Abstract
Background:
Sexual and reproductive health (SRH) services for HIV-positive women and men often neglect their fertility desires. We examined factors associated with pregnancy intent among recently diagnosed HIV-positive women (N = 106) and men (N = 91) who reported inconsistent condom use and were enrolled in an SRH intervention conducted in public sector HIV care clinics in Cape Town.
Methods:
Participants were recruited when receiving their first CD4+ results at the clinic. All reported unprotected sex in the previous 3 months. Logistic regression identified predictors of pregnancy intent for the total sample and by gender.
Results:
About three fifths of men and one fifth of women reported intent to conceive in the next 6 months. In the full-sample multiple regression analysis, men [adjusted odds ratio (AOR = 6.62)] and those whose main partner shared intent to conceive (AOR = 3.80) had significantly higher odds of pregnancy intent; those with more years of education (AOR = 0.81) and more biological children (AOR = 0.62) had lower odds of intending pregnancy. In gender-specific analyses, partner sharing pregnancy intent was positively associated with intent among both men (AOR = 3.53) and women (AOR = 13.24). Among men, odds were lower among those having more biological children (AOR = 0.71) and those unemployed (AOR = 0.30). Among women, relying on hormonal contraception was negatively associated with intent (AOR = 0.08), and main partner knowing her HIV status (AOR = 5.80) was positively associated with intent to conceive.
Conclusions:
Findings underscore the importance of providing integrated SRH services, and we discuss implications for clinical practice and care.
Key Words: condoms, fertility intent, childbearing, HIV+ women and men, South Africa
INTRODUCTION
The increased availability of antiretroviral (ARV) drugs and ARV coverage in sub-Saharan Africa has benefited women and men living with HIV by prolonging their lives, and also by enabling those who wish to do so to have children. Yet, reproductive health services and discourse in the context of HIV have centered almost exclusively on pregnancy prevention,1–4 a focus that runs counter to the cultural importance of fertility in sub-Saharan Africa.2,3,5
The perspective that pregnancy prevention among HIV-positive women should be universally endorsed has persisted since the pre-ARV era. Data offer some support: a recent analysis of population-based data on maternal deaths in sub-Saharan Africa estimated that roughly a quarter of pregnancy-related deaths are related to HIV.6 Yet data from the same report also indicate appreciable reductions in pregnancy-related mortality in HIV-positive women following the introduction of ARVs,6 reductions that likely will increase as ARVs become more widely available. The landscape in which HIV-positive persons weigh fertility options has changed in other ways: risk of mother-to-child transmission has continued to decline, pre- and post-exposure prophylaxis,7,8 treatment as prevention,9 and “lower-tech” safer conception approaches (timed intercourse and self-insemination with partner sperm)10,11 can reduce periconception and partner HIV transmission risk.
Our own research, and that of others, indicates that health care providers seldom discuss conception desires with their HIV-positive clients, possibly because of concerns about the effects of pregnancy on HIV-positive women's health, their own lack of knowledge about safer conception,2,12–16 and negative attitudes many providers still hold about childbearing for HIV-positive individuals.17,18 Nevertheless, accumulating research indicates that HIV-positive persons continue to seek and achieve pregnancy postdiagnosis.6,19–21
There are still significant gaps in understanding the reproductive health needs of HIV-positive women and men. Some research shows that knowledge of HIV status is associated with lower childbearing desire.19,22 Additionally, it often is assumed that newly diagnosed HIV-positive people (compared with those on ARVs) are not interested in immediate pregnancy because of concerns about disclosing to partners, integrating HIV into their everyday lives, transmitting HIV to HIV-negative partners or an infant,23 and being stigmatized by community members.24 However, this question requires further research, especially in a region where strong values for procreation make childlessness unacceptable25 and where biological parenthood plays an important role in women's and men's socially constructed identities and social worth.26 As Mantell et al10 note, “pervasive ‘pronatalist’ attitudes in sub-Saharan Africa place pressure on women to become pregnant, regardless of HIV status”. As a consequence, some HIV-positive women desire pregnancy so as to avoid HIV-associated stigma by proving that they are healthy enough to bear children.12,20 Moreover, the fertility desires of HIV-positive men have been understudied.27–30 Fatherhood is a socially constructed indicator of masculinity,31 and some studies suggest that not having children may result in stigmatization and loss of social status for men.32
Previous research suggests that determinants of pregnancy intent among HIV-positive persons include personal characteristics and circumstances (younger age of mother,29,33,34 being male13); longer time living with HIV/AIDS21,34,35; better perceived and actual health status16,21; being on ARVs36; knowledge (eg, of preventing vertical transmission and ARVs)12,33,37; reproductive factors (fewer biological children16,21,34,38,39); interpersonal and social factors (non-disclosure of HIV status to partner16,21,34); and geographical factors (by country).40 However, in the literature to date, there is limited comparison of gender differences in fertility intent and of the factors that lead newly diagnosed HIV-positive individuals to desire children in the immediate future. Among HIV-positive persons who do not use condoms consistently, it is unclear how many do so because of fertility desires. A review of the impact of ARV treatment on sexual risk behavior in sub-Saharan Africa concluded that, while taking ARVs seems to be associated with decreased risk behavior, there is concern about those who continue high-risk behavioral patterns after initiating ARVs.41 Although studies have primarily focused on promoting condoms to inconsistent condom users, for those who want to conceive, an alternate strategy is needed to decrease transmission risk and promote maternal health. Therefore, it is important to understand factors associated with intent to conceive.
