Abstract
Background
The Institute for Behavioral and Community Health (IBACH) is a transdisciplinary organization with a team-oriented approach to the translation of research to practice and policy within the context of behavioral medicine.
Objectives
This paper tracks the growth of IBACH — in the context of evolving multi-university transdisciplinary research efforts — from a behavioral medicine research focus to community approaches to disease prevention and control, ultimately specializing in Latino health research and practice. We describe how this growth was informed by our partnerships with community members and organizations, and training a diverse array of students and young professionals.
Methods
Since 1982, IBACH’s research has evolved to address a greater breadth of factors associated with health and well-being. This was driven by our strong community focus and emphasis on collaborations, the diversity of our investigative teams, and our emphasis on training. Although behavioral science still forms the core of IBACH’s scientific orientation, research efforts extend beyond those traditionally examined.
Conclusions
IBACH’s “team science” successes have been fueled by a specific population emphasis making IBACH one of the nation’s leaders in Latino health behavior research.
Keywords: transdisciplinary research, team science, Latino/Hispanic health, community health, community-based participatory research
Introduction
Applied behavioral and public health sciences have changed dramatically over the last 50 years due to the changing nature of where they are positioned. In the 1960s and 70s, academic fields usually remained inside their protected silos. Interdisciplinary centers that fostered collaborations across academic fields began to emerge in the 1970s and 80s and have become much more common in the last 20 years. These interdisciplinary centers have strengthened our conceptualizations of applied sciences. Because academic fields are slow to change their focus and curricula, they may not be best suited to embrace changes in methodology and substance. By their very nature, interdisciplinary centers are challenged to incorporate diverse views and synthesize novel ways of thinking.
Public health is an excellent example. For most of the last century, medicine and public health were dominated by the germ theory of disease. This relatively simple explanation of health determinants did not require substantial team science and cross-disciplinary collaboration. However, by the second half of the last century, chronic diseases rather than acute problems accounted for most of the demands on the healthcare system, which had to be rebuilt to deal with new scientific understanding of disease determinants. As we move further into the 21st century, scientific thinking is changing once again. Beyond germs and risk factors for chronic disease, we now recognize that health outcomes are determined by much more complex systems and environments. Furthermore, major demographic shifts are forcing a much more complex view of how to improve and maintain the health of populations. Recognizing these rapid changes, academic fields must keep pace with the constantly changing understanding of health determinants. In this paper, we present the evolution of one institute and how it has grown and adapted to the changing understanding of health determinants. We then identify what influenced this evolution, and their implications for other researchers, practitioners, and policymakers.
Materials and Methods
Building team science
Prior to 1980, there was very little intersection between the behavioral and medical sciences. Medical school faculties had few, if any, behavioral and social scientists and these positions tended to be concentrated in departments of psychiatry. Schools of public health included people with training in the behavioral and social sciences but were still dominated by a more traditional model that emphasized epidemiology and health services research, and with few exceptions were housed in medical schools. The subordination of public health to medicine began to change in the 1960s. In 1961, the initial publication of the Framingham Heart Study demonstrated that the major risk factors for heart disease included tobacco smoking, high blood pressure, elevated cholesterol, and diabetes1.
By the end of the 1970s, health behavioral studies were gaining momentum, not just in medical schools and schools of public health, but also in traditional behavioral and social science departments. In 1978, the Society of Behavioral Medicine was founded2, which brought together professionals from the biomedical, social, and behavioral sciences. In 1982 as part of these national changes, faculty in the Department of Psychology at San Diego State University (SDSU) established the Center for Behavioral Medicine (CBM) to promote research and academic programs relevant to the applications of behavioral science principles in medicine and health care. The rationale for CBM, the forerunner of the Institute for Behavioral and Community Health (IBACH), derived from a slowly developing evidence base suggesting that behavioral research could be useful in the prevention, diagnosis, treatment, and rehabilitation of a variety of health conditions. An excellent example of the need for team science is IBACH’s leadership on the NIH-funded Nuestra Salud, observational study. Nuestra Salud examined the relationships between socioeconomic status, intermediate psychosocial and behavioral risk and protective factors, and physiologic indicators of cardiovascular-metabolic risk in Mexican American women3–6. Our focus on examining sociocontextual and other social determinants of health necessitated the involvement of investigators from a variety of disciplines including psychology, sociology, public health, and medicine. These early efforts at interdisciplinary ‘team science’ helped launch and were reinforced by the establishment of the Graduate School of Public Health at SDSU, and PhD programs in Clinical Psychology (including Behavioral Medicine) and Public Health (Epidemiology, and now Health Behavior and Global Health) jointly sponsored by SDSU and UCSD. This unique partnership was soon to be promoted as a move toward interdisciplinary approaches in the health field (e.g., Rosenfield7; Kessel, Rosenfield, and Anderson8,9).
