Abstract
Smoking and OSA are widely prevalent and are associated with significant morbidity and mortality. It has been hypothesized that each of these conditions adversely affects the other, leading to increased comorbidity while altering the efficacy of existing therapies. However, while the association between smoking and OSA is plausible, the evidence is less than conclusive. Cigarette smoking may increase the severity of OSA through alterations in sleep architecture, upper airway neuromuscular function, arousal mechanisms, and upper airway inflammation. Conversely, some evidence links untreated OSA with smoking addiction. Smoking cessation should improve OSA, but the evidence to support this is also limited. This article reviews the current evidence linking both conditions and the efficacy of various treatments. Limitations of the current evidence and areas in need of future investigation are also addressed.
The year 2014 marks the 50th anniversary of the groundbreaking 1964 Surgeon General’s report, Smoking and Health.1 This milestone presents a unique opportunity to reassess the adverse effects of smoking on health. Cigarette smoking remains the leading cause of preventable mortality in the United States and is a major factor in cardiovascular disease. The all-cause mortality rate among smokers is almost three times that of those who have never smoked.2 Worldwide, 5 to 6 million people die annually due to the effects of smoking.3 Compared with 50 years ago, smoking prevalence in the United States has dropped from 43% to 18% among adults aged ≥ 19 years, although some states continue to struggle with rates as high as 30%.4 More than 40 million Americans smoke and are at risk of premature morbidity and mortality.5
OSA is also common, with prevalence estimates of 2% to 14% among community-screened patients, and 21% to 90% among patients referred for sleep evaluation.6 Untreated OSA can significantly impact morbidity and mortality.7,8 An immediate danger of OSA is daytime sleepiness, with impaired concentration and decreased psychovigilance,9 resulting in increased motor vehicle and industrial accidents. In the United Kingdom, motor vehicle crashes associated with excessive daytime sleepiness (of which OSA is the most common cause among sleep disorders) account for between 15% and 20% of all accidents, and up to 23% of all deaths and serious injuries.10 Chronic untreated OSA is associated with many comorbid conditions, including hypertension,11 cardiovascular disease,8,12-14 dementia,15,16 depression,17 and possibly cancer.18,19
The degree to which smoking and OSA are related has not been well characterized. In fact, current guidelines do not discuss assessing smoking status or even offering smoking cessation when managing patients with OSA.20 The purpose of this review is to examine the evidence regarding the relationship between smoking and OSA.
Methods
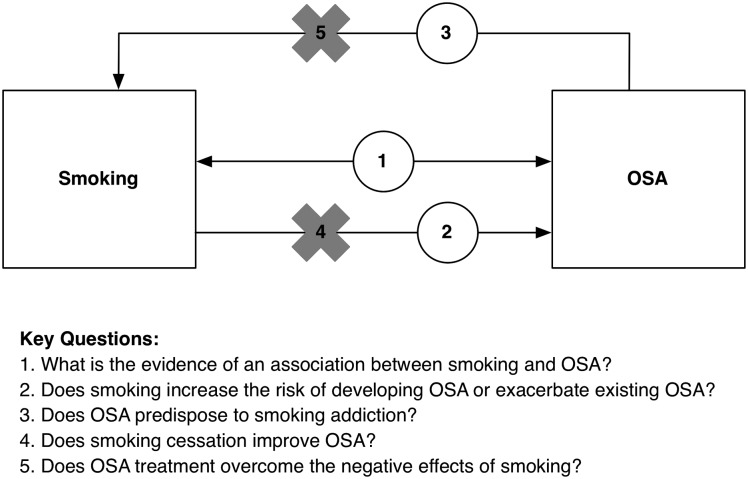
We sought to review all English-language articles in MEDLINE through March 20, 2014, that explore the relationship between cigarette smoking and sleep apnea. We identified five key questions a priori regarding the relationship between smoking and sleep apnea that provide the analytic framework for this review (Fig 1):
What is the evidence for an association between smoking and OSA?
Does smoking increase the risk of developing OSA or exacerbate existing OSA?
Does OSA predispose to smoking addiction?
Does smoking cessation improve OSA?
Does OSA treatment overcome the negative effects of smoking?
Figure 1 –
Smoking and OSA conceptual framework.
We found few prospective longitudinal studies or randomized controlled trials addressing these questions; most were cross-sectional in design. We reported the results of available studies, along with their limitations, and identified areas needing further study.
Is Smoking Associated With OSA?
