Supplemental Digital Content is Available in the Text.
Key Words: HIV/AIDS, disclosure, stigma, PMTCT, maternal health, Kenya
Abstract
Background:
In sub-Saharan Africa, women's disclosure of HIV-positive status to others may affect their use of services for prevention of mother-to-child transmission of HIV (PMTCT) of HIV and maternal and child health—including antenatal care, antiretroviral drugs (ARVs) for PMTCT, and skilled birth attendance.
Methods:
Using data from the Migori and AIDS Stigma Study conducted in rural Nyanza Province, Kenya, we compared the use of PMTCT and maternal health services for all women by HIV status and disclosure category (n = 390). Among HIV-infected women (n = 145), associations between disclosure of HIV-positive status and the use of services were further examined with bivariate and multivariate logistic regression analyses.
Results:
Women living with HIV who had not disclosed to anyone had the lowest levels of maternity and PMTCT service utilization. For example, only 21% of these women gave birth in a health facility, compared with 35% of HIV-negative women and 49% of HIV-positive women who had disclosed (P < 0.001). Among HIV-positive women, the effect of disclosure to anyone on ARV drug use [odds ratio (OR) = 5.8; 95% confidence interval (CI): 1.9 to 17.8] and facility birth (OR = 2.9; 95% CI: 1.4 to 5.7) remained large and significant after adjusting for confounders. Disclosure to a male partner had a particularly strong effect on the use of ARVs for PMTCT (OR = 7.9; 95% CI: 3.7 to 17.1).
Conclusions:
HIV-positive status disclosure seems to be a complex yet critical factor for the use of PMTCT and maternal health services in this setting. The design of interventions to promote such disclosure must recognize the impact of HIV-related stigma on disclosure decisions and protect women's rights, autonomy, and safety.
INTRODUCTION
Considerable advances have been made in global maternal and child health over the last few decades. In sub-Saharan Africa, however, death and disability for childbearing women and children remain exceptionally high. This region accounts for an estimated 62% of global burden of maternal mortality1 and 50% of deaths in children younger than 5 years.2 In addition to common causes of maternal mortality such as postpartum hemorrhage and preeclampsia, HIV infection contributes significantly to maternal mortality; women living with HIV during pregnancy or postpartum are 8 times more likely to die than women who are HIV negative.3,4 Ninety-one percent of global HIV-related maternal mortality occurs in sub-Saharan Africa,1 where estimates of maternal deaths attributable to HIV range from 4% to 25%.1,3 This region also accounts for 90% of global mother-to-child transmission of HIV,5 which is responsible for the majority of this infection in children.6
Services for prevention of mother-to-child transmission of HIV (PMTCT) and for maternal health can drastically reduce the incidence of adverse outcomes for women and children. PMTCT services, including the use of antiretroviral drugs (ARVs) during and after pregnancy, can improve survival of HIV-infected childbearing women7 and bring the rate of newborn infection to as low as 1%–2%.8,9 A critical component of both PMTCT and maternal health services is antenatal care (ANC), which includes HIV testing and counseling, pregnancy screening and monitoring, and treatment of complications. ANC also links women to other HIV, PMTCT, and maternal and child health services, including institutional delivery. Skilled care at birth has been associated with substantial declines in maternal mortality,10,11 as well as with enhancing effectiveness of PMTCT interventions that take place around the time of the birth.12–15 Often referred to as “skilled birth attendance,” this care is provided by a trained health worker proficient in midwifery skills (such as a midwife, nurse, or doctor) in a supportive environment (typically a primary or referral level health facility).16
Although these services are important, access to them can be extremely difficult in sub-Saharan Africa, where social and material inequalities are repeatedly shown to have strong effects on women's use of PMTCT and maternal health interventions. In this region, use of ANC and skilled birth attendance are influenced by factors such as age, parity, education, wealth, geographical proximity to care, women's autonomy, and personal interactions with health workers.17–20 A similar cluster of sociodemographic, sociocultural, and health system factors has been shown to affect HIV-positive women's use of PMTCT services.13,21–25
In such contexts, the effect of women's HIV-positive status disclosure on care-seeking behavior during pregnancy and postpartum remains incompletely understood. Decisions about whether to disclose HIV-positive status are often influenced by anticipations and experiences of HIV-related stigma, as evidenced by studies documenting women's fears of violence, abandonment, and loss of economic support as a result of this disclosure.26–30 Disclosure rates to a male sexual partner in sub-Saharan Africa range from 17% to 86%, and tend to be lower for women who test for HIV in ANC settings.27 Lack of disclosure to male partners can limit women's ability to receive HIV care for their own health, increase the risk for sexual transmission of HIV if the male partner is serostatus negative, and increase the likelihood of suboptimal adherence to PMTCT interventions.31,32 Disclosure to and involvement of a male partner in HIV testing have been associated with higher adherence to PMTCT interventions15,22,27,32–35 and improved infant outcomes.36 However, most studies to date have not examined the effects of disclosure to persons other than male partners, nor have they considered the impacts on use of maternal health services.
