Abstract
The purpose of this study was to provide novel information regarding the concurrent validity (primary aim) and reliability (secondary aim) of walking speed (WS) calculated via the GAITRite1 electronic walkway system and 3 meter walk test (3MWT) in the chronic stroke population. The 3MWT is a feasible option for clinicians working in environments where space is limited. Psychometric properties of the test have not been established. Participants with chronic stroke were stratified into three groups: household ambulators (HA) (self-selected WS <0.4 m/s, 12 participants, 31 observations), limited community ambulators (LCA) (self-selected WS 0.4–0.8 m/s, 24 participants, 60 observations), and community ambulators (CA) (self-selected WS >0.8 m/s, 26 participants, 71 observations). Three consecutive trials of GAITRite1 and 3MWT were performed at participant’s self-selected WS. Average WS measurements differed significantly (p <0.05) between GAITRite1 and 3MWT for all three groups. HA group: GAITRite1 0.25 (0.11) m/s, 3MWT 0.27 (0.11) m/s; LCA group: GAITRite1 0.56 (0.11) m/s, 3MWT 0.52 (0.10) m/s; CA group: GAITRite1 1.03 (0.16) m/s, 3MWT 0.89 (0.15) m/s. Both WS measures had excellent within-session reliability (ICC’s ranging from 0.85 to 0.97, SEM95 from 0.04 to 0.12 m/s, and MDC95 from 0.05 to 0.16 m/s). Reliability was highest for HA on both measures. Although both the 3MWT and the GAITRite1 are reliable measures of WS for individuals with chronic stroke, the two measures do not demonstrate concurrent validity.
Keywords: Stroke, Gait, Walking speed, Outcome measurement, Rehabilitation
INTRODUCTION
Walking speed (WS) is emerging as a convenient, cost effective, reliable measure (Flansbjer, Holmback, Downham, Patten, & Lexell, 2005; Green, Forster, & Young, 2002) of functional status and predictor of future adverse events. Occasionally referred to as the sixth vital sign, WS provides therapists with valuable information and is used to assess and monitor a wide-range of diagnoses, including stroke (Fritz & Lusardi, 2009; Hardy, Perera, Roumani, Chandler, & Studenski, 2007; Purser et al., 2005; Rabadi & Blau, 2005). Researchers have found WS to be a predictor of discharge location (Fritz & Lusardi, 2009; Rabadi & Blau, 2005), functional dependence (Shinkai et al., 2000), presence of subclinical cardiovascular disease (Hamer et al.), future adverse events such as falls or hospitalization (Abellan van Kan et al., 2009; Montero-Odasso et al., 2005), and mortality (Hardy et al., 2007; Studenski et al., 2011). Reference charts providing cutoff values that can be used to stratify patients into risk categories (Fritz & Lusardi, 2009), as well as predict a patient’s functional ambulatory status (Perry, Garrett, Gronley, & Mulroy, 1995), are available in the literature.
In the clinical setting WS data for a patient is often collected using the most appropriate method for that environment. The results are then compared to a chart of normative values and used to determine current functional status and to predict likelihood of future adverse events. The values being compared may or may not have been collected using similar techniques. For example, a clinician may be comparing an individual’s walking speed determined by the GAITRite1 electronic walkway system to a reference chart classifying functional status by walking speeds gathered via the 10 meter walk test, such as the one provided in the Fritz and Lusardi paper (Fritz & Lusardi, 2009). In order for accurate conclusions to be drawn by a clinician, it is important to determine if WS data collected via differing methods can be used interchangeably. The first step in this process is to determine the concurrent validity of the various methods for measuring walking speed. The 3 meter walk test (3MWT) may be an appropriate method for assessing a patient’s walking speed, especially for clinicians working in environments where space is limited. Although the test demonstrates clinical feasibility, the psychometric properties of the measure have not been determined. This paper adds to the body of knowledge concerning walking speed as an outcome measure by reporting information regarding the validity and reliability of the 3MWT in the chronic stroke population.
