Abstract
Background:
To better understand service-related needs and the current situation of persons with spinal cord injury (SCI) living in the community, a more comprehensive approach for studying their interrelationships (needs vs community living outcomes) is greatly needed.
Objective:
To describe the development, design, and findings of a Canadian survey portraying the life situation of people with SCI.
Method:
The SCI Community Survey covers demographics, health, SCI-specific needs, community participation, employment, quality of life, health care utilization, and overall health rating. A total of 1,549 persons with SCI completed the survey (Web or phone) between May 2011 and August 2012.
Results:
Some major expressed needs for services to support community living are met to a great extent for a substantial proportion of people with SCI. Complications remain highly prevalent for some health issues, including pain, sexual dysfunction, and musculoskeletal disorders. The extent of community participation based on values and preferences varies tremendously among daily activities and social roles. Some dimensions of quality of life are rated positively (eg, family life) while others are greatly disrupted (eg, sex life and physical health). Most of these findings vary significantly between people with traumatic and nontraumatic lesions.
Conclusion:
This survey is the first in Canada and among the first worldwide to draw a comprehensive picture of major aspects of the lives of people with SCI including service needs. The results will help to determine the links between various aspects of community living and guide service providers and policy makers in focusing on major issues to enhance quality of life after SCI.
Key words: community living, SCI-related needs, secondary health conditions, social participation, spinal cord injury, quality of life
There is a strong focus in acute care and rehabilitation on developing functional independence through education, teaching, health care, and services for people who sustain spinal cord injury (SCI). Nonetheless, after discharge from hospital or an SCI unit, rehabilitation is not complete and the challenging journey toward a full and productive life begins. Community living presents various physical, social, and attitudinal barriers that many people with SCI have difficulty overcoming, even though the UN Convention on the Rights of Persons with Disabilities1 enshrines the right to full and effective community participation, to live independently, to be included in the community, and to participate in political, public, and cultural life, recreation, and sports.
Various environmental and contextual dimensions influence community living and require attention. Among these, access to services in the community is critical to ensure that people with SCI achieve optimal quality of life. The World Report on Disability2 identified a series of community services that could influence effective participation, including home care and support, primary health care, transportation, social and family support, education and job training, and technologies to enhance mobility, communication, and home adaptation. While the report suggests critical community services, it is unclear to what extent such services correspond to met and unmet needs expressed by people with SCI, given the complex relationship between service use and unmet needs.3
Kennedy et al4 used a broad definition of need (circumstance requiring a course of action, want, or requirement) and included the prevention and treatment of health complications, increase in social participation, and quality of life with other needs that are more aligned with a focus on community (eg, wheelchair needs, relationships, emotional well-being, and accommodation). They found that employment and recreational activities were the needs that were least likely to be met.
The identification of service needs therefore remains a major issue, and only a few studies have investigated the expressed needs of persons with SCI and barriers to needs being met. Cox et al5 suggested areas with the greatest needs, such as physical changes in the environment, transportation, and work issues. They also identified the greatest perceived barriers to needs being met, with limited local specialist knowledge and inadequate funding being most important. In Canada, 2 national surveys examined self-reported needs as well as service availability for individuals with SCI living in the community,6,7 suggesting that needs for financial support, attendant care, equipment and accessibility, active living, and specialized equipment are largely unmet.
These previous surveys provided insight into needs that should be met for community integration or participation, but the needs identified were a combination of services (eg, recreational programs) and influencing factors (eg, accessible infrastructure). These surveys were not able to clarify the relationships between services and outcomes or to determine which factors facilitated or hindered access to services.
There is a general consensus that, following SCI, quality of life remains the ultimate goal of rehabilitation, but this is influenced by issues such as the occurrence of secondary health conditions (SHCs) and the extent of social participation.8 For example, some dimensions of participation are carried out in a satisfactory manner without difficulty but significant restrictions are observed in family roles (primarily activities related to housework, home maintenance, and role fulfillment at home), work, and education.9–11 To ensure that quality of life remains relatively constant across the lifespan, factors that influence it, including service needs, must be identified on a personal basis.
