Supplemental Digital Content is Available in the Text.
Key Words: depression, pregnancy, postpartum, perinatal, HIV infection, antiretroviral therapy, mental health, maternal health, Uganda
Abstract
Background:
Among HIV-infected women, perinatal depression compromises clinical, maternal, and child health outcomes. Antiretroviral therapy (ART) is associated with lower depression symptom severity but the uniformity of effect through pregnancy and postpartum periods is unknown.
Methods:
We analyzed prospective data from 447 HIV-infected women (18–49 years) initiating ART in rural Uganda (2005–2012). Participants completed blood work and comprehensive questionnaires quarterly. Pregnancy status was assessed by self-report. Analysis time periods were defined as currently pregnant, postpartum (0–12 months post-pregnancy outcome), or non–pregnancy-related. Depression symptom severity was measured using a modified Hopkins Symptom Checklist 15, with scores ranging from 1 to 4. Probable depression was defined as >1.75. Linear regression with generalized estimating equations was used to compare mean depression scores over the 3 periods.
Results:
At enrollment, median age was 32 years (interquartile range: 27–37), median CD4 count was 160 cells per cubic millimeter (interquartile range: 95–245), and mean depression score was 1.75 (s = 0.58) (39% with probable depression). Over 4.1 median years of follow-up, 104 women experienced 151 pregnancies. Mean depression scores did not differ across the time periods (P = 0.75). Multivariable models yielded similar findings. Increasing time on ART, viral suppression, better physical health, and “never married” were independently associated with lower mean depression scores. Findings were consistent when assessing probable depression.
Conclusions:
Although the lack of association between depression and perinatal periods is reassuring, high depression prevalence at treatment initiation and continued incidence across pregnancy and non–pregnancy-related periods of follow-up highlight the critical need for mental health services for HIV-infected women to optimize both maternal and perinatal health.
INTRODUCTION
Depression is a serious global public health issue,1,2 particularly among women of reproductive age.3 People living with HIV have higher rates of depression compared with those observed in the general population in western4,5 and sub-Saharan African countries.6 Among HIV-infected individuals, depression has deleterious effects on psychological well-being and quality of life6 and undermines HIV treatment through associations with poor adherence to antiretroviral therapy (ART),7–10 HIV disease progression,11 CD4 cell count decline, virologic failure,12,13 and increased mortality.14
Among HIV-infected women in Uganda and other sub-Saharan African countries, 15%–50% screen positive for probable depression.6,15–18 A high incidence of pregnancy19,20 and burden of perinatal depression among HIV-infected women21–23 further compromises HIV-related clinical, immunologic, and virologic outcomes,24 as well as overall maternal health. Maternal depression also impacts child health outcomes, including risks of perinatal HIV transmission, poor physical health,25 impaired cognitive, behavioral, and psychomotor development,26 and delayed socio-emotional development.27
Access to ART has expanded dramatically in HIV endemic, resource-limited settings,28 yielding clinical29–32 and population-level benefits.33–35 Recent data from sub-Saharan Africa suggest that receipt of ART is also associated with lower depression symptom severity,36–38 through physiological, psychological, and stigma reduction pathways.39,40 However, the extent to which ART affects depression across perinatal periods is not known.
The primary objective of this prospective study was to measure and compare depression symptom severity during non–pregnancy-related, pregnant, and postpartum periods among HIV-infected women initiating ART in rural Uganda. Understanding the relationship between depression and perinatal periods among women on ART may inform reproductive and mental health programming for HIV-infected women considering pregnancy to optimize maternal and perinatal health.
METHODS
Study Setting
Uganda is an important setting in which to investigate depression over perinatal periods given a total fertility rate of 6.2 births per woman41 and HIV prevalence of 7.2%,20,42 higher among women (8.2%) than among men (6.1%). In addition, 70% of treatment-eligible Ugandans access ART.20,28 ART coverage among women with pregnancy is expected to increase with Uganda's adoption of “Option B+” to prevent perinatal HIV transmission.43,44
Mbarara District is a primarily rural setting located approximately 265 km southwest of Kampala. Adult HIV prevalence in the district is estimated at 10%45 and is higher among women compared with men. The Mbarara University HIV clinic is located within the Mbarara Regional Referral Hospital and offers comprehensive HIV care services, including ART, at no cost to patients.46
Study Participants
Study participants were enrolled in the Uganda AIDS Rural Treatment Outcomes (UARTO) cohort study, initiated in July 2005 with the primary objective of determining predictors of virologic failure and antiretroviral resistance. Participants were recruited from HIV-infected, treatment-naive adults initiating ART at the Mbarara University HIV clinic. Patients who were at least 18 years old and living within 60 km of the clinic were eligible to enroll. At the time of this analysis, 447 women were enrolled in UARTO. Loss-to-follow-up (participants for whom we were unable to confirm vital status after ≥180 days without cohort follow-up) was 2% at 1 year and 5% at 2 years after enrollment.
Data Collection
Participants were seen at baseline (ie, at ART initiation) and quarterly for bloodwork and to complete standardized interviewer-administered questionnaires detailing sociodemographics, mental and physical health, sexual risk behaviour, and partner dynamics. Incident pregnancies were assessed by self-report. Interviews were administered in the dominant local language (Runyankole). This analysis includes data from female participants (18–49 years) enrolled from June 2005 followed through December 2012.