In South Africa, the site of this study, the highest HIV prevalence rates (23%) are among women in their reproductive years, aged 15–49 years,42 as they are in other high HIV prevalence settings in sub-Saharan Africa. In this study, we identified predictors of immediate pregnancy intent at baseline in a subset of HIV-positive women and men who reported unprotected vaginal intercourse in the previous 3 months. Data were drawn from the baseline interview with participants enrolled in a randomized controlled trial evaluating a sexual and reproductive health (SRH) care intervention promoting informed choices.43
METHODS
Study Population and Recruitment
The study was conducted in 4 public sector HIV care clinics in Cape Town, South Africa, between August 2010 and August 2011. These clinics serve low-income individuals from the surrounding townships. In the clinic waiting room before receiving their CD4+ cell count results, a clinic nurse gave clients an Information Sheet describing the study (as one about SRH services for HIV-positive women and men aimed at increasing understanding about how to improve the quality of these services within the HIV care system). Those who were interested were referred to research staff for more information. Potential participants were not informed of the study eligibility criteria.
To be eligible for the trial, participants had to be 18 years or older, attending the clinic to receive their first CD4+ cell count results since testing HIV-positive and therefore not on ARVs, not pregnant, reporting unprotected sex in previous 3 months and/or intent to conceive within the next 6 months, and being willing and able to provide informed consent. These criteria were selected because our intervention focused on both avoidance of pregnancy and adherence to safer conception among HIV-positive individuals who were trying to conceive. The main focus of this article is on HIV-positive inconsistent condom users.
All individuals given an Information Sheet discussed the study with research staff (N = 327); of those, 68 (20.8%) declined to be screened for eligibility, primarily because of time constraints (N = 56; 82.4%). There were no gender differences between those who agreed to be screened and those who did not (P = 0.45).
Informed consent (including access to medical records) was obtained from all interested eligible clients. The study was approved by the Institutional Review Board at the New York State Psychiatric Institute–Columbia University Department of Psychiatry and the Human Research Ethics Committee of the University of Cape Town.
Data Collection
Face-to-face interviews were conducted in isiXhosa or English, according to client preference, by experienced gender-matched interviewers in privacy in the clinic. The baseline interview was administered before participants' receipt of CD4+ cell count results, except for 8 participants, who completed this interview within 1 month of receiving their results. Participants received 50 rand (US $7.00 at the time of the study) for completing the baseline interview.
Measures
The outcome, intent to conceive, was based on a “yes” response to the question, “Are you thinking about trying to have a child in the next 6 months?” Other variables assessed were (1) demographic characteristics, including age, educational level, work status (working full-time or part-time; self-employed; unemployed), place of residence [living in an informal dwelling (makeshift structure), rents a room in someone else's home, or owns/rents home], and number of children currently under participant's care, (2) health status [years since HIV diagnosis and CD4+ cell count (from medical record)], (3) sexual partners and practices (whether participants had a main partner currently or in the past 3 months, and if so whether they lived with that partner), (4) disclosure of HIV status to main partner, and (5) reproductive history over the past 3 months [contraceptive practices, number of biological children, relying on a hormonal method, in relationship with current/recent main partner, and participant's perception of main partner's pregnancy intent (interested in immediately conceiving a child, no immediate intent, uncertain about partner's intent, or partner uninterested in conceiving a child)]. In addition, we assessed self-efficacy for communicating with one's partner about safer sex and SRH, a measure comprising 9 items with responses in the format of a 4-point Likert (sample item: “How confident are you that you could convince (a/your) regular partner in the next 3 months to use condoms?,” with response options ranging from “very unconfident = 1” to “very confident = 4”; Cronbach's alpha = 0.61), and self-efficacy for obtaining information on SRH services, consisting of 4 items and using the same format (sample item: “How confident are you that you could find additional information about contraceptive options at a clinic or hospital?”; Cronbach's alpha = 0.63).
Statistical Analysis
For these analyses, we excluded 17 of the 214 eligible people who reported pregnancy intent but not inconsistent condom use. Therefore, our analysis sample is restricted to those who reported inconsistent condom use, some with and without immediate fertility intent.
Descriptive statistics were generated for demographic variables and key potential predictors of participant's pregnancy intent in the next 6 months overall and by gender, with χ2 and t tests used to compare characteristics between women and men. Because of the highly skewed distribution of the CD4+ cell count variable (range = 73–1260), we used the Wilcoxon rank sum test to compare the median CD4+ cell count between women and men; the log-transformed CD4+ cell count was used in logistic regression analyses.