From individual risk factors to populations and environments
Early CBM research emphasizing physiology and behavioral aspects of coping with chronic diseases established a base that allowed us to innovate and expand our perspectives. Consistent with the evolution of the team, health policy and political science researchers began to broaden IBACH’s overall perspective and evolution away from traditional behavioral medicine research to broader system and policy change. As a result, subsequent efforts have typically adopted a social-ecological perspective which emphasizes intersecting levels of influence from the broadest sociocontextual perspective (e.g., socioeconomic status, acculturation assessed at the individual, family and community level), to proximal social characteristics (e.g., social support; family relationships), to individual psychological (e.g., stress, depression) and behavioral factors (e.g., diet, exercise), with some studies even examining the physiological pathways (e.g., stress hormones, inflammation, blood pressure responses) that ultimately tie them with health outcomes. This is reflected in much of our research efforts and best exemplified by our current obesity prevention and control intervention research and chronic disease epidemiological studies. Our role as one of four field centers of the NIH-funded Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is a primary example of the latter10. HCHS/SOL seeks to determine the role of acculturation in the prevalence and development of disease and to identify risk factors playing a protective or harmful role in the health of Hispanics/Latinos. To more thoroughly address how social, cultural, and psychological factors contribute to observed patterns of Hispanic/Latino health, IBACH and other HCHS/SOL investigators initiated the HCHS/SOL Sociocultural Ancillary Study, which administered a comprehensive battery of measures of risk and protective sociocultural factors in a separate assessment of about one third of the HCHS/SOL parent study participants to better understand their roles in cardiovascular, metabolic, and other health conditions among US Hispanics.
From clinical trials to cluster randomized designs
Corresponding to the broadening of our research on risk and protective factors was a need to move away from intervention studies predicated on targeting individual health behaviors to those that more fully involved, and in some cases sought to change, the organizations serving the target audience. By the early 1990s, nearly all of IBACH’s research efforts involved their constituent organizations, such as schools, child care centers, clinics, community college classrooms, churches, recreation centers, grocery stores, restaurants, and/or communities.
From a methodological perspective, in community-based behavioral intervention studies, randomizing by individual participant may not be desirable due to concerns over contamination between participants in experimental and control conditions. When interventions are delivered within a school, for example, control participants may be exposed to all or parts of the experimental intervention. Consequently, randomly assigning an entire school (or group of schools matched or cluster) to one condition can eliminate or substantially reduce contamination. Cluster randomization has become an important design feature in community intervention studies and has been used extensively at IBACH for the past two decades. Among the IBACH studies that have used cluster randomization include the aforementioned Sembrando Salud (schools)11, Aventuras Para Niños (schools)12,13, Fe en Acción (churches), MOVE/me Muevo (recreation centers)14, Vida Sana Hoy y Mañana and El Valor de Nuestra Salud (both grocery stores)15.