Measures
Primary Outcome: Depression
Depression symptom severity was measured using a modified version of the Hopkins Symptom Checklist (HSCL)-15 for depression.47 Based on previous studies using HSCL in Uganda, we included a 16th item, “Feeling like I don't care about my health.”48 Each symptom was scored on a 4-item Likert scale ranging from 1 (not at all) to 4 (extremely) and the total depression severity score was calculated as the mean of the 16 items, with higher scores indicating greater depression symptom severity. We also assessed a dichotomous measure of “probable depression” defined as an HSCL score >1.75, a commonly used threshold for a positive screen of depression.47–50
The depression subscale of HSCL has been used to assess depression in general population samples and among people living with HIV in sub-Saharan African countries.47–49,51–54 The HSCL has been further shown to have good reliability55 and construct validity56 among people living with HIV in Uganda specifically. Although the HSCL was not designed to specifically screen for perinatal depression, it and other generic depression scales are commonly used to measure depression among antenatal women.54,57–59 The most reliable, valid, and frequently used measure of perinatal depression in sub-Saharan Africa is the Edinburgh Postnatal Depression Scale54; however, the reliability and validity of the Edinburgh Postnatal Depression Scale outside of perinatal periods is unknown.
Primary Predictor Variable: Pregnancy Status
The primary predictor variable is a 3-level variable indicating pregnancy status, which we classified as being pregnant, up to 1 year postpartum or neither pregnant nor post-partum (“non–pregnancy-related”). Women who reported sterilization (tubal ligation or hysterectomy) at baseline were excluded from the analysis. If the procedure was reported during follow-up, women were censored upon reported date of the procedure.
Periods of pregnancy were defined based on self-report at baseline and over the follow-up period and included both first and subsequent pregnancies. Pregnancy start was defined as the visit date when pregnancy was first reported and pregnancy end was the subsequent date at which women reported no longer being pregnant. For the few women (n = 8) who reported a live birth outcome and had a computed period of pregnancy of <7 or >11 months, live birth date was used to back-calculate a start date to account for an estimated 9-month gestation. The postpartum period was defined as the period from the end of pregnancy until 12 months after any pregnancy outcome.60,61 All other follow-up times were assessed as non–pregnancy-related.
At study enrollment, women reported whether they were or had been pregnant in the previous 12 months but did not report dates of pre-enrollment pregnancy or postpartum status. Thus, no women were classified as postpartum at study entry.
Covariates
We examined the association between depression and pregnancy status, adjusting for baseline and time-updated covariates considered potential confounders. Baseline variables included sociodemographic characteristics (including age, education, employment, household income, and marital status), reproductive history (including parity), and clinical history (including time since HIV diagnosis, AIDS defining illnesses, CD4 cell count at enrollment, and body mass index). Time-updated variables were measured quarterly and included age, time on HIV treatment, CD4 cell count, HIV viral load <400 copies per milliliter (ie, viral suppression), the Medical Outcomes Study HIV Health Survey Physical Health Summary score (scored on a 0–100 scale, where a higher score indicates better health),62,63 and sexual activity in the previous 3 months.
Data Analysis
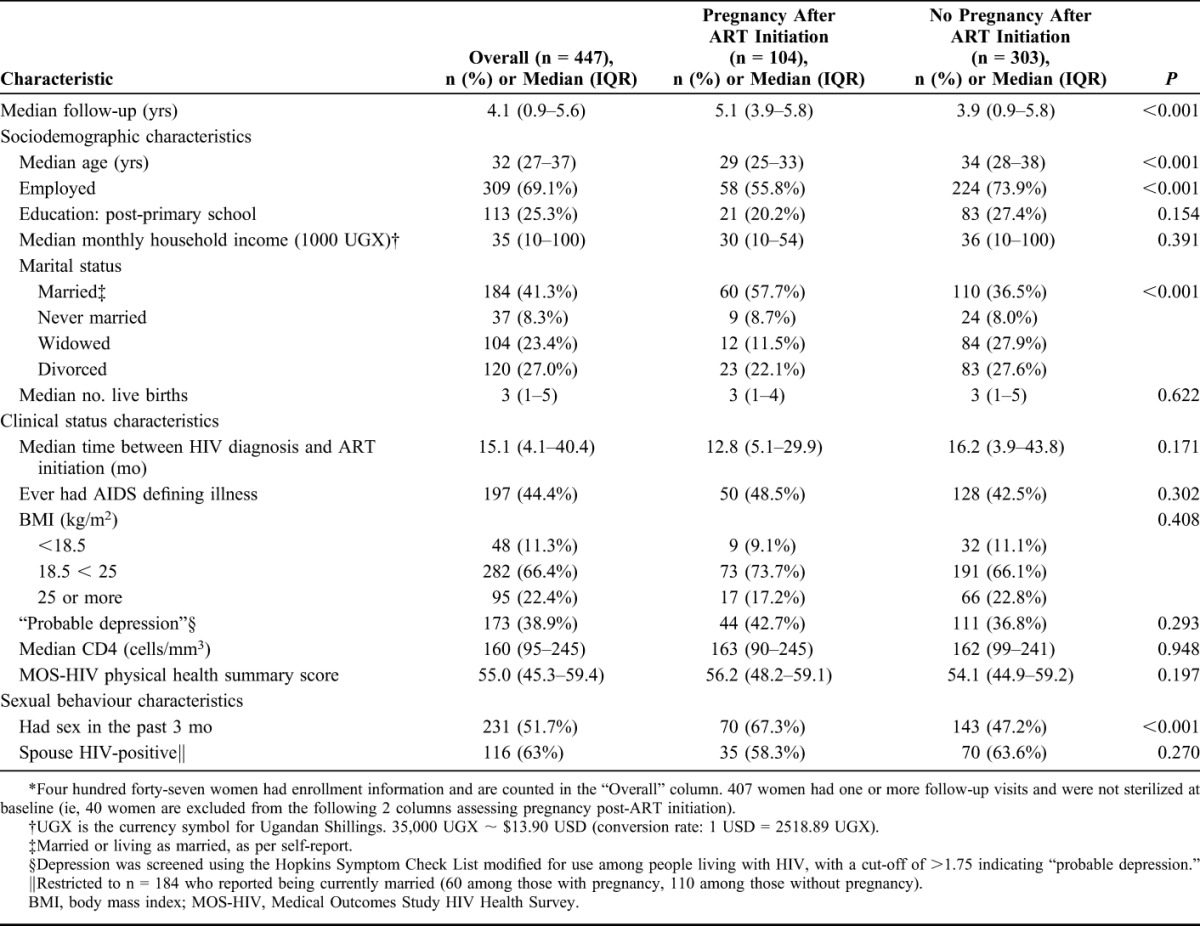
Descriptive statistics were used to characterize baseline distributions of study variables. Baseline differences between women with and without incident pregnancy were compared using Wilcoxon rank sum test for continuous variables and Pearson χ2 test for categorical variables. Although our regression models are based on time-varying pregnancy-related status, comparison of fixed categories of pregnancy are provided to inform understanding of differences between women who exclusively contributed to non-pregnant periods and those who contributed to all 3 periods of follow-up.
