Abstract
Background
Life-space mobility assesses the extent, frequency, and independence of an individual’s movement. Limited life-space may be an early marker of end-of-life.
Objectives
To evaluate the relation between life-space and mortality in older men.
Design
Prospective cohort study.
Setting
Six U.S. clinical sites.
Participants
Three thousand eight hundred ninety-two men aged 71–98 years, followed from 2007–2011.
Measurements
Life-space during the past month was assessed as 0 (daily restriction to one’s bedroom) to 120 (daily trips outside one’s town without assistance) and categorized into 20-point intervals. Primary outcome: non-cancer mortality. Secondary outcomes: all-cause, cardiovascular, cancer, and non-cardiovascular non-cancer mortality.
Results
Over 2.7 years (2007–2011), 373 (9.6%) men died, 230 from non-cancer causes. Unadjusted risk of non-cancer mortality was 41.2% among men with the lowest level of life-space (0–20 points, n=34) versus 2.4% among men with the highest life-space (101–120 points, n=868), a 17-fold difference. In multivariable-adjusted models, there was a strong linear trend between decreasing life-space and increasing risk of non-cancer mortality (P=0.005). Compared to men with the highest life-space, risk of non-cancer mortality was 3.8-fold higher (95%CI:1.3,11.5) among men with the lowest life-space. Each SD (24 point) decrease in life-space was associated with a 1.3-fold higher risk (1.1–1.5) of non-cancer mortality. Men who did not travel beyond their neighborhood without assistance (n=471) had a 1.5-fold higher risk (1.0–2.3) of non-cancer mortality. Results were similar for all-cause mortality and did not change after control for chronic disease burden.
Conclusion
Life-space predicted a variety of mortality endpoints in older men; scores ≤40 were associated with mortality independent of other risk factors.
Keywords: aged, mobility limitation, mortality, independence, activities of daily living
INTRODUCTION
Declining mobility is a hallmark of the aging process across multiple species that is associated with increased mortality. Older adults who maintain higher levels of energy expenditure, and therefore mobility, have decreased mortality.1 In addition, performance-based measures of mobility, such as aerobic fitness and 400-meter walk time, are strongly associated with mortality in older adults.2, 3
Life-space is a novel and integrated measure of mobility that assesses the extent, frequency, and independence of an individual’s movement within his environment.4, 5 Life-space is distinct from traditional performance-based measures of mobility because it assesses an individual’s enacted mobility rather than physical capacity at a given point in time. Life-space is therefore a multidimensional construct, conceived to be influenced by psychosocial and environmental factors in addition to physical capacity.
Life-space, as a comprehensive measure of mobility, may discriminate risk of death in older adults and thereby help to appropriately tailor care and target interventions that extend independent mobility and prevent premature mortality. The aim of this study was to test the hypothesis that lower levels of life-space are associated with greater non-cancer, all-cause, cardiovascular, and other (non-cardiovascular non-cancer) mortality.
METHODS
Study Population
Participants were from the Osteoporotic Fractures in Men (MrOS) study, a prospective observational study of aging. During the baseline examination from March 2000 to April 2002, 5,994 men ≥65 years were enrolled at six US clinical centers: Birmingham, Alabama; Minneapolis, Minnesota; Palo Alto, California; Monongahela Valley near Pittsburgh, Pennsylvania; Portland, Oregon; and San Diego, California. Men were not eligible to participate if they reported bilateral hip replacement or required assistance from another person in ambulation.6, 7 The protocol and consent forms were approved by the institutional review boards at all of the participating institutions. All participants provided written informed consent.
The University of Alabama at Birmingham Life-space Assessment 5 tool was administered by interview by trained clinic staff at the third follow-up visit for MrOS between March 2007 and March 2009 to ascertain movement in five life-space levels (described below) during the month prior to assessment. Participants with non-missing values for life-space were included in the analysis dataset for this study (n=3892; 79.8% of active participants at the third visit; 99.5% of active participants who had a clinic/home visit at the third visit).
Life-Space Assessment
Specific questions were: “During the past 4 weeks, have you been to: level 1-“other rooms of your home besides the room where you sleep?”; level 2-“an area outside your home such as your porch, deck, or patio, hallway (of an apartment building), or garage, in your own yard or driveway?”; level 3-“places in your neighborhood, other than your own yard or apartment building?”; level 4-“places outside your neighborhood, but within your town?”; level 5-“places outside your town?” For each level, participants were asked how often they traveled to that area and whether they needed assistance from equipment or another person. Participants decided their meaning of neighborhood and town.
The composite life-space score was calculated by assigning a score to each of the 5 levels and summing the 5 scores. Individual level scores were obtained by multiplying the level number (1–5) by a value for independence (2=no assistance; 1.5=use of equipment only; 1=use of another person with/without equipment) by a value for frequency (1=less than once/week; 2=1–3 times/week; 3=4–6 times/week; and 4=daily). Composite life-space scores could range from 0 (restricted to one’s bedroom) to 120 (traveled outside one’s town daily without assistance). The maximum life-space score for individuals who were restricted to their home (level 1) was 8 (daily trips outside their bedroom without any assistance); to areas outside their home (level 2) was 24; to their neighborhood (level 3) was 48, to their town (level 4) was 80, and to outside their town (level 5) was 120.
Mortality
Following life-space assessment, men were contacted by mail every 4 months. When men did not return these questionnaires and could not be reached by phone, next of kin were contacted; death certificates and medical records (where possible) were collected for all deaths. Central physician adjudicators reviewed date and cause of death from death certificates. Cause of death was broadly categorized by International Classification of Diseases (ICD)-9 codes as cardiovascular (codes 396.9–441.5), cancer (codes 141.9–205.0), and other causes (codes not in the previous categories). Follow-up for vital status was more than 99% complete during mean (SD) of 2.7 (0.6) years after life-space assessment through January 2011. The primary outcome was non-cancer mortality; we excluded cancer mortality because cancer is not a degenerative disease, and markers of longevity and aging typically have weak associations with cancer mortality.8 Secondary outcomes included total all-cause mortality, cardiovascular mortality, cancer mortality, and other mortality (non-cancer non-cardiovascular).
