Abstract
Background:
“Option B+” is a World Health Organization-recommended approach to prevent mother-to-child HIV transmission whereby all HIV-positive pregnant and lactating women initiate lifelong antiretroviral therapy (ART). This review of early Option B+ implementation experience is intended to inform Ministries of Health and others involved in implementing Option B+.
Methods:
This implementation science study analyzed data from 11 African countries supported by the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF) to describe early experience implementing Option B+. Data are from 4 sources: (1) national guidelines for prevention of mother-to-child HIV transmission and Option B+ implementation plans, (2) aggregated service delivery data between January 2013 and March 2014 from EGPAF-supported sites, (3) field visits to Option B+ implementation sites, and (4) relevant EGPAF research, quality improvement, and evaluation studies.
Results:
Rapid adoption of Option B+ led to large increases in percentage of HIV-positive pregnant women accessing ART in antenatal care. By the end of 2013, most programs reached at least 50% of HIV-positive women in antenatal care with ART, even in countries using a phased approach to implementation. Scaling up Option B+ through integrating ART in maternal and child health settings has required expansion of the workforce, and task shifting to allow nurse-led ART initiation has created staffing pressure on lower-level cadres for counseling and community follow-up. Complex data collection needs may be impairing data quality.
Discussion:
Early experiences with Option B+ implementation demonstrate promise. Continued program evaluation is needed, as is specific attention to counseling and support around initiation of lifetime ART in the context of pregnancy and lactation.
Key Words: prevention of mother-to-child transmission of HIV, antiretroviral therapy, Option B+, implementation science
INTRODUCTION
The launch of the Global Plan towards the elimination of new infections among children by 2015 and keeping their mother alive1 created strong political support for 2 time-bound targets in 22 focus countries: (1) reducing new HIV infections among children by 90% and (2) reducing AIDS-related maternal deaths by 50%. To reach these targets, programs to prevent mother-to-child HIV transmission (PMTCT) would have to increase coverage, scale-up use of efficacious antiretroviral drug (ARV) regimens, and strengthen retention of women and children within the health care system.
In 2010, the World Health Organization (WHO) recommended 2 PMTCT options for HIV-positive pregnant and breastfeeding women not eligible for lifelong antiretroviral therapy (ART) on clinical or immunologic criteria: (1) Option A prescribed a dual ARV regimen during the mother-to-child transmission risk period (pregnancy through end of breastfeeding) and (2) Option B prescribed ART for all HIV-positive pregnant women for the duration of the transmission risk period.2 In 2011, Malawi introduced Option B+, in which lifelong ART is initiated for all HIV+ pregnant and breastfeeding women regardless of CD4+ cell count or clinical stage.3 WHO issued a Programmatic Update in 2012 recommending that countries consider moving to Option B or B+.4 WHO formalized this recommendation in its 2013 consolidated ARV guidelines, recommending that countries adopt Option B or B+, thereby removing the step of CD4 testing before ART initiation in pregnancy (although not for ongoing monitoring of treatment).5 These guidelines also recommended providing ART in maternal and child health (MCH) settings, allowing easier initiation of ART during pregnancy, delivery, and breastfeeding.
Although there are many potential benefits of Option B+, WHO recognized the limited experience with its implementation. Moreover, the rapid adoption of Option B+ was worrisome to some6 given the lack of validated benefits and anticipated implementation challenges, including the shift of attention and resources required to implement a substantive new recommendation like Option B+. The need for close monitoring of the implementation of Option B+ to rapidly identify implementation issues was emphasized by WHO and others.7
To begin to address this need, the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF) reviewed its experience supporting Ministries of Health (MOH) and other local organizations with implementing Option B+. This review and analysis is intended to inform MOH, their implementing partners, and other stakeholders involved in implementing Option B+.
METHODS
EGPAF is a leading international non-governmental organization dedicated to ending AIDS in children through supporting program implementation, research, and advocacy. EGPAF provides MOH and other local organizations with program implementation support in Cameroon, Cote d'Ivoire, Democratic Republic of Congo, India, Kenya, Lesotho, Malawi, Mozambique, Swaziland, Tanzania, Uganda, Zambia, and Zimbabwe although the nature, programmatic scope, and geographic reach of EGPAF's support varies by country. As of March 2014, EGPAF was providing facility-level support in 6903 health facilities in these countries.