In this study, we explore the influence of HIV-positive status disclosure on women's use of essential PMTCT and maternal health services, hypothesizing that disclosure will be positively associated with service use. Specifically, we examine the effects of disclosure to different categories of persons (anyone, male partner, family, and other persons) on the use of ANC, ARVs for PMTCT, and skilled birth attendance, while controlling for established determinants of service use. Data were collected as part of the Maternity in Migori and AIDS Stigma (MAMAS) Study conducted from November 2007 to April 2009 in rural Nyanza Province, Kenya—an extremely low-resource setting where about 1 in 5 pregnant women is HIV positive,37 and HIV infection has been estimated to account for as much as 20% of maternal mortality.38
METHODS
Study Setting and Participants
The MAMAS Study was a longitudinal investigation of pregnant women attending rural antenatal clinics, with the aim of examining the effects of HIV-related stigma on use of maternal and PMTCT health services. Study recruitment occurred at 9 government facilities (4 subdistrict hospitals and 5 health centers or dispensaries) supported by Family AIDS Care and Education Services, a program funded by the President's Emergency Plan for AIDS Relief. Women were invited to participate in the baseline questionnaire if they were: 18 years or older, less than 29 weeks pregnant, attending their first ANC clinic visit, and unaware of their HIV status (ie, never tested or tested negative over 3 months ago). A total of 1777 women participated in the antenatal baseline questionnaire.30
Before the initial ANC visit, a trained study interviewer administered the baseline questionnaire in the participant's preferred language. Women were subsequently offered voluntary HIV counseling and rapid testing as part of the ANC visit, followed by posttest counseling and PMTCT services for those testing positive per Kenyan national guidelines.39 Information on women's acceptance of HIV testing and HIV serostatus were abstracted from medical records and contact information for potential follow-up was obtained.
Women selected for follow-up included all who tested HIV-positive (n = 226), all who were not tested for HIV at the first ANC visit (n = 145, including 94 women who refused testing), and a random sample who tested HIV-negative, roughly equal to the number of women who tested positive (n = 227). Among the total group (n = 598), 69% participated in a follow-up questionnaire 4–8 weeks after birth, administered by a trained interviewer either at the participant's home or at a health facility. On most sociodemographic and other characteristics examined, the women who completed this follow-up interview (n = 411) did not differ significantly from those who were lost to follow-up (n = 187).40 Of the women participating in the follow-up interview, 7 (1.7%) were excluded from the current analyses because they had experienced a miscarriage before 20 weeks of gestation, and 14 (3.4%) were only included in descriptive and bivariate analyses because they were missing data on disclosure. Thus, the study primarily used data from a total of 390 women, focusing on the 145 women with disclosure data who tested HIV-positive at baseline (n = 131) or reported subsequent HIV-positive testing (n = 14).
This study received ethical approval from the Kenya Medical Research Institute (KEMRI) Ethical Review Committee, the University of California, San Francisco Committee on Human Research, and the University of Alabama at Birmingham's Institutional Review Board. All women provided signed informed consent for participation in the questionnaires and abstraction of data from their medical records.
Measures
Use of PMTCT and Maternal Health Services
Study outcomes included women's use of ANC services, ARVs during pregnancy, and skilled birth attendance. In accordance with recommendations of the World Health Organization for focused ANC,41 we constructed a binary variable for having 4 or more ANC visits vs. having fewer visits. A binary variable was also created for having used ARVs during pregnancy, defined as whether a woman reported using these drugs for PMTCT or not (detailed information on adherence was not available). Finally, we created a binary variable for birth in a health facility vs. outside a health facility. Because skilled birth attendants do not assist births outside health facilities in this part of Kenya, we considered facility birth equivalent to skilled birth attendance. Each of these variables was based on women's self-reports on the postpartum questionnaire.
HIV-Positive Status Disclosure
The independent variables of interest included binary constructs for HIV-positive status disclosure to anyone (including male partner, immediate family members, and other persons; excluding health workers), disclosure to a male sexual partner, disclosure to an immediate family member (on the woman's side or on her male partner's side), and disclosure to other persons (friends, more distant relatives, and other members of the community). In addition, we created a 3-level categorical variable that was dummy coded as: (1) women who disclosed to no one, (2) women who disclosed to their male partner nonexclusively (ie, disclosure to male partner regardless of whomever else was disclosed to), and (3) women who disclosed to anyone other than their male partner (family and/or others only). Disclosure status was assessed at the postpartum interview, and the question used did not distinguish between intentional or accidental disclosure (“Who knows about your HIV-positive status?”).