The purpose of this study was to use same subject/same day data to determine the concurrent validity of WSs calculated via the GAITRite1 electronic walkway and the 3MWT in the chronic stroke population. The results of this study will provide preliminary information on the comparability of WS data collected via different measures in this population. A second aim was to determine the reliability of WS measurements as assessed using the GAITRite1 system and the 3MWT in individuals with chronic stroke.
METHODS
Participants
Sixty two participants with chronic unilateral stroke were continuously enrolled from two parent training studies at the University of South Carolina. This study was approved by the University of South Carolina’s Institutional Review Board. Prior to participation, all participants reviewed and signed an informed consent. Inclusion criteria included ≥18 years of age, >6 months post-stroke, the ability to reliably follow three-step instructions, and the ability to walk 20 feet with or without an assistive device. Participants were excluded if they had severe weight-bearing pain (rated >5/10 on the visual analog pain scale), severe visual impairment, other neurological conditions, and/or severe arthritis or orthopedic problems that limited ambulation ability. Multiple testing sessions occurred throughout each study (e.g., baseline, pre-intervention, post-intervention, follow-up assessments), and WS was one of several measures collected at each testing session.
Measures
The GAITRite1 system is a common objective measure of gait consisting of a portable electronic walkway approximately 5.3 meters long embedded with pressure-activated sensors that detect a series of footfalls as an individual walks across the length of the mat. The active area of the mat is 4.42 meters long and 66 cm wide, with sensors placed 1.27 cm apart. Data is sampled from the walkway at a frequency of 80 Hz. Instrumental software then calculates a wide range of temporal and spatial gait parameters, including WS, cadence, and step length. The GAITRite1 system has demonstrated high levels of concurrent validity when compared to a three-dimensional motion analysis system (Webster, Wittwer, & Feller, 2005), a Clinical Stride Analyzer consisting of footswitches placed inside subjects’ shoes (Bilney, Morris, & Webster, 2003), and a standard video camera (McDonough, Batavia, Chen, Kwon, & Ziai, 2001). Test-retest reliability has been investigated over several intervals of time, from same day measurements (McDonough et al., 2001) to measurements obtained over a 2-week period (Menz, Latt, Tiedemann, Mun San Kwan, & Lord, 2004), with repeat measurements demonstrating high reliability. For the 3MWT, WS was measured over the middle 3 meters of a seven-meter walk using a stopwatch.
Procedure
Each participant completed three consecutive trials for each walking test at his/her self-selected WS; the first trial was for practice and trials 2 and 3 were recorded for reliability. For both the GAITRite1 and 3MWT, participants were allowed approximately 2 meters for acceleration/deceleration outside the data collection area to help reduce gait variability introduced during these phases (Graham, Ostir, Fisher, & Ottenbacher, 2008; Lindemann et al., 2008). For the 3MWT, lines were placed on the floor marking the starting and stopping points for participants, as well as outlining the 3 meter timed walking area. The examiner started a stopwatch as soon as the participant’s leg crossed the first 3 meter marker and stopped the stopwatch when the participant’s first leg crossed the second marker. Both assessors that collected data were trained in this standardized approach. All trials for both the GAITRite1 and 3MWT were performed in the foot wear typically worn by the individual in the community. Participants were provided rest as needed throughout the testing sessions in order to minimize effects of fatigue.
Data Analysis
The sample consisted of 62 individuals with chronic stroke. Participants were stratified into 3 functional groups per the WS categories developed by Perry and colleagues (Perry et al., 1995), household ambulators (HA) (<0.4 m/s), limited community ambulators (LCA) (0.4–0.8 m/s), and community ambulators (CA) (>0.8 m/s). These cut points have been validated in individuals with chronic stroke (Bowden, Balasubramanian, Behrman, & Kautz, 2008) and have been used to stratify participants with stroke in large randomized controlled trials (Duncan et al., 2011). Transition from one category to another appears to be clinically meaningful in terms of function and quality of life (Schmid et al., 2007). Classification was based on WS derived from the average of the participant’s second and third GAITRite1 trials for each testing session. GAITRite1 data, rather than 3MWT data, was used for classification due to the instrument’s documented validity (Webster et al., 2005) and reliability (Ng & Hui-Chan, 2005); psychometric properties of the 3MWT have not been reported in the literature, and this was the purpose of the current study. Demographic information stratified by the three WS categories is presented in Table 1. Both parent studies included four testing sessions over time, making available a total of 162 WS observations for analysis (31 HA, 60 LCA, 71 CA). A WS observation was defined as complete data for trials 2 and 3 for both the GAITRite1 and 3MWT. WS observations were excluded if AD and/or orthotic use was not similar within and between measures. In addition, two observations from the limited community ambulator group and one from the community ambulator group were removed due to recording or analyzing problems with the GAITRite1 software.
