed] [Google Scholar]
- 16.Alayande BA, Amole IO, Olaolorun DA. Relative frequency and predictors of episiotomy in Ogbomosho, Nigeria. Internet J Med Update. 2012;7:41–4. [Google Scholar]
- 17.World Health Organization. Care in Normal Birth: A Practical Guide. 1996. [Last cited on 2014 Jan 17]. Available from: http://www.whqlibdoc.who.int/hq/1996/WHO_FRH_MSM_96.24.pdf .
- 18.Sullivan N. Episiotomy and How to Avoid It. MidwifeINSIGHT. 2008. [Last cited on 2014 Jan 17]. Available from: http://www.midwifeinsight.com/articles/episiotomy-and-how-to-avoid-it/
- 19.Enyindah CE, Fiebai PO, Anya SE, Okpani AO. Episiotomy and perineal trauma prevalence and obstetric risk factors in Port Harcourt, Nigeria. Niger J Med. 2007;16:242–5. [PubMed] [Google Scholar]
- 20.Chigbu B, Onwere S, Kamanu CI, Aluka C, Okoro O, Adibe E. Pregnancy outcome in booked and unbooked mothers in South Eastern Nigeria. East Afr Med J. 2009;86:267–71. doi: 10.4314/eamj.v86i6.54136. [DOI] [PubMed] [Google Scholar]
- 21.Cohain JS. Avoiding Episiotomy in the Year 2004. [Last cited on 2014 Jan 17]. Available from: http://www.leida.co.il/page.asp?id=85027 .
- 22.Schorn MN. Measurement of blood loss: Review of the literature. J Midwifery Womens Health. 2010;55:20–7. doi: 10.1016/j.jmwh.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 23.Zieve D, Kaneshiro NK. APGAR. Medline Plus. [Last cited on 2014 June 21]. Available from: http://www.nlm.nih.gov/medlineplus/ency/article/003402.htm .