Potential Confounders
Other factors that could influence the use of PMTCT and maternal health services were selected for their theoretical importance and significance in the literature. Sociodemographic factors measured at baseline included age, parity, marital status, education, and women's occupation. Age was not included in the final regression analyses because of its lack of significance in previous models and our desire to maintain parsimony given the small sample size. Parity was retained in the final analyses because we considered this variable to more directly reflect pregnancy and childbirth experience than age, and thus be more relevant for examining behaviors during these events. Occupation was used to indicate women's personal wealth and autonomy; specific categories were based on information from the study setting and included housework, farm or agricultural work, and other work outside the home (market sales, manual labor, etc). Baseline anticipations of HIV-related stigma (during pregnancy, before HIV testing) were measured with a 9-item scale initially developed and tested in a study in Botswana.30,42
Health care-related factors were measured postpartum and consisted of travel time from the woman's home to the nearest health facility (less than 1 hour vs. 1 hour or longer), the total number of ANC visits completed (3 or less vs. 4 or more), and having discussed plans for the birth with a male partner (Yes/No). As an independent variable, use of ANC indicated ties to the health care system in predicting use of ARVs and facility birth. Whether a woman discussed a birth plan with her male partner (Yes/No) was considered to signal involvement of the male partner in decision making for intrapartum care.
Analysis
We initially examined use of the selected outcome services among all women in the follow-up sample, comparing the following categories using the χ2 test: (1) HIV status negative or unknown, (2) HIV-positive disclosed (to anyone), and (3) HIV-positive undisclosed (had not disclosed to anyone). Given that there were no significant differences for these outcomes between women who tested HIV-negative and those whose HIV status was unknown, we combined these women into a single group. Among HIV-positive women, we first performed χ2 tests to examine differences between women who reported using the services with those who did not. Bivariate logistic regression analyses were then used to investigate associations of different HIV-positive status disclosure categories (anyone, male partner, family, others) with the use of ANC, ARVs, and birth in a health facility. Finally, multiple logistic regression models were estimated to examine the independent effects of different types of disclosure on each outcome, controlling for the potential confounders described above. To correct for any intracluster correlation, we used clustered robust estimates of variance with clinic as the primary sampling unit. All analyses were performed using Stata 12 statistical software package.43
RESULTS
Use of Services by HIV Serostatus and Disclosure to Anyone
Figure 1 gives the results for use of ANC visits, facility birth, and ARVs for PMTCT by HIV and disclosure status in the follow-up sample. The rate of birth in a health facility was similar when the 2 HIV status groups were compared: 35% of the women with an HIV-negative/unknown status (n = 245) and 34% of women who tested HIV-positive (n = 145) gave birth in a health facility. However, separating HIV-positive women into groups based on disclosure status revealed important differences. Birth in a facility was highest among HIV-positive women who had disclosed their HIV status to anyone (49%), followed by those with a negative/unknown HIV status (35%), whereas a much lower rate was observed among HIV-positive women who had not disclosed their status to anyone (21%) (P < 0.001). For ANC use, 51% of HIV-positive women who had disclosed their status and 47% of HIV-negative women had 4 or more ANC visits, compared with only 32% of HIV-positive women who had not disclosed (P = 0.03). Among HIV-positive women, 88% of those who had disclosed their status reported using ARVs for PMTCT, compared with 56% of those who had not disclosed (P = 0.002).
FIGURE 1.

Proportion of women with ≥4 ANC visits, facility birth, and use of ARVs for PMTCT by HIV and disclosure status (n = 390).
Use of Services by Different Types of HIV-Positive Status Disclosure
Table 1 presents descriptive statistics for all HIV-positive women in the total sample (n = 159), as well as bivariate analyses for use of PMTCT and maternal health services. Most women in the sample were 21–30 year-old, married, had experienced a previous birth, and had finished primary school. Of the 20 unmarried women, 16 reported that they were not currently living with a male partner. Among all women, 42% engaged in farming and 40% worked outside the home in another capacity. The women were almost evenly split on whether it took less than an hour or longer to reach the nearest health facility. Only 41% completed 4 ANC visits or more, but a majority (67%) discussed a birth plan with their male partner.
TABLE 1.