Table 1.
Baseline Characteristics of Study Participants by Walking Speed Category
| Household Ambulators (WS<0.4 m/s) (n=12) | Limited Community Ambulators (WS 0.4–0.8 m/s) (n=24) | Community Ambulators (WS>0.8 m/s) (n=26) | p-value | |
|---|---|---|---|---|
| Age (years) | 59.6 | 64.5 | 62.6 | 0.55 |
| SD | 11.4 | 10.3 | 14.9 | |
| Time since stroke (months) | 30 | 42 | 26.7 | 0.18 |
| SD | 29.7 | 35.8 | 21.4 | |
| Side of Hemiparesis | ||||
| Right (%) | 8 (67) | 15 (62.5) | 16 (62) | |
| Left (%) | 4 (33) | 9 (37.5) | 10 (38) | |
| Sex | ||||
| Males (%) | 8 (67) | 20(83) | 15 (58) | |
| Females (%) | 4 (33) | 4 (17) | 11 (42) | |
| Assistive Device | ||||
| RW (%) | 3 (25) | 2 (8) | 0 | |
| QC (%) | 2 (17) | 2 (8) | 0 | |
| SPC (%) | 0 | 4 (17) | 1 (4) | |
| Orthotic | ||||
| AFO (%) | 2 (17) | 3 (13) | 1 (4) | |
| WS Observations | 31 | 60 | 71 |
Abbreviations: WS, walking speed; SD, standard deviation; RW, rolling walker; QC, quad cane; SPC, single point cane; AFO, ankle-foot orthosis.
Data for each walking measure and trial was assessed for normality using the Kolmogorov-Smirnov test. Intraclass correlation coefficients (ICC2, 1) and the Bland-Altman method (Bland & Altman, 1986) (95% limits of agreement) were used to examine the level of agreement between average WS measurements (across trial 2 and 3) obtained with the GAITRite1 system and the 3MWT. The Bland-Altman method allows one to visually assess the agreement between two measurement methods by plotting the difference in measurements against the mean of the two measurements (Bland & Altman, 1986, 1999). The resulting plot shows the size and range of the measurement differences and their distribution around the mean. The 95% limits of agreement (mean difference ± 1.96*SD of the differences between measurements) provide an indication of how far apart measurements by the two methods are likely to be for most individuals (Bland & Altman, 1995). A smaller range between these two limits indicates a better level of agreement. In addition, two-tailed paired t-tests were performed to test for systematic differences in WS between the two measurement methods for each of the three groups, with level of significance set at p<0.05. Statistical analyses were conducted using SPSS version 17.02.
The within-session reliability of walking speed measurements across walking trials 2 and 3 for the GAITRite1 system and the 3MWT was examined using intraclass correlation coefficients (ICC3,1). To interpret ICC values, we used benchmarks suggested by Shrout and Fleiss (Shrout & Fleiss, 1979): >0.75 excellent reliability, 0.40–0.75 fair to good reliability, and <0.40 poor reliability. Additionally, to quantify the amount of change in WS that must be observed to be considered to exceed measurement error and variability, the minimal detectable change (MDC) was calculated at the 95% confidence level using the following formula: MDC95 = SEM95*√2. The standard error of measurement (SEM95) was determined using the formula 1.96*[SD x √(1−r)], where r is the test-retest reliability coefficient (in this case, ICC3,1) and SD is the standard deviation of walking trial 2 (Beaton, 2000; Haley & Fragala-Pinkham, 2006).
