Abstract
Breast cancer risk assessment and communication are much neglected aspects of women’s health care. Breast cancer is the most prevalent cancer-related disease that touches the deepest of a women’s feelings and the subject thus attracts much of the attention of the media. Disease prevalence and media coverage are the roots of inappropriate breast cancer risk perception. Many women overestimate their personal breast cancer risk. Inappropriate risk perception precedes inappropriate health behaviour and it is pivotal to understand the underlying mechanisms in order to plan intervention. Whether interventions such as patient education through counselling and objective risk assessment are effective in restoring inappropriate breast cancer risk perception remains a question unanswered, but the tools to measure breast cancer risk are available and were validated.
Keywords: Breast neoplasm, communication, media, patient education, perception, risk assessment
Introduction
Perceived risk is defined as one’s belief about the likelihood of personal harm (Weinstein and Klein,1995). Personal health risk perceptions may be an important determinant of specific health-related behaviour and it is the pivot in a number of theoretical models on health behaviour, the Health Belief model being generally well-known (Janz and Becker, 1984). It is therefore clarifying to explore the elements underlying risk perception and to study the relationship between perceived risk and consequent health-related behaviour in order to communicate health risks to the general public in a way that health-related behaviour is changed for the better (Lipkus et al., 2000). This review summarizes present knowledge on breast cancer risk perception and risk communication, two topics that are inherently related. The subject of breast cancer risk assessment and risk communication is well researched but lacks implementation in daily clinical practice as physicians are hardly familiar with it.
Breast cancer worry
How often does one hear women say: ”It seems to me breast cancer is all over the place: in my family, in my neighbourhood, in the newspapers and on TV”. Indeed women worry a lot about getting breast cancer more than about any other disease (Wang et al., 2009). Age-adjusted incidence of breast cancer indeed has increased over time (Horner et al., 2008). There is a high frequency of thinking about breast cancer probably triggered by events in our immediate environment, the so-called “social construction of the breast cancer epidemic” (Lantz and Booth, 1998). Most common triggers reported are media reports, daily social contacts, and meeting someone who suffered breast cancer (Mc Caul et al., 1998, Montgomery et al., 2003). Societies in Western Europe characterised by an ageing population with a higher prevalence of breast cancer, a recent introduction of breast cancer screening programmes associated with an increase of breast cancer diagnoses, and a widening of the public debate about breast cancer as a result of improved treatment outcome and an increasing number of breast cancer survivors are ideal grounds to nourish this availability heuristic. When people worry about breast cancer they most often think about their personal risk, about family or friends affected, and the high prevalence of the disease. Lerman et al. reported that 30% of women with first-degree relatives who had breast cancer said that they worried about breast cancer so much that it interfered with their daily functioning and quality of life (Lerman et al., 1993).
Breast cancer risk perception
Women commonly misjudge their breast cancer risk, overestimating their lifetime risk and cancer-related death risk of a significant degree (Mc Caul et al., 1998; Bunker et al., 1998). In one study women between 40 and 50 years of age overestimated their lifetime risk by 12-fold and their short-term risk of dying from breast cancer by 22-fold (Black et al., 1995). Only 7-37% of women, depending on the demographics and the education level of the women studied, had a realistic notion of the population lifetime breast cancer risk. The proportion of women that overestimate their risk of breast cancer varies widely between 50-90% depending on the population studied and the way information was obtained (Lerman et al., 1994; Smith et al., 1996; Alexander et al., 1996; Bowen et al., 1997; Herbert-Croteau et al., 1997; Dolan et al., 1997; Woloshin et al., 1999). The mean perceived lifetime risk of developing breast cancer in studies varies between 30 and 46%, much higher than the real lifetime risk of 12%. (Bowen et al., 1997; Davids et al., 2004; Fagerlin et al., 2005). Women in particular those who are young and those with a family history of breast cancer have unreal risk perceptions (Evans et al., 1993; Daly et al., 1996; Zakowski et al., 1997; Davids et al., 2004; Katapodi et al., 2004; Haas et al., 2005).
Factors underlying breast cancer risk perception
Breast cancer risk perception is influenced by both medical (subjective and objective) (Lipkus et al., 2000) and psychological factors (Gerend et al., 2004). Medical factors include family history and age. There is body of evidence that links a family history of breast cancer to perceived risk. Notwithstanding women’s risk of developing breast cancer increases with age, older women perceive themselves as less susceptible to breast cancer than do younger women (Wilcox and Stefanick, 1999; Katapodi et al., 2004). There is a well documented discrepancy between subjective and objective medical risk (Katapodi et al., 2004). Objective medical risk is measured in terms of absolute risk (e.g. “How likely is it that one will develop breast cancer in a lifetime?”) and direct comparative risk (e.g. compared with other women of the same age, how likely is it one will develop breast cancer?”). Objective medical risk can be calculated by various mathematical tools based on the Gail model (see risk calculation and communication, Gail et al., 1989).
Psychological factors that influence breast cancer risk perception include the perceived nature and the heuristic processing of breast cancer as a health threat. Regarding the nature of a threat it is shown that the more prevalent, severe, devastating, unexpected, difficult to control the nature of a threat is, the more it is associated with higher risks of perception (Slovic, 1987). Heuristic processing of a threat involves two cognitive functions: i) the availability heuristic judging the probability of an event by the ease with which examples of that event come to mind (for example, experience with a threat – be it personal, via family/friends or via the media – increases the availability of the threat and, as a result, its perceived likelihood (Weinstein, 1987); ii) the representativeness heuristic judging the probability of an event by its similarity to events with comparable features (for example, the belief that one is similar to the type of person who develops a specific disease is associated with a higher risk perception to that disease) (Lek and Bishop, 1995). This specific factor – perceived similarity to the person who develops breast cancer- is the single strongest correlate of perceived breast cancer risk followed by the perceived prevalence of breast cancer and the vicinity of a relative/friend with breast cancer (Gerend et al., 2004).
