Abstract
Infective endocarditis complicated by abscess formation and coronary artery compression is a rare clinical event with a high mortality rate, and diagnosis requires a heightened degree of suspicion. We present the clinical, angiographic, and echocardiographic features of a 73-year-old woman who presented with dyspnea and was found to have right coronary artery compression that was secondary to abscess formation resulting from diffuse infectious endocarditis. We discuss the patient's case and briefly review the relevant medical literature. To our knowledge, this is the first reported case of abscess formation involving a native aortic valve and the right coronary artery.
Keywords: Abscess/complications; aortic diseases/complications; coronary stenosis/etiology; diagnosis, differential; endocarditis, bacterial/complications; fatal outcome; heart valve diseases/diagnosis
Infectious endocarditis (IE) occurs twice as frequently in men as in women. A higher prevalence is observed in high-risk populations such as intravenous drug users.1 Major clinical features of IE include fever, systemic emboli, congestive heart failure, and renal insufficiency; however, classic peripheral manifestations of endocarditis—splinter hemorrhages, Osler nodes, Roth spots, and Janeway lesions—are observed less often. Rarely is cardiac ischemia or myocardial infarction caused by coronary emboli or obstruction of the coronary ostia by large vegetations. Coronary artery compression by abscess formation, although even less frequent, is important to consider in patients who present with atypical features of an acute coronary syndrome. We discuss the case of an elderly patient in whom these features occurred, and we briefly review the relevant medical literature.
Case Report
A 73-year-old woman with a history of aortic stenosis, atrial fibrillation, diabetes mellitus, and a chronic gastrocutaneous fistula and sacral decubitus ulcer presented with sudden-onset back pain and shortness of breath. In the emergency department, she had a temperature of 102.2 °F, a heart rate of 123 beats/min, and a blood pressure of 119/50 mmHg. Physical examination revealed a normal S1 and S2 and a harsh grade 2/6 systolic ejection murmur that radiated to the carotid arteries. Also noted were a fistula in the left upper quadrant that drained serous fluid, and a healing sacral ulcer with minimal skin breakdown and no signs of gangrene. Laboratory results included a troponin level of 0.746 μg/L, a creatinine kinase level of 140 U/L, and a creatinine kinase-MB fraction of 11.9 ng/mL. A 12-lead electrocardiogram showed ST-segment elevation in leads V1, V2, and III, with ischemic-appearing ST-segment depression in leads I and aVL (Fig. 1). Urgent coronary angiograms revealed a mildly dilated ascending aorta and a long, tubular area of the right coronary artery with narrowing that extended almost to the crux (Fig. 2A). A possible flap suggested right coronary artery dissection, and the presumed diagnosis was coronary dissection. Computed tomographic angiograms of the ascending and descending aorta showed no dissection but revealed an irregular collection of contrast medium along the anterior right side of the aortic annulus (Fig. 2B).
Fig. 1.
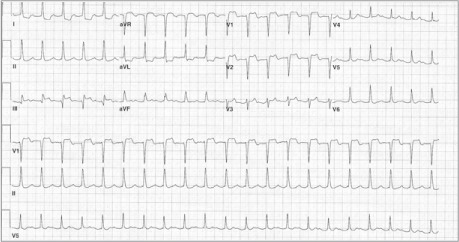
Electrocardiogram shows ST-segment elevation in leads V1, V2, and III, with ST-segment depression in leads I and aVL.
Fig. 2.
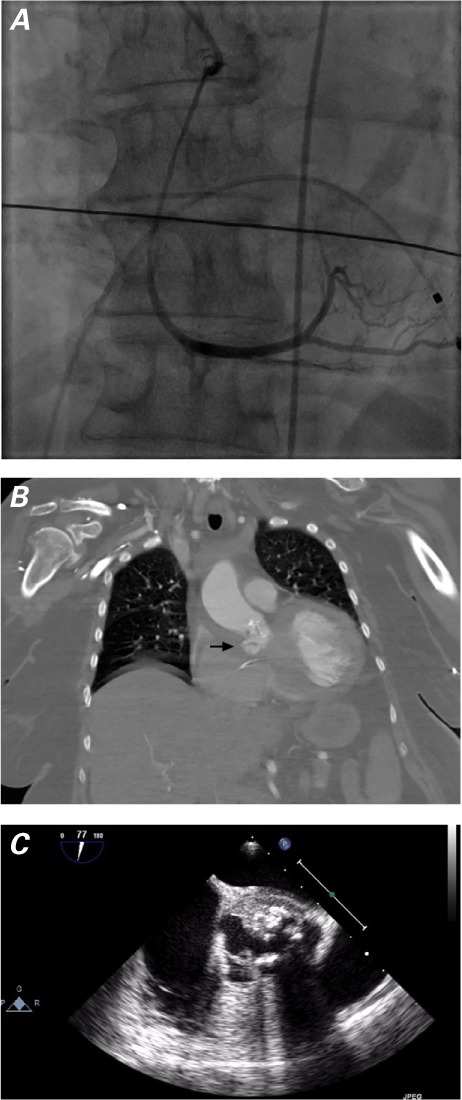
A) Coronary angiogram shows a long, tubular area of right coronary artery narrowing that extends almost to the crux. B) Computed tomographic angiogram of the aorta shows contrast medium collected along the right aortic annulus (arrow). C) Transesophageal echocardiogram shows vegetations on the aortic valve, along with an abscess in the aortic root that extends anteriorly into the right sinus of Valsalva.