We calculated the mean (SD) HSCL score at baseline and then compared mean HSCL scores across pregnant, postpartum, and non–pregnancy-related periods using analysis of variance. We plotted mean HSCL scores (with residual standard error bars) across the 3 periods by time on ART. We fit a multivariable linear regression model to the data, using generalized estimating equations to estimate model parameters. We used an autoregressive working correlation structure. Pregnancy and the postpartum period were investigated as independent predictors of depression symptom severity. After testing normality assumptions and collinearity, variables with a significant association with depression in bivariate analyses (at P < 0.20) were considered for the full model to obtain the relative contribution of each covariate. Model selection was achieved by minimizing the Akaike Information Criterion while maintaining P-values for covariates below 0.20.64 All statistical tests were 2-sided and were considered statistically significant at α = 0.05. Using a binary variable for “probable depression,” we also fit a multivariable GEE logistic regression model. The same model selection procedures and covariates were used. Data were analyzed with SAS version 9.3 (SAS Institute Inc., Cary, NC).65
Ethical Statement
All participants provided voluntary, written informed consent at study enrollment. Ethical approval for all study procedures was obtained from the Institutional Review Committee, Mbarara University of Science and Technology; the Partners Human Research Committee, Massachusetts General Hospital; the Committee on Human Research, University of California at San Francisco; and the Research Ethics Board of Simon Fraser University. Consistent with national guidelines, we received clearance for the study from the Uganda National Council for Science and Technology and from the Research Secretariat in the Office of the President.
RESULTS
Baseline Characteristics
Overall, 447 women aged 18–49 years with baseline data were eligible for this study. The analysis was restricted to 407 nonsterilized women with at least 1 follow-up visit. Participants contributed 1564.6 person-years (PYs) of follow-up with a median follow-up time of 4.1 years [interquartile range (IQR): 0.9–5.6 years].
Median age was 32 years (IQR: 27–37 years), 25% had more than a primary school education, 69% were employed, and median monthly household income was 35,000 (IQR: 10,000–100,000) Ugandan Shillings (∼$14 USD). Forty-one percent of women were currently married or living as married. Of 184 married women, 63% reported an HIV-positive spouse, of whom 53% were on ART. Median number of previous live births was 3 (IQR: 1–5) and 52% were sexually active. Median time between HIV diagnosis and ART initiation was 15 months (IQR: 4–40 months), 44% reported ever having an AIDS-defining illness, and median body mass index was 21.9 kg/m2 (IQR: 20.1–24.8 kg/m2). Median CD4 cell count at enrollment was 160 cells per cubic millimeter (IQR: 95–245 cells/mm3) and median Medical Outcomes Study HIV Health Survey Physical Health Summary score was 53 (IQR: 45–59). The mean depression symptom severity score at baseline was 1.75 (SD = 0.58) with 39% of women screening positive for probable depression (Table 1).
TABLE 1.
Baseline Characteristics of Participants (18–49 Years) by Pregnancy Status After ART Initiation*
Depression Symptom Severity by Pregnancy Status
Among 407 women with at least 1 follow-up visit, 104 women reported 151 pregnancies over the follow-up period. In unadjusted analyses, the mean depression symptom severity score did not differ across periods [1.28 (s = 0.37) during non–pregnancy-related periods, 1.29 (s = 0.38) during pregnant periods, and 1.34 (s = 0.49) during postpartum periods; P = 0.749]. Factors associated with lower depression symptom severity included increasing time on ART, viral suppression, better physical health, and having never been married.
After adjusting for covariates, there remained no significant difference in depression symptom severity scores by pregnancy status. However, depression scores during the postpartum were slightly elevated compared with non–pregnancy-related periods [b = 0.05; 95% confidence interval (CI): −0.01 to 0.10; P = 0.098]. In the adjusted model (Table 2), increased cumulative duration of ART receipt [mean score decreased by 0.14 after 6 months (b = −0.14; 95% CI: −0.17 to −0.11) and by 0.22 after 24 months of ART receipt (b = −0.22; 95% CI: −0.26 to −0.19], viral suppression (b = −0.20; 95% CI: −0.24 to −0.16), better physical health (b = −0.16; 95% CI: −0.18 to −0.13), and being never married (b = −0.10; 95% CI: −0.16 to −0.04) compared with currently married were independently associated with lower depression symptom severity. The decline in mean depression symptom severity score across the 3 periods by increasing time on ART is shown in Figure 1.
TABLE 2.