Fear of breast cancer partly results from being confronted with a potentially lethal disease. The first question that comes up in one’s mind once diagnosed with breast cancer is: “How long have I to live? What are my chances of surviving?”. Health care professionals should at some stage in the follow-up of breast cancer treatment picture the risk of dying of breast cancer within a broader context taking into account other real risks such as death from cardiovascular disease or car accident. Non-oncological diseases as these which pose a much greater risk to a woman’s life with a worse prognosis are underestimated and their threat is perceived to be low (Phillips et al., 1999). Again this disproportionate fear of breast cancer relative to other non-cancer diseases is irrational.
Media coverage and worry about breast cancer
It is a well accepted statement that the media has a substantial effect on a women’s health perceptions (Frost et al., 1997). We referred to availability heuristic as one of the mechanisms that influences one’s perception of risk. Availability heuristic probably mediates the heightened personal and general vulnerability perceptions induced by media coverage of health topics. Women who had been exposed occasionally to programs on breast cancer on TV were twice (95% CI 1.1-3.4) more likely to be very afraid of breast cancer. Depending on the degree of media exposure the odds ratio of expressing high levels of fear of breast cancer increased to 7.5 (95% CI 2.4-23.8) (Lemal and Van den Bulck, 2009). Moreover media coverage of breast cancer is over-represented (Gerlach et al. 1997; Blanchard et al., 2002) and frequently involves personal stories with accent on emotional experiences (Atkin et al., 2008) to give it a dimension of “newsworthiness” (Lantz and Booth, 1998). The same has been found in the popular written press were stories on breast cancer misrepresent the age distribution of the disease, focusing on atypical cases of early-onset breast cancer and their often dramatic social impact. (Burke et al., 2001). These magazines are (were) known to be an important source of health information (Meissner et al., 1992; O’Keefe et al., 1998) certainly before the era of the internet. The emphasis on young age found in popular magazines follows women’s misperceptions about risk and may nourish them. The effect of risk factors related to breast cancer is another item that is miscommunicated by the popular press. In 1996, many women were concerned after publication of a review of the association of breast cancer and hormonal contraceptives which stated that the risk of breast cancer was increased by 20% in users (Collaborative Group on Hormonal Factors in Breast Cancer, 1996). If the risk was communicated as an absolute risk increase from 16 to 18.7 per 10 000 women or one additional breast cancer diagnosis per year among 3700 women taking oral contraceptive, risk perception would have been totally different. Similarly, the Women’s Health Initiative Study results of hormone replacement therapy as a primary prevention trial of chronic diseases such as cardiovascular disease were summarized in the media as a 26% increase of breast cancer in users being the main message (Rossouw et al., 2002). Again if the risk was communicated in terms of absolute risk (19 additional breast cancer for combined therapy and 5 for estrogen-only therapy per 10 000 user-years) the message would have been more shaded.
Pleas made by the medical community (Woloshin and Schwartz, 2002; Schwartz and Woloshin, 2004) and guidelines proposed by journalists (Russell, 1999; Brody, 1999) for media to present health issues in a scientifically justified and balanced way have not filtered through yet as they are inferior to commercial interests.
Breast cancer risk calculation and communication
With respect to the autonomy of women seeking medical care, providers should inform their patients to that extent that they feel comfortable in making decisions about their care. With regard to breast cancer risk perception and how to respond appropriately in terms of preventive strategies, women need accurate counselling. Communicating health risk with patients is assumed to be a part of routine care/education provided by health care professionals (Sabatino et al., 2007). In fact receiving information on heath-related issues from health care professionals in particular information about cancer risk is very much appreciated by patients (Schwartz et al., 1999; Buchanan et al., 2005). Very little is known about how breast cancer risk is assessed in daily practice. A study on risk communication defined as a discussion on health behaviour, participation in early detection or other preventive health strategies revealed that risk was discussed in only 26% of primary care visits and that risk was presented numerically in only 3% of visits (Kalet et al., 1994). Lack of knowledge and a busy consultation time schedule are obvious reasons why physicians fail to deliver effective health risk information. Breast cancer risk information is important information to be communicated with patients for a number of reasons. In the first place it is an attempt to correct inappropriate perceived risk. Secondly, evaluation of risk status may influence health-related decisions about screening (Pichert et al., 2003), chemoprevention (Howell A, 2008), referral for genetic counselling and testing (Nelson et al., 2005), and even prophylactic surgery (Evans et al., 2009). There are a number of tools available that may be worthwhile in facilitating communication about breast cancer risk (Euhus, 2001; Jacobi et al., 2009). Providing women with a personalized numerical breast cancer risk estimates on the one hand could bring the message much more clearly than general messages on breast cancer risk (Skinner et al., 1995). However, focusing on a single disease-specific risk could overemphasize that risk disproportionately to other even more important health issues (Schwartz et al., 1999).