A strong association between smoking and OSA has been demonstrated in observational studies. In one small cross-sectional study, investigators found a smoking prevalence of 35% in patients with OSA (apnea-hypopnea index [AHI] > 10) compared with only 18% in an unmatched group of patients without OSA (AHI < 5) (P < .01).21 Kim et al22 examined 28 male smokers and 29 male nonsmokers without COPD who underwent uvulopalatopharyngoplasty for OSA. The smokers had a higher mean AHI than did the nonsmokers (mean ± SD, 30 ± 15 vs 22 ± 11; P = .03). In a study of 301 randomly chosen Israeli driver’s license applicants, smoking several times daily was found to be the third most important predictor for sleep-disordered breathing, after age and sleepiness (Epworth Sleepiness Scale), but before BMI.23 The University of Wisconsin Sleep Cohort Study, one of the largest cohort studies to investigate OSA in the United States, reported the results of overnight polysomnography of, and health interviews with, 811 participants. Current smokers had a greater odds of moderate or severe OSA compared with nonsmokers (OR, 4.4; 95% CI, 1.5-13).24 This result persisted after adjustment for sex, age, BMI, education, daily amount of caffeinated beverages consumed, and weekly number of alcoholic beverages consumed. Persons smoking at least two packs of cigarettes each day had the greatest risks of mild OSA (OR, 6.7; 95% CI, 1.2-38) and moderate or severe OSA (OR, 40; 95% CI, 1.4-50). Former smoking, however, was not related to OSA (OR, 1.3; 95% CI, 0.8-2.3), suggesting that the predominant effect of smoking on OSA risk may be short term or the sample size of this large epidemiologic study was not sufficient to detect a difference. It appears from these studies that, even in the absence of COPD, there is a relationship between smoking and OSA.
Not all studies have found a positive association between current smoking and worsening OSA. The Sleep Heart Health Study recruited 6,132 participants from ongoing, multicenter, population-based cardiovascular and respiratory studies between 1995 and 1998.25 At every level of AHI from 1.5 to ≥ 30, there were higher proportions of never smokers compared with current smokers (P < .001). Current smokers were more likely than never smokers to have an AHI < 1.5. However, across the same categories of increasing AHI beginning at 5, former smokers were more prevalent than never smokers. Never smokers were more prevalent at AHI < 5. It is not clear which factors in this study differed from previous ones, but in this study, previous exposure to smoking was associated with worsening OSA.
Does Smoking Cause OSA?
Despite conflicting evidence and a lack of longitudinal studies supporting the association between smoking and OSA, many researchers have proposed potential mechanisms for the relationship. Commonly suggested mechanisms to explain how smoking may cause OSA include (1) changes in sleep architecture, (2) relaxation of the upper airway muscles and neural reflexes caused by nicotine, (3) increased arousal threshold from sleep caused by nicotine, and (4) increased upper airway inflammation due to smoke inhalation.
Smoking and Changes in Sleep Architecture:
One of the proposed mechanisms for the effect of smoking on OSA is disrupted sleep architecture, including sleep deprivation and sleep fragmentation.26 Several studies found an association between smoking and self-reported sleep quality. Two studies used comprehensive sleep and health questionnaires to assess sleep quality.27,28 In these studies, current smokers were significantly more likely than nonsmokers to report difficulty falling asleep, difficulty staying asleep, and daytime sleepiness. Female smokers were more likely to report daytime sleepiness, whereas male smokers were more likely to report nightmares.27 Using the 2005-2006 National Health and Nutrition Examination Survey, investigators showed that current smokers were more likely to report poorer sleep quality (less total sleep time, longer sleep latency, and increased insomnia symptoms) compared with nonsmokers and former smokers.29 Similar results were found using data from the Sleep Heart Health Study, in which current smokers were found to have longer sleep latency and a shift toward lighter sleep stages as compared with nonsmokers or former smokers.30
Subsequently, a prospective study using objective data from home sleep studies examined sleep quality in smokers compared with nonsmoking control participants matched by age, sex, race, BMI, and anthropometric measurements.31 Using EEG spectral analysis, they found that differences in sleep quality between smokers and nonsmokers were greatest in the early part of the sleep period and decreased toward the end. Another study, using in-laboratory polysomnography, compared 44 smokers with 44 healthy nonsmokers matched by age and sex. Multiple derangements of sleep were also found, including longer sleep latency, shorter sleep time, and higher rapid eye movement (REM) sleep density.32 A larger cohort study published by Conway et al,33 using in-laboratory sleep study data from 1,492 adults, demonstrated a higher arousal index in current smokers (≥ 15 pack-years) compared with nonsmokers (23 ± 18/h vs 18 ± 16/h, P < .05).
Few studies have addressed the association between the use of smokeless tobacco or exposure to second-hand smoke with sleep quality. In a large cohort study using the 2008 Behavioral Risk Factor Surveillance System, 83,072 people were enrolled.34 Current users of smokeless tobacco, including snuff and chewing tobacco, had an increased risk of insufficient rest or sleep in the previous 30 days compared with nonusers (adjusted OR, 1.5; 95% CI, 1.2-1.8), and those who both smoked cigarettes and used smokeless tobacco had the highest odds of insufficient rest or sleep (adjusted OR, 2.2; 95% CI, 1.7-2.9). Nonsmokers subjected to second-hand smoke (defined by ≥ 1 exposure days per week) had greater odds of insufficient rest or sleep compared with nonsmokers who were not exposed to second-hand smoke (adjusted OR, 1.3; 95% CI, 1.0-1.6).