Simple logistic regression analysis was used to examine the association between each independent variable and pregnancy intent. All potential predictors with a corresponding P-value <0.05 in simple logistic regression were considered for a modified forward stepwise selection procedure, in which insignificant variables are removed from the model before adding a significant variable at each step. We used a P-value = 0.10 for removing variables in the final model selection procedure. Each addition or deletion of a variable to or from a model is a separate step in the selection process, and at each step, a new model is fitted. This approach defines an a posteriori order based on the relative uniqueness of the variables in the sample. A P-value <0.10 was considered statistically significant in the final model. Analyses were conducted for the total sample and separately by gender. The data were analyzed using the PASW SPSS ver. 18.0 (SPSS Inc., Chicago, IL).
RESULTS
Background Characteristics
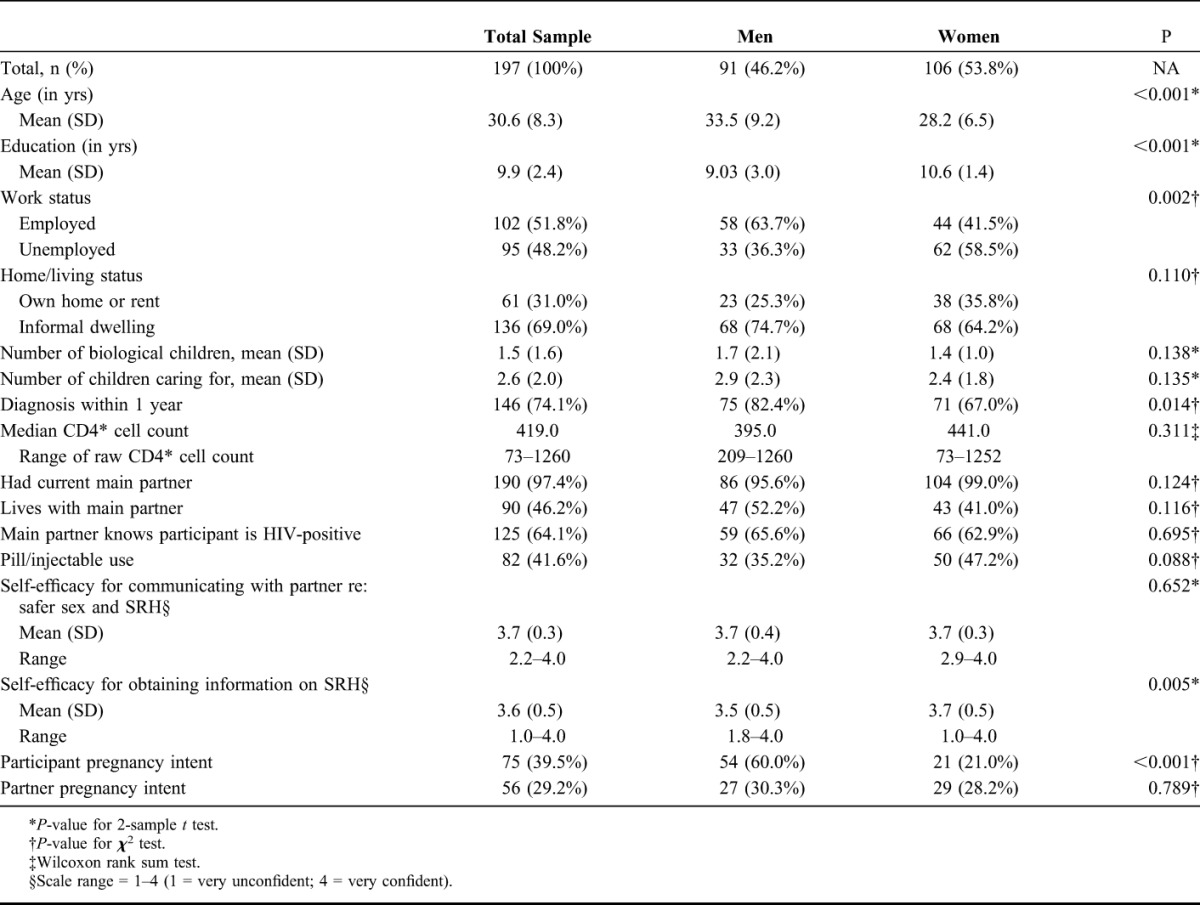
Participants were, on average, 30.6 years of age (median = 29 years; range = 18–63 years; 95.4% were 45 years or younger) and had completed about 10 years of school. More than half worked full- or part-time, and 69.0% resided in an informal dwelling or lived with someone else. On average, they had 1 biological child and cared for 2 children. Seventy-four percent were diagnosed with HIV within the previous year, and median CD4+ cell count was 419 cells per cubic millimeter (range = 73–1260 cells/mm3; 31.0% had CD4 <350 cells/mm3). The majority (97.4%) reported having a main partner, and 46.2% lived with their main partner. Nearly two-thirds (64.1%) of participants indicated that their main partner knew they were HIV positive, with no differences by gender. About two-fifths (41.6%) reported that they or their partner used hormonal contraception. Hormonal contraceptive use was higher among those not wishing to conceive than among those seeking pregnancy (78.8% vs. 21.2%; P < 0.001; not tabled). Compared with women, men were significantly older, less educated, more likely to be employed, live in an informal dwelling, and more recently diagnosed with HIV. Women reported higher self-efficacy for communicating with their main partner about safer sex and SRH and for obtaining SRH information than men.