The risk of developing breast cancer of 1 in 10 is a statistic that is often used in the popular press as it is appealing and frightening at the same time. It is even more frightening to know that the figure is on the rise. Unqualified quoting of such statistics equals disinformation of the public. However I do not see initiatives to ease the public opinion most probably out of fear that rectification of this sort of disinformation won’t help breast cancer screening programmes. From an ethical point of view this sequence of events is most questionable.
So how should one counsel a women with regard to her breast cancer risk? It is not easy task and it requires a sense of numeracy (quantitative literacy) on the patient’s part. Low numeracy is pervasive and constrains patient choice, limits access to treatments, reduces compliance with therapy, and impairs risk communication as it is associated with difficulty in understanding and assessing probabilities of risk and risk-related information, especially when that information was presented to them in a quantitative, numerical format. (Schwartz et al., 1997; Lipkus et al., 2001; Davids SL et al., 2004; Nelson et al., 2008). Intervention trials designed to improve communication on quantitative data about health risk or treatment benefit showed variable results with regard to risk perception (Woloshin and Schwartz, 1999; Vernon, 1999). Graphic displays on understanding health risks are of general benefit and may be especially helpful to those who are least numerate (Ancker et al., 2006).
As mentioned earlier there are a number of breast cancer risk assessment tools available. An overview of these tools is given by Jacobi et al. who, running the models for two healthy women from BRCA-negative/unknown status families, found that the Tyrer-Cuzick and the BOADICEA model were most appropriate in predicting breast cancer risk (Jacobi et al., 2009).
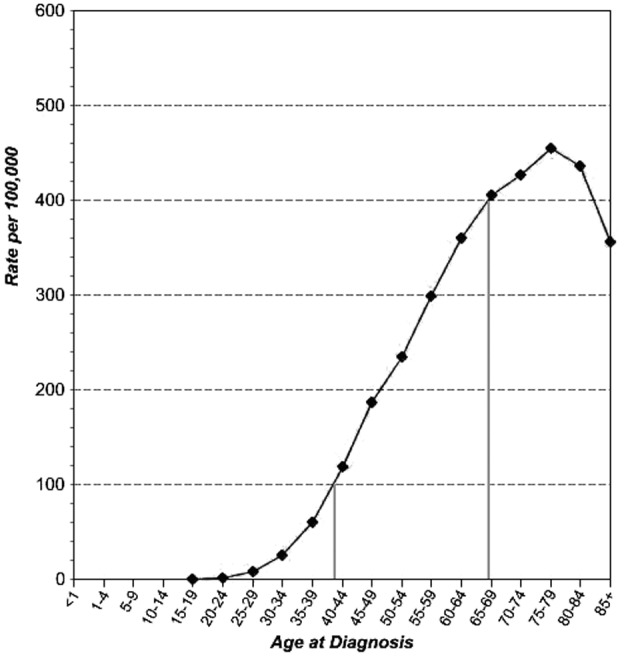
The most basic method of communicating breast cancer risk involves the use of the SEER data (Surveillance, Epidemiology, and End-Results), the most exhaustive cancer database presently available on the internet (http://seer.cancer.gov/statistics/). A lifetime table analysis of the cumulative incidence of breast cancer in the population will help to explain the 1 in 8 (12%) lifetime risk for breast cancer (Table I). From Figure 1 it is clear that at the age of 39 a women has a risk of 1 in 1000 to contract breast cancer in that calender year. For a women at the age of 69 this risk has increased to one in 250 for that year. Table 1 shows us that a women at the age of 35 have a 1 in 115 risk of getting breast cancer in the next 10 years. This risk increases with age becoming 1 in 40 by age 50, 1 in 25 by age 65. This type of age-specific data should take care of any disproportionate fear of breast cancer amongst women. These life table estimates are population-based data and represent averages that do not take into account patient-specific risk variables such as age at menarche, age at first pregnancy, a family history of breast cancer, etc. Ideally an individual should be counselled about her risk of developing breast cancer taking in consideration not only her age but also her risk factors. The most important risk factor for the development of breast cancer apart from age is a positive family history for breast cancer (Dumitrescu and Cotarla, 2005).
Table I. Probability of women developing breast cancer, all ages, all races, SEER data 2004-2006.
| Cancer Free Age | Age 25 | Age 30 | Age 35 | Age 40 | Age 45 | Age 50 | Age 55 | Age 60 | Age 65 | Age 70 | Age 75 | Age 80 | Age 85 | Age 90 | Age 95 | Age 95+ |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age 20 | 0.010 | 0.057 | 0.192 | 0.491 | 1.059 | 1.909 | 2.940 | 4.180 | 5.643 | 7.205 | 8.719 | 10.095 | 11.173 | 11.821 | 12.115 | 12.241 |
| Age 25 | 0.047 | 0.182 | 0.482 | 1.052 | 1.903 | 2.937 | 4.179 | 5.646 | 7.211 | 8.729 | 10.108 | 11.189 | 11.838 | 12.133 | 12.259 | |
| Age 30 | 0.136 | 0.437 | 1.008 | 1.862 | 2.899 | 4.146 | 5.617 | 7.187 | 8.710 | 10.093 | 11.177 | 11.828 | 12.124 | 12.251 | ||
| Age 35 | 0.302 | 0.876 | 1.735 | 2.776 | 4.028 | 5.507 | 7.084 | 8.614 | 10.004 | 11.092 | 11.747 | 12.044 | 12.171 | |||
| Age 40 | 0.579 | 1.444 | 2.493 | 3.755 | 5.245 | 6.834 | 8.376 | 9.776 | 10.874 | 11.533 | 11.833 | 11.961 | ||||
| Age 45 | 0.876 | 1.940 | 3.218 | 4.728 | 6.339 | 7.900 | 9.320 | 10.432 | 11.100 | 11.403 | 11.533 | |||||
| Age 50 | 1.085 | 2.390 | 3.930 | 5.573 | 7.167 | 8.615 | 9.750 | 10.432 | 10.741 | 10.874 | ||||||
| Age 55 | 1.341 | 2.925 | 4.614 | 6.252 | 7.741 | 8.907 | 9.608 | 9.926 | 10.062 | |||||||
| Age 60 | 1.646 | 3.401 | 5.104 | 6.651 | 7.863 | 8.591 | 8.922 | 9.063 | ||||||||
| Age 65 | 1.858 | 3.659 | 5.296 | 6.579 | 7.349 | 7.699 | 7.849 | |||||||||
| Age 70 | 1.955 | 3.732 | 5.124 | 5.961 | 6.341 | 6.503 | ||||||||||
| Age 75 | 2.007 | 3.579 | 4.524 | 4.953 | 5.136 | |||||||||||
| Age 80 | 1.898 | 3.039 | 3.557 | 3.779 | ||||||||||||
| Age 85 | 1.549 | 2.253 | 2.554 | |||||||||||||
| Age 90 | 1.166 | 1.664 |
Fig. 1. Age-specific breast cancer incidence rates, all ages, all races, SEER data 2000-2006.