Other Measurements
Race (white/not white), education (≥college), and marital status (married/not married) were self-reported. Height was measured with a wall-mounted Harpenden stadiometer (Holtain Ltd, DyFed, UK), and body weight was measured with a balance beam or digital scale. Body mass index (BMI) was calculated as weight (kg)/height (m2). Overall self-rated health (excellent/good vs. fair/poor/very poor) and smoking status (never/past/current) were ascertained by questionnaire. Cognitive function was assessed by interview with the Teng modified mini-mental state (3MS) examination.
Participants reported whether a clinician had ever told them they had certain medical conditions, including diabetes, high or low thyroid, coronary heart disease (myocardial infarction, angina, or blocked coronary arteries requiring angioplasty or stenting), congestive heart failure, stroke, hypertension, peripheral vascular disease, dementia or Alzheimer’s disease, Parkinson’s disease, chronic kidney disease, chronic obstructive pulmonary disease (COPD), liver disease, rheumatoid arthritis, and non-skin non-melanoma cancer.
Depression symptoms were assessed by the Geriatric Depression Scale (score ≥6).9 Gait speed was assessed as the fastest of two trials of usual-pace walking over a 6-meter over-ground course. Physical activity was assessed with the Physical Activity Scale for the Elderly.10 Participants reported whether they had limited their activities because of back pain in the past 12 months and the degree to which pain interfered with normal work inside and outside the home (not at all/a little bit vs. moderately/quite a bit/extremely).11 Men also reported limitations in five instrumental activities of daily living (meal preparation, shopping, heavy housework, managing money, taking medications) and in four activities of daily living (walking 2–3 blocks, climbing 10 stairs, getting in/out of bed/chairs, bathing or showering); those who reported any difficulty with any activity or not doing an activity because of a health or physical problem were considered to have an IADL or ADL limitation, respectively.12
Statistical Analysis
Characteristics of men were compared across levels of life-space using ANOVA for normally distributed continuous variables, Kruskal-Wallis for skewed continuous variables, and χ2 tests for categorical variables.
Life-space was analyzed as a continuous variable (per SD decrease) and as a categorical variable using previously defined levels based on 20-point intervals (0–20;21–40;41–60;61–80;81–100;101–120).4 Restricted independent life-space was defined as confinement to one’s neighborhood if assistance (equipment or personal) was not used or available; participants with restricted independent life-space had life-space scores between 4–102 with mean (SD) of 42.1 (15.9).
Kaplan-Meier product-limit survival curves were used to illustrate survival by life-space level. Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) of mortality in relation to life-space. Base models were adjusted for age. Next, gait speed was added, as it is a strong predictor of mortality in older adults13 and together with life-space provides a fairly complete picture of an individual’s capacity for movement and actual amount of daily movement. Next, a set of potential confounders were screened to construct multivariable model: clinic, season of life-space assessment, BMI, physical activity, cognitive function, race, marital status, education, self-rated health, current smoking status, pain that interfered with normal work inside or outside the home, limited activity because of back pain, ADL limitation, IADL limitation, and each of the medical conditions listed previously. Covariates that were not significantly associated at P<0.10 with life-space or with at least one of the five mortality outcomes in age-adjusted models were dropped. All others were included in initial multivariable models. Of these, covariates that were not associated with at least one mortality outcome in initial multivariable models at P<0.05 were dropped; all others were retained in the final multivariable models.
Men who were lost to follow-up (n=13) were considered censored in all analyses. In cause-specific mortality analyses, men who died of another cause were censored at the time of their death, and 43 men were excluded because cause of death was pending adjudication at the end of follow-up.
Several sensitivity analyses were performed. To examine the extent to which life-space reflects underlying illness, we excluded men (n=1910) who reported a history of any of the following medical conditions at the time of life-space assessment: diabetes, COPD, coronary heart disease, congestive heart failure, stroke, peripheral vascular disease, or dementia/Alzheimer’s; then we re-ran age-adjusted models on the resulting “healthy” subset of the study population. To account for chronic disease burden, we adjusted multivariable models for number of self-reported medical conditions instead of individual medical conditions. To determine if living arrangements explained the relation between life-space and mortality, we excluded men (n=56) who reported living in nursing homes or assisted living centers and re-ran multivariable models.
RESULTS
Life-space scores were approximately normally distributed with mean (SD) of 84.9 (24.2) and median (IQR) of 90 (72,100). Lower levels of life-space were associated with older age, greater BMI, slower gait speed, less physical activity, and poorer cognitive function (Table 1). Men with lower levels of life-space were less likely to be white, married, have a college education, or report excellent/good health; they were more likely to report pain interfering with normal work, limited activities in the past 12 months due to back pain, ADL and IADL limitations, and a variety of medical conditions.
Table 1.
Characteristics of Men in the U.S. Osteoporotic Fractures in Men (MrOS) Study by Life-Space (LS), 2007–2009.