Pregnancy Intent
More men than women reported intent to conceive in the next 6 months (60.0% of men and 21.0% of women; P < 0.001). There was no statistically significant difference by gender in the proportion of women and men who reported that their main partner had an immediate intent to have a child (30.3% of men; 28.2% of women; P = 0.789) (Table 1).
TABLE 1.
Participant Characteristics, HIV-Positive Women and Men, Reporting Inconsistent Condom Use
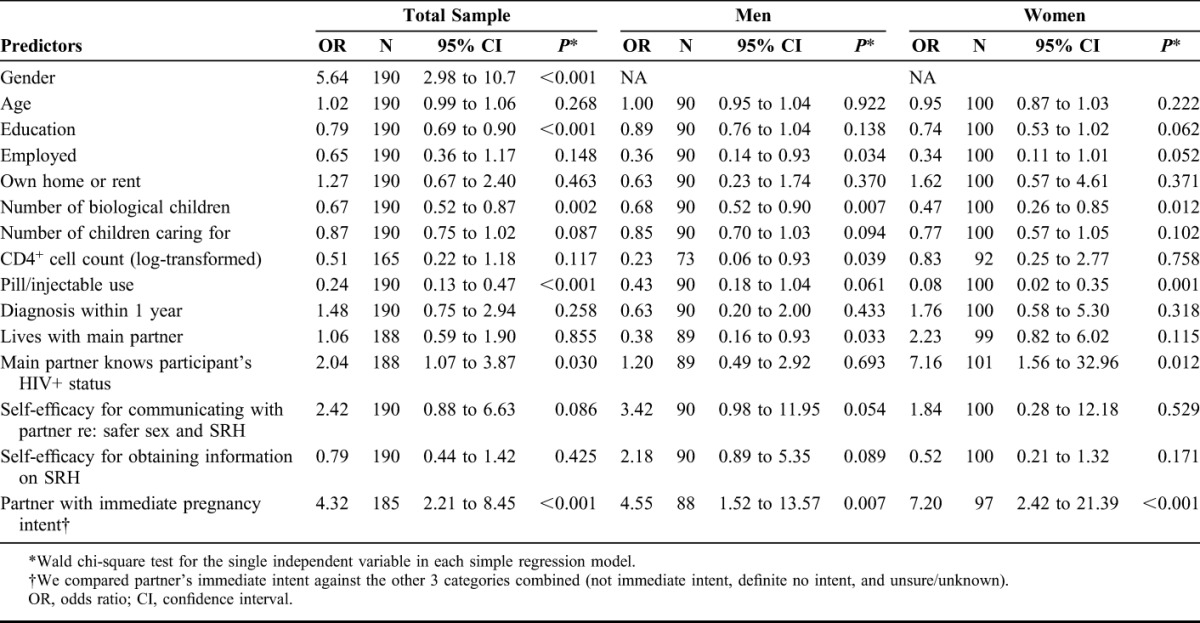
The results of the simple regression analyses for pregnancy intent among the total sample and by gender are shown in Table 2. In the full sample, the odds of pregnancy intent in the next 6 months were 5.64 times greater among men than among women (P < 0.001) and were lower for each additional year of education, although education was not associated with pregnancy intent in the gender subgroup analysis. In the total sample and among women and men separately, having more biological children was associated with lower odds of pregnancy intent, and having a partner who also intended immediate pregnancy was associated with higher odds of intent. Among men, higher CD4+ cell count was associated with lower odds of pregnancy intent as was living with a main partner. Among women, main partner knowing they were HIV-positive was associated with higher odds of pregnancy intent, and use of a hormonal contraceptive was associated with lower odds of intent.
TABLE 2.