Although randomization often occurs at the organizational or community level, the primary outcomes of most IBACH intervention studies are measured at the individual level and involve more than one follow-up time-point to assess both the initial efficacy of the intervention, as well as whether changes are maintained over time. It has long been recognized (e.g., Donner and Klar16; Murray17) that participants within a cluster are not statistically independent. As such sample size estimation and statistical analyses must take the clustering into account. One important element is measuring the degree of dependence using the intraclass correlation. The stronger the dependence, the greater adjustment to sample size must be made in study design, as has been the case in many IBACH efforts. To address both clustering and repeated measures, data structures are typically three levels with repeated measures nested within participants and participants nested within clusters. To handle such complex data structures, mixed effects regression models and generalized linear mixed models have been used to analyze the data. In addition to being part of the ongoing development of these models, IBACH has contributed intraclass correlation estimates to the literature (e.g., Slymen, Elder, et al.18) which can be quite useful to investigators planning studies with similar clusters and outcomes. For example, in the MOVE/me Muevo14 study we were able to demonstrate an individual-level change in obesity among girls enrolled in recreation centers after determining that there was no cluster effect for the recreation centers themselves.
Working with the community
Parallel to the complexity of cluster-randomized designs is the need to change the investigators’ perception of the “participant” away from that of a relatively passive patient in a clinical trial. Instead, we consider our participants to be part of dynamic communities and their constituent organizations who desire an active voice not only in how research is conducted but at times in its very theme. Whether our grants have comprised true “community based participatory research” (CBPR)19–21, or due to the priorities of the funding agency, “community placed research”19, it is always characterized by respect for and involvement of the community to the greatest extent possible. For example, from the Kaiser Family Foundation-funded Project Salsa of two decades ago to our current San Diego Prevention Research Center’s Familias Sanas y Activas, representatives from the community have not only selected the project’s health priorities, but have contributed to the development of the research methodology. Further, many IBACH studies utilize the “community health worker” (“promotora”) model which is critical to our ability to communicate with participants, and at the same time, contribute to the variety and depth of research in the nation22.
In randomized community trials, our respect for partner involvement and concern for the health of the community is often manifested by providing the “control group” an intervention, whether concurrent with the delivery of the intervention in the experimental condition or using the delayed treatment approach. Active control conditions have included home safety and CPR training in a tobacco and substance use prevention study (Sembrando Salud) and a cancer prevention and control curriculum in a study of church-based physical activity promotion (Fe en Acción). In fact, we were able to establish the benefits of the home safety and CPR condition in Sembrando Salud by using those exposed to the smoking/alcohol prevention condition as the control group23.
Expanding funding base: sources and foci
Consistent with changes in our research paradigm, changes also have occurred in source of funding. In the mid 1980s, CBM had funding from several institutes at the National Institutes of Health (NIH), foundation funding from the American Diabetes Association and the American Cancer Society and was home to the Minority Access to Research Careers (MARC) program funded by the National Institute of General Medical Sciences, anticipating a later emphasis on health disparities research. The early 1990s saw a rapid growth of funding for tobacco research, training, and policy evaluation efforts24, with the addition of “Prop(osition) 99,” funding to existing NIH-funded tobacco control research at IBACH. Prop 99 funding extended our ability to compete for NIH grants, including the NCI-funded Sembrando Salud11,23,25, a tobacco and substance use prevention study for children of migrant farmworkers that represented a convergence of our backgrounds in tobacco control and Latino health. This study taught us that the prevention of tobacco use simply was not perceived as a top priority by under-served Latino (largely Mexican-derived) families. Thus, we redirected our research emphases toward the promotion of healthy eating and physical activity, behaviors that are more closely linked to the major chronic disease problems of local Latino communities. The NHLBI-funded Language for Health26 and NCI-funded Secretos de la Buena Vida27,28 studies represented our first randomized trials reflecting this new emphasis and marked a transition away from tobacco control research. More recent funding from CDC reflects an interest in community-based participatory research, and funding from the Robert Wood Johnson Foundation a focus on policy and system change.
Results
From the inception of CBM in 1982 to its evolution into IBACH in 2013, investigators have transitioned from focusing on medical issues related to clinical practice to emphasizing multilevel, multisector approaches to public health research, with a specialization in Latino health research and practice. Early on, CBM/IBACH investigators built interdisciplinary collaborations between physicians and basic scientists from a variety of disciplines. This resulted in several multi-university transdisciplinary research efforts29 between SDSU and the University of California, San Diego (UCSD) School of Medicine. Figure 1 presents a few of the research studies conducted or currently underway by CBM/IBACH researchers over its 30 year history.