Collectively, the evidence suggests the need for further objective data in support of the hypothesis that current smoking or tobacco exposure is associated with poor sleep quality leading to obstructive sleep apnea. Nonetheless, the current evidence does suggest that smoking is associated with sleep quality insufficiency, an intermediate step on the pathway toward OSA. Given that the disturbances are found during the earlier part of the night in the smoking cohort, they may be attributable to the immediate effects of nicotine and/or the effects of nicotine withdrawal during the sleep period.
Smoking and Upper Airway Neuromuscular Reflexes:
Impairment of the upper airway neuromuscular protective reflexes by nicotine is another potential explanation for the effect of smoking on sleep apnea. Supporting data come largely from physiologic studies using animal models. St-Hilaire et al35 studied laryngeal chemoreflexes in newborn lambs. They found that passive smoke exposure resulted in enhanced respiratory inhibition with laryngeal stimulation (67% vs 51% reduction in respiratory rate, P < .05) and in more apneas (2.2 vs 1.1, P < .05). In a prior study by Haxhiu et al,36 nicotine administered to the ventrolateral medullary surface of paralyzed and artificially ventilated cats before and after carotid sinus denervation increased phrenic activity and constricted the rostral segment of the trachea. These studies in animal models support the premise that nicotine exposure in the form of smoking may elicit collapsibility and constriction of the upper airways.
Data in adult humans to support this hypothesis are admittedly sparse. Indirectly, the findings of the previously cited study by Conway et al33 provide some justification for the idea. In their study, although current smokers exhibited a higher arousal index compared with nonsmokers and more total sleep time with oxyhemoglobin saturation < 90% (11% ± 17% vs 6% ± 13%, P < .05), there was no increase in AHI. This suggests that current smoking may not induce upper airways collapse, but that once collapse occurs, the upper airways’ reflexive mechanisms are not as effective in restoring airway patency. This study, interestingly, was one of the few studies that found a difference between former smokers and nonsmokers as well. Former smokers had more total sleep time with oxyhemoglobin saturation < 90% (9% ± 18% vs 6% ± 13%, P < .04) and a higher mean arousal index (20 ± 17 vs 17 ± 15, P < .04) compared with nonsmokers. The magnitude of effect of former smoking was not as large as current smoking, but some of the differences may have been related to the presence of lower airways disease, including COPD, which was not explored in the study. In humans, there may be a difference in the effects on the upper airways between cigarette smoke and nicotine. A small study of eight men with OSA exposed to nicotine gum resulted in fewer apneas and hypopneas in the first 2 h of sleep, compared with those without nicotine.37 These possibly conflicting data may also be a result of the short half-life of nicotine (2-4 h), dilating effects of nicotine on the upper airways, or varying effects over the course of a night of sleep. We could find no direct evidence in humans of upper airway neuromuscular reflex impairment during sleep following primary smoke exposure.
Smoking and Arousal Threshold:
Arousals from sleep have been implicated in the pathogenesis of smoking and OSA.38 Smoking may affect the arousal threshold, but the evidence is conflicting. Because of the short half-life of nicotine, its effects on the arousal threshold may be different during the acute effect phase vs the nicotine withdrawal phase during a single night of sleep. The hypothesis that smoking causes a higher arousal threshold is derived largely from pediatric clinical studies. In infants, environmental tobacco smoke is second only to prone positioning as a risk factor for the development of sudden infant death syndrome.39 Infants exposed to maternal smoking have reduced spontaneous and evoked arousability from sleep, again suggesting that the arousal threshold is impaired with exposure to smoke.40,41 Although the higher arousal threshold (and therefore reduction in arousals) may result in less sleep instability and decreased upper airways collapsibility,26 there may still be an effect on OSA. In a previously cited study of 1,492 adults referred for sleep evaluation, subjects who currently smoked exhibited a higher overall arousal index, but yet, during episodes of upper airways collapse, events were longer and desaturations were greater. This implies that the usual stimulus to trigger an arousal during an apneic event may also be impaired.33 Clearly, further clinical data in adults with cigarette smoke exposure are needed to substantiate this hypothesis.