Characteristics of HIV-Positive Women by Use of PMTCT and Maternal Health Services (n = 159)
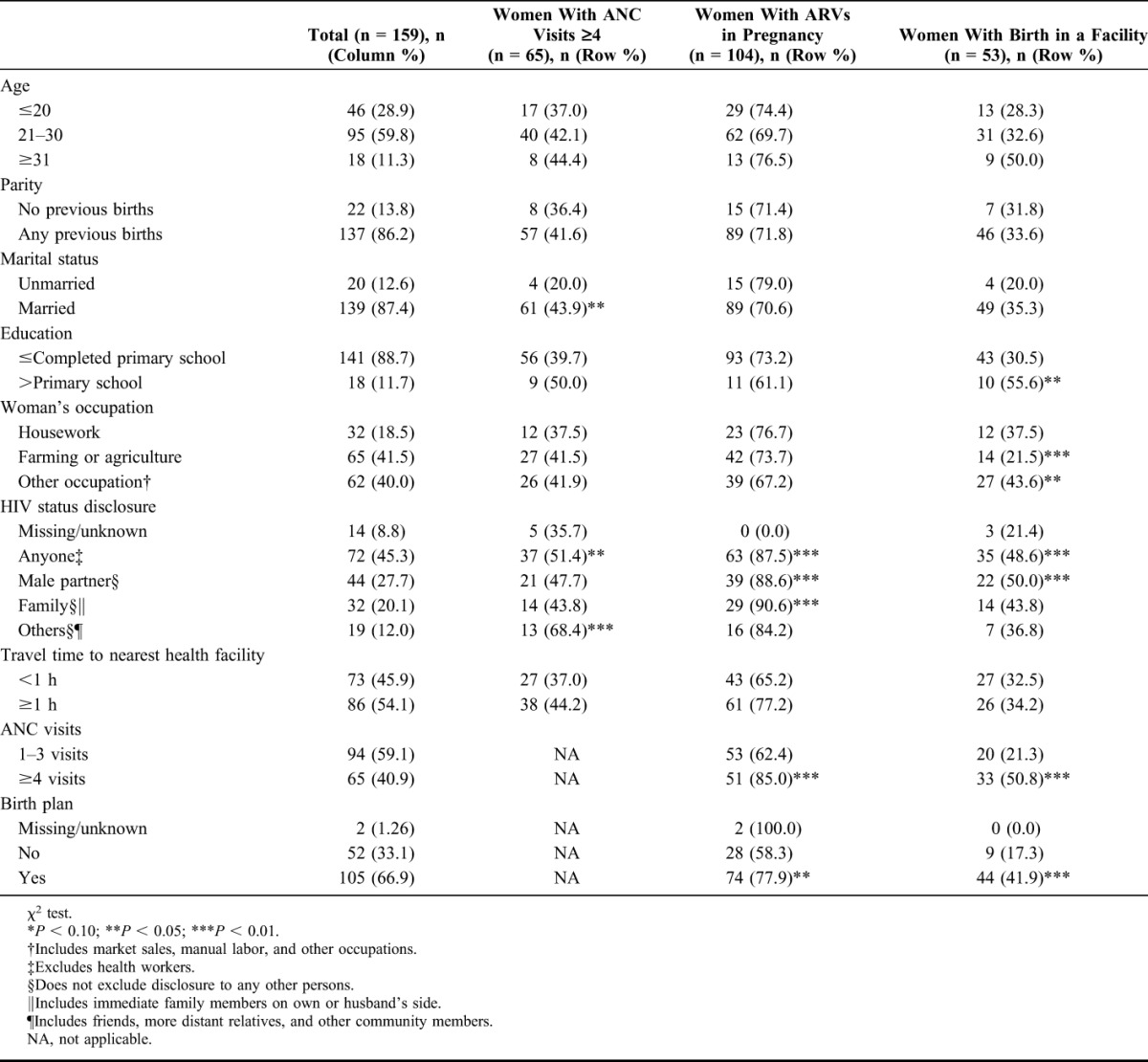
Regarding HIV-positive status disclosure, 45% (n = 72) of women reported having disclosed to anyone, with 28% (n = 44) disclosing nonexclusively to a male partner, 20% (n = 32) to a family member, and 12% (n = 19) to another person. The χ2 results in Table 1 indicate that these disclosure variables tended toward association with use of the selected health services. Descriptive statistics for the 3-level disclosure variable described in the Methods section (among the 145 women who had disclosure data) are as follows: 50% (n = 73) disclosed to no one, 30% (n = 44) disclosed nonexclusively to a male partner, and 19% (n = 28) disclosed to anyone other than a male partner (family and/or others). Additional descriptive statistics for exclusive disclosure and for other combinations of disclosure to different categories of persons can be found in Table S1 (see Supplemental Digital Content, http://links.lww.com/QAI/A578).
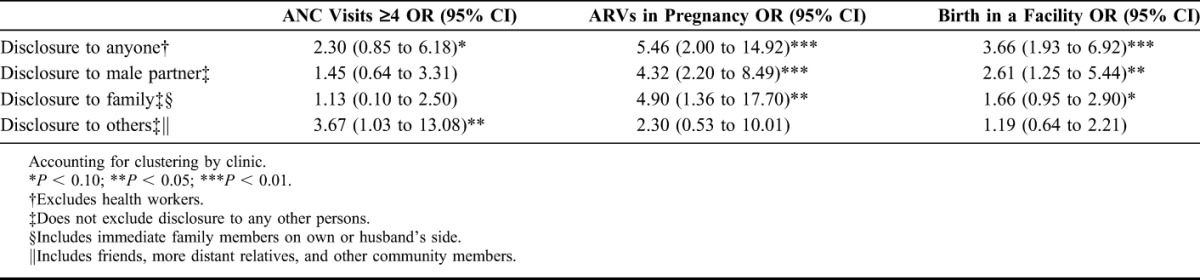
Bivariate logistic regression analyses revealed significant relationships between the different disclosure types and use of services, as shown in Table 2. Compared with women who had not disclosed their HIV-positive status to anyone, women who had disclosed to anyone were more than 5 times as likely to use ARVs during pregnancy (P < 0.01), almost 4 times as likely to give birth in a health facility (P < 0.01), and tended to have greater odds of completing at least 4 ANC visits (P < 0.10). Nonexclusive disclosure to a male partner was significantly associated with both ARV use and birth in a health facility, whereas nonexclusive disclosure to a family member was associated with use of ARVs. In contrast, nonexclusive disclosure to others was significantly associated with having completed 4 or more ANC visits, but not with the other outcomes. Although significant correlations were found between anticipated HIV-related stigma and subsequent disclosure, this variable was not associated with any of our service use outcomes (data not shown).