| Life-space score | P | ||||||
|---|---|---|---|---|---|---|---|
| LS 0–20 (N= 37) | LS 21–40 (N= 204) | LS 41–60 (N= 373) | LS 61–80 (N= 828) | LS 81–100 (N= 1581) | LS 101–120 (N= 869) | ||
|
| |||||||
| Age, y | 85.6 ± 6.5 | 83.2 ± 5.8 | 81.7 ± 5.7 | 79.8 ± 5.1 | 78.6 ± 4.8 | 77.8 ± 4.5 | <0.01 |
| BMI, kg/m2 | 29.5 ± 6.0 | 27.3 ± 5.2 | 27.1 ± 4.4 | 27.0 ± 3.8 | 27.0 ± 3.7 | 27.1 ± 3.6 | 0.01 |
| Gait speed, m/s | 0.69 ± 0.25 | 0.80 ± 0.22 | 1.0 ± 0.24 | 1.15 ± 0.22 | 1.21 ± 0.22 | 1.25 ± 0.21 | <0.01 |
| Physical activity from PASE | 26.6 ± 29.3 | 62.0 ± 51.7 | 89.1 ± 55.9 | 122.0 ± 62.3 | 139.4 ± 64.7 | 158.1 ± 68.8 | <0.01 |
| 3MS score (range 0–100) | 80.7 ± 12.3 | 85.7 ± 11.1 | 88.8 ± 9.1 | 90.9 ± 7.9 | 93.3 ± 5.2 | 93.5 ± 6.2 | <0.01 |
| Season, life-space assessment | 0.03 | ||||||
| Fall | 11 (29.7) | 51 (25.0) | 78 (20.9) | 157 (19.0) | 354 (22.4) | 179 (20.6) | |
| Winter | 7 (18.9) | 42 (20.6) | 68 (18.2) | 184 (22.2) | 277 (17.5) | 144 (16.6) | |
| Spring | 4 (10.8) | 65 (31.9) | 125 (33.5) | 265 (32) | 526 (33.3) | 308 (35.4) | |
| Summer | 15 (40.5) | 46 (22.5) | 102 (27.3) | 222 (26.8) | 424 (26.8) | 238 (27.4) | |
| White, non-Hispanic | 32 (86.5) | 178 (87.3) | 311 (83.4) | 725 (87.6) | 1464 (92.6) | 804 (92.5) | <0.01 |
| Married | 21 (56.8) | 134 (65.7) | 253 (67.8) | 642 (77.5) | 1277 (80.8) | 691 (79.5) | <0.01 |
| Excellent/good self-rated health | 25 (67.6) | 118 (57.8) | 263 (70.9) | 680 (82.2) | 1416 (89.6) | 806 (93.1) | <0.01 |
| College education or greater | 19 (51.4) | 93 (45.6) | 179 (48.0) | 436 (52.7) | 950 (60.1) | 529 (60.9) | <0.01 |
| Smoking status | 0.22 | ||||||
| Never | 12 (32.4) | 80 (39.2) | 135 (36.2) | 308 (37.2) | 648 (41.0) | 350 (40.3) | |
| Past | 24 (64.9) | 113 (55.4) | 226 (60.6) | 487 (58.8) | 887 (56.1) | 499 (57.4) | |
| Current | 1 (2.7) | 11 (5.4) | 12 (3.2) | 33 (4.0) | 45 (2.8) | 20 (2.3) | |
| Pain interfered with normal work | 11 (29.7) | 109 (53.4) | 142 (38.1) | 200 (24.2) | 270 (17.1) | 133 (15.3) | <0.01 |
| Limited activities in past 12 mo. due to back pain | 10 (27.0) | 75 (36.8) | 105 (28.2) | 155 (18.7) | 280 (17.7) | 137 (15.8) | <0.01 |
| Any ADL limitation | 30 (81.1) | 174 (85.3) | 207 (55.5) | 179 (21.6) | 238 (15.1) | 104 (12.0) | <0.01 |
| Any IADL limitation | 29 (78.4) | 142 (69.6) | 179 (48.0) | 133 (16.1) | 182 (11.5) | 66 (7.6) | <0.01 |
| Medical history | |||||||
| Diabetes | 13 (35.1) | 41 (20.1) | 84 (22.5) | 127 (15.3) | 227 (14.4) | 106 (12.2) | <0.01 |
| High thyroid | 2 (5.4) | 3 (1.5) | 18 (4.8) | 18 (2.2) | 40 (2.5) | 23 (2.6) | 0.08 |
| Low thyroid | 4 (10.8) | 17 (8.3) | 46 (12.3) | 75 (9.1) | 143 (9.1) | 72 (8.3) | 0.35 |
| Parkinson’s Disease | 0 (0) | 13 (6.4) | 15 (4.0) | 12 (1.5) | 18 (1.1) | 8 (0.9) | <0.01 |
| Liver disease | 0 (0) | 5 (2.5) | 5 (1.3) | 15 (1.8) | 31 (2.0) | 18 (2.1) | 0.87 |
| Rheumatoid arthritis | 3 (8.1) | 37 (18.1) | 45 (12.1) | 63 (7.6) | 96 (6.1) | 59 (6.8) | <0.01 |
| Coronary heart disease | 9 (24.3) | 66 (32.4) | 119 (31.9) | 217 (26.2) | 404 (25.6) | 187 (21.5) | <0.01 |
| Congestive heart failure | 6 (16.2) | 36 (17.6) | 41 (11.0) | 48 (5.8) | 102 (6.5) | 40 (4.6) | <0.01 |
| Stroke | 14 (37.8) | 33 (16.2) | 43 (11.5) | 49 (5.9) | 80 (5.1) | 48 (5.5) | <0.01 |
| Hypertension | 24 (64.9) | 124 (61.1) | 220 (59.1) | 454 (54.8) | 846 (53.5) | 462 (53.2) | 0.09 |
| Peripheral vascular disease | 1 (2.7) | 34 (16.7) | 42 (11.3) | 44 (5.3) | 77 (4.9) | 41 (4.7) | <0.01 |
| Dementia/Alzheimer’s disease | 6 (16.2) | 20 (9.8) | 22 (5.9) | 22 (2.7) | 18 (1.1) | 10 (1.2) | <0.01 |
| Chronic kidney disease | 2 (5.4) | 11 (5.4) | 15 (4.0) | 17 (2.1) | 41 (2.6) | 16 (1.8) | 0.02 |
| Non-skin (non-melanoma) cancer | 11 (29.7) | 71 (34.8) | 91 (24.4) | 234 (28.3) | 401 (25.4) | 234 (26.9) | 0.06 |
| Depression, GDS ≥ 6 | 11 (29.7) | 59 (28.9) | 49 (13.2) | 55 (6.6) | 68 (4.3) | 26 (3) | <0.01 |
| Number of medical conditions | 2.9 (1.7) | 3.0 (1.9) | 2.6 (1.7) | 1.9 (1.4) | 1.8 (1.4) | 1.8 (1.4) | <0.01 |
Abbreviations: 3MS, modified mini-mental state examination; ADL, activities of daily living; BMI, body mass index; GDS, Geriatric Depression Scale; IADL, independent activities of daily living; PASE, Physical Activity Scale for the Elderly.