Depression Symptom Severity and Odds of Probable Depression by Pregnancy Status
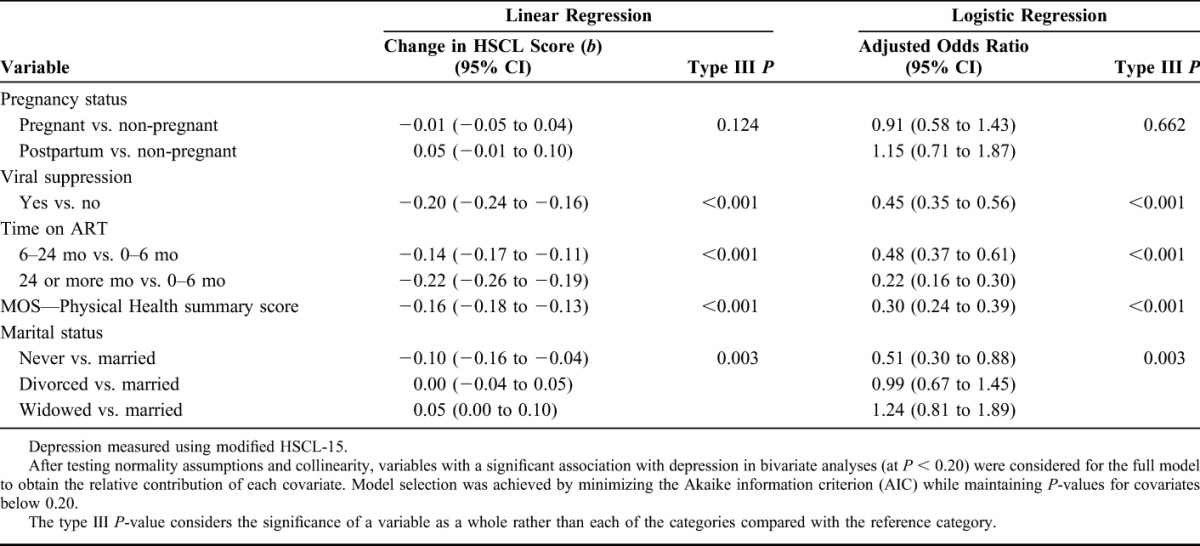
FIGURE 1.
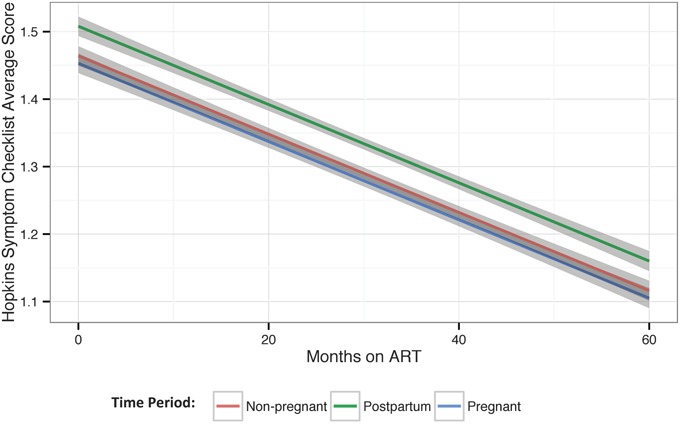
Mean depression symptom severity score over time on ART by pregnancy status (note: error bars are based on the residual standard error).
Probable Depression by Pregnancy Status
The proportion of study visits where women screened positive for probable depression did not differ across periods. The criteria for probable depression was met during 9.5% of study visits overall, including 9.3% of non–pregnancy-related visits, 10.3% of pregnant visits, and 12.1% of postpartum visits (P = 0.37). Consistent with linear models, in adjusted logistic models, increasing time on ART [adjusted odds ratio (aOR) = 0.48; 95% CI: 0.37 to 0.61 after 6 months and aOR = 0.22; 95% CI: 0.16 to 0.30 after 24 months], viral suppression (aOR: 0.45; 95% CI: 0.35 to 0.56), better physical health (aOR: 0.30; 95% CI: 0.24 to 0.39), and being never married (aOR: 0.51; 95% CI: 0.30 to 0.88 compared with being married) were independently associated with lower odds of probable depression (Table 2). The unadjusted odds of probable depression are included in Table S1 (see Supplemental Digital Content, http://links.lww.com/QAI/A586).
DISCUSSION
Among HIV-infected women on ART, we found no difference in depression symptom severity between pregnant and postpartum periods compared with non–pregnancy-related periods. Increasing time on ART and associated improvements in viral suppression and physical health were independently associated with declines in depression symptom severity.
We observed a high prevalence of probable depression at ART initiation (39% of women). This prevalence was higher than rates observed in the general Uganda population (9%–24%)52,66 or among HIV-infected individuals in Uganda18,67 and other sub-Saharan African settings.6,54,68 Although some degree of variability in depression estimates may be because of heterogeneity in screening measures and cultural-specific expressions of depression, the high rate of probable depression observed here is cause for concern.
Over the follow-up period, we did not observe a significant difference between depression and pregnancy status, although depression symptom severity was elevated during postpartum visits (not statistically significant). Findings from other sub-Saharan African countries suggest that among untreated HIV-infected women24 and women in general,69,70 depression rates increase during perinatal follow-up. In our study, the high overall prevalence of depression may mask increases associated with perinatal periods.
The prevalence of probable depression decreased with increasing time on ART. After 6 months of treatment, odds of depression were half those observed at baseline and after 2 years of treatment, odds of probable depression were 78% lower compared with baseline. These results are consistent with work showing substantial mental health benefits of HIV treatment and care, particularly within the first year of ART initiation.36,38 Although depression symptom severity drops with increasing time on ART irrespective of pregnancy status, criteria for probable depression was still met at 9.3%–12.1% of visits across the 3 follow-up periods. Clearly, HIV treatment alone does not treat mental illness among women living with HIV and does not compensate for a lack of comprehensive mental health care.