Simple Logistic Regression for Predictors of Participant's Immediate (Next 6 Months) Intent to Become Pregnant (or Get Female Partner Pregnant Among Male Participants) Overall and by Gender Among a Sample of HIV-Positive Women and Men Reporting Inconsistent Condom Use
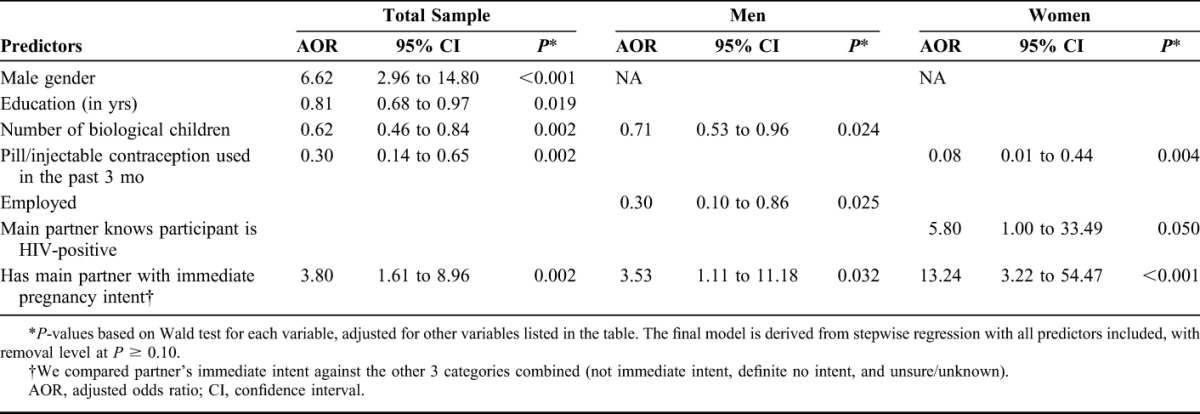
In the final multiple regression analysis for the total sample (Table 3), male gender [adjusted odds ratio (AOR) = 6.62; P < 0.001] and main partner having immediate pregnancy intent (AOR = 3.80; P = 0.002) were significantly associated with higher odds of pregnancy intent, whereas more years of education (AOR = 0.81; P = 0.019), having more biological children (AOR = 0.62; P = 0.002), and relying on hormonal contraception (AOR = 0.30; P = 0.002) were associated with lower odds of pregnancy intent. Among men, having more biological children (AOR = 0.71; P = 0.024) and being employed (AOR = 0.30; P = 0.025) were associated with lower odds of pregnancy intent, whereas partner having immediate pregnancy intent (AOR = 3.53; P = 0.032) was associated with higher odds of participant's pregnancy intent. Among women, using hormonal contraceptives was associated with lower odds of pregnancy intent (AOR = 0.08; P = 0.004), whereas main partner being aware of her HIV-positive status (AOR = 5.80; P = 0.050) and partner having immediate pregnancy intent were associated with higher odds (AOR = 13.24; P < 0.001).
TABLE 3.
Final Multiple Logistic Regression Models Determined Using Stepwise Regression (P < 0.1 for Inclusion) for Identifying Predictors of Immediate Intent to Become Pregnant (or Get Female Partner Pregnant Among Male Participants) Overall and by Gender Among a Sample of HIV-Positive Inconsistent Condom Users
DISCUSSION
Among this sample of HIV-positive women and men who had engaged in unprotected sex in the 3 months before enrolling in HIV care, we found that 59.3% of men and 19.8% of women reported an immediate intent to conceive a child (P < 0.001). Consistent with other studies,12,26,29,36,44 these data underscore the importance of improving reproductive services to assist women and men living with HIV to either prevent unwanted pregnancies through consistent condom use (perhaps coupled with a hormonal contraceptive as dual protection) or conceive and give birth as safely as possible. Separation of HIV care, reproductive healthcare, maternal and child health, and paternal concerns into discrete service silos results in critical missed opportunities—to provide as-needed contraceptive, risk-reduction, pre-conception services, and care through pregnancy and beyond.45,46
The high fertility intent among HIV-positive men in our sample likely reflects notions of masculinity, including the desire to demonstrate one's virility and to “leave one's name behind,” motivations noted in other studies.12,26,30,38 In the full sample, participants who reported that their partner also had immediate pregnancy intent were almost 4 times likely to want to have children themselves. Believing that one's main partner wished to conceive in the near future was positively associated with pregnancy intent among both women and men, although partner's intent was more strongly associated with women's intent than men's, reflecting gendered social roles. These findings highlight the need for “male-friendly” services to help HIV-positive men and their partners make informed decisions about parenthood and understand how to minimize HIV risk to negative partners when trying to conceive. This is especially critical given that reproductive health services have traditionally been oriented toward women and unfriendly to men.47
In our study, nearly two-thirds of the women had shared their HIV status with their partners, and in the multiple regression analysis, women whose partners were aware of their status had almost 6 times higher odds of desiring to conceive in the next 6 months compared with those who had not. This association was not found in Phaweni's study of HIV-positive women recruited from antenatal services in Mpumalanga, South Africa,40 perhaps because these women had recently given birth. Our findings indicated that disclosure had already occurred among many women interested in conceiving, suggesting that partners could join them directly in pre-conception counseling about safer conception.
Having fewer biological children was positively associated with pregnancy intent, a finding noted in other studies.16,21,27,34,38 Having more education was associated with lower pregnancy intent, consistent with findings from a study among HIV-positive women and men in Nigeria,17 but not consistently found in a recent meta-analysis.48 Using hormonal contraception was also associated with lower odds of pregnancy intent in the whole sample and among women, as would be expected, suggesting that some may be using contraceptives instead of condoms to prevent pregnancy, thus putting themselves and their partners at risk for sexually transmitted infection (STI) transmission/acquisition (54.8% of our sample did not use condoms but reported hormonal contraceptive use; not tabled).
Unlike several other studies,21,36,39 age was not a significant predictor of intent to conceive in the next 6 months. Many studies do not specify a definitive time frame for intent, whereas our study asked about intent to conceive in the next 6 months. In addition, differences in sample characteristics (eg, age range, gender composition, newly diagnosed with HIV or not, initiated ARVs or not, in relationship or not) and sample size may account for the lack of association in our study.