At the national level in most countries where it works, EGPAF staff regularly liaise with MOH counterparts, actively participate in national technical working groups, and provide technical assistance to MOH, including support in adaptation of WHO recommendations to local country contexts. At the district, facility and community levels, EGPAF country teams provide on-site technical assistance; support planning; facilitate trainings and refreshers; support development, printing, distribution, and training on revised monitoring and evaluation tools; and contribute to supportive supervision and mentoring of health workers, as well as other capacity building activities.
Given the varied nature, programmatic scope, and geographic reach of EGPAF's support, we used a variety of data sources to gain insight into Option B+ implementation. Specifically, we used data through March 2014 from 11 countries (for all countries where EGPAF provides implementation support except India and Cote d'Ivoire that have not adopted Option B+) from the following sources:
Review of national PMTCT guidelines and Option B+ implementation plans to understand the rollout model, approach to scaling up Option B+, and factors influencing implementation in each setting.
Analysis of aggregated service delivery data between January 2013 and March 2014 in facilities where EGPAF provides implementation support to assess uptake of Option B+ services and retention of mother–baby pairs in care and treatment services. EGPAF compiles and analyzes such routinely collected aggregated facility-level data that are reported to MOH from the sites it supports. Analysis was limited to descriptive statistics (eg, percentages, comparisons over time, and between groups).
Field visits by EGPAF's global network of Technical Directors to sites implementing Option B+ in Malawi (10 facilities, October 2012), Uganda (Mulago Hospital, March 2013), and Lesotho (12 facilities, October 2013). Using a structured guide, teams reviewed registers, analyzed routine service delivery data available from the MOH, and observed infrastructure, client flow, service provision, data systems, supportive supervision, and community involvement, and recorded these observations.
Review of ongoing or completed EGPAF research, evaluation, and quality improvement (QI) studies that were relevant to Option B+ implementation.
The authors then reviewed and analyzed these data to describe the implementation experience and draw key observations across countries.
RESULTS
National Policy Adaptation and Scale-up of Option B+
All 11 countries in this review adopted Option B+ as national policy. Adaptation of the 2013 WHO PMTCT guidelines for Option B/B+ to the national context was rapid following the trend of rapid adaptation seen for the 2010 WHO PMTCT guidelines,8 with several countries implementing Option B+ even before the formal release of the WHO guidelines in July 2013. Review of implementation plans showed that countries chose models of scale-up to national implementation to fit their context. As shown in Table 1, Malawi and Lesotho opted for a rapid, national scale-up model, whereas Uganda had a national rollout to facilities already offering PMTCT services, but not yet to all facilities offering antenatal care (ANC); all 3 countries have reached 100% coverage of Option B+ in PMTCT facilities. Other countries are using a phased approach based on HIV prevalence and facility capabilities, beginning in facilities already providing ART. The slower pace of Option B+ scale-up to other facilities, especially to lower-level facilities, allows time to strengthen the MCH platform to deliver ART—providing enough qualified staff to manage ART, identifying proper space, strengthening laboratories, and adapting and strengthening supply chain and data management systems. Integrating planning and management of separate programs for ART, PMTCT, and MCH also required time in many countries.9,10
TABLE 1.