The calculation of a more personalized objective medical risk is based on the Gail model (Gail et al., 1989). The original Gail model is a statistical model based on relative risk conferred by specific risk factor populations defined in the Breast Cancer Detection Demonstration Project, a large American mammography screening trial between 1973 and 1980. To date a modified version linked to updated SEER data is known as the “Breast Cancer Risk Assessment Tool” and can be found on the website of the National Cancer Institute (http://www.cancer.gov/bcrisktool/). Risk is expressed as a 5-year and a life-time absolute and comparative average risk. Risk factors that are taken into account are age, age at menarche, age at first live birth, number of first-degree relatives with breast cancer, and number of previous breast biopsies. Other risk factors, such as age at menopause, dense breast tissue on mammography, use of hormonal contraceptives or replacement therapy, high-fat diet, alcohol intake, low physical activity, obesity, or environmental exposures, are not included in risk estimates as they do not increase the accuracy of Gail model. The modified Gail model has been validated to provide accurate estimates of breast cancer risk of women without prior history of breast cancer (Costantino et al., 1999). In contrast to the Gail model which incorporates basic information on family history limited to the number of first-degree relatives only, the Claus model provides age-specific breast cancer risk estimates based on a more extensive family history including first- and second-degree relatives as well as the age at the time of diagnosis of breast cancer (Claus et al., 1994). Risk is presented as a probability of developing cancer at a certain age with five-year increments up to the age of 79. BRCAPRO, also known as the John Hopkins Bayesian model, is another statistical tool which analyzes family history information on breast and ovarian cancer even more extensively in order to determine the probability of a BRCA1/BRCA2 gene mutation in the proband (Berry et al., 2002). To do so the model uses the observed incidences of breast and ovarian cancer among BRCA1/BRCA2 gene mutation carriers and noncarriers. Given this BRCA1/BRCA2 gene mutation probability the risk of getting breast cancer is estimated. The accuracy of this estimation is based on the knowledge of the exact mutation frequency of the BRCA1/BRCA2 gene in the population this individual belongs to. The BRCAPRO Model was further refined by incorporating non-genetic risk factors such as age at menarche, age at first born, age at menopause, atypical hyperplasia, lobular carcinoma in situ, height and body mass index, known as the Tyrer-Cuzick Model (Tyrer et al., 2004). Finally, CancerGene is a software computer program (http://www8.utsouthwestern.edu/utsw/cda/dept47829/files/65844.htlm) that provides an interface for collecting risk factor information needed to run the Gail, Claus, and Bayesian model based risk predictions. The program automatically calculates breast cancer risk and BRCA gene mutation probabilities.
Older models such as the Gail and the Claus model tend to underestimate the baseline life-time risk for breast cancer as they were developed in the eighties and nineties at a time when the incidence of breast cancer was significantly lower (Jacobi et al., 2009). Therefore newer models with updated epidemiological data (NCI Breast Cancer Risk Assessment Tool) and those incorporating also personal risk factors, such as a family history of ovarian cancer, age at menarche, and age at first born (BOADICEA Model (Antoniou et al., 2004), Jonker Model (Jonker et al., 2003), Claus-Extended Formula (van Asperen et al., 2004) , Tyrer-Cuzick Model (Tyrer et al., 2004)), yield higher life-time risk estimates.
At present breast cancer risk assessment is an active research topic where in an attempt to improve risk prediction, new models using novel risk factors are developed (Gail, 2009). Adding more information or incorporating new risk factors to the proband will ultimately increase breast cancer risk estimates. This implies that current NICE guidelines regarding threshold risk for increased mammographic surveillance of ≥ 17% life-time risk based on family history risks only, need to be reconsidered (http://www.nice.org.uk/CG041).
Worry and self-protective behaviour
The relationship between worry and screening behaviour is not well established. Some researchers believe that excessive worry inhibits whilst others argue that worry facilitates screening behaviour. To date general opinion (evidence level II-3) is that thinking and worrying about breast cancer in women with a realistic perceived breast cancer risk may motivate self-protective behaviour (Leventhal et al., 1999; Consedine et al., 2004; Hay et al., 2006). Trait anxiety on the other hand does not predict self-protective behaviour. However high levels of breast cancer worry in general are said to be uncommon (Hay et al., 2006). A Flemish study though reported high levels of breast cancer fear in about 30% of a random sample of 500 women (Lemal and Van den Bulck, 2009).