Smoking and Upper Airway Inflammation:
Tobacco and other ingredients in cigarettes comprise the inhalants to which the upper airways may be exposed during smoking. Smoke exposure can contribute to airway inflammation, which can narrow the upper airways and predispose to collapse and obstructive apneas. Among 40 patients referred for nasal surgery for snoring or suspicion of sleep-disordered breathing, smokers tended to be younger than nonsmokers and had greater snoring times and snoring intensities.42 Furthermore, they tended to have a higher total nasal resistance after decongestion, independent of OSA severity or BMI. OSA alone is associated with upper airway inflammation. Kim et al22 studied 57 subjects (28 heavy smokers vs 29 nonsmokers) and, using upper airway mucosal biopsy , demonstrated that all subjects with moderate to severe OSA exhibited increased thickness and edema of the uvular mucosa lamina propria. However, patients who smoked also showed increased calcitonin gene-related peptide (a neuroinflammatory marker) in the uvular mucosa, potentially contributing to the upper airway inflammation in these patients. The finding of histologic changes to the upper airway mucosa with smoke exposure supports the theory that additional airway inflammation is caused by smoking, but further studies are warranted to directly attribute the upper airway inflammation caused by smoking to the pathogenesis of OSA.
Does OSA Predispose to Smoking?
Although we could find no longitudinal studies focusing on the incidence of smoking among patients with and without OSA, a still untested hypothesis was proposed in 1994. Wetter et al24 and Schrand43 believed that smoking becomes an addiction as individuals with undiagnosed OSA gain psychologic, emotional, physical, and societal reward from smoking. Wetter et al24 believed that individuals with frequent sleep disturbance (such as those with OSA) have nonrestorative sleep, difficulty waking up, and daytime hypersomnolence, which leads them to self-medicate through smoking.
Nicotine increases dopamine levels in the nucleus accumbens. The resultant increase in dopamine release has been shown to induce arousal and a sensation of reward, both of which have the potential to lead to addiction.44,45 Hypoxia has also been found to influence the release of dopamine levels in the carotid body.46,47 Collins48 speculated that through adaptation, long-term hypoxia (as observed in OSA) may be responsible for more nicotine binding sites observed in smokers. An increased number of nicotine binding sites is known to further perpetuate the vicious cycle of smoking. More available nicotine receptors could lead to an increase in smoking frequency. In the presence of chronic hypoxia due to hypoventilation or apnea, smoking (via nicotine) transiently augments ventilation while simultaneously stimulating the pleasure/reward center, encouraging addiction and compulsive activity. Additionally, societal pressures, such as the desire for mental alertness and a slender physique, may influence tobacco use in the obese, sleepy individual with OSA.
Nicotine can also induce stimulation of serotonergic neurons in the dorsal raphe nucleus of the pons. Stimulation of these neurons has been hypothesized to be responsible for mood improvements in patients with major depression who smoke.49 Both depression and mood disorders are common in patients with sleep apnea and thus may represent another reason why individuals with OSA may be drawn to smoking addiction.
Does Smoking Cessation Improve OSA?
Although mechanisms by which smoking can result in OSA have been explored, little has been reported regarding the effect of smoking cessation on reversing these mechanisms. Smoking cessation can be considered by duration of the cessation, by method of cessation (eg, without assistance, with nicotine replacement therapy, or with other pharmacologic aids), and by the indirect effects of cessation.
In the first 1 to 2 days after smoking cessation, symptoms of nicotine withdrawal, such as increased insomnia and irritability, may mimic OSA symptoms.50 Sometime after this initial phase, however, long-term smoking cessation appears to be beneficial for sleep quality, as compared with continued smoking. For example, in the previously mentioned National Health and Nutrition Examination Survey, current smokers showed considerably worse sleep quality as compared with former smokers.29 Similarly, in another large epidemiologic study, former smokers were found not to have a significantly increased prevalence of sleep-disordered breathing, as compared with nonsmokers.24 The temporal nature of the effects of nicotine withdrawal may explain the discrepancy (in the acute cessation phase, sleep quality is impaired), but as these withdrawal symptoms subside, sleep quality improves and the risk of sleep-disordered breathing lessens. Additional studies must follow patients with OSA who quit smoking to determine if or when any positive effects manifest.
Nicotine Replacement Therapy:
Evidence from small studies has been conflicting regarding the effect of nicotine replacement therapy on OSA. In the first study of its kind, nicotine gum was administered in a total dose of 14 mg to eight male patients with OSA (two with chronic hypoventilation and Pco2 levels > 60 mm Hg while awake) and various degrees of smoke exposure. Compared with their baseline state without nicotine, administration of nicotine gum diminished the total number of obstructive and mixed apneas during sleep.37 There was no observed effect of nicotine on end-tidal CO2 during wakefulness, on sleep patterns, or on central apneas. However, the results in this study were reported for only the first 2 h of sleep, when blood nicotine levels are believed to be at their peak.51 The effects of nicotine gum on apneas for the entire sleep period or over a longer duration remain unknown.
