Abstract
Background
It is not known whether various forms of emotion regulation are differentially related to cardiovascular disease risk.
Purpose
The purpose of this study is to assess whether antecedent and response-focused emotion regulation would have divergent associations with likelihood of developing cardiovascular disease.
Methods
Two emotion regulation strategies were examined: reappraisal (antecedent-focused) and suppression (response-focused). Cardiovascular disease risk was assessed with a validated Framingham algorithm that estimates the likelihood of developing CVD in 10 years. Associations were assessed among 373 adults via multiple linear regression. Pathways and gender-specific associations were also considered.
Results
One standard deviation increases in reappraisal and suppression were associated with 5.9 % lower and 10.0 % higher 10-year cardiovascular disease risk, respectively, in adjusted analyses.
Conclusions
Divergent associations of antecedent and response-focused emotion regulation with cardiovascular disease risk were observed. Effective emotion regulation may promote cardiovascular health.
Keywords: Emotion regulation, Suppression, Reappraisal, CVD
Introduction
Despite substantial recent declines in death rates from coronary heart disease and stroke, the burden of cardiovascular diseases in the USA remains significant [1]. The recent forecast from the American Heart Association predicts a mounting burden and markedly escalating costs of cardiovascular disease through 2030, including a tripling in annual costs from $273 billion currently to $818 billion in 2030 [2]. However, cardiovascular disease is often preventable as is cardiovascular risk. Increasing evidence suggests that psychological, behavioral, and biological factors interact to influence cardiovascular outcomes [3, 4]. Moreover, positive emotional and behavioral factors may promote cardiovascular health beyond simply marking the absence of risk [5, 6]. The capacity to regulate emotions is a critical component of healthy psychological functioning and may be one such modifiable factor that can also help to protect health and promote resilience. As emotion regulation is not a fixed trait and instead reflects the use of learned behaviors and psychological responses, identifying whether and how emotion regulation is associated with biologic risk for disease may inform novel avenues for intervention.
Emotion regulation is a higher order feature of emotional functioning that encompasses positive and negative emotions and involves the monitoring and management of emotional experience and response [7, 8]. Emotion regulation reflects a set of strategies learned through socialization and experience that are systematically employed over the life course [8]. According to Gross and John’s theoretical model for emotion regulation, strategies can be distinguished from one another according to when during an emotion generative process they are employed [7]. Antecedent-focused strategies are employed early on in the emotion generative process and refer to cognitive changes employed in response to a situation and take place before emotion responses are manifest. Response-focused emotion regulation occurs later in the emotion generative process and refers to the modulation of responses to emotion (e.g., experiential, behavioral, physiologic). Reappraisal, considered an antecedent-focused strategy, involves altering how to think about an emotion-eliciting situation in order to change its emotional impact prior to its occurrence. For example, reappraising a job interview as an opportunity to excel rather than as a stressful experience may help to minimize the potentially harmful effects of anxiety and to facilitate a more positive emotional experience. Suppression, considered a response-focused emotion regulation strategy, involves inhibiting the expression of emotion that has occurred in response to an emotion-eliciting event. For example, suppression may involve deliberately keeping a straight face despite feeling angry in a confrontational situation. Whether and when an emotion regulation strategy is adaptive or maladaptive is context dependent. For example, suppression may be appropriate in some situations, and reappraisal may not always be beneficial. However, emotion regulation theory and research suggest that regulating the emotion earlier in the emotion generative process may be more effective than doing so in the later response-focused stage of the process [9]. As such, while the suitability of any given strategy is context dependent, consistent reliance on response-focused (e.g., suppression) over antecedent-oriented (e.g., reappraisal) regulation may differentially impact biologic processes and cardiovascular disease risk [10].
Prior work has suggested that inhibitive and suppressive type regulatory strategies may carry health risks because suppression appears to require significant mental exertion [9, 11] and still leaves individuals with negative emotional states that are unchecked internally. These experiences may impose a tax on body systems (e.g., via dysregulated stress-related hormones). In contrast, because reappraisal is employed before an emotion occurs and involves changing cognitive appraisals about the situation, this strategy may help to prevent the occurrence or reduce the intensity of negative emotions [7–9], thereby avoiding activation of stress-related dysregulation. As a result, regulatory strategies like reappraisal may be health promoting [7, 11, 12]. Building on prior work in this area, we hypothesize that reappraisal may confer cardiovascular protection whereas suppression may increase cardiovascular risk.
Recent research suggests that emotion regulation is associated with cardiovascular disease risk [6, 10, 12, 13]. One prospective study of 1,122 males (mean age = 60.3 years) found a 20 % reduced risk of incident coronary heart disease associated with high levels of self-regulation (i.e., ability to manage impulses, feelings, and behaviors with emotion regulation being a central feature) over 13 years of follow-up [14]. While this study demonstrated the relation between higher order regulatory capacity and cardiovascular outcome, the specific forms of regulation as well as pathways linking regulation to coronary heart disease remain unknown. Similarly, in a cross-sectional study among 181 Finnish adults, aspects of emotion regulation were associated with metabolic syndrome, a cluster of cardiovascular disease risk conditions including hypertension, elevated lipid levels, central adiposity, and insulin resistance [15]. Specifically, use of regulatory strategies that reduced negative mood and made positive emotions more likely (i.e., mood repair and mood maintenance) were associated with reduced risk of metabolic syndrome at age 42 while emotional ambivalence (a specific form of emotion dysregulation) was associated with increased risk of metabolic syndrome. However, this study had limited covariate control, and it is unclear whether associations would be maintained independent of demographic, socioeconomic factors, and prior cardiovascular health. Similarly, a recent study by our group in the sample used for the present study found divergent associations for reappraisal and suppression with C-reactive protein [12], an inflammatory risk marker which when elevated is thought to indicate increased risk of cardiovascular disease [16–18]. We found that a one standard deviation increase in reappraisal was associated with 21 % lower odds of having C-reactive protein concentrations consistent with the CDC/American Heart Association’s cut-point for being at high risk of cardiovascular disease [18] whereas a one standard deviation increase in suppression was associated with 43 % higher odds of having such high-risk C-reactive protein concentrations. While this study suggests that there are divergent associations among these different emotion regulation strategies with cardiovascular disease risk, there is a debate as to whether C-reactive protein is causally related to cardiovascular disease [16, 19]. In another study by our group in this sample, we found divergent associations between behavioral measures of adaptive and maladaptive child emotional functioning and adulthood cardiovascular disease risk as measured by the Framingham algorithm [20]. However, as the child emotion measures do not assess emotion regulation and instead reflect outcomes of effectively regulated and dysregulated emotion, it not known whether regulation of emotion would also associate with cardiovascular disease risk.