Men with the highest level of life-space (101–120 points) all made daily trips to places in their neighborhood, most made daily trips to places outside their neighborhood in their town, and almost half made daily trips to places outside their town (Table 2). With few exceptions, they made these trips without any type of assistance. Men with the lowest level of life-space (0–20), with one exception, made daily trips to rooms in their home outside their bedrooms, but most required personal assistance. No men in this category made daily trips any further than their yard or driveway, nor were they able to go to places beyond their yard or driveway without personal assistance. Only two men in this category ever traveled outside their town.
Table 2.
Life-Space Distribution in the U.S. Osteoporotic Fractures in Men (MrOS) study, 2007–2009.
| Score
|
Level
|
Frequency
|
Assistancea
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | <1/wk | 1–3/wk | 4–6/wk | Daily | None | Equip. | Personal | ||
| 0–20 | ||||||||||
| Rooms outside bedroom | 37 | 0 | 0 | 0 | 1 | 36 | 9 | 1 | 27 | |
| Outside home, in yard or driveway | 34 | 3 | 5 | 10 | 3 | 16 | 3 | 0 | 31 | |
| In neighborhood, other than yard or apt. | 24 | 13 | 17 | 7 | 0 | 0 | 0 | 0 | 24 | |
| Outside neighborhood, within town | 12 | 25 | 12 | 0 | 0 | 0 | 0 | 0 | 12 | |
| Outside town | 2 | 35 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | |
| 21–40 | ||||||||||
| Rooms outside bedroom | 204 | 0 | 0 | 0 | 4 | 200 | 70 | 6 | 128 | |
| Outside home, in yard or driveway | 204 | 0 | 3 | 25 | 32 | 144 | 32 | 4 | 168 | |
| In neighborhood, other than yard or apt. | 196 | 7 | 17 | 124 | 37 | 18 | 15 | 5 | 176 | |
| Outside neighborhood, within town | 187 | 16 | 35 | 126 | 21 | 5 | 8 | 6 | 173 | |
| Outside town | 107 | 96 | 64 | 43 | 0 | 0 | 1 | 3 | 103 | |
| 41–60 | ||||||||||
| Rooms outside bedroom | 373 | 0 | 0 | 0 | 1 | 372 | 302 | 5 | 66 | |
| Outside home, in yard or driveway | 373 | 0 | 0 | 14 | 43 | 316 | 260 | 7 | 106 | |
| In neighborhood, other than yard or apt. | 373 | 0 | 4 | 161 | 112 | 96 | 205 | 20 | 148 | |
| Outside neighborhood, within town | 367 | 6 | 46 | 210 | 72 | 39 | 171 | 36 | 160 | |
| Outside town | 216 | 157 | 87 | 95 | 26 | 8 | 38 | 24 | 154 | |
| 61–80 | ||||||||||
| Rooms outside bedroom | 828 | 0 | 0 | 0 | 3 | 825 | 827 | 0 | 0 | |
| Outside home, in yard or driveway | 828 | 0 | 0 | 10 | 34 | 784 | 825 | 0 | 3 | |
| In neighborhood, other than yard or apt. | 828 | 0 | 0 | 308 | 263 | 257 | 805 | 9 | 14 | |
| Outside neighborhood, within town | 828 | 0 | 10 | 552 | 176 | 90 | 787 | 21 | 20 | |
| Outside town | 630 | 198 | 291 | 328 | 5 | 5 | 578 | 32 | 20 | |
| 81–100 | ||||||||||
| Rooms outside bedroom | 1581 | 0 | 0 | 0 | 2 | 1579 | 1581 | 0 | 0 | |
| Outside home, in yard or driveway | 1581 | 0 | 0 | 0 | 19 | 1562 | 1581 | 0 | 0 | |
| In neighborhood, other than yard or apt. | 1581 | 0 | 0 | 0 | 351 | 1230 | 1580 | 1 | 0 | |
| Outside neighborhood, within town | 1581 | 0 | 0 | 158 | 672 | 751 | 1571 | 8 | 2 | |
| Outside town | 1581 | 0 | 244 | 1171 | 162 | 4 | 1562 | 14 | 5 | |
| 101–120 | ||||||||||
| Rooms outside bedroom | 869 | 0 | 0 | 0 | 0 | 869 | 869 | 0 | 0 | |
| Outside home, in yard or driveway | 869 | 0 | 0 | 0 | 0 | 869 | 869 | 0 | 0 | |
| In neighborhood, other than yard or apt. | 869 | 0 | 0 | 0 | 0 | 869 | 869 | 0 | 0 | |
| Outside neighborhood, within town | 869 | 0 | 0 | 0 | 156 | 713 | 868 | 1 | 0 | |
| Outside town | 869 | 0 | 0 | 0 | 466 | 403 | 867 | 2 | 0 | |
Equip., equipment.
Assistance was assessed as “none”, “equipment only”, or “personal assistance from another person.”
Assistance of any type was rare among men with life-space scores above 80 (Table 2). Most men with moderate life-space scores (61–80) also did not require assistance at any level of life-space; when assistance was required, equipment was as common as personal assistance. In contrast, assistance was commonly required at all levels of life-space among men with lower life-space scores (0–60), and personal assistance was more common than equipment only.