To better understand the service needs of persons with SCI living in the community and their short- and long-term life situation after discharge from hospital or rehabilitation, a comprehensive study examining the relationships between needs and influencing factors and their impact on important outcomes is needed. Such a survey should include data on major life dimensions identified in the literature and by community advocates, namely quality of life and community participation, as well as other influencing variables, such as the occurrence of SHCs.12
The aim of this article is to describe the development, design, and initial findings of a Canadian survey portraying the life situation of people with SCI living in the community. Specifically, the survey aimed to (a) identify the proportion of people with SCI requiring services for community living and the extent of met and unmet needs, (b) determine the barriers or facilitators to service utilization, and (c) describe the outcome in the lives of people with SCI (occurrence of SHCs, degree of participation in major life areas including productive activities, quality of life) and their interrelationships with service needs (met and unmet).
Methods
Procedures for developing the survey
The survey design is described in detail here, because this article serves as the reference article in this issue on the Canadian SCI Community Survey (SCICS) that will look at the interrelationships between needs and other aspects of the participants’ lives (SHCs, social participation, quality of life, health care utilization, employment, etc).
The SCICS is a series of measures identified by Canadian experts, including people with SCI, researchers, health care professionals, and service providers, to assess important aspects of community living. A research team was responsible for developing and testing the survey. Some measures (eg, Short Form-12) were previously developed, whereas others were created and validated as part of the Rick Hansen SCI Registry Community follow-up questionnaire.13 The research team reviewed each measure to determine its order in the survey and ensure appropriate reading level and language (eg, instructions, definition of concepts). A beta version of the survey was piloted by 18 individuals with SCI who met inclusion criteria and completed the survey online twice, with 5 days between each administration. After completing the 2 surveys, they attended a focus group to provide feedback on the questions. The pilot data were analyzed to ensure the questions were clear and accurately described the constructs. The research team revised the measures and survey process based on this feedback. A second round of testing was conducted with individuals who met the inclusion criteria to validate the modifications.
Measures
Demographics included date of SCI, age, relationship status and living arrangement, gender, ethnic origin, language, postal code, education level, income (personal, household), and source of income. An SCI classification measure provided information on the type and severity of injury as well as the cause (traumatic, nontraumatic) of the SCI.
The SCI Health Questionnaire (SCI-HQ) comprised 2 sections assessing the most frequent SHCs (n = 21) and comorbidities (n = 13) that can occur after SCI (over the previous 12 months).13 The secondary complication scale asks about the occurrence of each complication on a 6-point ordinal scale (0 = never to 5 = every day) and their interference with a person’s daily activities on a 5-point ordinal scale (1 = not at all to 5 = completely). Four complications used a dichotomous scale (yes/ no) (eg, deep venous thrombosis, joint contracture, neurological deterioration, weight problems) and pressure ulcers were described by the number of new episodes (1, 2, 3, 4 or 5+) in the previous 12 months.
The SCI-related needs measure included information on needs for services that foster community integration and participation for people with SCI, such as housing, equipment and support services, transportation, health care, healthy living, and job training. For each SCI need, questions were asked about (a) the expressed needs after discharge into the community; (b) the extent to which each need was met or unmet (1 = completely to 5 = not at all); (c) help received from family, friends, and governments/community organizations; and (d) obstacles preventing access to services to meet needs (eg, availability, affordability and features of services, physical accessibility, lack of information, SCI knowledge of service providers). There were also questions about the participants’ satisfaction with the help they received and the importance of the need to live a full life.
Community participation was addressed using the person-perceived Participation in Daily Activities Questionnaire (PDAQ)13 covering 26 daily activities and social roles. Questions include the extent of participation (as much as wanted or not) and the desire to participate in cases of nonparticipation. The PDAQ also asks about the assistance required to participate in the activity, difficulties encountered when participating, and reasons for not participating, such as the level of disability, lack of assistance, and environmental barriers (physical or social). The occupation measure asks about the participants’ occupational activities (including hours per week they participate in each activity). Other questions included pre-injury and current level of education, pre-injury and current employment in major work sectors (eg, management, business, health, sales and service, etc), and, if applicable, reasons for not working, types of support required to obtain or maintain gainful employment, and satisfaction with current employment.