Some work on emotional functioning and cardiovascular disease suggests that women may be more vulnerable to the deleterious effects of poor emotional functioning (a marker for dysregulated emotion) [21], while also being more influenced by the protective effects of positive emotional functioning (often considered a marker for effectively regulated emotion) [20]. Moreover, a recent review found higher comorbidity of depression and cardiovascular disease and stronger associations of depression and psychosocial stressors with cardiovascular disease for women than men [22]. While depression, psychosocial stress, and poor emotional functioning are not synonymous with emotion regulation and instead reflect constellations of chronically elevated maladaptive cognitions, behaviors, and emotions of which dysregulated emotion is one feature [23], this work may indirectly suggest that problems regulating emotion might have differential impacts on cardiovascular disease for men and women. While a growing body of work suggests that some emotion regulation strategies contribute to increased risk of cardiovascular disease while other strategies may protect cardiovascular health, whether associations of emotion regulation and cardiovascular disease risk would be similar for men and women has not yet been looked at carefully.
While emerging work in this area is highly suggestive of an association between emotion regulation and cardiovascular disease, many studies are hampered by lack of rigorous control for early life factors including childhood health and early life psychosocial factors. Emotion regulation is learned through socialization and experience over time, with childhood being an important period of development as temperament, biology, and social factors interact to build regulatory skills and strategies that are then used across the life course [8, 24–26]. Child health, socioeconomic position, and cognitive ability may influence the development of emotion regulation skills during childhood [27], while also contributing to adulthood cardiovascular disease risk [28–30]. As prior work in this area generally does not account for such early life factors, observed associations between emotion regulation and cardiovascular disease among adults could be spurious. Moreover, these studies have largely not examined the mechanisms linking emotion regulation with cardiovascular disease risk. Prior work has suggested that in addition to biologic risk markers like C-reactive protein [12], social and behavioral factors may help explain how emotion regulation may contribute to cardiovascular disease risk [6, 10, 13]. For example, individuals with better emotion regulatory capacity may engage in more health-protective behaviors to cope with emotion whereas individuals with poor emotion regulation may engage in less healthy behaviors to cope with negative emotions. Such potential pathway variables have not been examined.
In the current cross-sectional study, we build on the emerging evidence linking emotion regulation to cardiovascular disease risk and examine whether reappraisal (an antecedent-focused emotion regulation strategy) and suppression (a response-focused emotion regulation strategy) have divergent associations with the likelihood of developing cardiovascular disease over the next 10 years using the validated Framingham General Cardiovascular Risk algorithm [31]. Risk scores are derived based on a mix of biological measures (e.g., lipid levels), presence of specific health conditions (e.g., diabetes), and behaviors (e.g., cigarette smoking). We hypothesized that suppression would be associated with higher 10-year risk of developing cardiovascular disease whereas reappraisal would be associated with lower 10-year cardiovascular disease risk, and that associations would be more robust for women as compared to men. This work contributes to the existing literature in several important ways. To our knowledge, this is the first study to directly assess whether the use of specific emotion regulation strategies is associated with the likelihood of developing cardiovascular disease. Also, where past work has had limited control for early life potential confounding variables, we test study hypotheses while accounting for important early life factors including prospectively assessed childhood cardiovascular health and socioeconomic position and cognitive ability. Moreover, this is the first study to examine whether associations of emotion regulation and cardiovascular disease risk are patterned by gender. Additionally, as past work has not considered the pathways through which emotion regulation may affect cardiovascular disease risk, we examine a wide range of social, behavioral, and physiologic factors from adulthood (i.e., physical activity, alcohol consumption, diet, C-reactive protein) that may help explain emotion regulation and cardiovascular disease risk associations.