In the simple (but not multiple) regression analysis, CD4+ cell count was inversely related to pregnancy intent for men, but not for women, consistent with findings from our previous qualitative work.12 CD4+ cell count is a surrogate measure of immunological and health status; it is one of the most important biomarkers of health status for HIV-positive people, and among both HIV-positive women and men in Nigeria, low CD4+ cell count was an independent predictor of intent to have more children.21 Fertility desires of some HIV-positive men with immunocompromised health status may intensify, leading them to seek a(nother) child as part of their “legacy.” In contrast, Mmbaga et al16 found that higher CD4+ cell counts were associated with greater reproductive desire among HIV-positive women and men in rural Tanzania. Finally, other studies have found no significant relationship between CD4+ cell count and current fertility intentions.2,13 The strength and direction of the association between CD4+ cell count and fertility intent most likely is a function of sample characteristics, study design, and/or operationalization of pregnancy intent. However, providers should not deduce that HIV-positive men with low CD4+ cell counts are uninterested in procreation; they should universally assume that all HIV-positive clients, even those newly diagnosed or ARV-naive, could very well be interested in conceiving in the near future.
We note a number of limitations. First, the study was not designed to assess prevalence of pregnancy intent. Among those screened for eligibility, only 8.6% of men and less than a quarter of women reported neither pregnancy intent nor unprotected sex, suggesting that the sample may be atypical. Therefore, the proportion of men and women reporting interest in becoming pregnant in the near future for inconsistent condom users is likely an overestimate. Second, with our small sample size, we have limited power to detect factors that may have weaker but important associations with pregnancy intent. Third, we did not assess the HIV status of participants' partners, which may be a determinant of fertility intent. Our measure of partner's pregnancy intent was reported by study participants and therefore may reflect the participant's rather than the partner's beliefs. In addition, we asked about contraceptive use in the past 3 months and fertility intent in the next 6 months. Thus, some participants with fertility intent might have used contraceptives in the past 3 months before deciding to become pregnant. However, our finding that those who used contraceptives in the past 3 months had lower odds of fertility intent is, as would be expected, despite this temporal issue.
Our study findings underscore the need for tailored reproductive health counseling based on reproductive goals that can help HIV-positive women and men and their partners make informed decisions about their fertility desires. Sexual risk-reduction counseling, which generally emphasizes abstinence or condom use with a standard recommendation to augment with hormonal contraception, does not speak to the needs of HIV-positive women and men with fertility intentions. It is also not responsive to HIV-positive individuals without fertility intent who do not use effective contraception (among 122 participants without fertility intent in our sample, 45.2% did not use effective contraception; not tabled). Both groups run the risk of transmitting HIV to negative partners, acquiring an STI or another HIV strain from partners, and the latter group also risks having unintended pregnancies. Thus, both groups need to be prioritized for risk-reduction counseling, but the form of that counseling must be responsive to the fertility goals of the HIV-positive individual. It is imperative for providers to explore “safer conception” with their HIV-positive clients because those who desire children may not know how to minimize disease transmission risk to their HIV-negative partners17 or themselves and may unwittingly choose to conceive at times that are suboptimal for parental and fetal health.
Until reproductive guidelines for people living with HIV are translated into public policy in South Africa and elsewhere, supported by training and fiscal commitment, HIV-positive persons seeking to have a child are operating without medical guidance. HIV/AIDS service organizations and advocates should increase efforts to further HIV-positive persons' reproductive goals, including safer maternal health and avoidance of HIV/STI transmission and unintended pregnancy.
ACKNOWLEDGMENTS
The authors especially appreciate the women and men who participated in this study and the Departments of Health in the Western Cape and City of Cape Town. The authors also acknowledge the contributions of other co-investigators of the study—Chelsea Morroni, PhD, MBChB, and Keith Cloete, MBChB, and the team who ran the day-to-day operations of the study—Nomazizi Cishe and Ntobeko Nywagi.
Footnotes
Supported by the National Institute of Mental Health (NIMH) Grant R01 MH 078770 (to J.E.M. and D.C.), a Center Grant NIMH P30 MH43520 (to R.H.R.), and an African Knowledge Grant from the Promotion of Enhancement of Research Capacity Program at the University of Cape Town.
The authors have no conflicts of interest to disclose.
The views and opinions expressed in this article are solely those of the authors and do not necessarily represent the official views of the National Institute of Mental Health.