We found that improvements in physical health were associated with significant decreases in depression symptom severity. This is not surprising and consistent with known improvements in physical function that accompany HIV treatment and care and the relationship between physical and mental health outcomes. Moreover, recent related findings from this cohort reveal a secular trend of declining depression symptom severity scores among participants at study enrollment. This trend was largely explained by higher physical health status among participants presenting for ART initiation over time.71 In addition to the known clinical29–32 and population-health33–35,72 benefits of HIV treatment and care, these findings suggest that earlier initiation of ART, among HIV-infected patients in better physical and clinical health, may have a positive impact on mental health outcomes.
Our finding of an independent lower depression risk among “never married” compared with “currently married” women seems to contrast with literature suggesting a protective mental health effect of marriage. However, in general, health benefits of marital status are highly gendered, with more protective benefits for men than women.73 Such differences relate, in part, to gender and unequal power dynamics within relationships, which are often exacerbated in the context of childbearing. With respect to risk factors for postpartum depression in particular, evidence suggests that the availability of social support in general (within and/or external to the marital relationship) is more strongly protective against postpartum depression than marital status alone.74 Moreover, a recent Ugandan study similarly found that co-habitation with the male partner and marital discord was associated with higher depression scores among postpartum women.69 A related line of research indicates that women with greater relationship power have lower rates of depression.75 This suggests that our findings of a higher depression risk among “currently married” compared with “never married” women may reflect unmeasured discord within those marital relationships.
The pathways through which HIV treatment may lead to declines in depression symptom severity have been summarized36 and include (1) improved physical health leading to better social and economic conditions; (2) facilitation of regular access to general clinic services, counseling, and support (including mental health services, when available) that enable development of positive coping and resiliency; (3) reduced neurotoxic effects of HIV; and (4) lower internalized HIV-related stigma.56 Recent work has also elucidated potential biological pathways through which HIV treatment-mediated changes may reduce depression.39 In our observational study, reductions in depression over time on ART may also reflect a retention bias if women with depression were more likely to be lost-to-follow-up compared with women without depression. However, such biases are unlikely to fully explain our findings given the overall low loss-to-follow-up rate among women enrolled in UARTO (3% and 7% at years 1 and 5, respectively) with no differences in loss-to-follow-up between women with and without pregnancy (7% vs. 8% at time of last observation).
Among pregnant HIV-infected women in settings with a high cultural value on childbearing, these findings suggest that receipt of ART and the resultant opportunity to have an HIV-uninfected child may overwhelm other biological or psychosocial drivers of depression. The observation of no significant increase in postpartum depression among women receiving ART supports the need for research to understand the experience of depression in the context of changing reproductive and maternal health for HIV-infected women in high fertility settings such as Uganda.76,77
Implications
Depression has serious consequences for HIV outcomes and quality of life and can impact maternal and child health and development.6,16,37 The observed high prevalence of depression among HIV-infected women highlights the need for clinical management of depression during and external to perinatal periods. Currently, however, although effective treatments are available for perinatal depression,78,79 depression is unlikely to be formally diagnosed or treated in settings like Uganda, where mental health services are generally limited.80 In this setting, the Mbarara Regional Referral Hospital has a full-service mental health clinic, where counseling and medical treatment services for depression are available. A persistent challenge, however, is that depression (during or outside of pregnancy) often goes undetected in HIV treatment clinics because of a lack of routine screening and referral processes, time constraints within clinical visits, and the underprioritization of mental health concerns relative to the physical ailments of HIV.6 Given the high rates of depression symptom severity among HIV-infected women initiating ART observed here, the development, testing, and implementation of a short screening instrument and referral process must be prioritized within HIV treatment clinics to connect women with existing treatment and counseling services at the onsite mental health clinic.
Additional opportunities exist to connect women with mental health services available at smaller, community-based health care centers throughout Mbarara District. Short and ultra-short screening instruments are readily available for depression screening during the perinatal period,54,81,82 but it is unclear whether screening is ultimately associated with improved health or mental health outcomes.83 One study from Uganda showed that routine clinical screening for depression among HIV-infected patients by primary care workers or community health workers significantly improved case detection and the proportion of patients receiving antidepressants.84 Task shifting of mental health programming to counselors and integration within HIV services have also been shown to be important for addressing the high burden of depression among people living with HIV.10 To achieve better uptake of such services, however, additional efforts are required to increase care-seeking for depression among HIV-infected women.6 Furthermore, any proposed screening and treatment pathways must be thoroughly tested before being widely implemented.
Limitations
This study has several limitations. First, given quarterly follow-up and self-report of pregnancy and pregnancy outcomes, dates used to compute periods of pregnancy vs. postpartum vs. non–pregnancy-related are estimates and subject to misclassification bias. Such misclassification may have yielded conservative estimates of risk of postpartum depression because such risks may be higher after preterm vs. term births.74 Second, at study enrollment, women reported prevalent pregnancy and whether they had been pregnant in the previous 12 months but did not report dates of pre-enrollment pregnancy or postpartum status. Thus, no women were classified as postpartum at study entry. Given high rates of depression at baseline, including postpartum women with non-pregnant women may have biased our comparisons of baseline depression toward the null. Third, others have validated the use of the HSCL-25 to measure depression symptom severity in pregnancy and have suggested a much lower cut-off to determine probable depression (HSCL > 1.06)59 rather than using the same cut-off across periods. A lower criteria for probable depression identified a higher percentage of women as depressed; however, in sensitivity analyses, there remained no association between depression and pregnancy-related periods of follow-up (data not shown). Fourth, HSCL is a screening tool. Assessing depression in PLWH is complicated by the potential for overlap between somatic symptoms of depression and HIV disease85 as well as somatic symptoms of depression and pregnancy. Depression may also be experienced more somatically in non-western cultures.59,79 Given uncertain cultural and/or linguistic equivalency of HSCL items, future research must be informed by locally validated measures. Finally, our participants are enrolled in an intensive follow-up cohort study and may not be representative of the general population of women living with HIV.