RESULTS
Comparison Between the GAITRite1 System and 3 Meter Walk Test
Average WS measurements differed significantly (p<0.05) between GAITRite1 and 3 meter walk assessments for all three WS categories. The difference was greatest for community ambulators, with the GAITRite1 system obtaining faster WS values [mean 1.03 m/s; SD 0.16 m/s] compared to those calculated from the 3MWT [mean 0.89 m/s; SD 0.15 m/s]. For limited community ambulators, the GAITRite1 system also recorded faster WS values [mean 0.56 m/s; SD 0.11 m/s] compared to the 3MWT [mean 0.52 m/s; SD 0.10 m/s]. In contrast, WS values were faster for household ambulators during the 3MWT [mean 0.27 m/s; SD 0.11 m/s] than during ambulation across the GAITRite1 walkway [mean 0.25 m/s; SD 0.11 m/s].
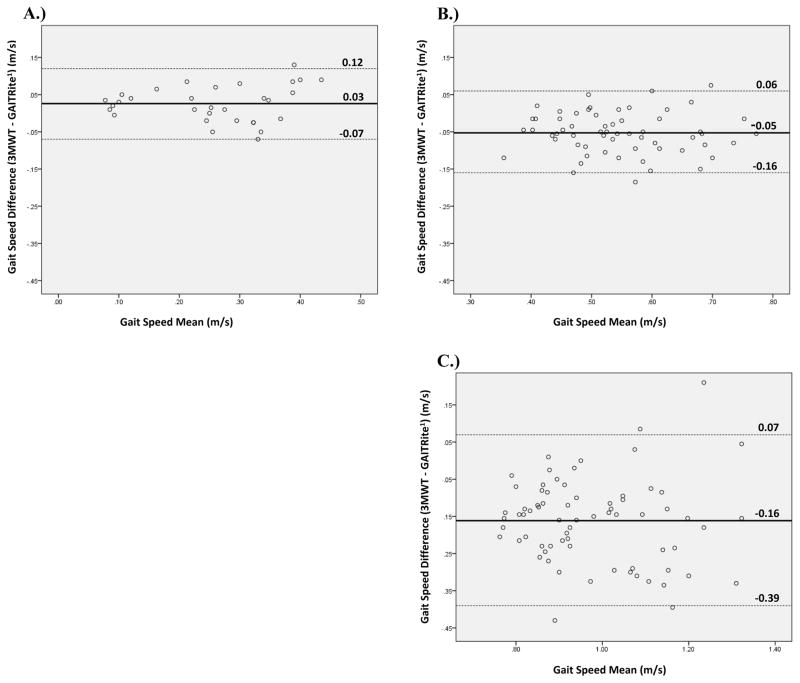
The ICC for average WS measurements between the GAITRite1 system and 3MWT was 0.89 (95% CI: 0.72–0.95) for household ambulators, 0.75 (95% CI: 0.22–0.90) for limited community ambulators, and 0.49 (95% CI: −0.09–0.78) for community ambulators. The Bland-Altman plots in Figure 1 show the differences in WS between the two methods for each WS category. The plots indicate larger between-method differences in WS measurements for community ambulators as demonstrated by a greater mean difference in WS, a larger range between the 95% limits of agreement, and a higher number of observations falling outside of this range compared to limited community or household ambulators. Household ambulators demonstrated the smallest between-method differences in WS, the smallest range between the 95% limits of agreement, and the least number of observations falling outside this range.
Figure 1.
Bland-Altman plots of the difference between GAITRite1 and 3MWT gait speed measurements against their mean for: (A) household ambulators (walking speed <0.4 m/s), (B) limited community ambulators (walking speed 0.4–0.8 m/s), and (C) community ambulators (walking speed >0.8 m/s). The solid line marks the mean difference in walking speed between the two methods, with the dashed lines representing the upper and lower 95% limits of agreement.
Test-Retest Reliability
Both GAITRite1 and 3MWT measurements were shown to have excellent within-session reliability, with ICC’s ranging from 0.85 to 0.97 (Table 2). Reliability between WS measurements was highest in household ambulators compared to limited community and community ambulators, indicating less variability in WS measurements at slower WSs.
Table 2.