Over a mean 2.7 years (SD, 0.6 yrs; range 0 days to 3.7 yrs) of follow-up, 373 (9.6%) men died (unadjusted rate 35.8 deaths/1000 person years, 95% CI: 32.2, 39.5). Of these, 115 (30.8%) were classified as cardiovascular deaths, 100 (26.8%) as cancer deaths, and 115 (30.8%) as other (non-cardiovascular, non-cancer); 43 (11.5%) deaths were unclassified and therefore excluded from cause-specific mortality analyses. Among cardiovascular deaths, the most common sub-type was ischemic heart disease (N=50, ICD-9 codes 410–414). Among cancer deaths, the most common sub-type was lung cancer (N=26, ICD-9 codes 162). Among other deaths, the most common sub-type was COPD (N=18, ICD-9 codes 490–496).
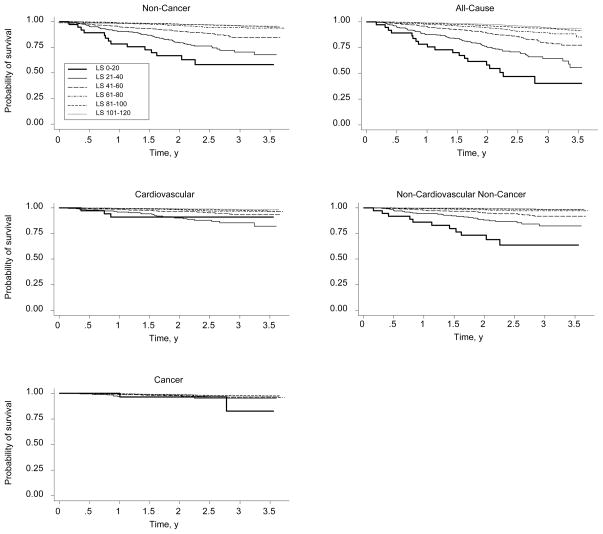
Unadjusted Kaplan-Meier curves for each mortality endpoint by category of life-space are shown in Figure 1. Lower levels of life-space were strongly associated with higher crude rates of non-cancer mortality, with a 17-fold difference in risk of non-cancer mortality between the lowest (41.2%) and highest (2.4%) levels of life-space (Table 3).
Figure 1.
Kaplan-Meier Survival Plots by Life-Space in the Osteoporotic Fractures in Men (MrOS) Study, 2007–2011.
Table 3.
Event Rates and Hazard Ratios for Mortality by Life-Space (LS) in the U.S. Osteoporotic Fractures in Men (MrOS) Study, 2007–2011.
| No. of persons | No. of deaths | Risk (%) | Events /1000 PY | Age-Adjusted
|
Age- and Gait Speed-Adjusted
|
Multivariable-Adjusteda
|
||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |||||
| Non-cancer mortality | ||||||||||
| Overall | 3849 | 230 | 6.0 | 22.3 | ||||||
| LS 0–20 | 34 | 14 | 41.2 | 225.4 | 12.94 | 6.36, 26.31 | 5.69 | 2.05, 15.76 | 3.82 | 1.27, 11.53 |
| LS 21–40 | 198 | 51 | 25.8 | 117.1 | 8.38 | 4.94, 14.23 | 4.12 | 2.26, 7.51 | 2.15 | 1.12, 4.11 |
| LS 41–60 | 363 | 43 | 11.8 | 47.1 | 3.77 | 2.21, 6.42 | 2.58 | 1.47, 4.51 | 1.70 | 0.93, 3.08 |
| LS 61–80 | 818 | 45 | 5.5 | 21.0 | 2.02 | 1.20, 3.39 | 1.66 | 0.98, 2.82 | 1.42 | 0.82, 2.46 |
| LS 81–100 | 1568 | 56 | 3.6 | 13.0 | 1.39 | 0.84, 2.30 | 1.29 | 0.78, 2.14 | 1.21 | 0.72, 2.05 |
| LS 101–120 | 868 | 21 | 2.4 | 8.7 | 1.00 | 1.00 | 1.00 | |||
| P for trend | <0.001 | <0.001 | 0.005 | |||||||
| Per SD decrease LS (24 pts) | 1.93 | 1.70, 2.18 | 1.49 | 1.28, 1.73 | 1.25 | 1.06, 1.47 | ||||
| Restricted independent LS | 471 | 102 | 21.7 | 93.9 | 4.47 | 3.36, 5.94 | 2.53 | 1.78, 3.61 | 1.54 | 1.03, 2.29 |
| Model N | 3849 | 3703 | 3658 | |||||||
| All-cause mortality | ||||||||||
| Overall | 3892 | 373 | 9.6 | 35.8 | ||||||
| LS 0–20 | 37 | 19 | 51.4 | 279.5 | 9.65 | 5.48, 17.00 | 5.07 | 2.29, 11.26 | 3.77 | 1.61, 8.83 |
| LS 21–40 | 204 | 65 | 31.9 | 144.1 | 5.69 | 3.81, 8.51 | 3.13 | 1.97, 4.99 | 1.79 | 1.08, 2.96 |
| LS 41–60 | 373 | 65 | 17.4 | 69.1 | 2.89 | 1.95, 4.30 | 2.17 | 1.43, 3.30 | 1.51 | 0.97, 2.35 |
| LS 61–80 | 828 | 81 | 9.8 | 37.2 | 1.80 | 1.24, 2.62 | 1.58 | 1.08, 2.32 | 1.36 | 0.92, 2.02 |
| LS 81–100 | 1581 | 100 | 6.3 | 23.0 | 1.22 | 0.85, 1.74 | 1.17 | 0.82, 1.69 | 1.12 | 0.77, 1.61 |
| LS 101–120 | 869 | 43 | 4.9 | 17.7 | 1.00 | 1.00 | 1.00 | |||
| P for trend | <0.001 | <0.001 | 0.002 | |||||||
| Per SD decrease LS (24 pts) | 1.71 | 1.55, 1.88 | 1.38 | 1.23, 1.55 | 1.19 | 1.05, 1.35 | ||||
| Restricted LS | 487 | 135 | 27.7 | 119.7 | 3.36 | 2.67, 4.23 | 2.05 | 1.54, 2.72 | 1.35 | 0.98, 1.85 |
| Model N | 3892 | 3743 | 3697 | |||||||
| Cardiovascular mortality | ||||||||||
| Overall | 3849 | 115 | 3.0 | 11.2 | ||||||
| LS 0–20 | 34 | 3 | 8.8 | 48.3 | 4.45 | 1.21, 16.37 | 3.86 | 0.82, 18.17 | 2.36 | 0.45, 12.43 |