Quality of life was measured in 2 dimensions (overall and domain specific). A single question asked participants to rate their overall quality of life in the previous 2 weeks (1 = very bad to 5 = very good).13 The Life Satisfaction Questionnaire (LiSAT-11), a standardized quality of life measure, includes 11 questions exploring satisfaction with various aspects of life (1 = very dissatisfying/ dissatisfied to 6 = very satisfying/satisfied). Each question in the LiSAT-11 and an overall average score can be reported.14
The health care utilization measure is a modified version of the Canadian Community Health Survey (CCHS)15 section on health care utilization. Added to the list were rehabilitation health professionals (eg, physiatrist, urologist, orthotist/ prosthotist, sexual health clinician) who were seen or talked to regarding a health issue or considered in a single item (eg, occupational therapist, spine surgeon) rather than combined (eg, medical doctors, rehabilitation professionals). Participants also indicated whether they had been admitted to a hospital overnight in the past 12 months (and the number of nights if applicable) and whether they had not received needed health care in the past 12 months and the reasons for not receiving services.
Overall health rating was measured with the Short Form-12 (SF-12), a generic health status instrument. It contains 12 questions covering the following domains: physical function, role physical function, mental function, role mental function, social function, bodily pain, vitality, and general health. For most questions, participants must choose how often the statement is true (1 = all of the time to 5 = none of the time).16
Recruitment and data collection
The primary recruitment strategy was conducted through a national consumer awareness campaign including national and local media advertisements as well as a survey-specific Web site. The recruitment strategy included sending information packages to SCI community groups (eg, Spinal Cord Injury Canada, Canadian Wheelchair Sports Association, etc) for distribution to their members as well as using the Rick Hansen SCI Registry at Canadian SCI centers to identify eligible participants (Canadians with SCI caused by a trauma or disease, living in a community setting for at least 1 year after discharge from hospital/rehabilitation, and ≥18 years of age).
Data collection was performed using a Web site developed by the Mustel Group (http://www.mustelgroup.com), a market research organization with experience conducting online surveys. Two urls were available for study participants (English and French). Participants first reviewed and electronically signed the informed consent form and then received a confirmation e-mail with a link to the survey. If they logged off, they could re-enter the survey later and finish it. If a participant did not re-access the survey within 3 weeks, a reminder e-mail was sent and a final e-mail was sent 1 week later. An option to have trained interviewers complete the survey on the phone was offered. Participants provided verbal consent prior to starting the survey.
Ethics
Ethical approval was obtained from an independent ethics board (Institutional Research Board Services) and also from the Research Ethics Board of Université Laval (principal investigator’s institution). Ethical approval from local research ethics boards was also obtained to recruit from SCI centers across Canada.
Data management
During data acquisition (May 2011 to August 2012), the Mustel Group monitored all surveys that were submitted to ensure that each participant had only 1 record. For instance, a participant may have created a new record (eg, in a second session) to report a major change in his/her life conditions or provide additional information, but only the last valid complete record was kept in the database. As with any Internet survey, participants with multiple entries (4 ≤ nrecords≤ 10) were excluded in this survey (n = 7). The Mustel Group ensured that communication channels (IP addresses or phone numbers) were from Canadian locations, and incomplete records or those without informed consent were excluded.
Data were also checked for unrealistic responses. For instance, a person could not answer that he/ she lived with a spouse and then report being single in another question. Twenty-eight data quality checks were done; 96% of participants had consistent answers and none failed more than 1 check. Participants could describe their situation in response to several questions. All answers were read and reclassified when the proposed categories were clearly applicable. When a new category had to be created, a new parallel variable was created, because this category was not explicitly mentioned to every respondent.