Progress Toward Rolling Out of Option B+ in 11 African Countries (Data Source: National Implementation Plans, EGPAF Program Data)
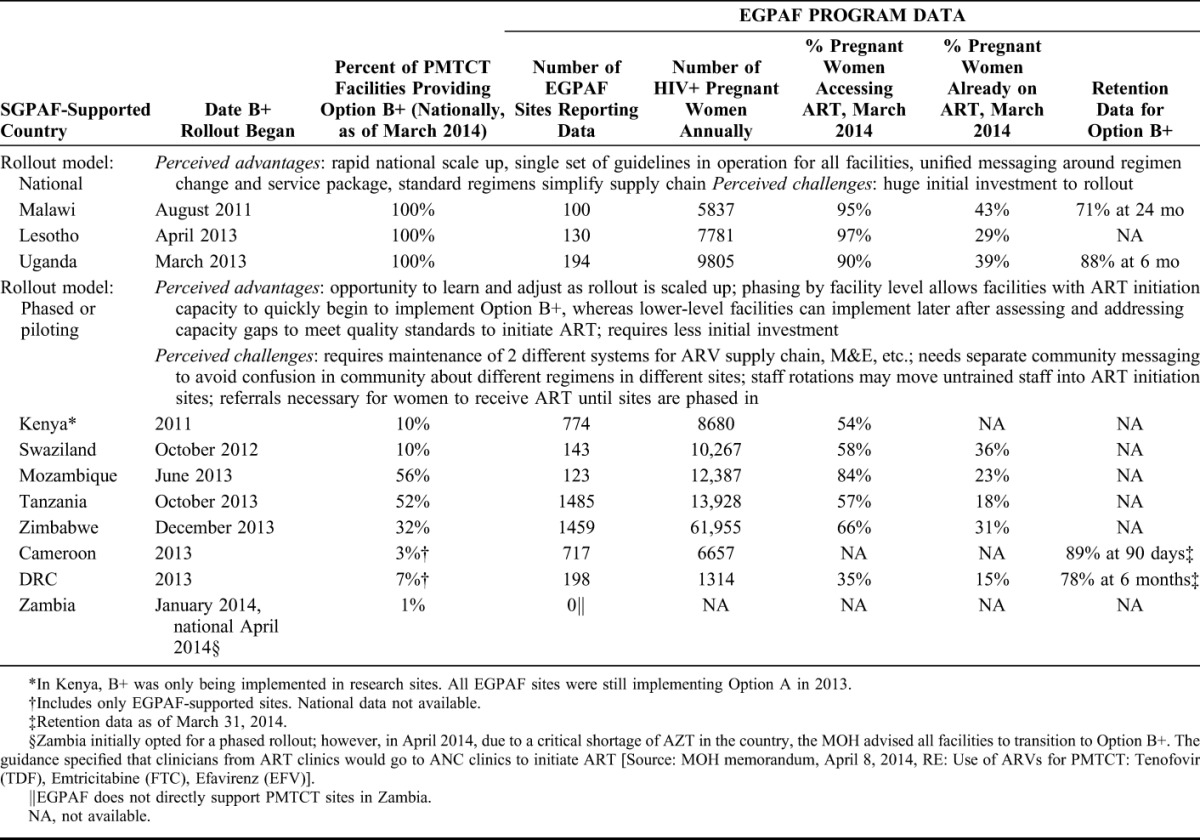
A common feature of the preparation for Option B+ was facility readiness assessments before rollout, using tools adapted from previous in-country tools or from such internationally available tools as the Option B+ Site Readiness Assessment tool (This tool will soon be available at: www.emtct-iatt.org/toolkit).
Rapid Increase in Access to ART for Pregnant Women
In 2012–2013, Lesotho, Uganda, Mozambique, and Tanzania began implementation of Option B+, and large increases were immediately seen in the percentage of pregnant women accessing ART in ANC (Fig. 1). This was particularly striking because the first programs to begin Option B+ were generally the ones with the lowest percentage of HIV+ pregnant women receiving ART. For instance, in the southwestern region of Uganda, the percent of HIV-positive pregnant and lactating women initiating ART rose from 20.5% at the end of 2012 to 89.6% by March 2014. During the same period in the Gaza province of Mozambique, HIV-positive pregnant women in ANC accessing ART increased from 15.2% to 84.7%. By the end of 2013, most EGPAF-supported country programs were reaching at least 50% of HIV-positive pregnant women in ANC with ART, regardless of the roll-out strategy being implemented.
FIGURE 1.
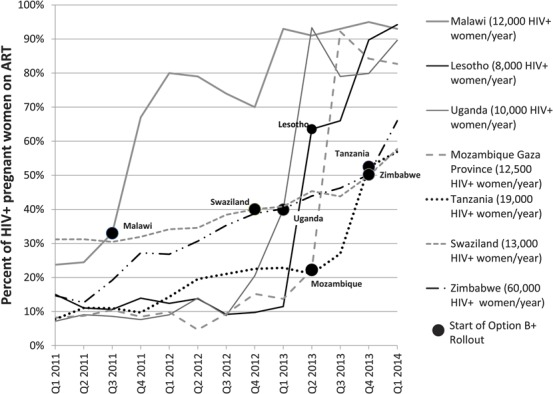
Percent of HIV-positive pregnant women on antiretroviral therapy in ANC in EGPAF-supported facilities, by quarter, 2011–2013 (Source: MOH data for EGPAF-supported sites).