The patient's history of chronic infection and elevated white blood cell count on presentation (21 ×109/L) raised concerns of IE, so further imaging of the heart was performed. Two-dimensional transthoracic echocardiograms (TTE) revealed a thickened, calcified, severely stenotic aortic valve with apparent vegetations. A 2-dimensional transesophageal echocardiogram (TEE) revealed vegetations on the aortic valve and an abscess in the aortic root that extended anteriorly into the right sinus of Valsalva (Fig. 2C). Antimicrobial therapy for endocarditis was initiated with daptomycin, aztreonam, and levofloxacin, and blood cultures were subsequently positive for coagulase-negative Staphylococcus aureus. The patient declined surgical intervention and died several days later despite aggressive medical therapy. Her family did not permit an autopsy.
Discussion
We searched the English-language medical literature for reports of adult patients with aortic valve endocarditis complicated by abscess formation and subsequent coronary artery compression.2–20 We found 21 unique cases, the earliest from 1987. Only 2 cases involved abscess compression of the right coronary circulation.9,16 Both patients had prosthetic aortic valves, and we think that ours is the first report of abscess formation involving a native aortic valve and the right coronary artery. Nine cases (43%) involved prosthetic replacement of native aortic valves that were either congenitally bicuspid or tricuspid but with significant stenosis. Surgical intervention, performed in 18 of the 21 cases, ranged from lone abscess resection to valve replacement and coronary artery bypass grafting. Leontyev and colleagues21 reviewed 172 cases of surgically repaired IE complicated by abscess formation and reported a 30-day mortality rate of 25%, with mean 1- and 5-year survival rates of 55% ± 4% and 50% ± 4%, respectively. Of these cases, 76 (44%) involved prosthetic aortic valves, which is comparable to our own reviewed percentage.
Sequelae of IE include valve destruction, embolic events, pseudoaneurysms, and abscess formation. The deleterious effects of these sequelae underscore the importance of quickly and accurately diagnosing IE. The European Society of Cardiology recommends obtaining a TTE on any patient suspected of having IE, as well as a follow-up TEE if the TTE is positive or of poor quality, or if the patient has a history of a prosthetic valve or intracardiac device. Follow-up TEE is also recommended if the initial TTE is negative but the clinical suspicion of IE is high.22 The sensitivity for detecting IE on native valves ranges from 40% to 63% with use of TTE and 90% to 100% with TEE; the ranges are slightly lower for prosthetic valves (TTE, 36%–69%; and TEE, 86%–94%).23
Given the urgency with which a patient presents during an episode of acute coronary syndrome, it is important to recognize the angiographic appearance of coronary stenosis brought on by extrinsic compression from an intracardiac abscess. Although surgical intervention is not associated with consistent outcomes, a missed diagnosis might prove fatal.3 Angiographically, an IE abscess causing compression can resemble a diffuse stenotic lesion—which, in the context of a febrile patient with an elevated white blood cell count, should help guide clinicians toward diagnoses other than atherosclerosis.
Footnotes
From: Division of Cardiology, Essentia Health, Fargo, North Dakota 58103
Dr. Jenny is now at The University of Texas Southwestern Medical Center, Dallas, Texas.
References
- 1.Hoen B, Duval X. Clinical practice. Infective endocarditis [published erratum appears in N Engl J Med. 2013;368(26): 2536] N Engl J Med. 2013;368(15):1425–33. doi: 10.1056/NEJMcp1206782. [DOI] [PubMed] [Google Scholar]
- 2.Cripps T, Guvendik L. Coronary artery compression caused by abscess formation in infective endocarditis. Int J Cardiol. 1987;14(1):99–102. doi: 10.1016/0167-5273(87)90184-7. [DOI] [PubMed] [Google Scholar]
- 3.Wickline CL, Goli VD, Buell JC. Coronary artery narrowing due to extrinsic compression by myocardial abscess. Cathet Cardiovasc Diagn. 1991;23(2):121–3. doi: 10.1002/ccd.1810230212. [DOI] [PubMed] [Google Scholar]
- 4.Dean JW, Kuo J, Wood AJ. Myocardial infarction due to coronary artery compression by aortic root abscess. Int J Cardiol. 1993;41(2):165–7. doi: 10.1016/0167-5273(93)90157-c. [DOI] [PubMed] [Google Scholar]