When secondary questions were not applicable, they were skipped and the observation was recorded as missing data. Answers “don’t know” and “prefer not to answer” were also recorded with unique codes and defined as missing data. When needed, it was possible to redefine these categories as nonmissing data. To maximize the sample for the multivariate analyses, these categories could also be grouped with other categories. For instance, in reporting health complications, a “don’t know” answer could be assumed to be a “no.” Based on expert opinion, missing data were inferred to create new equivalent variables, and the researchers could use either the original or a new variable depending on their statistical needs. When there was the option to answer “other,” code 96 was applied and the answers were logged in another variable. The answer “don’t know” was coded 97. When the question was “not applicable,” code 98 was applied for that question. “Prefer not to answer” responses were coded 99. The exception to that was the question on employment sectors, where choices extend up to 100; in that case, “don’t know” was coded 997 and “prefer not to answer” was coded 999.
The database is stored on secure servers, and its utilization is strictly controlled via data-sharing agreement. Beyond the main research team, access is restricted to sections related to the specific hypotheses under study. Statistical analyses were selected to take into account that most variables are ordinal or nominal scales. Several derived variables were computed, and they can also be an aggregate based on several variables, such as an estimate of the American Spinal Injury Association Impairment Scale (AIS) grade, latent variables drawn from structural equation modeling, or inertias from multiple correspondence analyses. When assumptions were reasonably met, continuous and derived variables were analyzed with parametric tests. The α level was set at 0.05; when realistic, the results were examined with an α correction for multiple comparisons. Further detailed statistical procedures are reported in other articles in this issue.
Results
The recruitment process ensured significant representativeness from the major Canadian regions, and the 2 largest provinces (Ontario and Quebec) accounted for almost 50% of the total sample (Table 1). Most participants lived in large urban areas (>100,000 people), and about 20% lived in small communities (<10,000 people). A high proportion of participants were Caucasian (91%), English-speaking (76%), and male (67%). Living arrangements suggested that a significant proportion of people lived alone (about 30%). Whereas 14% of participants did not complete high school, 62% had a postsecondary degree including a university degree (28%). Income was relatively low, as half the sample earned less than 30,000 Canadian dollars annually, mostly from pensions or government insurance programs (70%); 32% had a household income less than $30,000. Data on severity of injury showed that 33% of the sample sustained a complete lesion and 58% had an injury at the thoracolumbar level (paraplegia). People with at least 1 year of community living could participate in the survey. Their mean age was around 50 years (range, 18-90) with a mean duration of injury exceeding 18 years (range, 1-81).