Methods
Sample
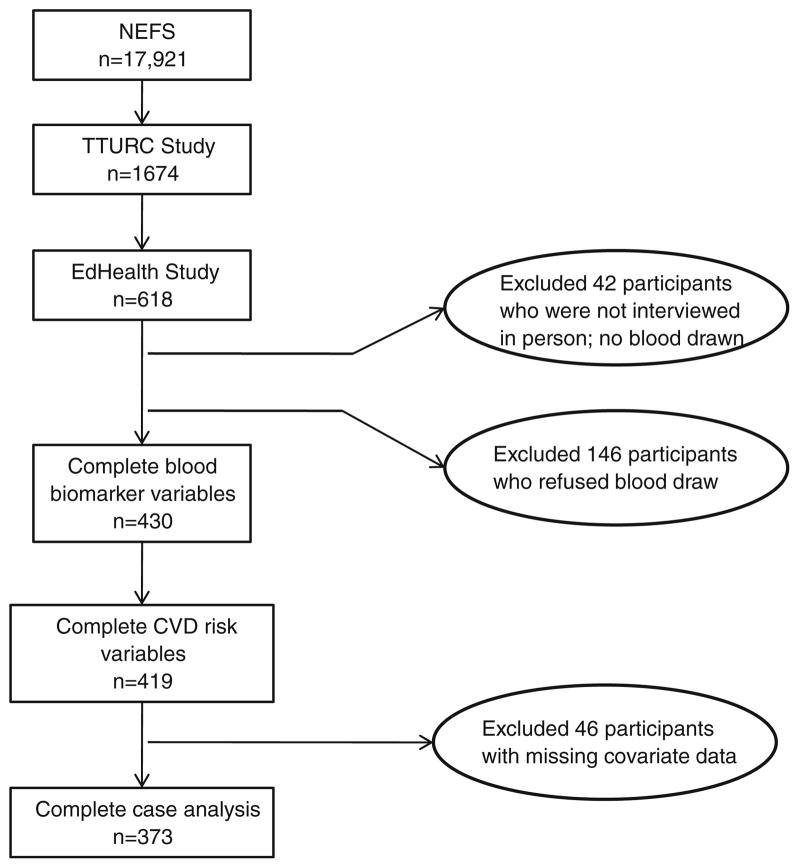
Figure 1 displays a flow chart describing how the study sample was selected. The sample comes from offspring of participants of the Collaborative Perinatal Project. Pregnant women enrolled between 1959–1966 [32, 33], and their offspring were regularly assessed from birth-7 years. The New England Family Study is a set of follow-up studies of the now adult offspring from the Boston and Providence sites. Details on the selection of the current sample is described elsewhere [34]. Briefly, our sample includes New England Family Study participants involved in two adult follow-up studies: first in the Brown-Harvard Transdisciplinary Tobacco Use Research Center (TTURC) and subsequently in the EdHealth study which included 618 TTURC participants, selected with preference for racial/ethnic minorities and those with low and high levels of education as required by the aims of the project. Of the 618 individuals interviewed (69 % response rate), 42 who were not interviewed in-person (and did not complete physiological assessments) were excluded, resulting in 576 eligible participants. Of these, 430 (75 %) participated in the clinical assessment, where a blood sample and anthropomorphic measurements were obtained by trained study personnel. Of these, 419 had data on algorithm components to calculate cardiovascular disease risk. A complete case analysis was then conducted among 373 individuals who also had complete data on all covariates. Across the 618 participants in the interview sample, there were no significant differences by gender, education, and reappraisal or suppression among those who were excluded (n = 245) and included in the study (n = 373) (all ps>0.05), although excluded participants were older by 0.78 years (t(615) = −5.3, p<0.001) and less likely to be white (χ2(1, n = 373) = 8.8, p<0.01). Human subjects committees at the Harvard School of Public Health and Brown University approved the study protocol. All participants provided informed consent.
Fig. 1.
Flow chart of included and excluded study participants. NEFS New England Family Study, TTURC Transdisciplinary Tobacco Use Research Center, CVD cardiovascular disease
Measures
Emotion Regulation
Emotion regulation involves the monitoring and management of emotional experience and response [7, 8]. In this study, we examined two emotion regulation strategies as measured by the Emotion Regulation Questionnaire [7, 8]. The Emotion Regulation Questionnaire assesses emotion reappraisal and suppression strategies with 10 items (six items for the reappraisal subscale, four items for the suppression subscale). Reappraisal involves altering how to think about an emotion-eliciting situation in order to change its emotional impact (e.g., “When I’m faced with a stressful situation, I make myself think about it in a way that keeps me calm.”). Suppression involves inhibiting emotional expression in response to an emotion eliciting event (e.g., “I control my emotions by not expressing them.”). Raw items were summed and subscale scores were standardized to have a mean of zero and standard deviation of one to improve interpretability of reappraisal and suppression scores. These regulation strategies are generally considered to be orthogonal and largely non-overlapping [7]. Reappraisal and suppression were examined as continuous measures. The Emotion Regulation Questionnaire has demonstrated divergent and convergent validity with coping strategies used in stressful situations, high internal consistency reliability, and has a test-retest reliability of 0.7 [7, 8]. Additional information on validation and psychometric properties have been reported elsewhere [7]. In this sample, internal consistency reliability was high for both reappraisal (α = 0.87) and suppression (α = 0.77).
10-Year Calculated Risk of Cardiovascular Disease
The 10-year risk of cardiovascular disease in adulthood was calculated using the Framingham General Cardiovascular Risk algorithm [31]. The algorithm has demonstrated good predictive validity in the Framingham Heart Study cohorts for cardiovascular disease events (c statistic = 0.76 for men, 0.79 for women) [31], which include coronary death, myocardial infarction, coronary insufficiency, angina, ischemic stroke, hemorrhagic stroke, transient ischemic attack, intermittent claudication, and heart failure. The algorithm uses gender-specific Cox proportional-hazard regression models that incorporate information on age, total cholesterol, HDL cholesterol, systolic blood pressure, antihypertensive medication use, smoking, and diabetes. Risk scores indicate the likelihood of developing cardiovascular disease in the next 10 years. Actual cardiovascular disease endpoints were not observed in this study.
Total and HDL cholesterol were measured in nonfasting plasma samples at CERLab (Harvard Medical School, Boston, MA) using a Hitachi 911 analyzer (Roche, Basel, Switzerland). Total cholesterol was measured enzymatically (CV = 1.7 %) [35]. HDL cholesterol was determined using a direct enzymatic colorimetric assay (CV = 3.3 %) [36]. Blood pressure was measured in seated, resting participants, using automated blood pressure monitors (VSMedTech BpTru, Coquitlam, BC, Canada) [37]. Systolic blood pressure was calculated as the mean of the lowest three readings of the five collected, excluding the first measure. Physician prescribed antihypertensive medication use, presence of physician-diagnosed diabetes, and current smoking were based on self-reports obtained during the clinical interview.
Covariates
A range of factors assessed during childhood and adulthood were included as covariates. Childhood factors including cardiovascular health, cognitive ability and socioeconomic status were included to determine whether emotion regulation was independently associated with cardiovascular disease risk; adulthood social and behavioral risk factors for cardiovascular disease were included to determine if they could partially explain the primary associations of interest. Covariates were selected based on theoretical and empirical considerations.