Among 20 nonsmoking men and women with OSA (mean AHI = 16 ± 19 in men and 11 ± 11 in women) who were randomized to receive 11 mg of transdermal nicotine for 12 h, or placebo, there were no acute improvements in snoring or sleep-disordered breathing.52 Total sleep time and sleep efficiency were decreased with the administration of nicotine. Interestingly, there was a negative correlation between serum nicotine concentration and mean duration of apnea and hypopnea events (r = −0.7, P ≤ .001). These results are consistent with self- reports from users of the nicotine patch who have described insomnia as one of the most common adverse events.50
In another study, nicotine tooth patches in doses of 2 and 4 mg that release continuous nicotine were administered in two treatments to 10 subjects with OSA.53 Although high nicotine levels were achieved in the saliva that persisted for approximately 4 h, low levels were noted in the plasma. There was no association between administration of this form of nicotine and the AHI or stages of sleep. Overall, these small studies seem to suggest that nicotine replacement therapy does not improve OSA in the acute setting.
Other Pharmacologic Aids for Smoking Cessation:
Despite bupropion and varenicline being widely prescribed as non-nicotine-based treatments for smoking cessation, their effects on OSA have not been well characterized. Although there is a paucity of data looking specifically at the effect of bupropion and sleep apnea, studies on its use as an antidepressant in the general population have indicated that it has a negative impact on sleep continuity.54 Unlike other antidepressants, bupropion does not appear to have REM-suppressant effects and may even increase the portion of REM sleep and decrease REM latency,55 potentially leading to worsened symptoms, especially for those with increased apneic events in REM sleep. A formulation of naltrexone-sustained release and bupropion-sustained release (NB32) is a fixed-dose drug combination currently being investigated for obesity treatment and for nicotine dependence in obese patients. Compared with placebo, patients administered NB32 over 56 weeks had a significant mean decrease in body weight (−1.3% vs −6.1%, P < .001).56 Although intriguing, the effects of this therapy on OSA are unclear.
Indirect Effects of Smoking Cessation on OSA:
Among the many benefits of smoking cessation is decreased morbidity from cardiopulmonary and vascular disease. Diseases such as emphysema and chronic bronchitis often demonstrate improved symptom management and control with smoking cessation. This in turn can result in less sleep disturbance from symptoms such as cough and wheezing. Nocturnal hypoxia and hypercarbia may also be improved with smoking cessation, because there is less airway inflammation, bronchoconstriction, and mucous production. These benefits may translate into improved OSA symptoms from better-quality sleep.
Undeniably, weight gain is a dreaded consequence of smoking cessation. Median weight gain after cessation is about 2 kg. About 10% of quitters, however, experience a > 13 kg increase in weight.57 Excessive weight gain may be counterproductive to OSA and may also serve to heighten one’s anxiety about his or her appearance, thus thwarting quit attempts.
Does OSA Treatment Affect Smoking?
We could find no data demonstrating a clear effect of OSA treatment on smoking behavior; however, again, there are anecdotal data. In one of the first longitudinal studies of the prolonged effects of CPAP therapy, Chaouat et al58 followed 63 men and two women after they underwent 5 years of CPAP therapy. At baseline, 50 of the 65 participants (77%) were current smokers and 27 (42%) of those were heavy smokers (> 30 pack-year history). Twenty percent of participants had an FEV1 to vital capacity ratio ≤ 65% (suggesting the presence of COPD), whereas the average FEV1 to vital capacity ratio across the cohort was 72% ± 10%. The baseline AHI was 87 ± 33 events/h, consistent with severe OSA. After a mean duration of nasal CPAP therapy of 64 ± 6 months (and mean daily use of 5.2 h/night), 30 of the 50 smokers (60%) had stopped smoking. Without a control group or adjustment for potential confounding factors, it is difficult to attribute the observed smoking cessation to CPAP therapy, but a 60% reduction in smoking in 5 years is impressive. Unfortunately, CPAP therapy did not seem to attenuate the decline in FEV1 attributable to smoking. The average annual decrease of FEV1 was 48 ± 74 mL in the 15 never smokers, 44 ± 78 mL in the 30 former smokers, and 56 ± 72 in the 20 current smokers. In the only study we could find examining the effects of surgical treatment of OSA, relief of nasal obstruction was not associated with smoking status.42 The extremely limited work in this area prevents any meaningful conclusions from being made regarding OSA treatment and smoking.
Potential Future Areas of Work
Although much has been elucidated regarding the association between smoking and OSA, this current review has identified significant areas for further exploration. Objective assessment of smoke exposure,59-63 OSA diagnosis, and OSA treatment are needed to remove the subjective bias found in many of the available studies. Many of the conflicting findings on the association between smoking and OSA may result from the short half-life of nicotine and the differences in the effects of nicotine exposure alone, tobacco smoke exposure, and/or nicotine withdrawal. Future studies should tease out the effects of each of these influences on OSA. Larger longitudinal studies would facilitate the discovery of more robust findings regarding the effects of smoking cessation on OSA, as well as the effect of OSA treatment on success rates of smoking cessation. Physiologic studies in adult patients would help to elucidate the mechanisms by which smoking may contribute to OSA and OSA severity. Much of the current evidence for the impairment of neuromuscular reflexes and arousal threshold are derived from animal models and pediatric observational studies.