Figure 2 compares women on ART under Option A and Option B+ as of December 2013. With Option B+, the total proportion of HIV+ pregnant women in ANC accessing ART across countries increased to 80%–95%; however, the proportion of pregnant women already on ART at entry into ANC as of December 2013 had stayed at around 30% in most countries. It is likely that this proportion will increase as women receiving Option B+ become pregnant again in the future.
FIGURE 2.
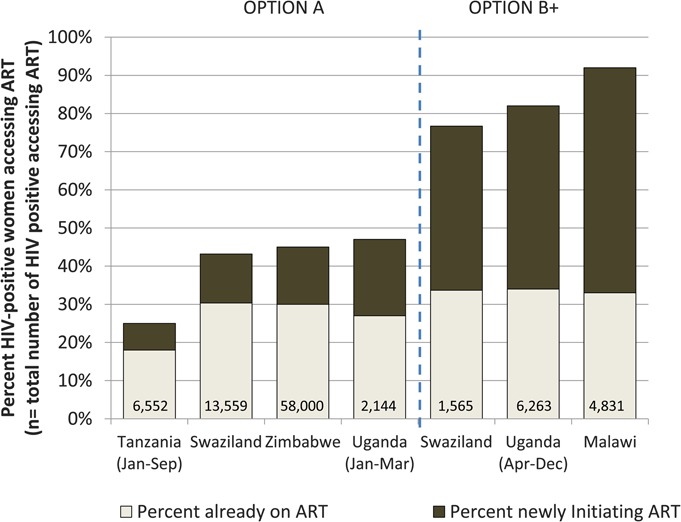
Number and percent of pregnant women already on and initiating antiretroviral therapy under options A and B+, 2013 (Source: MOH data for EGPAF-supported sites).
Meeting Human Resource Demands
Scaling up Option B+ through integrating the delivery of ART in MCH settings has required expansion of the workforce at several levels. For instance, in an evaluation in Malawi, increased facility staff workload was among the major challenges reported.11 To address this, the MOH undertook an extensive effort to train all health care providers implementing PMTCT. Its 120 trainers trained over 4000 health care providers and 359 clinical mentors. To implement Option B+ in Uganda, the MOH recruited more than 8000 additional health care workers (mostly nurses and midwives).12 Uganda used district trainers to roll out Option B+. In general, 8 health care workers were trained per hospital, 5 were trained per Health Center IV, and 2–3 were trained per Health Center III; not all health workers in each facility were trained because of limited funds and the desire for rapid rollout. Each country developed training materials and training plans, and held trainings of varying length. Both Uganda and Zimbabwe teams reported that trainings of 3–5 days were not enough for all nurses in MCH clinics to feel comfortable managing ART. Efforts to strengthen ongoing mentoring to improve skill levels were required to address this gap.
Task shifting to allow nurse-led ART initiation in MCH has created staffing pressure on lower-level cadres for other aspects of care, particularly counseling and community follow-up.13 EGPAF teams reported several strategies to address this. In Malawi, Health Surveillance Assistants were trained to assist with infant follow-up, including dried blood spot sample collection for infants; in Zambia, 600 community health assistants were trained to support Option B+; in Tanzania, a new cadre of MNCH Community Health Workers was introduced to retain mother–baby pairs along the continuum of care14; and in Mozambique, new lay counselors were recruited to assist with client counseling.