Table 1. Demographic information on all participants with a traumatic (TR) or nontraumatic (NT) SCI.
| Category variables |
All participants (N = 1,549) % (95% CI) |
TR lesion (n = 1,137) % (95% CI) |
NT lesion (n = 412) % (95% CI) |
Pa |
| Canadian regions | NS | |||
| Atlantic | 10.1 (9-12) | 10.2 (9-12) | 10.0 (7-13) | |
| Quebec | 25.6 (23-28) | 24.2 (22-27) | 29.4 (25-34) | |
| Ontario | 22.3 (20-25) | 21.5 (19-24) | 24.5 (20-29) | |
| Prairies | 22.9 (21-25) | 24.1 (22-27) | 19.4 (16-24) | |
| British Columbia | 19.1 (17-21) | 20.0 (18-22) | 16.7 (13-21) | |
| Location of residence (population) | .0506 | |||
| >100,000 | 62.2 (58-63) | 60.5 (58-63) | 67.1 (62-72) | |
| 10,000-100,000 | 16.5 (14-18) | 17.6 (15-20) | 13.4 (10-17) | |
| <10,000 | 21.3 (19-23) | 21.9 (20-24) | 19.5 (16-24) | |
| Ethnicity | NS | |||
| Majority (White) | 91.4 (90-93) | 92.0 (90-93) | 90.0 (87-93) | |
| Minorities | 8.6 (7-10) | 8.0 (7-10) | 10.0 (7-13) | |
| Language preference | .032 | |||
| French | 24.3 (22-27) | 22.9 (20-25) | 28.2 (24-33) | |
| English | 75.7 (73-78) | 77.1 (75-80) | 71.8 (67-76) | |
| Gender | <.001 | |||
| Male | 67.2 (65-70) | 70.9 (68-73) | 57.0 (52-62) | |
| Female | 32.8 (30-35) | 29.1 (27-32) | 43.0 (38-48) | |
| Living arrangement | .029 | |||
| Single individual living with others | 5.9 (5-7) | 6.3 (5-8) | 4.9 (3-8) | |
| Single individual living alone | 26.0 (24-28) | 26.9 (24-30) | 23.5 (20-28) | |
| Living with spouse/partner | 40.8 (38-43) | 39.6 (37-42) | 44.2 (39-49) | |
| Parent living with spouse or partner and children | 10.1 (9-12) | 10.4 (9-12) | 9.5 (7-13) | |
| Single parent living with children | 5.2 (4-6) | 5.9 (5-7) | 3.4 (2-6) | |
| Child living with 2 parents with or without siblings | 8.5 (7-10) | 8.4 (7-10) | 9.2 (7-13) | |
| Other | 2.5 (2-3) | 2.0 (1-3) | 3.6 (2-6) | |
| Undeclared | 0.8 (0-1) | 0.5 (0-1) | 1.7 (1-4) | |
| Marital status | NS | |||
| Married | 41.8 (39-44) | 41.0 (38-44) | 43.9 (39-49) | |
| Common-law | 9.7 (8-11) | 9.4 (8-11) | 10.4 (8-14) | |
| Widowed, separated, or divorced | 18.2 (16-20) | 18.0 (16-20) | 18.7 (15-23) | |
| Single, never married | 29.4 (27-32) | 31.0 (28-34) | 24.8 (21-29) | |
| Undeclared | 1.0 (1-2) | 0.5 (0-1) | 2.2 (1-4) | |
| Education level | NS | |||
| Less than high school | 14.3 (13-16) | 13.9 (12-16) | 15.5 (12-19) | |
| High school | 23.3 (21-26) | 23.7 (21-26) | 22.4 (19-27) | |
| Postsecondary education | 34.8 (32-37) | 34.0 (31-37) | 36.9 (32-42) | |
| University | 27.6 (25-30) | 28.4 (26-31) | 25.1 (21-30) | |
| Personal incomeb | <.001 | |||
| <$30,000 | 50.7 (48-53) | 48.1 (45-51) | 58.1 (53-63) | |
| $30,000 to $59,999 | 30.6 (28-33) | 31.0 (28-34) | 29.7 (25-35) | |
| $60,000 and over | 18.7 (17-21) | 21.0 (18-24) | 12.2 (9-16) | |
| Household incomeb | .007 | |||
| <$30,000 | 32.1 (30-35) | 30.3 (27-33) | 37.2 (32-43) | |
| $30,000 to $59,999 | 28.5 (26-31) | 27.7 (25-31) | 30.6 (26-36) | |
| $60,000 and over | 39.5 (37-42) | 41.9 (39-45) | 32.2 (27-38) | |
| Income sourcesc | ||||