Demographic covariates included age, race (white/not white), education attainment (years), and original study location (Boston, Massachusetts; Providence, Rhode Island). Childhood factors included being born small for gestational age (birth weight was less than or equal to the tenth percentile for gestational age at delivery), child cognitive ability (IQ; assessed at age 7 with the Wechsler Intelligence Scale for Children [38]), presence of a childhood chronic health condition (child experienced one or more chronic physical health conditions from birth-7 years as identified by study pediatricians or maternal report), socioeconomic status (index adapted from the U.S. Census Bureau which reflects the education, occupation, and income of the head of household when the child was age 7 ranging from 0/low–100/high [39]) and childhood cardiovascular health indicators at age 7 (body mass index, blood pressure, diabetes). Child body mass index, blood pressure, and presence of diabetes mellitus were assessed at a scheduled study visit when the child was 7 years old. Body mass index was calculated as kg/m2 using height and weight obtained by study personnel. Systolic and diastolic blood pressure (mmHg) was measured by a study pediatrician using standard equipment for the time. Presence of childhood diabetes was diagnosed by a study pediatrician. However, as only one child was a suspected case and no children received a diagnosis of diabetes, we did not include this variable in analysis.
Adulthood covariates included conventional cardiovascular risk factors. Behaviors included physical activity (assessed with a single item asking about vigorous activity), heavy alcohol consumption (more than one drink daily for women; more than two drinks daily for men [40]), and western and prudent dietary patterns (assessed with a 25-item food frequency questionnaire [41, 42]). Western diets were characterized by higher consumption of red meats, processed meats, refined grains, high-fat dairy products, and sugar-sweetened beverages; prudent diets were characterized by higher consumption of fruits, vegetables, legumes, whole grains, fish, and poultry. Body mass index was assessed with height and weight obtained by study personnel and calculated as kg/m2. C-reactive protein concentrations were determined using an immunoturbidimetric assay on the Hitachi 917 analyzer (Roche Diagnostics, Indianapolis, IN), using reagents and calibrators from DiaSorin (Still-water, MN). This assay has a sensitivity of 0.03 mg/L. The day-to-day variabilities of the assay at concentrations of 0.91, 3.07, and 13.38 mg/L are 2.81, 1.61, and 1.1 %, respectively. C-reactive protein levels ranged from 0.07 to 80.10 mg/L in this sample. C-reactive protein was (natural) log transformed due to skewed distribution and examined continuously.
Analysis
Bivariate associations of participant characteristics with each emotion regulation strategy were evaluated via Pearson’s correlations. Multiple linear regression models assessed the associations of each emotion regulation strategy with cardiovascular disease risk. The distribution of cardiovascular disease risk scores was skewed and therefore log (natural) transformed. To maintain the original units of the cardiovascular disease risk algorithm, regression coefficients were exponentiated and reported as the percent change in cardiovascular disease risk per one standard deviation increase in emotion regulation score [43]. Three multiple linear regression models were fit separately for reappraisal and suppression strategies to assess the association between each type of emotion regulation strategy and cardiovascular disease risk. Demographic and childhood covariates were considered as potential confounders, while adulthood covariates were considered as possible pathways by which emotion regulation might influence cardiovascular disease risk. The demographics model included the emotion regulation measure plus age, race, gender, education attainment, and study site. The childhood model additionally included whether or not the child was born small for gestational age, child cognitive ability, chronic health conditions, socioeconomic status, and childhood cardiovascular health (body mass index, systolic and diastolic blood pressure). The pathways model additionally included adult body mass index, physical activity, heavy alcohol use and western and prudent dietary patterns, and C-reactive protein. Evidence of mediation was assessed via observation of coefficient changes for the emotion regulation variables from the childhood model to the pathways model with the addition of the hypothesized mediators to the model [44, 45]. Because the data for the adulthood factors are cross-sectional, we do not formally test potential mediation and acknowledge that the direction of effects could be reversed (i.e., adult body mass index may influence emotion regulation). Also, we examined whether emotion regulation and cardiovascular disease risk differed according to gender via interaction terms and stratified models. Finally, to evaluate which components of the cardiovascular disease algorithm may be most strongly related to emotion regulation, regression models were fit for these variables as outcomes. All models were fit in SAS 9.1 using PROC GENMOD to adjust variance estimates for the presence of multiple siblings from the same mother in the sample. Statistical significance was determined by 95 % confidence intervals and p values less than 0.05.
Results
Descriptive Statistics
Table 1 summarizes sample characteristics for the analytic sample and also displays bivariate associations of reappraisal and suppression with covariates. Participants were more likely to be female, white, were an average of 42 years old, and had approximately 13.5 years of education. Higher reappraisal scores were significantly associated with being female, born small for gestational age, lower C-reactive protein, lower adulthood body mass index, greater adherence to a prudent diet, higher educational attainment, and fewer depressive symptoms (ps<0.05). Higher suppression scores were associated with being male, lower childhood diastolic blood pressure, lower childhood socioeconomic status, lower childhood cognitive ability, higher C-reactive protein, higher adulthood body mass index, greater adherence to a western diet, less adherence to a prudent diet, and lower educational attainment (ps<0.05).
Table 1.