| LS 21–40 | 198 | 24 | 12.1 | 55.1 | 6.47 | 3.13, 13.36 | 3.68 | 1.64, 8.24 | 1.88 | 0.79, 4.49 |
| LS 41–60 | 363 | 19 | 5.2 | 20.8 | 2.78 | 1.33, 5.83 | 1.90 | 0.87, 4.13 | 1.21 | 0.54, 2.73 |
| LS 61–80 | 818 | 24 | 2.9 | 11.2 | 1.84 | 0.92, 3.70 | 1.56 | 0.77, 3.16 | 1.26 | 0.61, 2.60 |
| LS 81–100 | 1568 | 33 | 2.1 | 7.7 | 1.42 | 0.73, 2.75 | 1.30 | 0.67, 2.54 | 1.16 | 0.59, 2.29 |
| LS 101–120 | 868 | 12 | 1.4 | 5.0 | 1.00 | 1.00 | 1.00 | |||
| P for trend | <0.001 | 0.001 | 0.164 | |||||||
| Per SD decrease LS (24 pts) | 1.63 | 1.37, 1.94 | 1.37 | 1.12, 1.68 | 1.16 | 0.93, 1.44 | ||||
| Restricted independent LS | 471 | 45 | 9.6 | 41.4 | 3.53 | 2.34, 5.32 | 2.31 | 1.41, 3.76 | 1.52 | 0.88, 2.62 |
| Model N | 3849 | 3703 | 3658 | |||||||
| Other (non-cardiovascular non-cancer mortality) | ||||||||||
| Overall | 3849 | 115 | 3.0 | 11.2 | ||||||
| LS 0–20 | 34 | 11 | 32.4 | 177.1 | 25.72 | 10.14, 65.24 | 8.26 | 2.08, 32.75 | 6.27 | 1.37, 28.70 |
| LS 21–40 | 198 | 27 | 13.6 | 62.0 | 11.01 | 5.04, 24.07 | 4.73 | 1.93, 11.62 | 2.62 | 0.98, 7.02 |
| LS 41–60 | 363 | 24 | 6.6 | 26.3 | 5.12 | 2.35, 11.18 | 3.53 | 1.56, 7.99 | 2.43 | 0.99, 5.96 |
| LS 61–80 | 818 | 21 | 2.6 | 9.8 | 2.24 | 1.02, 4.91 | 1.79 | 0.80, 3.99 | 1.66 | 0.71, 3.88 |
| LS 81–100 | 1568 | 23 | 1.5 | 5.3 | 1.34 | 0.62, 2.90 | 1.27 | 0.59, 2.75 | 1.24 | 0.54, 2.82 |
| LS 101–120 | 868 | 9 | 1.0 | 3.7 | 1.00 | 1.00 | 1.00 | |||
| P for trend | <0.001 | <0.001 | 0.008 | |||||||
| Per SD decrease LS (24 pts) | 2.28 | 1.91, 2.72 | 1.64 | 1.32, 2.04 | 1.38 | 1.09, 1.77 | ||||
| Restricted independent LS | 471 | 57 | 12.1 | 52.5 | 5.62 | 3.77, 8.38 | 2.81 | 1.67, 4.71 | 1.58 | 0.89, 2.83 |
| Model N | 3849 | 3703 | 3658 | |||||||
| Cancer mortality | ||||||||||
| Overall | 3849 | 100 | 2.6 | 9.7 | ||||||
| LS 0–20 | 34 | 2 | 5.9 | 32.2 | 2.80 | 0.63, 12.36 | 1.87 | 0.24, 14.68 | 2.00 | 0.23, 17.48 |
| LS 21–40 | 198 | 8 | 4.0 | 18.4 | 1.74 | 0.75, 4.03 | 0.85 | 0.29, 2.46 | 0.65 | 0.22, 1.99 |
| LS 41–60 | 363 | 12 | 3.3 | 13.1 | 1.29 | 0.62, 2.66 | 1.04 | 0.48, 2.26 | 0.84 | 0.37, 1.90 |
| LS 61–80 | 818 | 26 | 3.2 | 12.1 | 1.28 | 0.72, 2.29 | 1.19 | 0.66, 2.17 | 1.12 | 0.61, 2.06 |
| LS 81–100 | 1568 | 31 | 2.0 | 7.2 | 0.80 | 0.46, 1.39 | 0.81 | 0.46, 1.43 | 0.79 | 0.45, 1.40 |
| LS 101–120 | 868 | 21 | 2.4 | 8.7 | 1.00 | 1.00 | 1.00 | |||
| P for trend | 0.042 | 0.648 | 0.904 | |||||||
| Per SD decrease LS (24 pts) | 1.18 | 0.97, 1.44 | 1.02 | 0.81, 1.28 | 0.95 | 0.74, 1.21 | ||||
| Restricted independent LS | 471 | 17 | 3.6 | 15.7 | 1.43 | 0.83, 2.48 | 0.91 | 0.46, 1.77 | 0.68 | 0.33, 1.40 |
| Model N | 3849 | 3703 | 3658 | |||||||
CI, confidence interval; PY, person years
Adjusted for age, gait speed, physical activity, body mass index, Teng 3MS, married, self-rated health, high thyroid, COPD, coronary heart disease, congestive heart failure, hypertension, dementia/Alzheimer’s, non-skin non-melanoma cancer, ADL limitation.
In age-adjusted models, there was a strong linear relationship between decreasing life-space and increasing risk of non-cancer mortality (Ptrend<0.001) (Table 3). Men with the lowest level of life-space (0–20 points) had a 13-fold higher risk of non-cancer mortality than men with the highest life-space (101–120 points). Men with life-space scores from 21–80 also had substantially elevated risk of non-cancer mortality compared to men with the highest life-space. Each SD (24 point) decrease was associated with a 1.93-fold increase in risk of non-cancer mortality. Men with restricted independent life-space (confined to one’s neighborhood) had a 4.5-fold higher risk of non-cancer mortality than men without restricted life-space.