| Wage/salary | 26.2 (24-28) | 28.9 (26-32) | 18.7 (15-23) | <.001 |
| Government pension | 27.8 (26-30) | 25.5 (23-28) | 34.0 (29-39) | <.001 |
| Employer pension | 11.6 (10-13) | 9.8 (8-12) | 16.7 (13-21) | <.001 |
| Vehicle insurance | 9.7 (8-11) | 12.5 (11-15) | 1.9 (1-4) | <.001 |
| Provincial program | 11.6 (10-13) | 10.4 (9-12) | 14.8 (12-19) | .008 |
| Federal program | 14.8 (13-17) | 14.6 (13-17) | 15.3 (12-19) | NS |
| Do not want to answer | 7.6 (6-9) | 6.9 (5-9) | 9.7 (7-13) | NS |
| Lesion severity | <.001 | |||
| Complete | 33.3 (31-36) | 39.1 (36-42) | 17.5 (14-22) | |
| Incomplete | 66.7 (64-69) | 60.9 (58-64) | 82.5 (78-86) | |
| Lesion level | <.001 | |||
| Paraplegia | 57.8 (55-60) | 50.3 (47-53) | 78.6 (74-82) | |
| Tetraplegia | 42.2 (40-45) | 49.7 (47-53) | 21.4 (18-26) | |
| AISd | <.001 | |||
| A | 36.7 (34-39) | 42.8 (40-46) | 19.9 (16-24) | |
| B | 7.5(6-9) | 9.1 (7-11) | 3.2 (2-5) | |
| C | 19.5 (18-22) | 18.3 (16-21) | 22.8 (19-27) | |
| D | 20.6 (19-23) | 15.0 (13-17) | 35.9 (31-41) | |
| E | 2.4(2-3) | 1.5 (1-2) | 4.9 (3-8) | |
| Undetermined | 13.3 (12-15) | 13.3 (11-15) | 13.3 (10-17) | |
| Scale variables | Mean (SD) | Mean (SD) | Mean (SD) | |
| Age | 49.6 (13.9) | 48.3 (13.3) | 53.1 (14.9) | <.001 |
| Years since injury | 18.5 (14.3) | 18.5 (13.1) | 18.7 (17.1) | NS |
| Age at injury, years | 31.1 (17.0) | 29.9 (14.9) | 34.5 (21.6) | <.001 |
Significance or not statistically significant (NS) between people with a TR or NT lesion, chi-square (category variables) or t test (scale variables).
Percentage of those who answered the question. Income is given in Canadian dollars.
The participants could choose all answers that applied to their situation.
The American Spinal Injury Association Impairment Scale (AIS) was evaluated indirectly from participants’ answers about their lesion and sensorimotor and mobility capabilities.
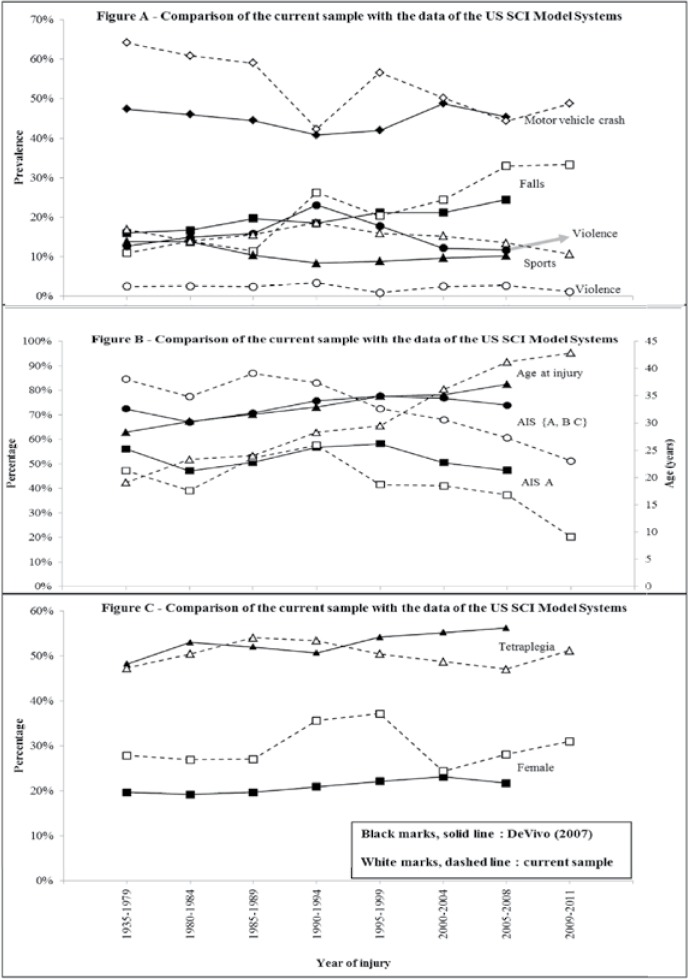
Because the survey recruited participants who sustained their injury in different decades, there are huge variations in the sample for characteristics such as cause, type, and severity of injury as well as age at injury. Figure 1 shows these variations and compares the sample information with data reported from the SCI Model Systems program in the United States.17 Motor vehicle accidents remained the leading cause of SCI, even though they decreased from over 60% (before 1980) to below 50% in the last decade (2002-2011) in Canada and remained relatively stable over time (40%-50%) in the United States (Figure 1A). Falls causing SCI rose since the late 1980s in both Canada and the United States. The major difference between the Canadian and American counterpart data was SCIs caused by violence; these SCIs were stable below 4% in the current sample but reached 14% to 27% in the United States for some decades of injury. Two additional major trends over time were observed in the current sample regarding the severity and age at injury, namely a large decline in more severe injuries (AIS ABC) from 85% to 55% in the last 30 years, and a constant increase in age at injury from about 20 to 25 years to more than 40 years in the more recent period.