Characteristics of participants and correlations with emotion regulation strategies
| Characteristic | Mean (SD) or % | Reappraisal r | Suppression r |
|---|---|---|---|
| Cardiovascular disease risk, % | 4.9 (4.5) | −0.13* | 0.20*** |
| Demographic factors | |||
| Gender, female, % | 57.6 | 0.15** | −0.21*** |
| Race, not white, % | 18.0 | 0.06 | 0.11* |
| Age, years | 42.2 (1.7) | −0.03 | 0.04 |
| Education, years | 13.5 (2.6) | 0.11* | −0.18*** |
| Childhood factors | |||
| Small for gestational age, % | 10.7 | 0.12* | 0.06 |
| Systolic blood pressure, mmHg | 104.5 (10.8) | 0.07 | −0.02 |
| Diastolic blood pressure, mmHg | 60.5 (10.2) | −0.02 | −0.13* |
| Chronic condition, % | 18.2 | −0.02 | 0.02 |
| Body mass index, kg/m2 | 16.1 (1.6) | −0.04 | −0.03 |
| Socioeconomic status | 54.2 (22.9) | 0.05 | −0.22*** |
| Cognitive ability, IQ | 102.3 (13.6) | −0.02 | −0.12* |
| Adulthood factors | |||
| C-reactive protein, mg/L | 1.03 | −0.16** | 0.19*** |
| Body mass index, kg/m2 | 29.2 (7.8) | −0.18*** | 0.15** |
| Western diet, z | 0.03 (1.1) | 0.03 | 0.14** |
| Prudent diet, z | −0.002 (0.67) | 0.22*** | −0.15** |
| Heavy drinker, % | 7.8 | 0.04 | 0.09+ |
| Vigorous physical activity, % | 72.9 | −0.03 | 0.04 |
p<0.10;
p<0.05;
p<0.01;
p<0.001
Cardiovascular disease risk was significantly higher among males (7.3 %) compared to females (3.1 %; t(371) = −9.9, p<0.001). Cardiovascular disease risk was positively associated with age (r(371) = 0.28, p<0.001), childhood systolic blood pressure (r(371) = 0.13, p<0.05), C-reactive protein (r(371) = 0.12, p < 0.05), adulthood body mass index (r(371) = 0.32, p < 0.001), western diet (r(371) = 0.13, p<0.05), heavy drinking (t(371) = −2.0, p<0.05), and negatively associated with childhood socioeconomic status (r(371) = −0.16, p<0.01), educational attainment (r(371) = −0.15, p<0.01), physical activity (t(371) = 2.0, p<0.05), and prudent diet (r(371) = −0.16, p<0.01). Although some covariates were not associated with emotion regulation or cardiovascular disease risk measures, all factors were included in the regression models to be conservative. There was no correlation among suppression and reappraisal scores (r(371) = −0.06, p = 0.21), which is consistent with other work that indicates the two emotion regulation strategies are largely independent of one another [7].
Emotion Regulation and 10-year Cardiovascular Disease Risk
Table 2 summarizes the results from the multiple linear regression models predicting 10-year cardiovascular disease risk. After controlling for demographic and childhood factors, a one standard deviation increase in reappraisal was marginally associated with 5.9 % lower 10-year cardiovascular disease risk. Therefore, given the average 10-year cardiovascular disease risk in our sample was 4.9 % (Table 1), our models suggest that a one standard deviation increase in reappraisal may lower this risk by 5.3 %, resulting in 10-year cardiovascular disease risk of 4.6 % (4.9−[0.059 × 4.9] = 4.6). This is similar in magnitude to the reduction in risk associated with following a prudent diet. For example, a one standard deviation increase in the prudent diet score was associated with 7.4 % lower 10-year cardiovascular disease risk (p<0.05), which suggests a lower average 10-year cardiovascular disease risk of 4.5 % (4.9−[0.074 × 4.9] = 4.5).
Table 2.
Multiple linear regression coefficients (standard error) representing change in adult 10-year cardiovascular disease risk per one standard deviation change in emotion regulation
| Demographic | Childhood | Pathways | |
|---|---|---|---|
| Reappraisal | −5.3+ (1.04) | −5.9+ (1.03) | −0.01 (1.04) |
| Suppression | 10.5** (1.03) | 10.0** (1.03) | 5.0+ (1.03) |
Demographic model adjusts for age, race, gender, education, and study site. Childhood model adjusts for demographic and childhood factors (born small for gestational age, socioeconomic status, chronic conditions, cognitive ability, body mass index, blood pressure). Pathways model adjusts for demographic, childhood and adulthood factors (physical activity, body mass index, alcohol use, diet, and C-reactive protein)
p<0.10;
p<0.01
Significant associations were also observed for suppression, but in the opposite direction. After controlling for demographic and childhood factors, a one standard deviation increase in suppression was associated with 10 % increase in 10-year cardiovascular disease risk, suggesting a new 10-year cardiovascular disease risk of 5.4 % (4.9+[0.10 × 4.9] = 5.4). This is similar in magnitude to the increased risk associated with following a western diet. For example, a one standard deviation increase in the western diet score was associated with 7.0 % increase in 10-year cardiovascular disease risk, which suggests a higher average 10-year cardiovascular disease risk of 5.2 % (4.9+[0.07 × 4.9] = 5.2).
As indicated in Table 2, pathway models, the associations for reappraisal and suppression were attenuated with additional adjustment for the adulthood pathway variables, suggesting that these adulthood factors might help explain the observed associations. In the fully adjusted models, the marginal association for reappraisal with cardiovascular disease risk was completely attenuated. Suppression maintained a marginally significant association with cardiovascular disease risk but was attenuated 50 % from the prior model. In the pathways models for both reappraisal and suppression, C-reactive protein, adulthood body mass index, western diet, and heavy drinking were strongly associated with cardiovascular disease risk (all ps<0.05). These coefficient changes suggest that the associations between emotion regulation and cardiovascular disease risk may be explained in part by C-reactive protein, body mass index, diet, and heavy alcohol consumption.
Gender-Specific Associations
Controlling for demographic and childhood factors, a one standard deviation increase in reappraisal was marginally associated with 8 % lower 10-year cardiovascular disease risk (SE = 1.0, p<0.10) and a one standard deviation increase in suppression was associated with 12 % higher cardiovascular disease risk (SE = 1.0, p<0.05) among women. However, for men, emotion regulation was not significantly associated with cardiovascular disease risk (βreappraisal = −4.1, SE = 1.0, p>0.10; βsuppression = 4.1, SE = 1.1, p>0.10). The gender inter-action terms were not significant for either reappraisal (β = −5.5, SE = 1.1, p>0.10) or suppression (β = 6.8, SE = 1.1, p>0.10). Although there is an appearance of a gender difference in the association of emotion regulation and cardiovascular disease risk, there is insufficient evidence to make such a conclusion.
Emotion Regulation and Components of the Cardiovascular Disease Risk Algorithm
To evaluate which components of the cardiovascular disease algorithm were most strongly related to reappraisal and suppression or possibly driving effects, separate regression models were fit with the algorithm component parts as outcomes (Table 3). Reappraisal was associated with each algorithm component in a consistent manner; most associations did not reach statistical significance, although reappraisal was marginally associated with higher HDL cholesterol. Suppression was also associated with all components in a consistent manner and magnitude of effect was often statistically significant (e.g., higher systolic blood pressure, greater likelihood of antihypertensive medication use, and smoking; ps<0.05).