REFERENCES
- 1.Myer L, Carter R, Katyal M, et al. Impact of antiretroviral therapy on incidence of pregnancy among HIV-infected women in sub-Saharan Africa: a cohort study. PLoS Med. 2010;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwartz SR, Mehta SH, Taha TE, et al. High pregnancy intentions and missed opportunities for patient-provider communication about fertility in a South African cohort of HIV-positive women on antiretroviral therapy. AIDS Behav. 2012;16:69–78. [DOI] [PubMed] [Google Scholar]
- 3.van Der Spuy Z. HIV and reproductive health: a South African experience. Reprod Biomed Online. 2009;18:3–10. [DOI] [PubMed] [Google Scholar]
- 4.Schaan MM, Taylor M, Puvimanasinghe J, et al. Sexual and reproductive health needs of HIV-positive women in Botswana—a study of health care worker's views. AIDS Care. 2012;24:1120–1125. [DOI] [PubMed] [Google Scholar]
- 5.Beyeza-Kashesya J, Ekstrom AM, Kaharuza F, et al. My partner wants a child: a cross-sectional study of the determinants of the desire for children among mutually disclosed sero-discordant couples in Uganda. BMC Public Health. 2010;10:247 Available at: http://www.biomedcentral.com/1471-2458/10/247. Accessed April 10, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaba B, Calvert C, Marston M, et al. Effect of HIV infection on pregnancy-related mortality in sub-Saharan Africa: secondary analyses of pooled community-based data from the network for Analysing Longitudinal Population-based HIV/AIDS data on Africa (ALPHA). Lancet. 2013;381:1763–1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367:399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367:423–434. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mantell J, Smit J, Stein Z. The right to choose parenthood among HIV-infected women and men. J Public Health Policy. 2009;30:367–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chadwick R, Mantell JE, Moodley J, et al. A review of safer conception interventions for HIV-affected couples: implications for resource-constrained settings. Top Antivir Med. 2011;19:148–155. [PMC free article] [PubMed] [Google Scholar]
- 12.Cooper D, Harries J, Myer L, et al. “Life is still going on”: reproductive intentions among HIV-positive women and men in South Africa. Soc Sci Med. 2007;65:274–283. [DOI] [PubMed] [Google Scholar]
- 13.Cooper D, Moodley J, Zweigenthal V, et al. Fertility intentions and reproductive health care needs of people living with HIV in Cape Town, South Africa: implications for integrating reproductive health and HIV care services. AIDS Behav. 2009;13(suppl 1):38–46. [DOI] [PubMed] [Google Scholar]
- 14.Harries JD, Cooper D, Myer L, et al. Policy makers and health care providers' perspectives on reproductive decision-making amongst HIV-infected individuals in South Africa. BMC Public Health. 2007;7:282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moodley J, Cooper D, Mantell JE, et al. Health care provider perspectives on pregnancy and parenting in HIV-positive individuals in South Africa. BMC Health Serv Res. 2014;14:384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mmbaga EJ, Leyna GH, Ezekiel MJ, et al. Fertility desire and intention of people living with HIV/AIDS in Tanzania: a call for restructuring care and treatment services. BMC Public Health. 2013;13:86 Available at: http://www.biomedcentral.com/1471-2458/13/86. Accessed May 2, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erhabor O, Akani CI, Eyindah CE. Reproductive health options among HIV-infected persons in the low-income Niger Delta of Nigeria. HIV AIDS (Auckl). 2012;4:29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Messersmith L, Semrau K, Anh TL, et al. Women living with HIV in Vietnam: desire for children, use of sexual and reproductive health services, and advice from providers. Reprod Health Matters. 2012;20:27–38. [DOI] [PubMed] [Google Scholar]
- 19.Dube AL, Baschieri A, Cleland J, et al. Fertility intentions and use of contraception among monogamous couples in northern Malawi in the context of HIV testing: a cross-sectional analysis. PLoS One. 2012;7:e51861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bankole A, Biddlecom AE, Dzekedzek K. Women's and men's fertility preferences and contraceptive behaviors by HIV status in 10 sub-Saharan African countries. AIDS Educ Prev. 2011;23:313–328. [DOI] [PubMed] [Google Scholar]
- 21.Oladapo OT, Daniel OJ, Odusoga OL, et al. Fertility desires and intentions of HIV-positive patients at a suburban specialist centre. J Natl Med Assoc. 2005;97:1672–1681. [PMC free article] [PubMed] [Google Scholar]
- 22.Yeatman SE. The impact of HIV status and perceived status on fertility desires in rural Malawi. AIDS Behav. 2009;13(suppl 1):12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nduna M, Farlane L. Women living with HIV in South Africa and their concerns about fertility. AIDS Behav. 2009;13(suppl 1):62–65. [DOI] [PubMed] [Google Scholar]
- 24.McCarraher D, Cuthbertson C, Kung D, et al. Sexual behavior, fertility desires and unmet need for family planning among home-based care clients and caregivers in Kenya. AIDS Care. 2008;20:1057–1065. [DOI] [PubMed] [Google Scholar]
- 25.Ibisomi L, Mudege NN. Childlessness in Nigeria: perceptions and acceptability. Cult Health Sex. 2014;16:61–75. [DOI] [PubMed] [Google Scholar]