Acceptability of Lifelong ART Among HIV-Positive Pregnant Women
Preliminary results of several EGPAF research studies have highlighted the importance of counseling and support provided to pregnant women in increasing their acceptance of lifelong ART. A qualitative study on barriers to ART initiation in Swaziland using focus groups among pregnant women who did and did not accept ART and among health care workers identified crucial factors in acceptance of ART among eligible women.15 Although all women faced similar barriers of stigma and disclosure, distance to the facility, cost of transport, lack of knowledge about ART, and anxiety about lifetime commitment, health care workers who were more skilled in counseling reported that their clients were better able to overcome those barriers and initiate ART. In this same study, pregnant women reported being “scared” and “traumatized” by the seriousness of the commitment to lifelong ART and that acceptance of ARV prophylaxis only was easier. In a Malawi study, women diagnosed with HIV and offered ART initiation on the same day reported feeling overwhelmed with having to cope with the HIV diagnosis, disclosure to their partner or family, and having to initiate lifelong ART.16 Women in both studies who disclosed to their partner or family felt supported to initiate and adhere to ART. In Zimbabwe, to address the issue of women who were unwilling to begin lifelong ART during pregnancy, when the rollout of Option B+ began, the MOH implemented a policy of providing Option B to women who decline lifelong ART, with counseling continuing during pregnancy and breastfeeding.17
In Malawi, after noticing suboptimal early acceptance of Option B+ and believing that community engagement was an important missing element, some health workers conducted outreach on their own to improve knowledge and acceptance in communities and reported that women in these communities had fewer refusals of ART. Community engagement was a notable component in the Option B+ roll-out process in Uganda, Lesotho, Mozambique, and Zambia, including through multimedia campaigns.
Continuity of Care
To reap the benefits of Option B+ for both the mother and the infant, continued retention in care is critical. In Malawi, where the experience with Option B+ implementation is longest, retention data for pregnant women on ART in EGPAF-supported facilities show lower retention for pregnant women than for other adults on ART (Fig. 3). In 149 EGPAF-supported facilities in Uganda, however, retention on ART at 6 months for women initiated on Option B+ during pregnancy was 88%, similar to the 87% seen among other adults. In addition, a subanalysis comparing retention rates for pregnant women initiating ART at facilities with and without family support groups suggested modest added benefit of the groups, with 91% retention at 6 months in facilities with family support groups and 77% in those without.
FIGURE 3.
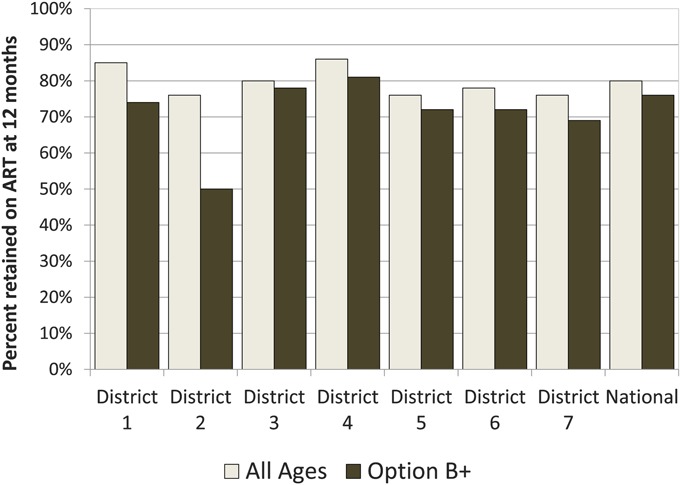
Percent of women alive and on antiretroviral therapy 12 months after initiation, Malawi, September 2013 (Source: MOH data for EGPAF-supported sites).
EGPAF-supported facilities in the 7 countries for which data are available reached 56% of HIV-exposed infants with HIV testing in the first 8 weeks of life; however, there was much variability across settings (Fig. 4). In an effort to improve infant follow-up in Tanzania, a cohort register is being developed for mother–baby care and follow-up. Nzega District of Tanzania implemented several QI innovations to prepare for implementation of Option B+. For example, with the introduction of a new HIV-exposed infant follow-up card and the adoption of the ART card to be used for PMTCT services in ANC, health workers devised the approach of putting the 2 cards together during pregnancy. In these sites, QI data showed that the ratio of the number of HIV-exposed infants registered in care to HIV-positive mothers (1.05) was more than twice the region-wide ratio (0.45). QI efforts in Uganda led to combining the mother and infant client files, increasing retention of the mother–baby pairs at 6 weeks postpartum from 20% to 80% at 1 pilot facility.
FIGURE 4.