CONCLUSIONS
The lack of association between depression and perinatal periods is an important finding for HIV-infected women considering pregnancy after ART initiation and further support the role of HIV treatment in improving maternal health outcomes. In an HIV-endemic setting with high cultural value of childbearing, sustained access to ART may improve perinatal mental health for women. However, the high prevalence of depression at treatment initiation and continued incidence over a sustained follow-up across pregnancy and non–pregnancy-related periods of follow-up demands prioritization of mental health programming for HIV-infected women to optimize maternal and perinatal health.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank UARTO study participants and the clinical and research teams for their contributions to this study.
Footnotes
Supported by the US National Institutes of Health R21HD069194, R01MH054907, P30AI027763, and U01CA066529; and the Sullivan Family Foundation. L.T.M. received support from K23MH095655, A.C.T. received support from K23MH096620, S.K. received support from a Canadian Institutes of Health Research (CIHR) doctoral research award, C.P. received support from K23MH096651, and D.R.B. received support from K24MH087227.
Preliminary data were presented at the Mbarara University of Science and Technology Annual Dissemination Conference, November, 2013, Mbarara, Uganda; at the fifth semi-annual University of California at San Francisco-East Africa Collaborative Scientific meeting, January, 2014, Kisumu, Kenya; and at the 20th International AIDS conference, July, 2014, Melbourne, Australia.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. [DOI] [PubMed] [Google Scholar]
- 2.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. [DOI] [PubMed] [Google Scholar]
- 3.Ribeiro PS, Jacobsen KH, Mathers CD, et al. Priorities for women's health from the Global Burden of Disease study. Int J Gynaecol Obstet. 2008;102:82–90. [DOI] [PubMed] [Google Scholar]
- 4.Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58:721–728. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095–3105. [DOI] [PubMed] [Google Scholar]
- 6.Collins PY, Holman AR, Freeman MC, et al. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS. 2006;20:1571–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ammassari A, Antinori A, Aloisi MS, et al. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004;45:394–402. [DOI] [PubMed] [Google Scholar]
- 8.Do NT, Phiri K, Bussmann H, et al. Psychosocial factors affecting medication adherence among HIV-1 infected adults receiving combination antiretroviral therapy (cART) in Botswana. AIDS Res Hum Retroviruses. 2010;26:685–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Starace F, Ammassari A, Trotta MP, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31(suppl 3):S136–S139. [DOI] [PubMed] [Google Scholar]
- 10.Mayston R, Kinyanda E, Chishinga N, et al. Mental disorder and the outcome of HIV/AIDS in low-income and middle-income countries: a systematic review. AIDS. 2012;26(suppl 2):S117–S135. [DOI] [PubMed] [Google Scholar]
- 11.Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285:1466–1474. [DOI] [PubMed] [Google Scholar]
- 12.Pence BW, Miller WC, Gaynes BN, et al. Psychiatric illness and virologic response in patients initiating highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2007;44:159–166. [DOI] [PubMed] [Google Scholar]
- 13.Evans DL, Ten Have TR, Douglas SD, et al. Association of depression with viral load, CD8 T lymphocytes, and natural killer cells in women with HIV infection. Am J Psychiatry. 2002;159:1752–1759. [DOI] [PubMed] [Google Scholar]
- 14.Cook JA, Grey D, Burke J, et al. Depressive symptoms and AIDS-related mortality among a multisite cohort of HIV-positive women. Am J Public Health. 2004;94:1133–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brandt R. Putting mental health on the agenda for HIV+ women: a review of evidence from sub-Saharan Africa. Women Health. 2009;49:215–228. [DOI] [PubMed] [Google Scholar]
- 16.Brandt R. The mental health of people living with HIV/AIDS in Africa: a systematic review. Afr J AIDS Res. 2009;8:123–133. [DOI] [PubMed] [Google Scholar]
- 17.Kaharuza FM, Bunnell R, Moss S, et al. Depression and CD4 cell count among persons with HIV infection in Uganda. AIDS Behav. 2006;10(4 suppl):S105–S111. [DOI] [PubMed] [Google Scholar]
- 18.Kinyanda E, Hoskins S, Nakku J, et al. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry. 2011;11:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaida A, Matthews LT, Kanters S, et al. Incidence and predictors of pregnancy among a cohort of HIV-positive women initiating antiretroviral therapy in Mbarara, Uganda. PLoS One. 2013;8:e63411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2013. Geneva, Switzerland: UNAIDS; 2013. [Google Scholar]
- 21.Fisher J, Cabral de Mello M, Patel V, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90:139G–149G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disord. 2010;123:17–29. [DOI] [PubMed] [Google Scholar]
- 23.Kapetanovic S, Dass-Brailsford P, Nora D, et al. Mental health of HIV-seropositive women during pregnancy and postpartum period: a comprehensive literature review. AIDS Behav. 2014;18:1152–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nachega JB, Uthman OA, Anderson J, et al. Adherence to antiretroviral therapy during and after pregnancy in low-income, middle-income, and high-income countries: a systematic review and meta-analysis. AIDS. 2012;26:2039–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahman A, Iqbal Z, Bunn J, et al. Impact of maternal depression on infant nutritional status and illness: a cohort study. Arch Gen Psychiatry. 2004;61:946–952. [DOI] [PubMed] [Google Scholar]