Figure 1. Comparisons between survey data and those of the US SCI Model Systems (from DeVivo and Chen 2011).17.
Comparisons between people with a traumatic SCI (TR) and nontraumatic SCI (NT) revealed major differences; this points up the importance of separating these subsamples in the analyses. There was a significantly higher proportion of single individuals living alone (44%), women (43%), and older people (53 ± 15 years) in the NT sample compared to the TR sample. Their income was lower and more of it came from a government pension (34%). Due to a difference in the cause of injury (disease vs trauma), a significantly higher proportion of injuries in the NT sample was incomplete (82%) and located in the thoracolumbar region (78%), leading to paraplegia in the NT sample.
Expressed and met needs
Community living soon after discharge from rehabilitation brings about major life changes, and people with SCI expressed their needs in various ways. Needs for equipment and technical aids, health care, short-distance transportation, accessible housing, and SCI-specialized health care (Table 2) were expressed by almost all survey participants (TR >85%; NT >70%). Other needs were expressed by about half the participants and were related to attendant care, income support, healthy living, and case management and, to a lesser extent, emotional counselling, job training, and peer support. Notably, significant differences exist in needs based on the type of lesion, particularly for attendant care, accessible housing, long-distance transportation, income support, and job training (difference of proportions between TR and NT groups, 12% ≤ d ≤ 18%; P ≤ .001).
Table 2. Percentage of participants (95% CI) with a traumatic (TR) or nontraumatic (NT) SCI expressing needs and having their needs met (to a great extent or more).
| Expressed needsa | Met needsb | |||||
| SCI-related needs | TR lesion (n = 1,137) % (95% CI) | NT lesion (n = 412) % (95% CI) | Pc | TR lesion (n = 1,137) % (95% CI) | NT lesion (n = 412) % (95% CI) | Pc |
| Equipment and technical aids | 92.6 (91-94) | 81.8 (78-85) | <.001 | 74.7 (72-77) | 73.3 (68-78) | NS |
| General health care | 90.0 (88-92) | 85.9 (82-89) | .017 | 72.4 (70-75) | 74.9 (70-80) | NS |
| Short-distance transportation | 87.1 (85-89) | 76.9 (73-81) | <.001 | 78.6 (76-81) | 75.7 (70-80) | NS |
| Accessible housing | 86.5 (84-88) | 71.4 (67-76) | <.001 | 81.1 (78-83) | 73.8 (68-79) | .007 |
| SCI-specialized health care | 86.5 (84-88) | 75.7 (71-80) | <.001 | 60.5 (57-64) | 64.7 (59-70) | NS |
| Long-distance transportation | 73.1 (70-76) | 54.9 (50-60) | <.001 | 58.7 (55-61) | 58.0 (51-65) | NS |
| Attendant care | 56.8 (54-60) | 39.3 (35-44) | <.001 | 75.0 (71-79) | 71.4 (63-79) | NS |
| Income support | 56.6 (54-59) | 43.9 (39-49) | <.001 | 36.9 (33-41) | 30.8 (24-38) | NS |
| Healthy living and leisure programs | 52.3 (49-55) | 51.9 (47-56) | NS | 40.7 (37-45) | 35.4 (29-42) | NS |
| Case management | 51.1 (48-54) | 44.4 (40-49) | .012 | 54.2 (50-59) | 50.6 (43-58) | NS |
| Emotional counselling | 36.3 (34-39) | 37.6 (33-43) | NS | 43.3 (38-49) | 43.1 (35-52) | NS |
| Job training | 33.2 (31-36) | 19.9 (16-24) | <.001 | 48.1 (42-54) | 34.9 (24-48) | .039 |
| SCI peer support | 31.5 (29-34) | 25.7 (22-30) | .016 | 55.7 (50-61) | 41.9 (32-53) | .014 |
Note: Data are listed in decreasing order of the proportion of participants with traumatic injury who reported their needs as met.