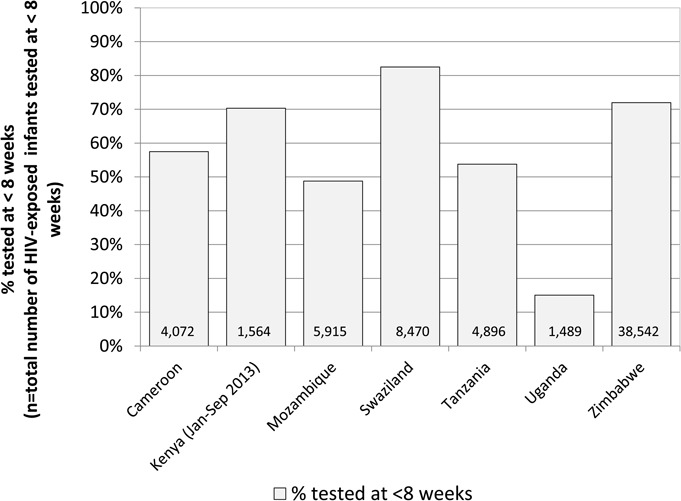
Number and percent HIV-exposed infants tested for HIV by 8 weeks of age, 2013 (Source: MOH data for EGPAF-supported sites).
Data and Monitoring
Longitudinal patient-level tracking of HIV-infected women and their infants is critical for both protection against HIV transmission to the infant and for the mother's health yet is difficult to manage with paper-based longitudinal ANC registers. With the introduction of ART into the MCH settings, several countries, such as Swaziland and Malawi, began using ART clinic files or cards to monitor client retention. Uganda, Zimbabwe, Mozambique, and Lesotho are beginning to add longitudinal electronic data systems to track ART delivery in MCH clinics. Zambia has a national PMTCT module in its “SmartCare” electronic medical record system, and Tanzania is adopting a national electronic care and treatment system for PMTCT.18
With the implementation of Option B+, countries revised many of their national indicators and monitoring and evaluation tools to manage the complex data needs for accurate monitoring. In many countries, it was reported that sites were continuing to use Option A registers and tools because of delays in finalization, printing/distribution, or training on the new Option B+ tools. These gaps made early monitoring of progress very difficult, and it took extensive efforts of health workers to compile facility reports for PMTCT. The additional data demands of Option B+ also have had negative effects on data quality. In a recent Project ACCLAIM data quality audit across Swaziland, Uganda, and Zimbabwe, EGPAF staff traced the documentation of service provision from the client record to the register to the national reporting system (Cathcart R, Kieffer MP, Woelk G, unpublished data, 2013). Although the overall correct reporting of services delivered was generally good (above 90%), it varied substantially by facility and data element. In Uganda, multiple errors were made at health facilities in completing the complex coding for PMTCT in the new registers. At some facilities, correct reporting of critical PMTCT indicators was below 40%. The MOH and the EGPAF team in Uganda are undertaking broad action to improve the tools and reporting processes for PMTCT, including additional training and mentoring of staff, and addressing facility-specific issues regarding client flow and service delivery processes.
Supply Chain Issues
Supply chain issues also affected Option B+ rollout. For instance, in Tanzania and Uganda, the rollout was postponed for 3–6 months awaiting arrival of ARVs in country. Stock-outs of HIV test kits have also affected Option B+ implementation. Malawi had a severe stock-out of test kits in 2012, resulting in a drop in the proportion of women accessing ART (Fig. 1). It was necessary to harmonize separate MCH and ART supply chain systems as part of Zimbabwe's rollout process.10
DISCUSSION
Option B+ represents a substantial change in the approach to PMTCT that holds promise for not only effectively reducing new HIV infections in children, but also improving the health of their mothers. This approach has been endorsed by WHO and is being rapidly implemented in many countries. We took advantage of EGPAF's presence supporting MOH in 11 countries that have adopted Option B+ to analyze their early experience implementing Option B+. This review found that most countries quickly adopted and began scale up of Option B+, some even before the formal WHO guidelines were released. This scale up resulted in substantial increases in percentages of HIV+ pregnant women in ANC who started on ART.
To achieve the promise of Option B+ as a strategy for both prevention and treatment, ART must not only be started early enough in pregnancy to reduce maternal viral load and adhered to throughout the period of transmission risk to the infant, including during labor, delivery, and breastfeeding, but also must be taken consistently and lifelong to maintain viral suppression and avoid the development of antiretroviral resistance. Thus, key imperatives of this approach include rapid identification of HIV infection, rapid initiation on ART, and close adherence to ongoing treatment.