- 26.Kingston D, Tough S, Whitfield H. Prenatal and postpartum maternal psychological distress and infant development: a systematic review. Child Psychiatry Hum Dev. 2012;43:683–714. [DOI] [PubMed] [Google Scholar]
- 27.Weissman MM, Pilowsky DJ, Wickramaratne PJ, et al. Remissions in maternal depression and child psychopathology: a STAR*D-child report. JAMA. 2006;295:1389–1398. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization (WHO). Global HIV/AIDS Response: Epidemic Update and Health Sector Progress Towards Universal Access: Progress Report 2011. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 29.Hogg RS, Heath KV, Yip B, et al. Improved survival among HIV-infected individuals following initiation of antiretroviral therapy. JAMA. 1998;279:450–454. [DOI] [PubMed] [Google Scholar]
- 30.Hogg RS, O'Shaughnessy MV, Gataric N, et al. Decline in deaths from AIDS due to new antiretrovirals. Lancet. 1997;349:1294. [DOI] [PubMed] [Google Scholar]
- 31.Hogg RS, Yip B, Chan KJ, et al. Rates of disease progression by baseline CD4 cell count and viral load after initiating triple-drug therapy. JAMA. 2001;286:2568–2577. [DOI] [PubMed] [Google Scholar]
- 32.Palella FJ, Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–860. [DOI] [PubMed] [Google Scholar]
- 33.Montaner JS, Lima VD, Barrios R, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cooper ER, Charurat M, Mofenson L, et al. Combination antiretroviral strategies for the treatment of pregnant HIV-1-infected women and prevention of perinatal HIV-1 transmission. J Acquir Immune Defic Syndr. 2002;29:484–494. [DOI] [PubMed] [Google Scholar]
- 36.Okeke EN, Wagner GJ. AIDS treatment and mental health: evidence from Uganda. Soc Sci Med. 2013;92:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel R, Kassaye S, Gore-Felton C, et al. Quality of life, psychosocial health, and antiretroviral therapy among HIV-positive women in Zimbabwe. AIDS Care. 2009;21:1517–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wagner GJ, Ghosh-Dastidar B, Garnett J, et al. Impact of HIV antiretroviral therapy on depression and mental health among clients with HIV in Uganda. Psychosom Med. 2012;74:883–890. [DOI] [PubMed] [Google Scholar]
- 39.Martinez P, Tsai AC, Muzoora C, et al. Reversal of the kynurenine pathway of tryptophan catabolism may improve depression in ART-treated HIV-infected Ugandans. J Acquir Immune Defic Syndr. 2014;65:456–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsai AC, Bangsberg DR, Bwana M, et al. How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS Behav. 2013;17:2725–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Uganda Bureau of Statistics (UBOS) and ICF International Inc. Uganda Demographic and Health Survey 2011. Kampalas, Uganda: UBOS and ICF International Inc.; 2012. [Google Scholar]
- 42.Ugandan Ministry of Health. 2011 Uganda AIDS Indicator Survey (UAIS). Kampala, Uganda: Government of Uganda, Ministry of Health; 2012. [Google Scholar]
- 43.Centers for Disease Control and Prevention (CDC). Impact of an innovative approach to prevent mother-to-child transmission of HIV–Malawi, July 2011-September 2012. MMWR Morb Mortal Wkly Rep. 2013;62:148–151. [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization (WHO). Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach (2013). Geneva, Switzerland: World Health Organization (WHO); 2013. [PubMed] [Google Scholar]
- 45.Ministry of Health (Uganda) and ORC Macro. Uganda HIV/AIDS Sero-behavioural Survey 2004–2005. Calverton, MD: Ministry of Health (Uganda) and ORC Macro; 2006. [Google Scholar]
- 46.Geng EH, Bwana MB, Kabakyenga J, et al. Diminishing availability of publicly funded slots for antiretroviral initiation among HIV-infected ART-eligible patients in Uganda. PLoS One. 2010;5:e14098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Derogatis LR, Lipman RS, Rickels K, et al. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1–15. [DOI] [PubMed] [Google Scholar]
- 48.Bolton P, Ndogoni L. Cross-cultural Assessment of Trauma-related Mental Illness (Phase II): A Report of Research Conducted by World Vision Uganda and the Johns Hopkins University. Baltimore, Maryland: US Agency for International Development, The Johns Hopkins University, and World Vision International; 2001. [Google Scholar]
- 49.Martinez P, Andia I, Emenyonu N, et al. Alcohol use, depressive symptoms and the receipt of antiretroviral therapy in southwest Uganda. AIDS Behav. 2008;12:605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Winokur A, Winokur DF, Rickels K, et al. Symptoms of emotional distress in a family planning service: stability over a four-week period. Br J Psychiatry. 1984;144:395–399. [DOI] [PubMed] [Google Scholar]
- 51.Bass JK, Annan J, McIvor Murray S, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. N Engl J Med. 2013;368:2182–2191. [DOI] [PubMed] [Google Scholar]
- 52.Bolton P, Wilk CM, Ndogoni L. Assessment of depression prevalence in rural Uganda using symptom and function criteria. Soc Psychiatry Psychiatr Epidemiol. 2004;39:442–447. [DOI] [PubMed] [Google Scholar]
- 53.Epino HM, Rich ML, Kaigamba F, et al. Reliability and construct validity of three health-related self-report scales in HIV-positive adults in rural Rwanda. AIDS Care. 2012;24:1576–1583. [DOI] [PubMed] [Google Scholar]