TABLE 2.
Bivariate Logistic Regression Results for HIV Status Disclosure Type and Use of Maternity and PMTCT Services Among HIV-Positive Women (n = 145)
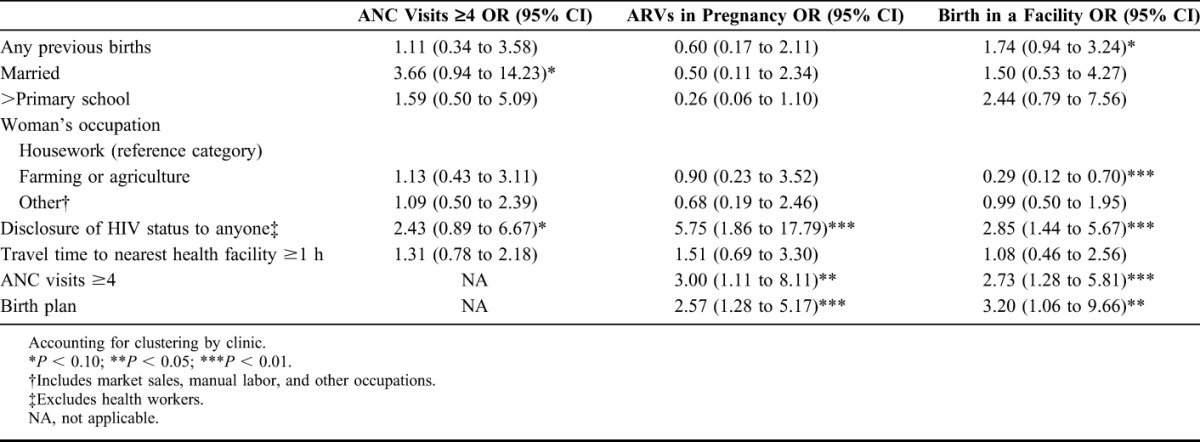
Results of the multiple regression models for disclosure to anyone are presented in Table 3. Disclosure to anyone retained its strong associations with use of ARVs and facility birth in these analyses: women who had disclosed to anyone still had 5.8 [95% confidence interval (CI): 1.9 to 17.8] higher odds of using ARVs, and 2.9 (95% CI: 1.4 to 5.7) higher odds of giving birth in a health facility. Again, disclosure to anyone tended to be associated with having completed 4 or more ANC visits, but not to a significant degree. Other factors in these models that were strongly related to the service outcomes included farm work (facility birth), having 4 or more ANC visits (ARV use and facility birth), and having discussed plans for the birth with a male partner (ARV use and facility birth).
TABLE 3.
Multiple Logistic Regression Results for Disclosure to Anyone and Use of PMTCT and Maternal Health Services Among HIV-Positive Women (n = 145)
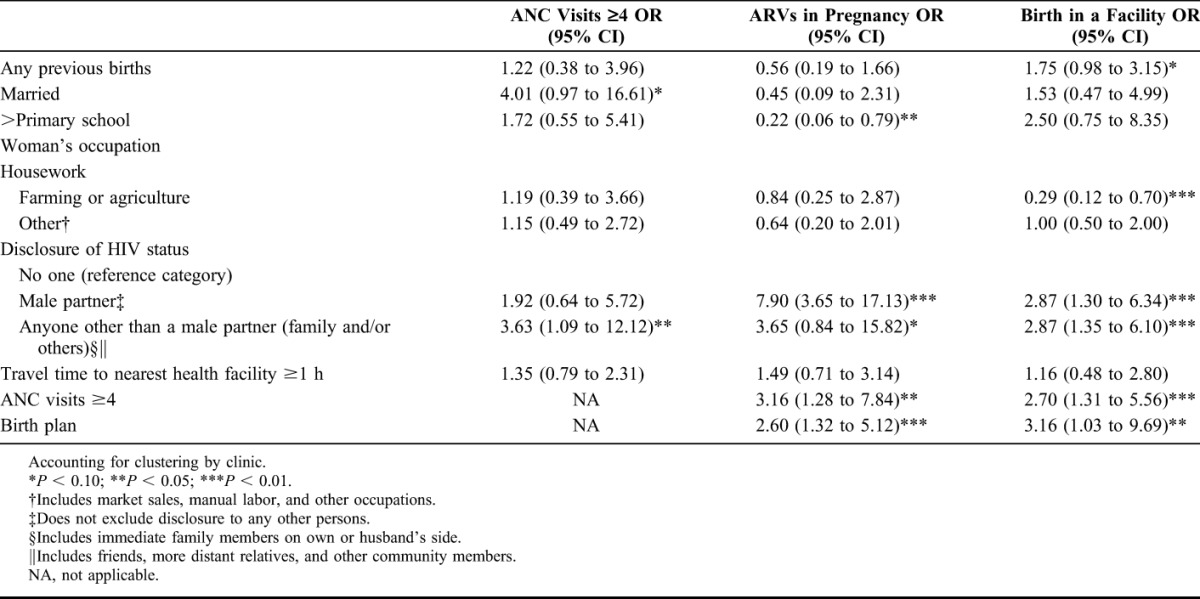
To examine the relative impact of different disclosure types on use of services, we estimated multiple regression models including the variables for nonexclusive disclosure to a male partner and disclosure to anyone other than a male partner (family and/or others), vs. disclosure to no one. These results are shown in Table 4. As compared with those who had not disclosed their HIV-positive status to anyone, women who had disclosed their status to a male partner had 7.9 (95% CI: 3.7 to 17.1) higher odds of using ARVs for PMTCT. Women who had disclosed their status to family and/or others only had a 3.6 (95% CI: 1.1 to 12.1) higher likelihood of completing 4 or more ANC visits. Both disclosure to male partner and disclosure to family and/or others were significant predictors for facility birth [odds ratio (OR) = 2.9, 95% CI: 1.3 to 6.3; OR = 2.9, 95% CI: 1.4 to 6.1, respectively].