Researchers distinguish between content-based worry (i.e. worry about a particular worry domain such as breast cancer) and general worry which is more related to general anxiety. The former is a “constructive” form of worrying and predicts problem solving, the latter is more predictive of avoidant coping (Davey, 1993). This is in accordance with the findings that worry about breast cancer promotes mammography screening uptake (McCaul et al., 1996) whereas anxiety appears to inhibit mammography screening (Kash et al., 1992). Studies examining the association between perceived risk and worry have noted that these variables operate independently in predicting cancer screening behaviours (McQueen et al., 2008; Moser et al., 2007). To date evidence is conflicting as to whether educational interventions as part of breast cancer early detection programs that aim to correct inappropriate perceived breast cancer risk can improve subsequent cancer screening (Vernon, 1999). This is a crucial deficit in the evidence supporting risk assessment and communication, a gap in our understanding of the mechanisms between perceived risk and impact on health behaviour that needs to be bridged before recommendations can be made. An important caveat associated with mammography breast cancer screening is the detection of an increasing number of precursor lesions with uncertain clinical significance. In those cases the ultimate diagnosis remains uncertain and in a climate of defensive medicine these women are often overtreated to anticipate progression into an invasive lesion. Indeed overdiagnosis and overtreatment are inherent to cancer screening (Zackrisson et al., 2006). Clinicians who take care of an increasing number of women with screen-detected ductal carcinoma in situ should be aware that many of these women have inaccurate perceptions of the breast cancer risk. In fact women with ductal carcinoma in situ, in spite of a better prognosis, have comparable perceptions of risk of recurrence and risk of dying of breast cancer as women with invasive disease and this causes persistent anxiety (van Gestel et al., 2007; Partridge et al., 2008).
Conclusion
Daily practice indicates that women are worried about breast cancer and overestimate their risk. This review summarizes the factors that play in the construction of breast cancer worry and perceived risk. Although physicians recognize the daily scenarios where women state that they do not wish to perform a breast self-examination out of fear of detecting a nodule as frequently as there are women who insist on having a yearly mammography, they have not taken up the challenge to rectify inappropriate health behaviour. Although physicians spent much time in counselling patients within the curative setting , counselling about preventive health care strategies including health risk communication and lifestyle management should be stepped up as an integral part of patient education. The tools as shown are available. Physicians should start using them in their clinic. As the evidence of benefit is lacking at the moment these actions should be taken within a setting of clinical research.
References
- Alexander NE, Ross J, Sumner W, Nease RF, Jr, Littenberg B. The effect of an educational intervention on the perceived risk of breast cancer. J Gen Intern Med. 1996;11:92–97. doi: 10.1007/BF02599584. [DOI] [PubMed] [Google Scholar]
- Ancker J, Senathirajah Y, Kukafka R, Starren J. Design features of graphs in health risk communication: a systematic review. J Am Med Inform Assoc. 2006;13:608–618. doi: 10.1197/jamia.M2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoniou AC, Pharoah PPD, Smith P, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br J Cancer. 2004;91:1580–1590. doi: 10.1038/sj.bjc.6602175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin CK, Smith SW, McFeters C, Ferguson V. A comprehensive analysis of breast cancer news coverage in leading media outlets focusing on environmental risk and prevention. 19. 2008;13:3–19. doi: 10.1080/10810730701806912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry DA, Iversen ES, Jr, Gudbjartsson DF, Hiller EH, Garber JE, Peshkin BN, Lerman C, Watson P, Lynch HT, Hilsenbeck SG et. BRCAPRO validation, sensitivity of genetic testing of BRCA1/BRCA2 , and prevalence of other breast cancer susceptibility genes. J Clin Oncol. 2002;20:2701–2712. doi: 10.1200/JCO.2002.05.121. [DOI] [PubMed] [Google Scholar]
- Black WC, Nease RF, Jr, Tosteson AN. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. J Natl Cancer Inst. 1995;87:720–731. doi: 10.1093/jnci/87.10.720. [DOI] [PubMed] [Google Scholar]
- Blanchard D, Erblich J, Montgomery GH, Bovbjerg DH. Read all about it: the over-representation of breast cancer in popular magazines. Prev Med. 2002;35:343–348. doi: 10.1006/pmed.2002.1088. [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Hickman KM, Powers D. Importance of psychological variables in understanding risk perceptions and breast cancer screening of African American women. Womens Health Res Gender Behav Policy. 1997;3:227–242. [PubMed] [Google Scholar]
- Brody JE. Communicating Cancer risk in print journalism. J Natl Cancer Inst Monogr. 1999;25:170–172. doi: 10.1093/oxfordjournals.jncimonographs.a024195. [DOI] [PubMed] [Google Scholar]