This review adds to other reports of the unique retention challenges to starting this approach during pregnancy,19 and highlights the need for specific counseling, male partner engagement, and community support to be successful. Given the levels of acceptance of lifelong ART by pregnant women, urgent attention is needed to high quality and ongoing counseling and support around the initiation of and adherence to lifetime ART in the context of pregnancy and lactation. It will be important to evaluate new counseling models, such as sequenced counseling messages that first introduce ART as a PMTCT tool to protect the baby during gestation, childbirth, and breastfeeding and then introduce the benefits of lifelong ART and prepare women for long-term adherence and retention.
The importance of ongoing adherence and retention also highlights the need for improved tracking systems to enable the health care system to better support women to address the challenge of adhering to chronic HIV care and to collect the data needed to track this issue at the population level. To do so, it will be necessary to invest in data systems, to develop more sensitive indicators to follow each mother–baby pair through the risk period for MTCT, and to enhance training and mentoring needed to accurately collect, analyze, and interpret such data. Enhanced monitoring tools and systems (eg, electronic databases) hold promise for broad application within health systems because they can provide reliable longitudinal tracking of women and children.
This review, as a form of implementation science,20 has both strengths and weaknesses in its methodology. By compiling data from a number of sources in a variety of countries from an implementer's perspective, clear trends can be observed that have generalizable relevance to implementation. At this early stage of Option B+ implementation, these findings can be disseminated in a timely manner to inform ongoing efforts globally. However, this early review across a broad number of countries and implementing contexts precludes a comprehensive evaluation of any particular country experience, and reliance on heterogeneous data sources from different countries reduces the precision of cross-country comparisons. Moreover, by reporting out only on the early experience with Option B+, important longer-term issues could not be addressed, such as long-term retention in care, the impact on quality of services with widespread task shifting of ART initiation to nurses and decentralization of ART to lower-level health facilities, and transmission rates to infants and partners.
Option B+ holds great promise for improving the lives and health of HIV-infected women and their children, but much more needs to be learned to address its many unknowns. Although this study provides an early snapshot of progress and emerging issues, more comprehensive research will be needed to evaluate different service delivery models, the impact of technical (eg, mHealth) and programmatic (eg, longitudinal and community-based counseling and support strategies) innovations, and the cost-effectiveness of implementing Option B+.21 Moreover, close linkages among researchers, implementers, and policy makers can quickly incorporate the growing experiential evidence base into policy, practice, and system adjustments to optimize the Option B+ approach.
ACKNOWLEDGMENTS
The authors thank Ministries of Health and EGPAF staff for their work expanding access to PMTCT services to support women, children, and their families, and for sharing data used in this article to help to inform the global community. The authors also recognize the following EGPAF staff who supported the development of this article including Christina Scaduto, Nick Hellman, Christian Pitter, Eric Nawar, Alex Angel, and Rebecca Cathcart.
The EGPAF Technical Directors Forum includes: Swaziland: Mary Pat Kieffer (cochair); Caspian Chouraya (cochair); Cameroon: Eveline Khan Mbo; Cote d'Ivoire: Patricia Fassinou/Noba Akouethale Valentin/Natalie Krou Danho; Democratic Republic of Congo: Jo Mushitu; India: Apparna Addala; Kenya: Lucy Matu; Lesotho: Appolinaire Tiam/Felix Ndagije; Malawi: Aida Yemane Berhan/Allan Ahimbisibwe; Mozambique: Alexandre Boon/Esmeralda Karajeanes; Tanzania: Roland van den Ven/Chrispine Kimario; Uganda: Moses Walakira; Zambia: Jack Menke; and Zimbabwe: Esther Tumbare.