Table 3.
Linear and logistic regression models for the association of emotion regulation strategies and modifiable components of the 10-year cardiovascular disease risk algorithm
| Algorithm component | M (SD) | Reappraisal β (SE) | Suppression β (SE) |
|---|---|---|---|
| Total cholesterol, mg/dL | 196.4 (39.9) | 0.33 (2.37) | −0.14 (1.99) |
| HDL cholesterol, mg/dL | 49.5 (16.6) | 1.22+ (0.75) | −1.28 (0.90) |
| Systolic blood pressure, mmHg | 114.5 (15.7) | −0.92 (0.81) | 1.76* (0.82) |
| % | OR (95 % CI) | OR (95 % CI) | |
| Antihypertensive medication use | 11.0 | 0.93 (0.69, 1.38) | 1.47* (1.03, 2.09) |
| Smoker | 27.9 | 0.87 (0.65, 1.10) | 1.28* (1.01, 1.64) |
| Diabetes | 4.3 | 0.75 (0.43, 1.29) | 1.17 (0.62, 1.03) |
Models are adjusted for demographic (age, race, gender, education, study site) and childhood (born small for gestational age, socioeconomic status, chronic conditions, cognitive ability, body mass index, blood pressure) covariates
p<0.10;
p<0.05
Discussion
The results of this study indicate that reappraisal (an antecedent-focused emotion regulation strategy) is associated with lower 10-year cardiovascular disease risk whereas suppression (a response-focused emotion regulation strategy) was associated with elevated 10-year cardiovascular disease risk. Moreover, our findings suggest that cardiovascular risk factors (e.g., C-reactive protein, body mass index, diet, heavy alcohol consumption) may be on the pathway linking these emotion regulation strategies with cardiovascular disease risk. These results are consistent with previous work in this sample and other population-based studies in finding emotion regulation to be associated with cardiovascular health.
This study expands the evidence base in several ways. Where other studies of emotion regulation strategies and cardiovascular disease risk to date have focused on general cardiovascular risk markers (metabolic syndrome, inflammation [12, 15]), this study directly estimates the likelihood of developing cardiovascular disease using a validated prediction algorithm. Moreover, where other work has focused on general markers of regulation [14] or unusual features of emotion regulation [15], this study focused on two commonly used emotion regulation strategies [7, 8]. Possible gender patterning in emotion regulation and cardiovascular disease associations were considered, and potential pathways linking emotion regulation to cardiovascular disease were identified. Moreover, associations between regulatory strategies and cardiovascular disease risk were observed over and above key early life factors including childhood cardiovascular health and early life psychosocial factors. As emotion regulation and cardiovascular disease both have developmental origins in childhood [8, 30], rigorous control for such early life factors yields more precise estimates of the magnitude and direction of the relationships between emotion regulation and cardiovascular disease than have previously been identified.
Although there is the appearance of a gender difference in the stratified models, there is insufficient evidence to confirm this. The interactions we observed did not reach statistical significance and findings from the gender-stratified models may be attributable in part to the sample having slightly more females than males. While suggestive of gender patterning in emotion regulation and cardiovascular disease risk associations, additional work in larger samples is needed to better test whether one gender is more strongly affected by emotion regulation than the other.
Findings from the pathways analyses suggest there are several behavioral and physiologic mechanisms through which reappraisal and suppression may affect cardiovascular disease risk. Both reappraisal and suppression were associated with C-reactive protein, adult body mass index, and cardiovascular disease -related risk behaviors, but in opposite directions: reappraisal was associated with having lower C-reactive protein, lower body mass index, and adherence to a healthy diet whereas suppression was associated with higher C-reactive protein, higher body mass index, adherence to an unhealthy diet, and heavy alcohol consumption. However, as the emotion regulation and potential pathway variables were assessed concurrently, we cannot rigorously test for mediation or rule out the possibility of reverse causation. We note these associations for descriptive purposes and encourage future work to examine these potential pathways using temporally distinct factors.
Emotion regulation may affect also cardiovascular disease risk via direct biological effects related to hypothalamic-pituitary-adrenal axis and sympathetic nervous system activation. Experimental studies have demonstrated that suppression leads to greater hypothalamic-pituitary-adrenal axis and sympathetic nervous system activation [10, 46, 47]. Such heightened hypothalamic-pituitary-adrenal axis and sympathetic nervous system activity is associated with cardiovascular disease-related pathophysiology including damage to the endothelium and resultant inflammation, as well as atherosclerosis and atherosclerotic lipid profiles [48]. The dysregulation of emotion and accompanying psychosocial stress may therefore promote heightened hypothalamic-pituitary-adrenal axis, sympathetic nervous system activity, and cardiovascular reactivity whereas reappraisal and the effective regulation of emotion and stress may prevent or limit such activity. Over time, use of such adaptive versus less adaptive regulatory strategies may cumulatively alter cardiovascular disease risk trajectories. Additional research is needed to identify underlying biological mechanisms more specifically.
In deconstructing the cardiovascular disease risk algorithm in relation to reappraisal and suppression, we found different components of the algorithm associated with each strategy. Reappraisal was associated with higher HDL or “good” cholesterol, which was congruent with the observed positive associations for reappraisal with healthy eating and lower body mass index. In contrast, suppression was most strongly associated with hypertension (indexed by higher systolic blood pressure and greater likelihood for antihypertensive medication use) and smoking. These findings suggest that while emotion regulation may contribute to cardiovascular disease risk, the mechanisms through which each strategy may influence risk could vary and in fact there may be multiple paths and systemic effects (i.e., the whole is greater than the sum of its parts). Moreover, these findings suggest that when emotion regulatory strategies are more adaptive it may be because they both enhance restorative processes (e.g., eating a healthy diet) and mitigate the likelihood of deteriorative processes (e.g., engaging in cigarette smoking), whereas less adaptive strategies may make deteriorative processes more likely [6]. This has significant implications for intervention as building adaptive emotion regulation skills and reducing use of less adaptive strategies may have different benchmarks in assessing progress for reducing cardiovascular disease risk.