TABLE 4.
Multiple Logistic Regression Results for Different Types of Disclosure and Use of PMTCT and Maternal Health Services Among HIV-Positive Women (n = 145)
DISCUSSION
In this high HIV-prevalence setting in sub-Saharan Africa, our findings indicate that disclosure of HIV-positive status is an important factor for use of PMTCT and maternal health services. HIV-positive women who had not disclosed their status had the lowest use of ARVs and facility birth. HIV-positive women who had disclosed their status (to anyone) had the highest use of services—higher even than that of HIV-negative/unknown women in the same communities. Closer examination revealed significant associations between HIV-positive status disclosure and service use. Although disclosure to anyone was more or less relevant for use of all services, bivariate results indicated that different disclosure types influenced service use in different ways: disclosure to male partner was associated with both ARV use and facility birth, disclosure to family was associated with ARV use, and disclosure to other persons was associated with completion of 4 or more ANC visits.
Controlling for potential confounders, multivariate analysis of disclosure to anyone demonstrated similar associations and trends. In the multivariate models examining the effects of different disclosure types, disclosure to male partner was significant for use of ARVs, disclosure to family and/or others was significant for use of ANC, and both disclosure to a male partner and to family and/or others were important for facility birth. Gender norms and distance in social relationships may partially account for these findings, as disclosure to male partner may be particularly salient for services requiring more social and economic resources, but less relevant for accessing routine care such as ANC. The effect of disclosure to other relations on completing 4 or more ANC visits suggests a positive impact from this source of social support, whereas the lack of effect for a male partner may signify the lack of male participation in ANC that is typical in this setting. Except for the weak showing of travel time to nearest health facility, the potential confounders yielded expected results. Especially notable are the consistently strong effects of both adequate ANC visits and male partner involvement in a birth plan on use of ARVs and facility birth.
Limitations of these analyses include the relatively small sample size of HIV-positive women and the resulting need for parsimony in the multiple regression models. Complex wealth measures were not captured in this study, and simple indicators such as individual household assets were not included because of lack of significance in preliminary analyses and because these measures may not accurately reflect woman's access to material resources for their own purposes. However, the occupation variable may have served as an indirect measure of household wealth, because women working in agriculture tend to live in less well-off households than those in which women work only at home or have other occupations. Other potential determinants not present in these analyses include measures of personal motivation and psychosocial support (beyond male partner involvement in a birth plan) that could influence both HIV-positive status disclosure and use of services.
Our previous findings suggest that women's fears and experiences of HIV-related stigma may be driving decisions to not disclose HIV-positive status and resultant avoidance of health services. In agreement with other studies of HIV-related stigma and use of PMTCT and maternal health interventions,44 prospective data from the MAMAS Study revealed that among all women, those with higher baseline perceptions of stigma were subsequently less likely to accept HIV testing30 and to give birth in a health facility40 than those with lower perceptions of stigma. With respect to facility birth, however, further analyses showed that these perceptions were more influential for HIV-negative women than for HIV-positive women. Regarding the correlation between stigma and disclosure, recent results from a study in Uganda indicate that the effect of HIV-related stigma may be more inhibiting for disclosure to more distal relations (community leaders, neighbors, strangers) than to closer relations (male sexual partners, family members, friends).45 Findings such as these suggest that further research is needed to unravel the complicated relationships between HIV-related stigma, disclosure, and use of PMTCT and maternal health services.