Figure 1.
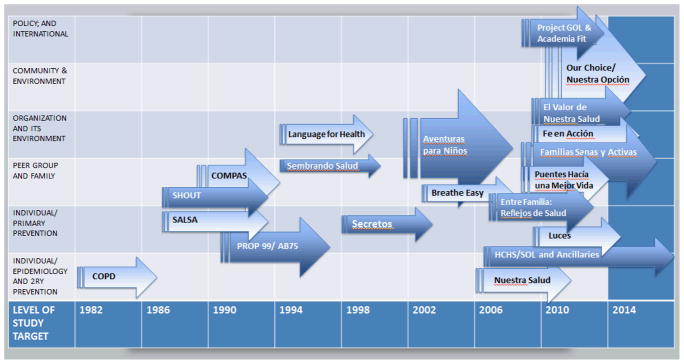
Selected IBACH Research Projects: 1982 to Present.
A general trend first toward family then organizational, community and policy intervention research, locally and internationally, is noted in this figure showing past and present IBACH projects; broader arrows denote multi-level research (e.g. individual as well as group), while more narrow ones imply an emphasis on a single level (e.g. only at the community level).
Since CBM was founded, it has witnessed major demographic changes in the San Diego region, with a rapidly growing Latino population gradually reflected in the students and new faculty hires at SDSU. Our first grant to focus exclusively on Latino health was funded in 1987. Project Salsa30 was a demonstration of community-wide approaches to promoting healthy eating and chronic disease prevention in a USA-Mexico border Spanish-speaking community, and anticipated the bulk of our subsequent research focusing on Latino health. Thus, the ethnic diversity of the IBACH faculty, student population, and research teams added a new dimension to the concept of transdisciplinary research in the institute; that is, our team has evolved to evidence racial/ethnic as well as disciplinary diversity.
This broader transdisciplinary research approach facilitated our ability to pivot toward health studies in the Mexican-American community that had theretofore received scant national research attention. As a result, we developed a deep and varied portfolio in ‘health disparities’ research well before the term was coined, which positioned us to be competitive for funding from the National Institute of Minority Health and Health Disparities (NIMHD) and other institutes. Included in this growing grant portfolio are training programs (R25) and diversity supplements emphasizing educating and mentoring Latinos and others representing underserved communities. IBACH became a leader in Latino health research and education two decades before its parent institution, SDSU, was officially designated a “Hispanic Serving Institution.”
Along with local and national efforts focusing on Latino health, funding through the San Diego Prevention Research Center (Project GOL) has helped us build a research bridge with counterpart institutions in Mexico including the Instituto Nacional De Salud Pública (INSP). INSP is considered one of the premier institutes for public health research acrossthe Americas. INSP almost exclusively serves American universities, bringing multiple contacts at international, regional, and local levels.
Finally, our work in Mexico has included co-sponsoring a course with colleagues from the Universidad Autónoma de Baja California (UABC) for masters and doctoral level students in public health. For more than 20 years, Dr. Elder has worked closely with UABC, which houses a very large School of Medicine and other largely professional study faculties near the San Diego-Tijuana border.
Collaboration grew between researchers to focus on community approaches to disease prevention, ultimately specializing in Latino health research and practice. Our initial efforts evolved from clinical to regional community research in the US/Mexico border region. More recently, work has expanded to encompass other areas elsewhere in Mexico and in other parts of Latin America while at the same time partnering with universities on the USA’s East Coast and in the Midwest that target Cuban, Dominican and Puerto Rican communities10.
As a result of the successes at CBM, and to reflect the almost exclusive focus on primary prevention in community settings, CBM was renamed IBACH given our increasing focus capacity building and training (the latter including the mentoring of young Latino investigators from throughout the USA and the Caribbean region). Over the ensuing years the addition of researchers from other disciplines as well as bilingual/bicultural faculty has allowed us to expand our research emphases to other socioecological levels31,32 and to other communities.