Within-Session Reliability of Walking Speed Measurements Across Consecutive Walking Trials.
| GAITRite1 (m/s)
|
3 Meter Walk Test (m/s)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Trial 2 (SD) | Trial 3 (SD) | ICC (95% CI) | SEM95 | MDC95 | Trial 2 (SD) | Trial 3 (SD) | ICC (95% CI) | SEM95 | MDC95 | |
| HA (<0.4 m/s) | 0.25 (0.11) | 0.24 (0.11) | 0.97 (0.93–0.98) | 0.04 | 0.05 | 0.27 (0.11) | 0.27 (0.12) | 0.97 (0.94–0.99) | 0.04 | 0.05 |
| LCA (0.4–0.8 m/s) | 0.56 (0.11) | 0.58 (0.11) | 0.89 (0.82–0.93) | 0.07 | 0.1 | 0.52 (0.10) | 0.52 (0.11) | 0.91 (0.85–0.94) | 0.06 | 0.08 |
| CA (>0.8 m/s) | 1.03 (0.16) | 1.09 (0.16) | 0.93 (0.88–0.95) | 0.09 | 0.12 | 0.89 (0.15) | 0.91 (0.17) | 0.85 (0.77–0.90) | 0.12 | 0.16 |
Abbreviations: HA, household ambulators; LCA, limited community ambulators; CA, community ambulators; SD, standard deviation; ICC, intraclass correlation coefficient; CI, confidence interval; SEM95, standard error of measurement at 95% confidence level; MDC95, minimal detectable change at 95% confidence level.
*WS values are expressed as mean (SD).
*SEM and MDC values are in m/s.
DISCUSSION
In order to evaluate walking performance after stroke and over time, we need outcome measures with sound psychometric properties. The psychometric properties of the 3MWT, a clinically feasible option, have not been established. The primary objective of this study was to establish the concurrent validity of WSs calculated via the GAITRite1 system and the 3MWT in the chronic stroke population. When comparing the two measurement methods, WS measurements obtained from the GAITRite1 system and 3MWT were statistically different across all three WS groups. A greater degree of agreement, however, was observed in individuals considered household ambulators (ICC 0.89) when compared to the other groups. Only a fair degree of agreement was found between the two methods for limited community (ICC 0.75) and community ambulators (ICC 0.49). One possible explanation for the greater variability observed at faster WSs is that individuals tend to take larger steps at faster WSs, affecting the number of footfalls collected by the GAITRite1 system for WS analyses.
Limited community (80%) and community (93%) ambulators demonstrated consistently faster speeds when measured by the GAITRite1 system versus the 3MWT; this pattern, however, was not observed in household ambulators. A study by Stokic and colleagues (Stokic, Horn, Ramshur, & Chow, 2009) found similar results. A possible explanation for the higher WSs observed in limited community and community ambulators on the GAITRite1 is the distance ambulated. The active portion of the GAITRite1 mat is 4.42 meters, which is longer than the distance covered during the 3MWT. Perhaps the observed differences in WS are a result of the participants accelerating over a longer distance and therefore achieving a faster peak speed. However, as mentioned previously, the opposite was observed in our household ambulator group; these individuals, on average, walked slower on the GAITRite1 than during the 3MWT. A possible explanation for the slower speeds observed on the GAITRite1 compared to the 3MWT in the household ambulator group may be that individuals perceived ambulation across the mat as a change in terrain. For those with greater mobility restrictions, the perimeter height of the mat, though small, may have been viewed as a potential tripping hazard. The external sensors along one side of the mat may also have been perceived as tripping hazards. Therefore, these individuals may have been more cautious during ambulation across the mat, resulting in decreased WS.
While the ICC quantifies the reliability of two methods, it alone is insufficient to evaluate patterns of discrepancy that may be present among differences in the data. The Bland-Altman plots (Figure 1) show that for household and limited community ambulators, while the mean difference in WS between the GAITRite1 system and 3MWT for both groups was small, the range between the two calculated limits of agreement was large (0.03±0.1 and −0.05 ±0.11 m/s respectively) and exceeded the MDCs for WS. For community ambulators, the Bland-Altman plot reveals even larger mean differences in WS between the two methods and larger limits of agreement (−0.16±0.23 m/s). Overall, the lack of agreement between measures indicates that the GAITRite1 system and 3MWT do not demonstrate concurrent validity, and therefore walking speeds calculated via these methods should not be used interchangeably.