- Buchanan AH, Skinner CS, Rawl SM, Moser BK, Champion VL, Scott LL, Strigo TS, Bastian L. Patients’ interest in discussing cancer risk and risk management with primary care physicians. Patient Educ Couns. 2005;57:77–87. doi: 10.1016/j.pec.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Bunker JP, Houghton J, Baum M. Putting the risk of breast cancer in perspective. BMJ. 1998;317:1307–1309. doi: 10.1136/bmj.317.7168.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke W, Olsen AH, Reynolds SE, Press NA. Misleading presentation of breast cancer in popular magazines. Eff Clin Pract. 2001;4:58–64. [PubMed] [Google Scholar]
- Claus EB, Risch N, Thompson WD. Autosomal dominant inheritance of early-onset breast cancer. Cancer. 1994;73:643. doi: 10.1002/1097-0142(19940201)73:3<643::aid-cncr2820730323>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Magai C, Krivoshekova YS, Ryzewicz L, Neugut AI. Fear, anxiety, worry, and breast screening behaviour: a critical review. Cancer Epidemiol Biomarkers Prev. 13:501–510. [PubMed] [Google Scholar]
- Costantino JP, Gail MH, Pee D, Anderson S, Redmond CK, Benichou J, Wieand HS. Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst. 1999;91:1541–1548. doi: 10.1093/jnci/91.18.1541. [DOI] [PubMed] [Google Scholar]
- Daly MB, Lerman CL, Ross E, Schwartz MD, Sands CB, Masny A. Gail model breast cancer risk components are poor predictors of risk perception and screening behaviour. Breast Cancer Res Treatment. 1996;41:59–70. doi: 10.1007/BF01807037. [DOI] [PubMed] [Google Scholar]
- Davey G. A comparison of three worry questionnaires. Behav Res Ther. 1993;31:51–56. doi: 10.1016/0005-7967(93)90042-s. [DOI] [PubMed] [Google Scholar]
- Davids SL, Schapira MM, McAuliffe TL, Nattinger AB. Predictors of pessimistic breast cancer risk perceptions in a primary care population. J Gen Intern Med. 2004;19:310–315. doi: 10.1111/j.1525-1497.2004.20801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan NC, Lee AM, McDermott MM. Age-related differences in breast carcinoma knowledge, beliefs, and perceived risk among women visiting an academic general medicine practice. Cancer. 1997;80:413–420. doi: 10.1002/(sici)1097-0142(19970801)80:3<413::aid-cncr9>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Dumitrescu RG, Cotarla I. Understanding breast cancer risk – where do we stand in 2005? J Cell Mol Med. 2005;9:208–221. doi: 10.1111/j.1582-4934.2005.tb00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euhus DM. Understanding mathematical models for breast cancer risk assessment and counseling. Breast J. 2001;7:224–232. doi: 10.1046/j.1524-4741.2001.20012.x. [DOI] [PubMed] [Google Scholar]
- Evans D, Burnell L, Hopwood P, Howell A. A perception of risk in women with a family history of breast cancer. Br J Cancer. 1993;67:612–614. doi: 10.1038/bjc.1993.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DG, Baildam AD, Anderson E, Brain A, Shenton A, Vasen HF, Eccles D, Lucassen A, Pichert G, Hamed H, et al. Risk reducing mastectomy: outcome in 10 European countries. J Med Genet. 2009;46:254–258. doi: 10.1136/jmg.2008.062232. [DOI] [PubMed] [Google Scholar]
- Fagerlin A, Fisher BJ, Ubel PA. How making a risk estimate can change the feel of that risk: shifting attitudes toward breast cancer risk in a general public survey. Patient Education Counseling. 2005;57:294–299. doi: 10.1016/j.pec.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Frost K, Frank E, Maibach E. Relative risk in the news media: a quantification of misinterpretation. Am J Public Health. 1997;87:842–845. doi: 10.2105/ajph.87.5.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, Mulvihill JJ. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–1886. doi: 10.1093/jnci/81.24.1879. [DOI] [PubMed] [Google Scholar]
- Gail MH. Value of adding single-nucleotide polymorphism genotypes to a breast cancer risk model. J Natl Cancer Inst. 2009;101:959–963. doi: 10.1093/jnci/djp130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend MA, Aiken LS, West SG, Erchull MJ. Beyond medical risk: investigating the psychological factors underlying women’s perceptions of susceptibility to breast cancer, heart disease, and osteoporosis. Health Psychol. 2004;23:247–258. doi: 10.1037/0278-6133.23.3.247. [DOI] [PubMed] [Google Scholar]
- Gerlach K, Marino C, Hoffmann-Goetz L. Cancer coverage in selected women’s magazines: what information are women receiving? J Cancer Educ. 1997;12:240–244. doi: 10.1080/08858199709528496. [DOI] [PubMed] [Google Scholar]
- Haas JS, Kaplan CP, Des Jarlais G, Gildengoin V, Pérez/Stable EJ, Kerlikowske K. Perceived risk of breast cancer among women at average and increased risk. J Women’s Health. 2005;14:845–851. doi: 10.1089/jwh.2005.14.845. [DOI] [PubMed] [Google Scholar]
- Hay JL, McCaul KD, Magnan RE. Does worry about breast cancer predict screening behaviour? A meta-analysis of the prospective evidence. Prev Med. 2006;42:401–408. doi: 10.1016/j.ypmed.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Herbert-Croteau N, Goggin P, Kishchuk N. Estimation of breast cancer risk by women aged 40 and over: a population based study. Canadian J Public Health. 1997;88:392–396. doi: 10.1007/BF03403913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner MJ, Ries LAG, Krapcho M, Neyman N, Aminou R, Howlader N, Altekruse SF, Feuer EJ, Huang L, Marriot A, et al. SEER Cancer Statistics Review, 1975-2006. Bethesda, MD: National Cancer Institute; [Google Scholar]