This study has some limitations. First, it was a cross-sectional examination of emotion regulation and cardiovascular disease risk measured at a single time point. Although the development of emotion regulation strategies largely occurs during childhood [8] and our outcome measure assesses future risk of developing cardiovascular disease, we cannot rule out the possibility that components of the cardiovascular disease risk algorithm could influence reports of emotion regulation. Similarly, emotion regulation, pathway, and outcome variables were assessed concurrently precluding rigorous tests of mediation. We encourage future work with temporally distinct measures of emotion regulation, potential pathways, and cardiovascular disease outcomes to replicate our findings and test mediation explicitly. Moreover, we encourage future work to consider the developmental origins of emotion regulation in association with cardiovascular disease risk by using prospective measures of childhood emotion regulation, adulthood emotion regulation, and cardiovascular disease risk. Also, while we control for a well-characterized set of potential confounders from childhood, unmeasured confounding may underlie the observed associations (e.g. genetics). Additionally, generalizability may be limited as participant selection was based on certain characteristics per the project aims. These limitations notwithstanding, this study has a number of strengths. First, our measure of cardiovascular disease risk is largely based on objectively measured biomarkers and has good predictive validity for cardiovascular disease events over the subsequent 10 years [31]. Biomarkers and prediction algorithms are not subject to reporting biases and can provide insight into physiologic mechanisms through which psychosocial functioning may influence health. Also, we used a validated measure of emotion regulation that has good psychometric properties. Finally, we controlled for several child health and early life psychosocial factors that are critical to the development of emotion regulation skills and cardiovascular disease; this improves confidence that observed relationships are not spurious.
There is a large literature indicating both positive and negative emotions are relevant in terms of maintaining cardiovascular health or developing cardiovascular disease [6, 49], although the exact nature of the relationship is not well understood. Investigators have begun to speculate that beyond effects of any specific emotion, it is the regulation of emotion that is critical. This study provides support for this hypothesis by demonstrating that response-focused emotion regulation may increase cardiovascular disease risk whereas antecedent-focused emotion regulation may reduce risk and promote cardiovascular health. These findings have significant implications for prevention and intervention as reappraisal and suppression are learned strategies and not innate traits [8]. It may be possible to teach individuals how to effectively manage their emotions which may not only improve psychological functioning, but may also promote resiliency and positive cardiovascular health as well.
Acknowledgments
This work was supported by National Institute of Aging grant AG023397, National Institutes of Health Transdisciplinary Tobacco Use Research Center (TTURC) Award (P50 CA084719) by the National Cancer Institute, the National Institute on Drug Abuse, and the Robert Wood Johnson Foundation. Dr. Appleton was supported by the National Heart Lung and Blood Institute Training Grant at the Harvard School of Public Health (T32 HL098048), and the Quantitative Biomedical Sciences training program at Geisel School of Medicine at Dartmouth (R25 CA134286).
Footnotes
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Appleton, Loucks, Buka, and Kubzansky declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Contributor Information
Allison A. Appleton, Email: aappleton@albany.edu, School of Public Health, Department of Epidemiology and Biostatistics, University at Albany, State University of New York, One University Place, Rensselaer, NY 12144-3456, USA.
Eric B. Loucks, Department of Epidemiology, Brown University School of Public Health, Providence, RI, USA.
Stephen L. Buka, Department of Epidemiology, Brown University School of Public Health, Providence, RI, USA.
Laura D. Kubzansky, Department of Society, Human Development and Health, Harvard School of Public Health, Boston, MA, USA.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: A report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics-2010 update: A report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 3.Miller G, Chen E, Cole SW. Health psychology: Developing biologically plausible models linking the social world to physical health. Annu Rev Psychol. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- 4.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular disease. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 5.Kobau R, Seligman MEP, Peterson C, et al. Mental health promotion in public health: Perspectives and strategies from positive psychology. Am J Public Health. 2011;101:e1–e9. doi: 10.2105/AJPH.2010.300083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boehm JK, Kubzansky LD. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychol Bull. 2012 doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- 7.Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships and well-being. J Pers Soc Psychol. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 8.John OP, Gross JJ. Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. J Pers. 2004;72:1301–1334. doi: 10.1111/j.1467-6494.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- 9.Gross JJ. Emotion regulation in adulthood: Timing is everything. Curr Dir Psychol Sci. 2001;10:214–219. [Google Scholar]
- 10.Appleton AA, Kubzansky LD. Emotion regulation and cardiovascular disease risk. In: Gross JJ, editor. Hanbook of Emotion Regulation. 2. New York: The Guilford Press; 2014. [Google Scholar]
- 11.Consedine NS, Magai C, Bonanno GA. Moderators of the emotion inhibition-health relationship: A review and research agenda. Rev Gen Psychol. 2002;6:204–228. [Google Scholar]
- 12.Appleton AA, Buka SL, Loucks EB, Gilman SE, Kubzansky LD. Divergent associations of adaptive and maladaptive emotion regulation strategies with inflammation. Health Psychol. 2013;13:748–756. doi: 10.1037/a0030068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rozanski A, Kubzansky LD. Psychologic functioning and physical health: A paradigm of flexibility. Psychosom Med. 2005;67:S47–S53. doi: 10.1097/01.psy.0000164253.69550.49. [DOI] [PubMed] [Google Scholar]