In contexts with high levels of HIV-related stigma and discrimination, HIV-positive status disclosure is a complex and sensitive issue. Such disclosure seems to have a strong and positive effect on women's use of lifesaving health services—possibly through allowing women to gain the support of close relations in accessing needed services and in reducing the negative impact of HIV-related stigma. Disclosure of positive HIV status may become even more critical for adherence to PMTCT programs as more countries opt to provide lifelong antiretroviral therapy to pregnant and breastfeeding women regardless of CD4 count.46 Whatever specific strategy is used, disclosure assistance should take into account women's social and economic needs as well as medical needs,47,48 and must be designed in a manner that protects women's rights, autonomy, and safety. Better understanding of HIV-related stigma, HIV status disclosure, and the impacts of these social processes on women's health care seeking could prove essential for more effective prevention of HIV transmission and for improving maternal and child health outcomes in sub-Saharan Africa.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank all of the Kenyan women who participated in the MAMAS Study and shared their experiences with us. They acknowledge the important logistical support of the KEMRI-UCSF Collaborative Group and especially Family AIDS Care and Education Services. They also gratefully acknowledge the Director of KEMRI, the Director of KEMRI's Centre for Microbiology, and the Nyanza Provincial Ministries of Health for their invaluable support in conducting this research.
Footnotes
Supported by the US National Institute of Mental Health, Award Number K01MH081777.
Presented at the 140th APHA Annual Meeting, October 27–31, 2012, San Francisco, CA, and 6th IAS Conference on HIV Pathogenesis, Treatment, and Prevention, July 17–20, 2011, Rome, Italy.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
REFERENCES
- 1.WHO, UNICEF, UNFPA, The World Bank, The United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 2.UN Inter-agency Group for Child Mortality Estimation. Levels & Trends in Child Mortality: Report 2013. New York, NY: UNICEF; 2013. [Google Scholar]
- 3.Calvert C, Ronsmans C. The contribution of HIV to pregnancy-related mortality: a systemic review and meta-analysis. AIDS. 2012;27:1631–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zaba B, Calvert C, Marston M, et al. Effect of HIV infection on pregnancy-related mortality in sub-Saharan Africa: secondary analysis of pooled community-based data from the network for Analyzing Longitudinal Population-based HIV/AIDS data on Africa (ALPHA). Lancet. 2013;381:1763–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UNAIDS. UNAIDS World AIDS Day Report. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 6.UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2013. Geneva, Switzerland: WHO; 2013. [Google Scholar]
- 7.Liotta G, Mancinelli S, Nielsen-Saines K, et al. Reduction of maternal mortality with highly active antiretroviral therapy in a large cohort of HIV-infected pregnant women in Malawi and Mozambique. PLoS One. 2013;8:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lehman DA, John-Stewart GC, Overbaugh J. Antiretroviral strategies to prevent mother-to-child transmission of HIV: striking a balance between efficacy, feasibility, and resistance. PLoS Med. 2009;6:e1000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mofenson LM. Protecting the next generation—eliminating perinatal HIV-1 infection. N Engl J Med. 2010;362:2316–2318. [DOI] [PubMed] [Google Scholar]
- 10.Graham WJ, Bell JS, Bullough CH. Can skilled attendance at delivery reduce mortality in developing countries? In: De Brouwere V, Van Lerberghe W, eds. Safe Motherhood Strategies: A Review of the Evidence. Vol. 17 Antwerp, Belgium: ITG Press; 2001:97–129. [Google Scholar]
- 11.Paxton A, Maine D, Freedman L, et al. The evidence for emergency obstetric care. Int J Gynaecol Obstet. 2005;88:181–193. [DOI] [PubMed] [Google Scholar]
- 12.Albrecht S, Semrau K, Kasonde P, et al. Predictors of nonadherence to single-dose nevirapine therapy for the prevention of mother-to-child HIV transmission. J Acquir Immune Defic Syndr. 2006;41:114–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kinuthia J, Kiarie JN, Farquhar C, et al. Uptake of prevention of mother to child transmission interventions in Kenya: health systems are more influential than stigma. J Int AIDS Soc. 2011;14:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ndirangu J, Newell ML, Tanser F, et al. Decline in early life mortality in a high HIV prevalence rural area of South Africa: evidence of HIV prevention or treatment impact? AIDS. 2010;24:593–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peltzer K, Mlambo M, Phaswana-Mafuya N, et al. Determinants of adherence to a single-dose nevirapine regimen for the prevention of mother-to-child HIV transmission in Gert Sibande district in South Africa. Acta Paediatr. 2010;99:699–704. [DOI] [PubMed] [Google Scholar]
- 16.WHO. Making Pregnancy Safer: The Critical Role of the Skilled Birth Attendant (A Joint Statement by WHO, ICM and FIGO). Geneva, Switzerland: WHO; 2004. [Google Scholar]
- 17.Hooseinpoor AR, Victoria CG, Bergen N, et al. Towards universal health coverage: the role of within-country wealth-related inequality in 28 countries in sub-Saharan Africa. Bull World Health Organ. 2011;89:881–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kyomuhendo GB. Low use of rural maternity services in Uganda: impact of women's status, traditional beliefs and limited resources. Reprod Health Matters. 2003;11:16–26. [DOI] [PubMed] [Google Scholar]