Future studies also need to accurately account for confounding conditions such as COPD, which is common among patients with OSA as well as smokers and is independently associated with additional morbidity and mortality. The term “overlap syndrome” is used to describe patients with concomitant OSA and COPD. Patients with overlap syndrome have an increased rate of hospitalization and mortality compared with patients with COPD alone.64 Adjusting for overlap syndrome and other confounding conditions will allow an independent assessment of the risk of smoking and OSA.
Electronic cigarettes and other forms of nicotine administration such as cigarillos have emerged as popular substitutes for cigarettes and adjuncts to cigarettes. Studies are needed to determine the impact that these newer forms of nicotine exposure may have on patients with OSA and how they differ from conventional cigarettes. Similarly, the effects of cannabis and other inhaled substances on OSA need further exploration.
Clinically, it would be equally beneficial to know whether effective OSA management can improve the success rates of smoking cessation. Just as behavioral interventions have been implemented for weight reduction and diabetes control, a similar comprehensive behavioral therapy intervention addressing OSA therapy, smoking cessation, and coexisting unhealthy lifestyles (eg, weight gain, alcohol intake) may be effective in improving the quality and duration of life of these patients. The efficacy of such interventions would be best explored through randomized controlled trials.
Despite the high prevalence of both smoking and OSA and the biologic plausibility of an association between the two disorders, the available evidence does not conclusively establish a clinically significant relationship. This highlights the need for more definitive physiologic studies, robust longitudinal studies, and intervention-based randomized controlled trials to further characterize their association. Clarifying the effect of one disorder on the other (or perhaps more pertinent to clinical care, the effect of treatment of one disorder on the other) may have significant implications in reducing the public health and economic burdens of smoking and OSA.
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- REM
rapid eye movement
Footnotes
FUNDING/SUPPORT: Dr Thornton is supported by the National Center on Minority Health and Health Disparities [Grant 1-P60MD002265-01] and by the US Department of Health and Human Services Health Resources and Services Administration [Grant R39OT22056].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.US Surgeon General’s Advisory Committee on Smoking and Health. Smoking and Health. Washington, DC: Public Health Service; 1964. [Google Scholar]
- 2.Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341-350. [DOI] [PubMed] [Google Scholar]
- 3.Jha P. Avoidable global cancer deaths and total deaths from smoking. Nat Rev Cancer. 2009;9(9):655-664. [DOI] [PubMed] [Google Scholar]
- 4.Schroeder SA, Koh HK. Tobacco control 50 years after the 1964 surgeon general’s report. JAMA. 2014;311(2):141-143. [DOI] [PubMed] [Google Scholar]
- 5.Schroeder SA. How clinicians can help smokers to quit. JAMA. 2012;308(15):1586-1587. [DOI] [PubMed] [Google Scholar]
- 6.Myers KA, Mrkobrada M, Simel DL. Does this patient have obstructive sleep apnea? The Rational Clinical Examination systematic review. JAMA. 2013;310(7):731-741. [DOI] [PubMed] [Google Scholar]
- 7.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071-1078. [PMC free article] [PubMed] [Google Scholar]
- 8.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6(8):e1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson ML, Howard ME, Barnes M. Cognition and daytime functioning in sleep-related breathing disorders. Prog Brain Res. 2011;190:53-68. [DOI] [PubMed] [Google Scholar]
- 10.Horne JA, Reyner LA. Sleep related vehicle accidents. BMJ. 1995;310(6979):565-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378-1384. [DOI] [PubMed] [Google Scholar]
- 12.Leung RS, Bradley TD. Sleep apnea and cardiovascular disease. Am J Respir Crit Care Med. 2001;164(12):2147-2165. [DOI] [PubMed] [Google Scholar]
- 13.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163(1):19-25. [DOI] [PubMed] [Google Scholar]
- 14.Garcia-Rio F, Alonso-Fernández A, Armada E, et al. CPAP effect on recurrent episodes in patients with sleep apnea and myocardial infarction. Int J Cardiol. 2013;168(2):1328-1335. [DOI] [PubMed] [Google Scholar]