A second aim of our study was to examine the reliability of WS measurements obtained using the GAITRite1 system and 3MWT in this patient population. Reliability is a fundamental requirement for any WS measure to ensure that observed differences in WS values between testing sessions reflect real change in walking ability, rather than systematic or random measurement error. Our results indicate that when assessments are performed consecutively within the same testing session, both the GAITRite1 system and the 3MWT provide highly reliable measurements of WS, with similar SEMs, for individuals with chronic stroke.
The SEM indicates the amount of error expected to be observed with repeated measurements. For example, if an individual’s WS calculated via the 3MWT is 0.5 m/s with a corresponding SEM95 of 0.01 m/s, we can be 95% confident that their true speed was between 0.48 m/s and 0.52 m/s [0.5 ± (1.96*SEM)]. Our WS measurements were collected within the same session, rather than using sessions that were days or even weeks apart; therefore, the SEM values calculated in this study should be a fairly accurate reflection of the “true” variability of measurement error associated with these tests, as there was no window for natural changes to occur within the participants. Having an accurate SEM for methods of calculating WS in individuals with chronic stroke will allow clinicians and researchers to determine the range into which a patient or subject’s true speed falls.
While the SEM provides useful information on a patient’s true speed, it is a reflection of measurement error only and does not take into account the natural variability that can also occur with repeated measurements. For this, the MDC is needed. Researchers have reported MDC values for WS in individuals with stroke ranging from 0.07 m/s to 0.36 m/s (Flansbjer et al., 2005; Fulk & Echternach, 2008; Goldie, Matyas, & Evans, 1996; Hill, Goldie, Baker, & Greenwood, 1994) depending on time since stroke, level of assistance with ambulation, and measurement methods used. The results of our study indicate that for individuals with chronic stroke who are household ambulators (with similar characteristics as those who participated in this study) a change in WS of ≥0.05 m/s is necessary for both GAITRite1 and 3MWT in order to be 95% confident that a true change has occurred. For limited community ambulators, a change in WS of ≥0.1 or ≥0.08 m/s is necessary for GAITRite1 and 3MWT assessments, respectively. The largest WS change is required for community ambulators on both the GAITRite1 (0.12 m/s) and the 3MWT (0.16 m/s) in order to be 95% certain a true change has occurred. One possible explanation for the greater variability in WS and larger MDC95 values seen in community ambulators is that there is more capacity for change in WS in individuals who are not as limited in their mobility compared to those who are more limited in their ambulation ability. This is consistent with a study by Fulk and Echternach (Fulk & Echternach, 2008) who found greater variability in WS assessments in individuals with stroke who could walk without assistance compared to those that required physical assistance or use of an assistive device (AD).
Overall, these results show that the variation between the two measurement methods is large enough to potentially mask true changes in WS over time if both methods are used. While the reliability of both walking tests is excellent, the 3MWT does not exhibit a high enough degree of concurrent validity with the GAITRite1 for these two measures to be used interchangeably for WS assessments in individuals with chronic stroke. Therefore, when performing repeat WS measurements over time, the same method should be used for all assessments.
Study Limitations
There are several limitations of this study that need to be discussed. First, different evaluators were used for the two parent studies in which WS assessments were collected, which could impact the reliability of measurements and decrease internal validity; however, this does improve external validity. Additionally, this study only examined the reliability of WS measures taken consecutively within the same testing session, limiting external validity. Reliability analyses among WS measures taken over a longer time interval (e.g. days, weeks) may result in different ICC and MDC values than the current study. Furthermore, while the inclusion of individuals who use an assistive device and/or orthotic to walk may improve external validity of our results, more research needs to be performed to examine how the use of such devices affects the reliability of WS measures obtained from the GAITRite1 system.