- 26.Taylor TN, Mantell JE, Nywagi N, et al. “He lacks his fatherhood”: safer conception technologies and the biological imperative for fatherhood among recently-diagnosed Xhosa-speaking men living with HIV in South Africa. Cult Health Sex. 2013;15:1101–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakayiwa S, Abang B, Packel L, et al. Desire for children and pregnancy risk behavior among HIV infected men and women in Uganda. AIDS Behav. 2006;10(suppl 4):S95–S104. [DOI] [PubMed] [Google Scholar]
- 28.Nattabi B, Li J, Thompson SC, et al. A systematic review of factors influencing fertility desires and intentions among people living with HIV/AIDS: implications for policy and service delivery. AIDS Behav. 2009;13:949–968. [DOI] [PubMed] [Google Scholar]
- 29.Myer L, Morroni C, Rebe K. Prevalence and determinants of fertility intentions of HIV-infected women and men receiving antiretroviral therapy in South Africa. AIDS Patient Care STDS. 2007;21:278–285. [DOI] [PubMed] [Google Scholar]
- 30.Sherr L, Barry N. Fatherhood and HIV-positive heterosexual men. J HIV Med. 2004;5:258–263. [DOI] [PubMed] [Google Scholar]
- 31.Lynch I, Brouard PW, Visser MJ. Constructions of masculinity among a group of South African men living with HIV/AIDS: reflections on resistance and change. Cult Health Sex. 2010;12:15–27. [DOI] [PubMed] [Google Scholar]
- 32.Dyer S, Abrahams N, Mokoena N, et al. “You are a man because you have children”: experiences, reproductive health knowledge and treatment seeking behaviours among men suffering from couple infertility in South Africa. Hum Reprod. 2004;19:960–967. [DOI] [PubMed] [Google Scholar]
- 33.Peltzer K, Chao LW, Dana P. Family planning among HIV positive and negative Prevention of Mother to Child Transmission (PMTCT) clients in a resource poor setting in South Africa. AIDS Behav. 2009;13:973–979. [DOI] [PubMed] [Google Scholar]
- 34.Phaweni K, Peltzer K, Mlambo F, et al. Factors influencing pregnancy desires among HIV positive women in Gert Sibande District in Mpumalanga, South Africa. Gend Behav. 2010;8:2960–2975. [Google Scholar]
- 35.Kawale P, Mindry D, Stramotas S, et al. Factors associated with desire for children among HIV-infected women and men: a quantitative and qualitative analysis from Malawi and implications for the delivery of safer conception counseling. AIDS Care. 2014;26:769–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maier M, Andia I, Emenyonu N, et al. Antiretroviral therapy is associated with increased fertility desire, but not pregnancy or live birth, among HIV+ women in an early HIV treatment program in rural Uganda. AIDS Behav. 2009;13(suppl 1):28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kanniappan S, Jeyapaul MJ, Kalyanwala S. Desire for motherhood: exploring HIV-positive women's desires, intentions and decision-making in attaining motherhood. AIDS Care. 2008;20:625–630. [DOI] [PubMed] [Google Scholar]
- 38.Paiva V, Filipe EV, Santos N, et al. The right to love: the desire for parenthood among men living with HIV. Reprod Health Matters. 2003;11:91–100. [DOI] [PubMed] [Google Scholar]
- 39.Wagner G, Linnemayr S, Kityo C, et al. Factors associated with intentions to conceive and its communication to providers among HIV clients in Uganda. Matern Child Health J. 2012;16:510–518. [DOI] [PubMed] [Google Scholar]
- 40.Bankole A, Biddlecom AE, Dzekedzeke K, et al. Does knowledge about antiretroviral therapy and mother-to-child transmission affect the relationships between HIV status and fertility preferences and contraceptive use? New evidence from Nigeria and Zambia. J Biosoc Sci. 2014;46:580–599. [DOI] [PubMed] [Google Scholar]
- 41.Kaye DK, Kakaire O, Osinde MO, et al. The impact of highly active antiretroviral therapy on high-risk behaviour of HIV-infected patients in sub-Saharan Africa. J Infect Dev Ctries 2013;7:436–447. [DOI] [PubMed] [Google Scholar]
- 42.Shisana O, Rehle T, Simbayi LC, et al. South Africa National HIV Prevalence, Incidence and Behaviour Survey 2012. Cape Town, South Africa: HSRC Press; 2014. [DOI] [PubMed] [Google Scholar]
- 43.Mantell JE, Cooper D, Moodley J, et al. Integrating sexual and reproductive health into HIV care in public sector clinics in Cape Town, South Africa: results of a phase 2 study. Poster #TUPE124 International AIDS Conference; July 2014; Melbourne, Australia.
- 44.Wagner GJ, Wanyenze R. Fertility desires and intentions and the relationship to consistent condom use and provider communication regarding childbearing among HIV clients in Uganda. ISRN Infect Dis. 2013;2013:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Myer L. Maternal deaths and HIV treatment in sub-Saharan Africa. Lancet. 2013;381:1699–1700. [DOI] [PubMed] [Google Scholar]
- 46.Horton R. What will it take to stop maternal deaths? Lancet. 2009;374:1400–1402. [DOI] [PubMed] [Google Scholar]
- 47.Ramirez-Ferrero E, Lusti-Narasimham M. The role of men as partners and fathers in the prevention of mother-to-child transmission of HIV and in the promotion of sexual and reproductive health. Reprod Health Matters. 2012;20:103–109. [DOI] [PubMed] [Google Scholar]
- 48.Berhan Y, Berhan A. Meta-analyses of fertility desires of people living with HIV. BMC Public Health. 2013;13:409. [DOI] [PMC free article] [PubMed] [Google Scholar]