- 15.Kim SJ, Lee JH, Lee DY, Jhoo JH, Woo JI. Neurocognitive dysfunction associated with sleep quality and sleep apnea in patients with mild cognitive impairment. Am J Geriatr Psychiatry. 2011;19(4):374-381. [DOI] [PubMed] [Google Scholar]
- 16.Lal C, Strange C, Bachman D. Neurocognitive impairment in obstructive sleep apnea. Chest. 2012;141(6):1601-1610. [DOI] [PubMed] [Google Scholar]
- 17.Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med. 2006;166(16):1709-1715. [DOI] [PubMed] [Google Scholar]
- 18.Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306(6):613-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nieto FJ, Peppard PE, Young T, Finn L, Hla KM, Farré R. Sleep-disordered breathing and cancer mortality: results from the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2012;186(2):190-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epstein LJ, Kristo D, Strollo PJ, Jr, et al. ; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-276. [PMC free article] [PubMed] [Google Scholar]
- 21.Kashyap R, Hock LM, Bowman TJ. Higher prevalence of smoking in patients diagnosed as having obstructive sleep apnea. Sleep Breath. 2001;5(4):167-172. [DOI] [PubMed] [Google Scholar]
- 22.Kim KS, Kim JH, Park SY, et al. Smoking induces oropharyngeal narrowing and increases the severity of obstructive sleep apnea syndrome. J Clin Sleep Med. 2012;8(4):367-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tzischinsky O, Cohen A, Doveh E, et al. Screening for sleep disordered breathing among applicants for a professional driver’s license. J Occup Environ Med. 2012;54(10):1275-1280. [DOI] [PubMed] [Google Scholar]
- 24.Wetter DW, Young TB, Bidwell TR, Badr MS, Palta M. Smoking as a risk factor for sleep-disordered breathing. Arch Intern Med. 1994;154(19):2219-2224. [PubMed] [Google Scholar]
- 25.Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000;283(14):1829-1836. [DOI] [PubMed] [Google Scholar]
- 26.Sériès F, Roy N, Marc I. Effects of sleep deprivation and sleep fragmentation on upper airway collapsibility in normal subjects. Am J Respir Crit Care Med. 1994;150(2):481-485. [DOI] [PubMed] [Google Scholar]
- 27.Wetter DW, Young TB. The relation between cigarette smoking and sleep disturbance. Prev Med. 1994;23(3):328-334. [DOI] [PubMed] [Google Scholar]
- 28.Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Arch Intern Med. 1995;155(7):734-737. [PubMed] [Google Scholar]
- 29.McNamara JP, Wang J, Holiday DB, et al. Sleep disturbances associated with cigarette smoking. Psychol Health Med. 2014;19(4):410-419. [DOI] [PubMed] [Google Scholar]
- 30.Zhang L, Samet J, Caffo B, Punjabi NM. Cigarette smoking and nocturnal sleep architecture. Am J Epidemiol. 2006;164(6):529-537. [DOI] [PubMed] [Google Scholar]
- 31.Zhang L, Samet J, Caffo B, Bankman I, Punjabi NM. Power spectral analysis of EEG activity during sleep in cigarette smokers. Chest. 2008;133(2):427-432. [DOI] [PubMed] [Google Scholar]
- 32.Jaehne A, Unbehaun T, Feige B, Lutz UC, Batra A, Riemann D. How smoking affects sleep: a polysomnographical analysis. Sleep Med. 2012;13(10):1286-1292. [DOI] [PubMed] [Google Scholar]
- 33.Conway SG, Roizenblatt SS, Palombini L, et al. Effect of smoking habits on sleep. Braz J Med Biol Res. 2008;41(8):722-727. [DOI] [PubMed] [Google Scholar]
- 34.Sabanayagam C, Shankar A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011;12(1):7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.St-Hilaire M, Duvareille C, Avoine O, et al. Effects of postnatal smoke exposure on laryngeal chemoreflexes in newborn lambs. J Appl Physiol (1985). 2010;109(6):1820-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haxhiu MA, Deal EC, Jr, Norcia MP, Van Lunteren E, Mitra J, Cherniack NS. Medullary effects of nicotine and GABA on tracheal smooth muscle tone. Respir Physiol. 1986;64(3):351-363. [DOI] [PubMed] [Google Scholar]
- 37.Gothe B, Strohl KP, Levin S, Cherniack NS. Nicotine: a different approach to treatment of obstructive sleep apnea. Chest. 1985;87(1):11-17. [DOI] [PubMed] [Google Scholar]
- 38.Eckert DJ, Younes MK. Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol (1985). 2014;116(3):302-313. [DOI] [PubMed] [Google Scholar]
- 39.DiFranza JR, Aligne CA, Weitzman M. Prenatal and postnatal environmental tobacco smoke exposure and children’s health. Pediatrics. 2004;113(suppl 4):1007-1015. [PubMed] [Google Scholar]
- 40.Thach BT. Maturation and transformation of reflexes that protect the laryngeal airway from liquid aspiration from fetal to adult life. Am J Med. 2001;111(suppl 8A):69S-77S. [DOI] [PubMed] [Google Scholar]