CONCLUSIONS
Although the 3MWT is a clinically feasible option for assessing WS in individuals with chronic stroke, evidence regarding its psychometric properties is lacking. This study has shown that the GAITRite1 system and the 3MWT produce highly reliable measurements of WS in individuals with chronic stroke when measured consecutively within the same testing session. There is a lack of concurrent validity, however, between the two WS tests to permit them to be used interchangeably in this population. Since WS is gaining popularity in the clinical setting as a convenient, cost effective method to assess and monitor a wide range of diagnoses, population-specific concurrent validity of the various walking speed measures should be determined. This will provide clinicians with the information necessary for selecting appropriate measurement methods and for accurately interpreting WSs calculated via these measures. When comparing a patient’s WS to either their previous assessment or to a reference chart, clinicians should exercise caution if different measures were used and the concurrent validity of these measures has not been established.
Acknowledgments
Funding Sources: American Heart Association (Scientist Development Grant) and Robert Wood Johnson Foundation (Health Games Research Grant). We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated and that all financial and material support for this research and work are clearly identified. The manuscript submitted does not contain information about medical device(s).
Footnotes
CIR Systems Inc, 376 Lafayette Ave, Suite 202, Sparta, NJ 07871.
IBM Corporation, 1 New Orchard Road, Armonk, New York 10504-1722.
DECLARATION OF INTEREST
The authors report no declarations of interest.
Study Location: Department of Exercise Science, Physical Therapy Program, University of South Carolina, Columbia, South Carolina
No parts of this manuscript have been previously presented.
References
- Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13(10):881–889. doi: 10.1007/s12603-009-0246-z. [DOI] [PubMed] [Google Scholar]
- Beaton DE. Understanding the relevance of measured change through studies of responsiveness. Spine (Phila Pa 1976) 2000;25(24):3192–3199. doi: 10.1097/00007632-200012150-00015. [DOI] [PubMed] [Google Scholar]
- Bilney B, Morris M, Webster K. Concurrent related validity of the GAITRite walkway system for quantification of the spatial and temporal parameters of gait. Gait Posture. 2003;17(1):68–74. doi: 10.1016/s0966-6362(02)00053-x. [DOI] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346(8982):1085–1087. doi: 10.1016/s0140-6736(95)91748-9. [DOI] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- Bowden MG, Balasubramanian CK, Behrman AL, Kautz SA. Validation of a speed-based classification system using quantitative measures of walking performance poststroke. Neurorehabil Neural Repair. 2008;22(6):672–675. doi: 10.1177/1545968308318837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Wu SS, Nadeau SE, et al. Body-weight-supported treadmill rehabilitation after stroke. N Engl J Med. 2011;364(21):2026–2036. doi: 10.1056/NEJMoa1010790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flansbjer UB, Holmback AM, Downham D, Patten C, Lexell J. Reliability of gait performance tests in men and women with hemiparesis after stroke. J Rehabil Med. 2005;37(2):75–82. doi: 10.1080/16501970410017215. [DOI] [PubMed] [Google Scholar]
- Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign”. J Geriatr Phys Ther. 2009;32(2):46–49. [PubMed] [Google Scholar]
- Fulk GD, Echternach JL. Test-retest reliability and minimal detectable change of gait speed in individuals undergoing rehabilitation after stroke. J Neurol Phys Ther. 2008;32(1):8–13. doi: 10.1097/NPT0b013e31816593c0. [DOI] [PubMed] [Google Scholar]
- Goldie PA, Matyas TA, Evans OM. Deficit and change in gait velocity during rehabilitation after stroke. Arch Phys Med Rehabil. 1996;77(10):1074–1082. doi: 10.1016/s0003-9993(96)90072-6. [DOI] [PubMed] [Google Scholar]