Results were attenuated but remained significant after adding gait speed and multivariable adjustment (Table 3). In multivariable models, the linear relationship between decreasing life-space and increasing mortality remained strong (Ptrend=0.005). Men with life-space scores ≤40 had an elevated risk of non-cancer mortality compared to men with the highest level of life-space, and risk of non-cancer mortality remained almost 4-fold higher among men with life-space scores ≤20 versus men with the highest life-space. Each SD decrease in life-space was associated with a 1.25-fold increase in risk of non-cancer mortality. Men with restricted independent life-space had a 1.54-fold higher risk of non-cancer mortality.
Associations between life-space and all-cause mortality were similar to those for non-cancer mortality (Table 3). Life-space was even more strongly associated with other mortality (non-cardiovascular non-cancer) than non-cancer mortality (Table 3). Results were weaker for cardiovascular mortality (Table 3). Life-space was not associated with cancer mortality (Table 3).
In sensitivity analyses, life-space was strongly associated with non-cancer, all-cause, cardiovascular, and other mortality in age-adjusted models among the population of “healthy” men (n=1982) free of a variety of medical conditions at baseline (data not shown). Adjusting for number of medical conditions as an index of chronic disease burden rather than adjusting for individual medical conditions did not alter the results (data not shown). Similarly, excluding 56 men who reported living in nursing homes or assisted living facilities did not alter the results (data not shown).
DISCUSSION
Life-space is a simple, novel, and integrated measure of mobility that captures the extent, frequency, and independence of an individual’s typical movement within their environment. In this prospective study of older men, unadjusted life-space scores discriminated risk for non-cancer, all-cause, and other (non-cardiovascular non-cancer) mortality from very low to extremely high risk. Furthermore, following adjustment for strong risk factors for these mortality endpoints, including age, self-rated health, chronic medical conditions, physical function including gait speed, and physical activity, life-space scores ≤40 were significantly associated with mortality, and a 24-point decrease in life-space was associated with a 19–38% increase in risk of mortality. Results were not altered after adjustment for chronic disease burden or the exclusion of men with baseline chronic medical conditions and those living in nursing homes or assisted living facilities. Thus, life-space provides unique information relevant to mortality over and above that provided by underlying illness among older men. Of note, men with life-space scores ≤40 exhibited characteristics of physical frailty including weakness, slowness, and low physical activity and often required personal assistance for mobility tasks inside and outside their homes. To this end, life-space may be a marker of physical frailty and the resources and supports available to compensate for it.
Why would life-space predict mortality? There are two possible interpretations. The first is that life-space directly influences mortality in older men, such that lesser amounts and independence of movement cause early mortality. For example, restrictions in life-space may lead to reductions in physical activity and fitness. Previous research has established that lower levels of fitness are associated with higher risk of mortality14 and improvements in fitness cause reductions in mortality.15 If life-space has a direct causal relationship with mortality, then alterations to life-space should impact mortality risk; future research is needed to test this hypothesis.
A competing interpretation is that life-space reflects underlying and unmeasured biological, and possibly social, factors that directly influence mortality; biological factors might include subclinical illness, the ability of skeletal muscle to generate ATP energy, the energy cost of mobility, and disturbances in organ systems. In this regard, life-space may be seen as an easily measured biomarker of aging that is useful in the early identification of individuals at elevated risk for functional decline and premature mortality. In support of this notion, shrinking life-space has been proposed as a behavioral adaptation to declining physiologic reserve and capacity.16 Moreover, involvement in a smaller life-space may reflect lower levels of social support and engagement, and cognitive and emotional functioning that impact mortality. Future research with longer follow-up will help to elucidate the pathways by which life-space is associated with mortality.
Our study adds to the growing list of prospective investigations of life-space. In previous studies, low levels of life-space have predicted increased risk of frailty,16 decline in cognitive function,17, 18 mild cognitive impairment,18 and Alzheimer’s Disease.18 More constricted life-space also predicted greater risk of all-cause mortality over 4 years of follow-up in older men and women without dementia 19 and greater risk of frailty-free mortality over 3 years of follow-up in disabled women.16 The current study extends our understanding of the relationship between life-space and mortality. We studied a large and relatively healthy community-dwelling population of older men, examined multiple mortality endpoints, adjusted for a large number of potential confounding factors, and used composite life-space scores, which are the most comprehensive description of an individual’s life-space. Previous studies16, 19 used modified versions of the life-space assessment that did not completely ascertain extent, frequency, and independence of movement, and they considered fewer confounders.19
We found that life-space provides unique information about risk of mortality over and above that provided by gait speed, which is widely recognized as the strongest physical performance predictor of mortality in older adults.13 This suggests that enacted mobility makes an important contribution to health and survival distinct from physical capacity, and highlights the importance of spatial contributions to health.
Mortality appears to be more strongly associated with life-space than other established risk factors, including chronic disease burden, gait speed, and self-rated health. We observed a 10-fold increase in crude risk of all-cause mortality between the lowest and highest categories of life-space. For comparison, the Cardiovascular Health Study found a 6.5-fold increase in crude risk of all-cause mortality between the lowest and highest levels of chronic disease burden by the Physiologic Index of Comorbidity 20, and the Health, Aging, and Body Composition Study observed a 3-fold increase in risk between the fastest and slowest quartiles of gait speed.3
The life-space questionnaire has strong potential to become a standard assessment tool in clinical practice and geriatric research. The questionnaire is simple, easy, and quick to administer, and our crude analyses showed it is able to identify older men with very low, moderate, and extremely high risk of mortality. In practice, such information can guide clinical decision making by helping to refine survival estimates in older adults. Patients with low risk of mortality may be considered for preventive interventions whose benefits take time to accrue, while patients with high risk of mortality may be candidates for intense risk factor modification. In research, life-space can be used to characterize the health status of study populations and as an endpoint in intervention research.