Footnotes
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Joint United Nations Programme on HIV/AIDS. Global Plan Towards the Elimination of New HIV Infections Among Children by 2015 and Keeping Their Mothers Alive. Geneva, Switzerland: UNAIDS; 2011. [Google Scholar]
- 2.World Health Organization. Antiretroviral Therapy for HIV Infection in Adults and Adolescents: Recommendations for a Public Health Approach. Geneva, Switzerland: WHO Department of HIV/AIDS; 2010. Revision. [PubMed] [Google Scholar]
- 3.Malawi Ministry of Health. Malawi's Revised Policy for PMTCT and ART. Lilongwe, Malawi: Malawi Ministry of Health; 2010. [Google Scholar]
- 4.World Health Organization. Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants: Programmatic Update. Geneva, Switzerland: WHO Department of HIV/AIDS; 2012. WHO/HIV/2012.6. [Google Scholar]
- 5.World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. Geneva, Switzerland: WHO Department of HIV/AIDS; 2013. [PubMed] [Google Scholar]
- 6.Coutsoudis A, Goga A, Desmond C, et al. Is Option B+ the best choice? Lancet. 2013;381:269–271. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed S, Kim MH, Abrams EJ. Risks and benefits of lifelong antiretroviral treatment for pregnant and breastfeeding women: a review of the evidence for the Option B+ approach. Curr Opin HIV AIDS. 2013;8:474–489. [DOI] [PubMed] [Google Scholar]
- 8.Ghanotakis E, Miller L, Spensley A. Country adaptation of the 2010 World Health Organization: recommendations for the prevention of mother-to-child transmission of HIV. Bull World Health Organ. 2012;90:921–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Implementation of Option B+ for Prevention of Mother-To-Child Transmission of HIV: The Malawi Experience. Brazzaville, Republic of Congo: WHO Regional Office for Africa; 2014. Available at: http://www.zero-hiv.org/wp-content/uploads/2014/04/Implementation-of-Option-B+-for-prevention-of-mother-to-child-transmissi....pdf. Accessed February 21, 2014. [Google Scholar]
- 10.Ministry of Health and Child Care, Zimbabwe. An Operational Plan for the Nationwide Transition to Option B+ in Zimbabwe: September 2013-November 2014. Available at: http://www.nac.org.zw/sites/default/files/MoHCC_OpPlan_081113.pdf. Accessed February 21, 2014. [Google Scholar]
- 11.Yemaneberhan A, Mazzeo C, Smith P, et al. A situational analysis of the facilitators and barriers to integrating ART with MCH services in Malawi. In: International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention; 17–20 July 2011; Rome, Italy. Abstract TUPE473.
- 12.Uganda Ministry of Health. Human Resources for Health Bi-annual Report: Improving HRH Evidence for Decision-making. Kampala, Uganda: Uganda Ministry of Health; 2013. [Google Scholar]
- 13.Dickinson C, Attawell K. Desk review of promising practices to strengthen human resources for health. Report Commissioned by UNAIDS. UNAIDS Discussion Paper; April 2013.
- 14.United Republic of Tanzania Ministry of Health and Social Welfare. National Integrated Community MNCH Guidelines. Dar es Salaam, Tanzania; 2012. [Google Scholar]
- 15.Swaziland Ministry of Health and Elizabeth Glaser Pediatric AIDS Foundation. Barriers to Antiretroviral Therapy Initiation for Eligible HIV-positive Pregnant Women in Antenatal Care. Mbabane, Swaziland; 2012. [Google Scholar]
- 16.Katirayi L, Namadingo H, Bobrow E, et al. Acceptability of lifelong treatment (Option B+) among HIV-positive pregnant and lactating women in Selected sites in Malawi. In: International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention; 20–25 July 2014. Melbourne, Australia. Abstract A-641-0287-09318.
- 17.National Medicine and Therapeutics Policy Advisory Committee (NMTPAC) and The AIDS and TB Directorate, Ministry of Health and Child Care, Zimbabwe. Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe. Harare, Zimbabwe; 2013. [Google Scholar]
- 18.United Republic of Tanzania Ministry of Health and Social Welfare. National Guidelines for Comprehensive Care Services for Prevention of Mother-to-child Transmission of HIV and Keeping Mothers Alive. Dar es Salaam, Tanzania; 2013. [Google Scholar]
- 19.Tenthani L, Haas A, Tweya H, et al. Retention in care under universal antiretroviral therapy for HIV-infected pregnant and breastfeeding women (“Option B+”) in Malawi. AIDS. 2014;28:589–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frequently Asked Questions about Implementation Science. Fogarty International Center. National Institutes of Health; May 2013. http://www.fic.nih.gov/News/Events/implementation-science/Pages/faqs.aspx. Accessed on August 14, 2014. [Google Scholar]
- 21.Fasawe O, Avila C, Shaffer N, et al. Cost-effectiveness analysis of option B+ for HIV prevention and treatment of mothers and children in Malawi. PloS One. 2013;8:e57778. [DOI] [PMC free article] [PubMed] [Google Scholar]