Discussion
IBACH has enjoyed 30 years of success for three reasons. First, we have remained at the forefront of innovation by recognizing the complexity of human behavior, acknowledging the importance of context, and adapting our approach to research accordingly. Since its inception, multi- and trans-disciplinary teams have been assembled to address a variety of multifaceted and complex health problems, yielding important innovations in study design, behavior change, multilevel and multisector intervention methods, measurement, and statistical analyses. The recent addition of a social demographer and a health systems researcher is strengthening our team and preparing us for future research possibilities that will involve an even more diverse set of disciplines. Related is our leadership in training students and young professionals. This has forced us to continually remain forward thinking and ensure that we are not only sharing the past but also stimulating ideas for the future.
Second, we have strived to ensure that our research is relevant to the needs of the community and of future generations by involving people and organizations who live and work in these communities in the research process. Over a substantial period of time it has become obvious that the population of the US (and most “Western” countries) will evidence increasingly more racial/ethnic diversity. As this demographic change was the case in California before most of the USA, the IBACH concept of “team” quickly evolved to include not only disciplinary but also racial/ethnic diversity among the investigators and the wide range of students and young professionals whom we mentored. This diversity has given us the cultural knowledge to conduct responsible research with the Latino community that is sensitive to its needs and priorities.
Finally, the interdisciplinary approach embraced by IBACH facilitates interinstitutional partnering as well as the development of a transdisciplinary perspective. By demonstrating an interest in health disparities research as well as developing the careers of young scholars from underserved communities, IBACH has been able to collaborate with a wide variety of health-related agencies, advocacy groups, and other organizations. These enduring partnerships have contributed extensively to our research and teaching success, the latter best manifested by our nationally-recognized training excellence, which has produced more than 20 PhDs with specialties in transdisciplinary research, health disparities, and the intersection of the two. The interdisciplinary theme of our research and training has strongly influenced the SDSU School of Public Health PhD program in “health behavior,” which helps meet the challenge for training transdisciplinary scientists33,34.
The development of a transdisciplinary research approach to community health research constitutes a journey and not a destination, and comprises both a conceptual ideal and practical considerations. IBACH researchers have adapted 30 years of national and regional priorities and challenges because the team is constantly evolving. Over the coming years, additional skills in engineering, social media, globalization, and infectious disease control will be among those necessary for us to thrive as we continue the evolution from multidisciplinarity to transdisciplinarity34. However, this expanded research focus can only address part of the challenge in addressing society’s health and education challenges. Scientists and engineers from traditionally disadvantaged racial/ethnic groups together comprise fewer than 10% of the workforce35. The IBACH team’s cultural diversity will optimize our potential for success in addressing the health priorities of our community.
Limitations
Although our research efforts are very much tied to the communities in which they occur and our training efforts seek to develop residents of local communities, the contents of this manuscript only reflect the opinions of researchers. This is necessitated by the fact that we have formed dozens of different partnerships over our 30 years, and it would not be appropriate to include individuals representing some of these and not others. Publications from individual projects will continue to benefit from involvement from community partners who may have a different perspective on this evolution and the factors that influenced that effort’s design, evaluation and success.
Practice Implications
The development of a transdisciplinary research approach to community health research constitutes a commitment to an ongoing journey where researchers have to be open to change and to ideas outside of their personal areas of expertise. Shifts in funding priorities and policy are needed 1) to transform investigators’ perception of the “participant” away from that of relatively passive, individual patients in a clinical trial to active community participants who are engaged in the change process, including changes to their physical and social environments, and 2) to ensure that racial and ethnic diversity among scientists better reflects that of participants and communities. There is an ongoing need for multi- and trans-disciplinary teams to address a variety of complex health problems, yielding important innovations in study design, behavior change, multilevel and multisector intervention methods, measurement, and statistical analyses.