For translation and implementation in clinical settings, life-space assessment done by questionnaire may prove more feasible than gait speed testing. Although the life-space-mortality relationship appears linear across the range, future work to define appropriate cut-points for clinical intervention may allow more quantitative interpretation of life-space scores. The current results suggest that older men who are unable to go places outside their neighborhood without assistance (restricted independent life-space) have a relatively high probability of death (28%) over 2.7 years.
This study has certain strengths and limitations. It included a large population of well-characterized older men and centralized physician adjudication of cause of death. Men in this study were well enough to attend the third clinic visit of MrOS and were thus healthier than the general population. As this is the first report of associations between life-space and multiple mortality endpoints, replication studies in other cohorts are needed. Life-space was measured at one time point only, so we were unable to determine how changes in life-space are associated with mortality. We excluded cancer mortality from the primary outcome because cancer is not a degenerative disease and markers of longevity and aging typically have weak associations with cancer mortality 8; the results of our study confirmed that life-space was not associated with cancer mortality. While hospitalization is associated with mortality and life-space,21 we did not have data on hospitalizations prior to life-space assessment, so our results are susceptible to residual confounding. We acknowledge that there are likely to be many reasons for life-space restriction in older age, including frailty, lack of personal assistance, and limited transportation options; however, examination of these reasons was beyond the scope of the present study. We also acknowledge that a good clinician might be able to estimate survival probabilities from participant responses to less structured queries. Nevertheless, studies of clinical judgment are difficult to compare across patients or cohorts, and less amenable to research for prevention protocols. Finally, with a short mean follow-up of 2.7 years we cannot completely rule out the possibility that life-space is a risk marker for existing disease rather than a risk factor for future mortality.
In summary, life-space predicts non-cancer, all-cause, and other (non-cardiovascular non-cancer) mortality in older men. Life-space scores ≤ 40 are associated with these mortality endpoints independent of other strong risk factors. The simple life-space questionnaire could become a standard assessment tool in clinical practice and geriatric research.
Acknowledgments
Funding/Support
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140.
Sponsor’s Role
The funding agencies had no direct role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, approval, or submission of the manuscript.
Footnotes
Previous Presentation: An abstract of results was presented at the Bay Area Clinical Research Symposium in San Francisco, CA, November 4, 2011. Neither this manuscript nor one with substantially similar content has been published or is being considered for publication elsewhere.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
All authors read and approved the final manuscript. All persons who contributed significantly to this work are listed as authors.
Author Contributions
DCM had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
DCM contributed to study conception and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, and statistical analysis.
JAC contributed to acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and obtaining funding.
EBC contributed to acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and obtaining funding.
JTS contributed to analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and supervision.
PMC contributed to conception and design, acquisition of the data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and supervision.
SRC contributed to conception and design, acquisition of data, analysis and interpretation of the data, critical revision of the manuscript for important intellectual content, obtaining funding, and supervision.
References
- 1.Manini TM, Everhart JE, Patel KV, et al. Daily activity energy expenditure and mortality among older adults. JAMA. 2006;296:171–179. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- 2.Blair SN, Kampert JB, Kohl HW, 3rd, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276:205–210. [PubMed] [Google Scholar]
- 3.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 4.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51:1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 5.Peel C, Sawyer Baker P, Roth DL, et al. Assessing mobility in older adults: The UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85:1008–1119. [PubMed] [Google Scholar]
- 6.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS) Contemp Clin Trials. 2005;26:557–568. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Dumurgier J, Elbaz A, Ducimetiere P, et al. Slow walking speed and cardiovascular death in well functioning older adults: Prospective cohort study. BMJ. 2009;339:b4460. doi: 10.1136/bmj.b4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Almeida OP, Almeida SA. Short versions of the geriatric depression scale: A study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int J Geriatr Psychiatry. 1999;14:858–865. doi: 10.1002/(sici)1099-1166(199910)14:10<858::aid-gps35>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 10.Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): Development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 11.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Cawthon PM, Fink HA, Barrett-Connor E, et al. Alcohol use, physical performance, and functional limitations in older men. J Am Geriatr Soc. 2007;55:212–220. doi: 10.1111/j.1532-5415.2007.01062.x. [DOI] [PubMed] [Google Scholar]
- 13.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blair SN, Kohl HW, 3rd, Paffenbarger RS, et al. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262:2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 15.Blair SN, Kohl HW, 3rd, Barlow CE, et al. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273:1093–1098. [PubMed] [Google Scholar]
- 16.Xue QL, Fried LP, Glass TA, et al. Life-space constriction, development of frailty, and the competing risk of mortality: The Women’s Health And Aging Study I. Am J Epidemiol. 2008;167:240–248. doi: 10.1093/aje/kwm270. [DOI] [PubMed] [Google Scholar]
- 17.Crowe M, Andel R, Wadley VG, et al. Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. J Gerontol A Biol Sci Med Sci. 2008;63:1241–1245. doi: 10.1093/gerona/63.11.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.James BD, Boyle PA, Buchman AS, et al. Life Space and risk of Alzheimer disease, mild cognitive impairment, and cognitive decline in old age. Am J Geriatr Psychiatry. 2011;19:961–969. doi: 10.1097/JGP.0b013e318211c219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyle PA, Buchman AS, Barnes LL, et al. Association between life space and risk of mortality in advanced age. J Am Geriatr Soc. 2010;58:1925–1930. doi: 10.1111/j.1532-5415.2010.03058.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newman AB, Boudreau RM, Naydeck BL, et al. A physiologic index of comorbidity: relationship to mortality and disability. J Gerontol A Biol Sci Med Sci. 2008;63:603–609. doi: 10.1093/gerona/63.6.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown CJ, Roth DL, Allman RM, et al. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009;150:372–378. doi: 10.7326/0003-4819-150-6-200903170-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]