- 41.Horne RSC, Parslow PM, Ferens D, et al. Arousal responses and risk factors for sudden infant death syndrome. Sleep Med. 2002;3(suppl 2):S61-S65. [DOI] [PubMed] [Google Scholar]
- 42.Virkkula P, Hytönen M, Bachour A, et al. Smoking and improvement after nasal surgery in snoring men. Am J Rhinol. 2007;21(2):169-173. [DOI] [PubMed] [Google Scholar]
- 43.Schrand JR. Is sleep apnea a predisposing factor for tobacco use? Med Hypotheses. 1996;47(6):443-448. [DOI] [PubMed] [Google Scholar]
- 44.Changeux JP, Bertrand D, Corringer PJ, et al. Brain nicotinic receptors: structure and regulation, role in learning and reinforcement. Brain Res Brain Res Rev. 1998;26(2-3):198-216. [DOI] [PubMed] [Google Scholar]
- 45.Balfour DJK. Neuroplasticity within the mesoaccumbens dopamine system and its role in tobacco dependence. Curr Drug Targets CNS Neurol Disord. 2002;1(4):413-421. [DOI] [PubMed] [Google Scholar]
- 46.Fidone S, Gonzalez C, Yoshizaki K. Effects of low oxygen on the release of dopamine from the rabbit carotid body in vitro. J Physiol. 1982;333:93-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fishman MC, Greene WL, Platika D. Oxygen chemoreception by carotid body cells in culture. Proc Natl Acad Sci U S A. 1985;82(5):1448-1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Collins AC. Genetic influences on tobacco use: a review of human and animal studies. Int J Addict. 1990-1991;25(1A):35-55. [DOI] [PubMed] [Google Scholar]
- 49.Guzmán-Marín R, Alam MN, Mihailescu S, Szymusiak R, McGinty D, Drucker-Colín R. Subcutaneous administration of nicotine changes dorsal raphe serotonergic neurons discharge rate during REM sleep. Brain Res. 2001;888(2):321-325. [DOI] [PubMed] [Google Scholar]
- 50.Colrain IM, Trinder J, Swan GE. The impact of smoking cessation on objective and subjective markers of sleep: review, synthesis, and recommendations. Nicotine Tob Res. 2004;6(6):913-925. [DOI] [PubMed] [Google Scholar]
- 51.McNabb ME, Ebert RV, McCusker K. Plasma nicotine levels produced by chewing nicotine gum. JAMA. 1982;248(7):865-868. [PubMed] [Google Scholar]
- 52.Davila DG, Hurt RD, Offord KP, Harris CD, Shepard JW., Jr Acute effects of transdermal nicotine on sleep architecture, snoring, and sleep-disordered breathing in nonsmokers. Am J Respir Crit Care Med. 1994;150(2):469-474. [DOI] [PubMed] [Google Scholar]
- 53.Zevin S, Swed E, Cahan C. Clinical effects of locally delivered nicotine in obstructive sleep apnea syndrome. Am J Ther. 2003;10(3):170-175. [DOI] [PubMed] [Google Scholar]
- 54.Winokur A, Gary KA, Rodner S, Rae-Red C, Fernando AT, Szuba MP. Depression, sleep physiology, and antidepressant drugs. Depress Anxiety. 2001;14(1):19-28. [DOI] [PubMed] [Google Scholar]
- 55.Nofzinger EA, Reynolds CF, III, Thase ME, et al. REM sleep enhancement by bupropion in depressed men. Am J Psychiatry. 1995;152(2):274-276. [DOI] [PubMed] [Google Scholar]
- 56.Greenway FL, Fujioka K, Plodkowski RA, et al. ; COR-I Study Group. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2010;376(9741):595-605. [DOI] [PubMed] [Google Scholar]
- 57.Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. N Engl J Med. 1991;324(11):739-745. [DOI] [PubMed] [Google Scholar]
- 58.Chaouat A, Weitzenblum E, Kessler R, et al. Five-year effects of nasal continuous positive airway pressure in obstructive sleep apnoea syndrome. Eur Respir J. 1997;10(11):2578-2582. [DOI] [PubMed] [Google Scholar]
- 59.Parker DR, Lasater TM, Windsor R, Wilkins J, Upegui DI, Heimdal J. The accuracy of self-reported smoking status assessed by cotinine test strips. Nicotine Tob Res. 2002;4(3):305-309. [DOI] [PubMed] [Google Scholar]
- 60.Montalto NJ, Wells WO. Validation of self-reported smoking status using saliva cotinine: a rapid semiquantitative dipstick method. Cancer Epidemiol Biomarkers Prev. 2007;16(9):1858-1862. [DOI] [PubMed] [Google Scholar]
- 61.Pérez-Ríos M, Santiago-Pérez MI, Alonso B, Malvar A, Hervada X, de Leon J. Fagerstrom test for nicotine dependence vs heavy smoking index in a general population survey. BMC Public Health. 2009;9:493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pulvers K, Scheuermann TS, Romero DR, Basora B, Luo X, Ahluwalia JS. Classifying a smoker scale in adult daily and nondaily smokers. Nicotine Tob Res. 2014;16(5):591-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Misailidi M, Tzatzarakis MN, Kavvalakis MP, Koutedakis Y, Tsatsakis AM, Flouris AD. Instruments to assess secondhand smoke exposure in large cohorts of never smokers: the smoke scales. PLoS ONE. 2014;9(1):e85809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325-331. [DOI] [PubMed] [Google Scholar]