References
- 1.Kannel W, Dawber T, Kagan A, Revotskie N, Stokes J. Factors of risk in the development of coronary heart disease–six year follow-up experience. The Framingham Study. Ann Intern Med. 1961;55:33–50. doi: 10.7326/0003-4819-55-1-33. [DOI] [PubMed] [Google Scholar]
- 2.Keefe F. Behavioral medicine: a voyage to the future. Ann Behav Med. 2011;41(2):141–151. doi: 10.1007/s12160-010-9239-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallo L, Fortmann A, Roesch S, et al. Socioeconomic status, psychosocial resources and risk, and cardiometabolic risk in Mexican-American women. Health Psychol. 2012;31(3):334–342. doi: 10.1037/a0025689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallo L, Fortmann A, De los Monteros K, et al. Individual and Neighborhood Socioeconomic Status and Inflammation in Mexican American Women: What Is the Role of Obesity? Psychosom Med. 2012;74:535–542. doi: 10.1097/PSY.0b013e31824f5f6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallo L, Shivpuri S, Gonzalez P, Fortmann A, De los Monteros KE, Matthews K. Socioeconomic status and stress in Mexican-American women: a multi-method perspective. J Behav Med. doi: 10.1007/s10865-012-9432-2. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiménez J, Shivpuri S, De los Monteros K, Matthews K, Mills P, Gallo L. Associations between socioeconomic status and catecholamine levels vary by acculturation status in Mexican-American women. Ann of Behav Med. 2012;44(1):129–135. doi: 10.1007/s12160-012-9365-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenfield P. The potential of transdisciplinary research for sustaining and extending linkages between the health and social sciences. Soc Sci Med. 1992;35(11):1343–1357. doi: 10.1016/0277-9536(92)90038-r. [DOI] [PubMed] [Google Scholar]
- 8.Kessel F, Rosenfield P, Anderson N. Expanding the Boundaries of Health and Social Science: Case Studies in Interdisciplinary Innovation. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 9.Kessel F, Rosenfield P, Anderson N. Interdisciplinary Research: Case Studies from Health and Social Science. New York, NY: Oxford University Press; 2008. [Google Scholar]
- 10.Daviglus M, Talavera G, Avilés-Santa M, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elder J, Litrownik A, Slymen D, et al. Tobacco and alcohol use-prevention program for Hispanic migrant adolescents. Am J Prev Med. 2002;23(4):269–275. doi: 10.1016/s0749-3797(02)00515-9. [DOI] [PubMed] [Google Scholar]
- 12.Ayala GX, Elder JP, Campbell NR, et al. Longitudinal intervention effects on parenting of the Aventuras para Niños study. Am J Prev Med. 2010;38(2):154–62. doi: 10.1016/j.amepre.2009.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crespo N, Elder J, Ayala G, et al. Results of a multi-level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Niños study. Ann Behav Med. 2012 Feb;43(1):84–100. doi: 10.1007/s12160-011-9332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carlson J, Crespo N, Patterson R, Sallis J, Elder J. Dietary-related and physical activity-related predictors of obesity in children: A 2-yr prospective study. Childhood Obes. 2012;8(2):110–115. doi: 10.1089/chi.2011.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baquero B, Ayala G, Linnan L, Laraia B, Bloom P. A food-marketing and environmental change intervention to promote fruit and vegetable consumption among Latinos through food stores: Vida Sana Hoy y Mañana. Paper presented at: 136th Meeting of the American Public Health Association; October 2008; San Diego, CA. [Google Scholar]
- 16.Donner A, Klar N. Design and Analysis of Cluster Randomization Trials in Health Research. London, England: Hodder Arnold; 2000. [Google Scholar]
- 17.Murray D. Design and Analysis of Group-Randomized Trials. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 18.Slymen D, Elder J, Litrownik A, Ayala G, Campbell N. Some methodologic issues in analyzing data from a randomized adolescent tobacco and alcohol use prevention trial. J Clin Epidemiol. 2003;56(4):332–340. doi: 10.1016/s0895-4356(03)00012-x. [DOI] [PubMed] [Google Scholar]