- Graham JE, Ostir GV, Fisher SR, Ottenbacher KJ. Assessing walking speed in clinical research: a systematic review. J Eval Clin Pract. 2008;14(4):552–562. doi: 10.1111/j.1365-2753.2007.00917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J, Forster A, Young J. Reliability of gait speed measured by a timed walking test in patients one year after stroke. Clin Rehabil. 2002;16(3):306–314. doi: 10.1191/0269215502cr495oa. [DOI] [PubMed] [Google Scholar]
- Haley SM, Fragala-Pinkham MA. Interpreting change scores of tests and measures used in physical therapy. Phys Ther. 2006;86(5):735–743. [PubMed] [Google Scholar]
- Hamer M, Kivimaki M, Lahiri A, Yerramasu A, Deanfield JE, Marmot MG, et al. Walking speed and subclinical atherosclerosis in healthy older adults: the Whitehall II study. Heart. 96(5):380–384. doi: 10.1136/hrt.2009.183350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc. 2007;55(11):1727–1734. doi: 10.1111/j.1532-5415.2007.01413.x. [DOI] [PubMed] [Google Scholar]
- Hill KD, Goldie PA, Baker PA, Greenwood KM. Retest reliability of the temporal and distance characteristics of hemiplegic gait using a footswitch system. Arch Phys Med Rehabil. 1994;75(5):577–583. [PubMed] [Google Scholar]
- Lindemann U, Najafi B, Zijlstra W, Hauer K, Muche R, Becker C, et al. Distance to achieve steady state walking speed in frail elderly persons. Gait Posture. 2008;27(1):91–96. doi: 10.1016/j.gaitpost.2007.02.005. [DOI] [PubMed] [Google Scholar]
- McDonough AL, Batavia M, Chen FC, Kwon S, Ziai J. The validity and reliability of the GAITRite system’s measurements: A preliminary evaluation. Arch Phys Med Rehabil. 2001;82(3):419–425. doi: 10.1053/apmr.2001.19778. [DOI] [PubMed] [Google Scholar]
- Menz HB, Latt MD, Tiedemann A, Mun San Kwan M, Lord SR. Reliability of the GAITRite walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture. 2004;20(1):20–25. doi: 10.1016/S0966-6362(03)00068-7. [DOI] [PubMed] [Google Scholar]
- Montero-Odasso M, Schapira M, Soriano ER, Varela M, Kaplan R, Camera LA, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60(10):1304–1309. doi: 10.1093/gerona/60.10.1304. [DOI] [PubMed] [Google Scholar]
- Ng SS, Hui-Chan CW. The timed up & go test: its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch Phys Med Rehabil. 2005;86(8):1641–1647. doi: 10.1016/j.apmr.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Perry J, Garrett M, Gronley JK, Mulroy SJ. Classification of walking handicap in the stroke population. Stroke. 1995;26(6):982–989. doi: 10.1161/01.str.26.6.982. [DOI] [PubMed] [Google Scholar]
- Purser JL, Weinberger M, Cohen HJ, Pieper CF, Morey MC, Li T, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005;42(4):535–546. doi: 10.1682/jrrd.2004.07.0087. [DOI] [PubMed] [Google Scholar]
- Rabadi MH, Blau A. Admission ambulation velocity predicts length of stay and discharge disposition following stroke in an acute rehabilitation hospital. Neurorehabil Neural Repair. 2005;19(1):20–26. doi: 10.1177/1545968304272762. [DOI] [PubMed] [Google Scholar]
- Schmid A, Duncan PW, Studenski S, Lai SM, Richards L, Perera S, et al. Improvements in speed-based gait classifications are meaningful. Stroke. 2007;38(7):2096–2100. doi: 10.1161/STROKEAHA.106.475921. [DOI] [PubMed] [Google Scholar]
- Shinkai S, Watanabe S, Kumagai S, Fujiwara Y, Amano H, Yoshida H, et al. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age Ageing. 2000;29(5):441–446. doi: 10.1093/ageing/29.5.441. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Stokic DS, Horn TS, Ramshur JM, Chow JW. Agreement between temporospatial gait parameters of an electronic walkway and a motion capture system in healthy and chronic stroke populations. Am J Phys Med Rehabil. 2009;88(6):437–444. doi: 10.1097/PHM.0b013e3181a5b1ec. [DOI] [PubMed] [Google Scholar]
- Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster KE, Wittwer JE, Feller JA. Validity of the GAITRite walkway system for the measurement of averaged and individual step parameters of gait. Gait Posture. 2005;22(4):317–321. doi: 10.1016/j.gaitpost.2004.10.005. [DOI] [PubMed] [Google Scholar]