- Howel A. The endocrine prevention of breast cancer. Best Pract Res Clin Endocrinol Metab. 2008;22:615–623. doi: 10.1016/j.beem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Jacobi CE, de Bock GH, Siegerink B, van Asperen CJ. Differences and similarities in breast cancer risk assessment models in clinical practice: which model to choose? Breast Cancer Res Treat. 2009;115:381–390. doi: 10.1007/s10549-008-0070-x. [DOI] [PubMed] [Google Scholar]
- Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Jonker MA, Jacobi CE, Hoogendoorn WE, et al. Modeling familial clustered breast cancer using published data. Cancer Epidemiol Biomarkers Prev. 2003;12:1479–1485. [PubMed] [Google Scholar]
- Kalet A, Roberts JC, Fletcher R. How do physicians talk with their patients about risks? J Gen Intern Med. 1994;9:402–404. doi: 10.1007/BF02629523. [DOI] [PubMed] [Google Scholar]
- Kash KM, Holland JC, Halper MS, Miller DG. Psychological distress and surveillance behaviours of women with a family history of breast cancer. J Natl Cancer Inst. 1992;84:24–30. doi: 10.1093/jnci/84.1.24. [DOI] [PubMed] [Google Scholar]
- Katapodi MC, Lee KA, Facione NC, Dodd MJ. Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analytic review. Prev Med. 2004;38:388–402. doi: 10.1016/j.ypmed.2003.11.012. [DOI] [PubMed] [Google Scholar]
- Lantz PM, Booth KM. The social construction of the breast cancer epidemic. Soc Sci Med. 1998;46:907–918. doi: 10.1016/s0277-9536(97)00218-9. [DOI] [PubMed] [Google Scholar]
- Lek Y, Bishop GD. Perceived vulnerability to illness threats: the role of disease type, risk factor perception and attributions. Psychol Health. 1995;10:205–217. [Google Scholar]
- Lemal M, Van den Bulck J. Television news exposure is related to fear of breast cancer. Prev Med. 2009;48:189–192. doi: 10.1016/j.ypmed.2008.11.011. [DOI] [PubMed] [Google Scholar]
- Lerman C, Daly M, Sands C, Balshem A, Lustbader E, Heggan T, Goldstein L, James J, Engstrom P. Mammography adherence and psychological distress among women at risk for breast cancer. J Natl Cancer Inst. 1993;85:1074–1080. doi: 10.1093/jnci/85.13.1074. [DOI] [PubMed] [Google Scholar]
- Lerman C, Kash K, Stefanek M. Younger women at increased risk of breast cancer: perceived risk, psychological well-being, and surveillance behavior. J Natl Cancer Inst Monogr. 1994;16:171–175. [PubMed] [Google Scholar]
- Leventhal H, Kelly K, Leventhal EA. Population risk, actual risk, perceived risk, and cancer control: a discussion. J Natl Cancer Inst Monogr. 1999;25:81–85. doi: 10.1093/oxfordjournals.jncimonographs.a024214. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Kuchibhatla M, McBride CM, Bosworth HB, Pollak KI, Siegler IC, Rimer BK. Relationships among breast cancer perceived absolute risk, comparative risk, and worries. Cancer Epidemiol Biomarkers Prev. 2000;9:973–975. [PubMed] [Google Scholar]
- Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Desic Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- McCaul KD, Branstetter AD, Schroeder DM, Glasgow RE. What is the relationship between breast cancer risk and mammography screening? A meta-analytic review. Health Psychol. 1996;15:423–429. doi: 10.1037//0278-6133.15.6.423. [DOI] [PubMed] [Google Scholar]
- McCaul KD, Branstetter AD, Donnell SM, Jacobsen K, Quinlan KB. A descriptive study of breast cancer worry. J Behav Med. 1998;21:565–579. doi: 10.1023/a:1018748712987. [DOI] [PubMed] [Google Scholar]
- McQueen A, Vernon SW, Meissner HI, Rakowski W. Risk perception and worry about cancer: does gender make a difference? J Health Commun. 2008;13:56–79. doi: 10.1080/10810730701807076. [DOI] [PubMed] [Google Scholar]
- Meissner HI, Potosky AL, Convissor R. How sources of health information relate to knowledge and use of cancer screening exams. J Community Health. 1992;17:153–165. doi: 10.1007/BF01324404. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Erblich J, DiLorenzo T, Bovbjerg DH. Family and friends with disease: their impact on perceived risk. Prev Med. 2003;37:242–249. doi: 10.1016/s0091-7435(03)00120-8. [DOI] [PubMed] [Google Scholar]
- Moser RP, McCaul K, Peters E, Nelson W, Marcus SE. Associations of perceived risk and worry with cancer health-protective actions: data from the Health Information National Trends Survey (HINTS) J Health Psychol. 2007;12:53–65. doi: 10.1177/1359105307071735. [DOI] [PubMed] [Google Scholar]
- Nelson HD, Huffman LH, Fu R, Harris EL. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2005;143:362–379. doi: 10.7326/0003-4819-143-5-200509060-00012. [DOI] [PubMed] [Google Scholar]
- Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: theory and practice. Ann Behav Med. 2008;35:261–274. doi: 10.1007/s12160-008-9037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe GJ, Boyd HH, Brown MR. Who learns preventive health care information from where: cross-channel and repertoire comparisons. Health Communication. 1998;10:25–36. doi: 10.1207/s15327027hc1001_2. [DOI] [PubMed] [Google Scholar]
- Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and hormonal contraceptives: further results. Contraception. 1996;54(suppl 3):1–106S. doi: 10.1016/s0010-7824(15)30002-0. [DOI] [PubMed] [Google Scholar]