- 19.Horowitz C, Robinson M, Seifer S. Community-based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009;119(19):2633–2642. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Israel B, Coombe C, Cheezum R, et al. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100(11):2094–2102. doi: 10.2105/AJPH.2009.170506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minkler M. Linking science and policy through community-based participatory research to study and address health disparities. Am J Public Health. 2010;100(suppl 1):S81–S87. doi: 10.2105/AJPH.2009.165720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayala G, Vaz L, Earp J, Elder J, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ Res. 2010;25(5):815–840. doi: 10.1093/her/cyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campbell N, Ayala G, Litrownik A, Slymen D, Zavala F, Elder J. Evaluation of a first aid and home safety program for Hispanic migrant adolescents. Am J Prev Med. 2001;20(4):258–265. doi: 10.1016/s0749-3797(01)00300-2. [DOI] [PubMed] [Google Scholar]
- 24.Elder J, Edwards C, Conway T, Kenney E, Johnson C, Bennett E. Independent evaluation of the California Tobacco Education Program. Public Health Rep. 1996;111(4):353–35. [PMC free article] [PubMed] [Google Scholar]
- 25.Litrownik A, Elder J, Campbell N, et al. Evaluation of a tobacco and alcohol use prevention program for Hispanic migrant adolescents: promoting the protective factor of parent-child communication. Prev Med. 2000;31(2 pt 1):124–133. doi: 10.1006/pmed.2000.0698. [DOI] [PubMed] [Google Scholar]
- 26.Elder J, Candelaria J, Woodruff S, Criqui M, GAT, Rupp J. Results of Language for Health: cardiovascular disease nutrition education for Latino English-as-a-second-language students. Health Educ Behav. 2000;27(1):50–63. doi: 10.1177/109019810002700106. [DOI] [PubMed] [Google Scholar]
- 27.Elder J, Ayala G, Campbell N, et al. Long-term effects of a communication intervention for Spanish-dominant Latinas. Am J Prev Med. 2006;31(2):59–166. doi: 10.1016/j.amepre.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 28.Elder J, Ayala G, Campbell N, Slymen D, Lopez-Madurga ET, Engelberg M. Interpersonal and print nutrition communication for a Spanish-dominant Latino population: Secretos de la Buena Vida. Health Psychol. 2005;24(1):49–57. doi: 10.1037/0278-6133.24.1.49. [DOI] [PubMed] [Google Scholar]
- 29.Cummings J, Kiesler S. Collaborative research across disciplinary and organizational boundaries. Soc Stud Sci. 2005;35(5):703–722. [Google Scholar]
- 30.Elder J, Campbell N, Candelaria J, et al. Project Salsa: development and institutionalization of a nutritional health promotion project in a Latino community. Am J Health Promot. 1998;12(6):391–401. doi: 10.4278/0890-1171-12.6.391. [DOI] [PubMed] [Google Scholar]
- 31.Sallis J, Owen N. Physical Activity and Behavioral Medicine. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 32.Elder J, Ayala G, Parra-Medina D, Talavera G. Health communication in the Latino community: issues and approaches. Annu Rev Public Health. 2009;30:227–251. doi: 10.1146/annurev.publhealth.031308.100300. [DOI] [PubMed] [Google Scholar]
- 33.Hall K, Feng A, Moser R, Stokols D, Taylor B. Moving the science of team science forward: collaboration and creativity. Am J Prev Med. 2008;35(suppl 2):S243–S249. doi: 10.1016/j.amepre.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stokols D, Hall K, Taylor B, Moser R. The science of team science: overview of the field and introduction to the supplement. Am J Prev Med. 2008;35(suppl 2):S77–89. doi: 10.1016/j.amepre.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Falkenheim J, Burrelli J. Diversity in Science and Engineering Employment in Industry. Arlington, VA: National Center for Science and Engineering Studies, National Science Foundation; 2012. NSF publication 12–311. [Google Scholar]