- 5.Vilacosta I, Camino A, Sarria C, Castillo JA, Rollan MJ, Roman JA et al. Mechanical compression of the left coronary artery resulting from periannular extension of aortic endocarditis: diagnosis by transesophageal echocardiography. Am Heart J. 1994;128(4):823–7. doi: 10.1016/0002-8703(94)90283-6. [DOI] [PubMed] [Google Scholar]
- 6.Schlaifer JD, Martin TD, Hill JA, Kerensky RA. Coronary artery obstruction caused by perivalvular abscess in aortic valve endocarditis. Am Heart J. 1996;131(2):413–6. doi: 10.1016/s0002-8703(96)90380-4. [DOI] [PubMed] [Google Scholar]
- 7.Rubin JM, Arias JC, Lambert JL. Unusual case of coronary stenosis caused by an external compression. Int J Cardiol. 1997;62(2):167–9. doi: 10.1016/s0167-5273(97)00199-x. [DOI] [PubMed] [Google Scholar]
- 8.Clarke NR, Forfar JC. Aortic root abscess presenting as unstable angina due to extrinsic compression of the left coronary artery. Postgrad Med J. 2002;78(917):168–9. doi: 10.1136/pmj.78.917.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horton CJ, Jr, Nanda NC, Nekkanti R, Mukhtar O, McGiffin D. Prosthetic aortic valve abscess producing total right coronary artery occlusion: diagnosis by transesophageal three-dimensional echocardiography. Echocardiography. 2002;19(5):395–8. doi: 10.1046/j.1540-8175.2002.00395.x. [DOI] [PubMed] [Google Scholar]
- 10.Kwok OH, Chow WH, Cheung DL. An unusual late complication of infective endocarditis. Asian Cardiovasc Thorac Ann. 2003;11(3):275. doi: 10.1177/021849230301100323. [DOI] [PubMed] [Google Scholar]
- 11.Zoffoli G, Gherli T. Images in cardiovascular medicine. Periaortic valve abscess presenting as unstable angina. Circulation. 2005;112(13):e240–1. doi: 10.1161/CIRCULATIONAHA.104.502153. [DOI] [PubMed] [Google Scholar]
- 12.Lembcke A, Rogalla P, Dohmen PM. Images in cardiology: coronary artery stenosis caused by an aortic root abscess. Heart. 2005;91(10):1302. doi: 10.1136/hrt.2004.058107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowan SW, Fiser SM, Albrecht M, Fifer M, Vlahakes GJ, Madsen JC. Management of coronary artery compression caused by recurrent aortic root abscess. J Card Surg. 2008;23(3):195–7. doi: 10.1111/j.1540-8191.2008.00640.x. [DOI] [PubMed] [Google Scholar]
- 14.O'Dwyer MJ, Mahon N, McCarthy J, Colreavey F. The presentation of an aortic root abscess as an acute coronary syndrome. J Cardiothorac Vasc Anesth. 2008;22(3):446–8. doi: 10.1053/j.jvca.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 15.Allan R, Hynes M, Burwash IG, Veinot JP, Chan KL. Coronary artery complications in infective endocarditis. Ann Thorac Surg. 2008;86(4):1381. doi: 10.1016/j.athoracsur.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 16.Pothula VR, Waked A, Sadel SM, McGinn JT, Jr, Cai J, Baldari D. Prosthetic aortic valve abscess producing intermittent right coronary artery compression. Ann Thorac Surg. 2009;87(3):963. doi: 10.1016/j.athoracsur.2008.07.074. [DOI] [PubMed] [Google Scholar]
- 17.Namboodiri N, Bohora S, Misra M, Bijulal S, Jayakumar K, Tharakan JA. Late presentation of aortic root abscess in endocarditis with coronary ischemia. Asian Cardiovasc Thorac Ann. 2009;17(6):647–9. doi: 10.1177/0218492309105567. [DOI] [PubMed] [Google Scholar]
- 18.Esen AM, Acar G, Alizade E. Prosthetic aortic valve abscess producing left main coronary artery occlusion in a patient with type IV dual left anterior descending coronary artery. J Invasive Cardiol. 2011;23(1):E233–5. [PubMed] [Google Scholar]
- 19.Misuraca L, De Cro F, De Carlo M, Barzaghi C, Scioti G, Minzioni G, Petronio AS. Left main compression by an aortic root abscess. J Cardiovasc Med. 2012;13(3):207–8. doi: 10.2459/JCM.0b013e3283511ec8. [DOI] [PubMed] [Google Scholar]
- 20.Harinstein ME, Marroquin OC. External coronary artery compression due to prosthetic valve bacterial endocarditis. Catheter Cardiovasc Interv. 2014;83(3):E168–70. doi: 10.1002/ccd.24578. [DOI] [PubMed] [Google Scholar]
- 21.Leontyev S, Borger MA, Modi P, Lehmann S, Seeburger J, Doenst T, Mohr FW. Surgical management of aortic root abscess: a 13-year experience in 172 patients with 100% follow-up. J Thorac Cardiovasc Surg. 2012;143(2):332–7. doi: 10.1016/j.jtcvs.2010.10.064. [DOI] [PubMed] [Google Scholar]
- 22.Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Disease (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J. 2009;30(19):2369–413. doi: 10.1093/eurheartj/ehp285. [DOI] [PubMed] [Google Scholar]
- 23.Evangelista A, Gonzalez-Alujas MT. Echocardiography in infective endocarditis. Heart. 2004;90(6):614–7. doi: 10.1136/hrt.2003.029868. [DOI] [PMC free article] [PubMed] [Google Scholar]