- Partridge A, Adolff K, Blood E, Dees EC, Kaelin C, Golshan M, Ligibel J, de Moor JS, Weeks J, Emmons K, Winer E. Risk perceptions and psychosocial outcomes of women with ductal carcinoma in situ: longitudinal results from a cohort study. J Natl Cancer Inst. 2008;100:243–251. doi: 10.1093/jnci/djn010. [DOI] [PubMed] [Google Scholar]
- Pichert G, Bolliger B, Buser K, Pagani O. Evidence-based management options for women at increased breast/ovarian cancer risk. Ann Oncol. 2003;14:9–19. doi: 10.1093/annonc/mdg030. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Glendon G, Knight JA. Putting the risk of breast cancer in perspective. New Engl J Med. 1999;340:141–144. doi: 10.1056/NEJM199901143400211. [DOI] [PubMed] [Google Scholar]
- Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- Russell C. Living can be hazardous to your health:how the news media cover cancer risks. J Natl Cancer Inst Monogr. 1999;25:167–170. doi: 10.1093/oxfordjournals.jncimonographs.a024194. [DOI] [PubMed] [Google Scholar]
- Sabatino SA, McCarthy EP, Phillips RS, Burns RB. Breast cancer risk assessment and management in primary care: provider attitudes, practices, and barriers. Cancer Det Prev. 2007;31:375–383. doi: 10.1016/j.cdp.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Int Med. 1997;127:966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Welch HG. Risk communication in clinical practice: putting cancer in context. J Natl Cancer Inst Monogr. 1999;25:124–133. doi: 10.1093/oxfordjournals.jncimonographs.a024187. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S. The media matter: a call for straightforward medical reporting. Ann Intern Med. 2004;140:226–228. doi: 10.7326/0003-4819-140-3-200402030-00015. [DOI] [PubMed] [Google Scholar]
- Skinner CS, Stretcher VJ, Hospers H. Physicians’ recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1995;14:247–254. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slovic P. Perception of risk. Science. 1987;236:280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- Smith BL, Gadd MA, Lawler C, et al. Perception of breast cancer risk among women in breast center and primary care settings: correlation with age and family history of breast cancer. Surgery. 1996;120:297–303. doi: 10.1016/s0039-6060(96)80301-1. [DOI] [PubMed] [Google Scholar]
- Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23:1111–1130. doi: 10.1002/sim.1668. [DOI] [PubMed] [Google Scholar]
- van Asperen CJ, Jonker MA, Jacobi CE, van Diemen-Bakker E, Breuning MH, van Houwelingen JC, de Bock GH. Risk estimation for healthy women from breast cancer families: new insights and new strategies. Cancer Epidemiol Biomarkers Prev. 2004;13:87–93. doi: 10.1158/1055-9965.epi-03-0090. [DOI] [PubMed] [Google Scholar]
- Van Gestel YR, Voogd AC, Vingerhoets AJ, Mols F, Nieuwenhuyzen GA, van Driel OJ, van Berlo CL, van de Poll-Franse LV. A comparison of quality of life,disease impact and risk perception in women with invasive breast cancer and ductal carcinoma in situ. Eur J Cancer. 2007;43:549–556. doi: 10.1016/j.ejca.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Vernon SW. Risk perception and risk communication for cancer screening behaviors: a review. J Natl Cancer Inst Monog. 1999;25:101–119. doi: 10.1093/oxfordjournals.jncimonographs.a024184. [DOI] [PubMed] [Google Scholar]
- Wang C, Neill SM, Rothrock N, Gramling R, Sen A, Acheson LS, Rubinstein WS, et al. Comparison of risk perceptions and beliefs across common chronic diseases. Prev Med. 2009;48:197–202. doi: 10.1016/j.ypmed.2008.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND. Unrealistic optimism about susceptibility to health problems: conclusions from a community-wide sample. J Behav Med. 1987;10:481–500. doi: 10.1007/BF00846146. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Klein WM. Resistance of personal risk perceptions to debiasing interventions. Health Psychol. 1995;14:132–140. doi: 10.1037//0278-6133.14.2.132. [DOI] [PubMed] [Google Scholar]
- Wilcox S, Stefanick ML. Knowledge and perceived risk of major diseases in middle-aged and older women. Health Psychol. 1999;18:346–353. doi: 10.1037//0278-6133.18.4.346. [DOI] [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM. How can we help people make sense of medical data? Eff Clin Pract. 1999;2:176–183. [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM, Black WC, Welch HG. Women’s perceptions of breast cancer risk: how you ask matters. Med Decis Making. 1999;19:221–229. doi: 10.1177/0272989X9901900301. [DOI] [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM. Press releases: translating research into news. JAMA. 2002;287:2856–2858. doi: 10.1001/jama.287.21.2856. [DOI] [PubMed] [Google Scholar]
- Zackrisson S, Andersson I, Janzon I, Manjer J, Garne JP. Rate of over-diagnosis of breast cancer 15 years after end of Malmö mammographic screening trial: follow-up study. BMJ. 2006;332:689–692. doi: 10.1136/bmj.38764.572569.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakowski SG, Valdimarsdottir HB, Bovbjerg D, Borgen P, Holand J, Kash K. Predictors of intrusive thoughts and avoidance in women with family histories of breast cancer. Ann Behav Med. 1997;19:362–369. doi: 10.1007/BF02895155. [DOI] [PubMed] [Google Scholar]