- 14.Kubzansky LD, Park N, Peterson C, Vokonas P, Sparrow D. Healthy psychological functioning and incident coronary heart disease: The importance of self-regulation. Arch Gen Psychiatr. 2011;68:400–408. doi: 10.1001/archgenpsychiatry.2011.23. [DOI] [PubMed] [Google Scholar]
- 15.Kinnunen M, Kokkonen M, Kaprio J, Pulkkinen L. The associations of emotion regulation and dysregulation with the metabolic syndrome factor. J Psychosom Res. 2005;58:513–521. doi: 10.1016/j.jpsychores.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 16.C Reactive Protein Coronary Heart Disease Genetics Collaboration. Association between C reactive protein and coronary heart disease: Mendelian randomisation analysis based on individual participant data. BMJ. 2011;342:1–8. doi: 10.1136/bmj.d548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Danesh D, Wheeler JG, Hirschfield GM, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. New Engl J Med. 2004;350:1387–1397. doi: 10.1056/NEJMoa032804. [DOI] [PubMed] [Google Scholar]
- 18.Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice. A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 19.Elliott P, Chambers JC, Zhang W, et al. Genetic loci associated with c-reactive protein levels and risk of coronary heart disease. JAMA. 2009;302:37–48. doi: 10.1001/jama.2009.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Appleton AA, Loucks EB, Buka SL, Rimm E, Kubzansky LD. Childhood emotional functioning and the developmental origins of cardiovascular disease risk. J Epidemiol Community Health. 2013;67:405–411. doi: 10.1136/jech-2012-201008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thurston RC, Kubzansky LD. Multiple sources of psychosocial disadvantage and risk of coronary heart disease. Psychosom Med. 2007;69:748–755. doi: 10.1097/PSY.0b013e31815772a3. [DOI] [PubMed] [Google Scholar]
- 22.Moller-Leimkuhler A. Higher comorbidity of depression and cardiovascular disease in women: A biopsychosocial perspective. World J Biol Psychiatry. 2010;11:922–933. doi: 10.3109/15622975.2010.523481. [DOI] [PubMed] [Google Scholar]
- 23.Lazarus RS. Emotion and Adaptation. New York: Oxford University Press; 1991. [Google Scholar]
- 24.Calkins SD, Hill A. Caregiver influences on emerging emotion regulation: Biological and environmental transactions in early development. In: Gross JJ, editor. Handbook of Emotion Regulation. New York: The Guilford Press; 2007. pp. 229–248. [Google Scholar]
- 25.Thompson R. Family influences on emotion regulation. In: Gross JJ, editor. Handbook of Emotion Regulation. 2. New York: The Guilford Press; 2014. [Google Scholar]
- 26.Rothbart M, Posner M. Temperament and emotion regulation. In: Gross JJ, editor. Handbook of Emotion Regulation. 2. New York: The Guilford Press; 2014. [Google Scholar]
- 27.Shonkoff JP, Phillips DA, editors. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 28.Hart CL, Taylor MD, Davey Smith G, et al. Childhood IQ and cardiovascular disease in adulthood: Prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. Soc Sci Med. 2004;59:2131–2138. doi: 10.1016/j.socscimed.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 29.Pollitt RA, Rose KM, Kaufman JS. Evaluating the evidence for models of life course socioeconomic factors and cardiovascular outcomes: A systematic review. BMC Public Health. 2005;5:7. doi: 10.1186/1471-2458-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berenson GS, Srnivasan SR. Cardiovascular risk factors in youth with implications for aging: The Bogalusa heart study. Neurobiol Aging. 2005;26:303–307. doi: 10.1016/j.neurobiolaging.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 31.D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117:742–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 32.Broman SH, Nichols PI, Kennedy WA. Preschool IQ: Prenatal and Early Developmental Correlates. New York: Hallstead Press; 1975. [Google Scholar]
- 33.Niswander KR, Gordon M. The Women and Their Pregnancies. Washington, DC: US Government Printing Office; 1972. [Google Scholar]
- 34.Almeida ND, Loucks EB, Kubzansky LD, et al. Quality of parental emotional care and calculated risk for coronary heart disease. Psychosom Med. 2010;72:148–155. doi: 10.1097/PSY.0b013e3181c925cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–475. [PubMed] [Google Scholar]
- 36.Rafai N, Cole TG, Iannotti E, et al. Assessment of interlaboratory performance in external proficiency testing programs with a direct HDL-cholesterol assay. Clin Chem. 1998;44:1452–1458. [PubMed] [Google Scholar]
- 37.Mattu GS, Heran BS, Wright JM. Overall accuracy of the BpTRU -an automated electronic blood pressure device. Blood Press Monit. 2004;9:47–52. doi: 10.1097/00126097-200402000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Wechsler D. Wechsler Intelligence Scale for Children. New York: The Psychological Corporation; 1949. [Google Scholar]
- 39.Myrianthopoulos N, French K. An application of the U.S. Bureau of the Census socioeconomic index to a large, diversified patient population. Soc Sci Med. 1968;2:283–299. doi: 10.1016/0037-7856(68)90004-8. [DOI] [PubMed] [Google Scholar]
- 40.CDC. Fact Sheets - Alcohol Use and Health. Retrieved 9/12/13, 2013 from http://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm.
- 41.Willett WC. Nutritional Epidemiology. 2. New York: Oxford University Press; 1998. [Google Scholar]
- 42.Michaud DS, Skinner HG, Wu K, et al. Dietary patterns and pancreatic cancer risk in men and women. J Natl Cancer Inst. 2005;97:518–524. doi: 10.1093/jnci/dji094. [DOI] [PubMed] [Google Scholar]
- 43.UCLA Academic Technology Services Statistical Consulting Group. Introduction to SAS. 2011. [Google Scholar]
- 44.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 45.Kramer HC, Kiernan M, Essex M. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approachs. Health Psychol. 2008;27:S101–S108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gross JJ, Levenson RW. Emotion suppression: Physiology, self-report, and expressive behavior. J Pers Soc Psychol. 1993;64:970–986. doi: 10.1037//0022-3514.64.6.970. [DOI] [PubMed] [Google Scholar]
- 47.Gross JJ, Levenson RW. Hiding feelings: The acute effects of inhibiting negative and positive emotion. J Abnorm Psychol. 1997;106:95–103. doi: 10.1037//0021-843x.106.1.95. [DOI] [PubMed] [Google Scholar]
- 48.Black PH, Garbutt LD. Stress, inflammation and cardiovascular disease. J Psychosom Res. 2002;52:1–23. doi: 10.1016/s0022-3999(01)00302-6. [DOI] [PubMed] [Google Scholar]
- 49.Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychol Bull. 2005;131:260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]