- 54.Tsai AC, Scott JA, Hung KJ, et al. Reliability and validity of instruments for assessing perinatal depression in African settings: systematic review and meta-analysis. PLoS One. 2013;8:e82521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tsai AC, Bangsberg DR, Frongillo EA, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74:2012–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tsai AC, Weiser SD, Steward WT, et al. Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS Behav. 2013;17:427–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mahenge B, Likindikoki S, Stockl H, et al. Intimate partner violence during pregnancy and associated mental health symptoms among pregnant women in Tanzania: a cross-sectional study. BJOG. 2013;120:940–946. [DOI] [PubMed] [Google Scholar]
- 58.Lee B, Kaaya SF, Mbwambo JK, et al. Detecting depressive disorder with the Hopkins Symptom Checklist-25 in Tanzania. Int J Soc Psychiatry. 2008;54:7–20. [DOI] [PubMed] [Google Scholar]
- 59.Kaaya SF, Fawzi MC, Mbwambo JK, et al. Validity of the Hopkins Symptom Checklist-25 amongst HIV-positive pregnant women in Tanzania. Acta Psychiatr Scand. 2002;106:9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gavin NI, Gaynes BN, Lohr KN, et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–1083. [DOI] [PubMed] [Google Scholar]
- 61.Born L, Zinga D, Steiner M. Challenges in identifying and diagnosing postpartum disorders. Prim Psychiatry. 2004;11:29–36. [Google Scholar]
- 62.Revicki DA, Sorensen S, Wu AW. Reliability and validity of physical and mental health summary scores from the Medical Outcomes Study HIV Health Survey. Med Care. 1998;36:126–137. [DOI] [PubMed] [Google Scholar]
- 63.Wu AW. MOS-HIV Health Survey Users' Manual. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; 1999. [Google Scholar]
- 64.Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19:716–723. [Google Scholar]
- 65.The SAS Institute. SAS Version 9.3. Cary, NC: The SAS Institute; 2011. [Google Scholar]
- 66.Ovuga E, Boardman J, Wasserman D. The prevalence of depression in two districts of Uganda. Soc Psychiatry Psychiatr Epidemiol. 2005;40:439–445. [DOI] [PubMed] [Google Scholar]
- 67.Nakasujja N, Skolasky RL, Musisi S, et al. Depression symptoms and cognitive function among individuals with advanced HIV infection initiating HAART in Uganda. BMC Psychiatry. 2010;10:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Myer L, Smit J, Roux LL, et al. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDS. 2008;22:147–158. [DOI] [PubMed] [Google Scholar]
- 69.Kakyo TA, Muliira JK, Mbalinda SN, et al. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery. 2012;28:374–379. [DOI] [PubMed] [Google Scholar]
- 70.Nakku JE, Nakasi G, Mirembe F. Postpartum major depression at six weeks in primary health care: prevalence and associated factors. Afr Health Sci. 2006;6:207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chan BT, Weiser SD, Boum Y, et al. Trends in depression among patients presenting for ART in rural Uganda. Conference on Retroviruses and Opportunistic Infections (CROI); March 3–6, 2014; Boston, MA (Abstract No. 1067).
- 72.Townsend CL, Byrne L, Cortina-Borja M, et al. Earlier initiation of ART and further decline in mother-to-child HIV transmission rates, 2000-2011. AIDS. 2014;28:1049–1057. [DOI] [PubMed] [Google Scholar]
- 73.Wanic R, Kulik J. Toward an understanding of gender differences in the impact of marital conflict on health. Sex Roles. 2011;65:297–312. [Google Scholar]
- 74.Robertson E, Grace S, Wallington T, et al. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26:289–295. [DOI] [PubMed] [Google Scholar]
- 75.Hatcher AM, Tsai AC, Kumbakumba E, et al. Sexual relationship power and depression among HIV-infected women in Rural Uganda. PLoS One. 2012;7:e49821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Snow RC, Mutumba M, Resnicow K, et al. The social legacy of AIDS: fertility aspirations among HIV-affected women in Uganda. Am J Public Health. 2013;103:278–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Maier M, Andia I, Emenyonu N, et al. Antiretroviral therapy is associated with increased fertility desire, but not pregnancy or live birth, among HIV+ women in an early HIV treatment program in rural Uganda. AIDS Behav. 2009;13(suppl 1):28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bledsoe SE, Grote NK. Treating depression during pregnancy and the postpartum: a preliminary meta-analysis. Res Soc Work Pract. 2006;16:109–120. [Google Scholar]
- 79.Psaros C, Geller PA, Aaron E. The importance of identifying and treating depression in HIV infected, pregnant women: a review. J Psychosom Obstet Gynaecol. 2009;30:275–281. [DOI] [PubMed] [Google Scholar]
- 80.Kakuma R, Minas H, van Ginneken N, et al. Human resources for mental health care: current situation and strategies for action. Lancet. 2011;378:1654–1663. [DOI] [PubMed] [Google Scholar]
- 81.Rochat TJ, Tomlinson M, Newell ML, et al. Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS). Arch Womens Ment Health. 2013;16:401–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tsai AC, Tomlinson M, Dewing S, et al. Antenatal depression case finding by community health workers in South Africa: feasibility of a mobile phone application. Arch Womens Ment Health. 2014;17:423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kagee A, Tsai AC, Lund C, et al. Screening for common mental disorders in low resource settings: reasons for caution and a way forward. Int Health. 2013;5:11–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Akena D, Stein DJ, Joska J. Does screening HIV-positive individuals in Uganda for major depressive disorder improve case detection rates and antidepressant prescription? AIDS Behav. 2013;17:2802–2807. [DOI] [PubMed] [Google Scholar]
- 85.Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188:662–670. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