- 19.Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85:812–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spangler SA, Bloom SS. Use of biomedical obstetric care in rural Tanzania: the role of social and material inequalities. Soc Sci Med. 2010;71:760–768. [DOI] [PubMed] [Google Scholar]
- 21.Delvaux T, Elul B, Ndagije F, et al. Determinants of nonadherence to a single-dose nevirapine regimen for the prevention of mother-to-child HIV transmission in Rwanda. J Acquir Immune Defic Syndr. 2009;50:223–230. [DOI] [PubMed] [Google Scholar]
- 22.Kirsten I, Sewangi J, Kunz A, et al. Adherence to combination prophylaxis for prevention of mother-to-child-transmission of HIV in Tanzania. PLoS One. 2011;6:e21020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mbonye A, Hansen K, Wamono F, et al. Barriers to prevention of mother-to-child transmission of HIV services in Uganda. J Biosoc Sci. 2010;42:271–283. [DOI] [PubMed] [Google Scholar]
- 24.Muchedzi A, Chandisarewa W, Keatinge J, et al. Factors associated with access to HIV care and treatment in a prevention of mother to child transmission programme in urban Zimbabwe. J Int AIDS Soc. 2010;13:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Otieno PA, Kohler PK, Bosire RK, et al. Determinants of failure to access care in mothers referred to HIV treatment programs in Nairobi, Kenya. AIDS Care. 2010;22:729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deribe K, Woldemichael K, Njau B, et al. Gender differences regarding barriers and motivators of HIV status disclosure among HIV-positive service users. SAHARA J. 2010;7:30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Medley A, Garcia-Moreno C, McGill S, et al. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004;82:299–307. [PMC free article] [PubMed] [Google Scholar]
- 28.Njunga J, Blystad A. “The divorce program”: gendered experiences of HIV positive mothers enrolled in PMTCT programs—the case of rural Malawi. Int Breastfeed J. 2010;5:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rujumba J, Neema S, Byamugisha R, et al. “Telling my husband I have HIV is too heavy to come out of my mouth”: pregnant women's disclosure experiences and support needs following antenatal HIV testing in eastern Uganda. J Int AIDS Soc. 2012;15:17429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Turan JM, Bukusi EA, Onono M, et al. HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: results from the MAMAS study. AIDS Behav. 2011;15:1111–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Desgrées-du-Loû A, Brou H, Traore AT, et al. From prenatal HIV testing of the mother to prevention of sexual HIV transmission within the couple. Soc Sci Med. 2009;69:892–899. [DOI] [PubMed] [Google Scholar]
- 32.Jasseron C, Mandelbrot L, Dollfus C, et al. Non-disclosure of a pregnant woman's HIV status to her partner is associated with non-optimal prevention of mother-to-child transmission. AIDS Behav. 2013;17:488–497. [DOI] [PubMed] [Google Scholar]
- 33.Farquhar C, Kiarie J, Richardson B, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37:1620–1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kalembo F, Zgambo M, Mulaga A, et al. Association between male partner involvement and the uptake of prevention of mother-to-child transmission of HIV (PMTCT) interventions in Mwanza District, Malawi: a retrospective cohort study. PLoS One. 2013;8:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kiarie J, Kriess J, Richardson B, et al. Compliance with antiretroviral regimens to prevent perinatal HIV-1 transmission in Kenya. AIDS. 2003;17:65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aluisio A, Richardson B, Bosire R, et al. Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV-free survival. J Acquir Immune Defic Syndr. 2011;56:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National AIDS and STI Control Programme MoH. Kenya AIDS Indicator Survey 2012: Preliminary Report. Nairobi, Kenya: Ministry of Health; 2013. [Google Scholar]
- 38.WHO, UNICEF, UNFPA, The World Bank. Trends in Maternal Mortality: 1990 to 2010. Geneva, Switzerland: WHO; 2012. [Google Scholar]
- 39.National AIDS and STI Control Programme MoH. Guidelines for Prevention of Mother to Child Transmission (PMTCT) of HIV/AIDS in Kenya. Nairobi, Kenya: Ministry of Health; 2012. [Google Scholar]
- 40.Turan JM, Hatcher AH, Medema-Wijnveen J, et al. The role of HIV-related stigma in utilization of skilled childbirth services in rural Kenya: a prospective mixed-methods study. PLoS Med. 2012;9:e1001295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.WHO Department of Making Pregnancy Safer. Standards for Maternal and Neonatal Care. Provision of Effective Antenatal Care. Geneva, Switzerland: WHO; 2006. [Google Scholar]
- 42.Weiser SD, Heisler M, Leiter K, et al. Routine HIV testing in Botswana: a population-based study on attitudes, practices, and human rights concerns. PLoS Med. 2006;3:e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 44.Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav. 2013;17:2528–2539. [DOI] [PubMed] [Google Scholar]
- 45.Tsai AC, Bangsberg DR, Kegeles SM, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013;46:285–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.WHO. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection. Geneva, Switzerland: WHO; 2013. [PubMed] [Google Scholar]
- 47.Kiula ES, Damian DJ, Msuya SE. Predictors of HIV serostatus disclosure to partners among HIV-positive pregnant women in Morogoro, Tanzania. BMC Public Health. 2013;13:433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Medley AM, Kennedy CE, Lunyolo S, et al. Disclosure outcomes, coping strategies, and life changes among women living with HIV in Uganda. Qual Health Res. 2009;19:1744–1754. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