Participants answered yes to the question, “Since leaving the hospital or rehabilitation centre, have you had such a need?”
Percentage of people who had such a need met to a great extent or more.
NS = not statistically significant between people with a TR vs NT lesion. Significance of difference from persons with a traumatic SCI determined by chi-square test.
About three-quarters of the sample indicated that their needs in critical domains (equipment and technical aids, health care, transportation, and accessible housing) were met (to a great extent or completely) to support community living. This proportion of met to unmet needs decreased, and less than half the participants (<50%) who had needs for income support, healthy living, emotional counselling, or job training considered them met at the moment of the survey. Whereas there was a difference between the TR and NT groups in the expression of needs, the extent of met needs did not vary significantly, except for accessible housing, job training, and peer support.
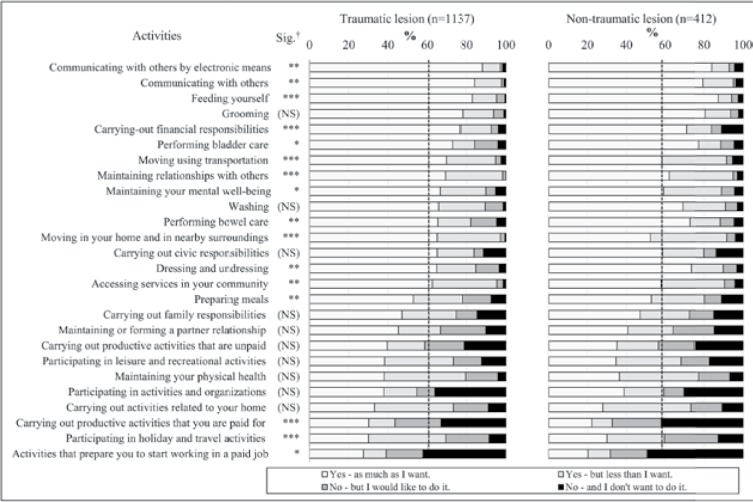
Community participation
Data on community participation relates to person-perceived participation based on personal choices and preferences. In many daily activities and social roles (15 and 14 out of 26 activities in the TR and NT groups, respectively), more than 60% of people indicated that they participated as much as they wanted (Figure 2). More attention should be placed on activities that are not carried out or are carried out less than wanted (eg, partner relationships, productive activities/ work, recreation, holidays and travel, maintaining physical health). Moreover, based on personal choices, a substantial proportion of participants (30%-40%) indicated that they did not want to participate in activities related to work or community organizations. Differences between the TR and NT groups varied significantly, particularly in activities related to mobility, feeding, holidays, and work.
Figure 2. Bar graphs representing the variation in the extent of participation in 26 activities in participants with a traumatic or nontraumatic lesion (data sorted by activities in decreasing order of percentage of participants with a traumatic lesion, responding “Yes - as much as I want”). Dashed lines represent the mean proportion of participants who responded “Yes - as much as I want” across the 26 items. † Sig. = significant difference between traumatic and nontraumatic lesion determined by chi-square test. *P ≤ .05; **P ≤ .01; ***P ≤ .001; NS = not significant.
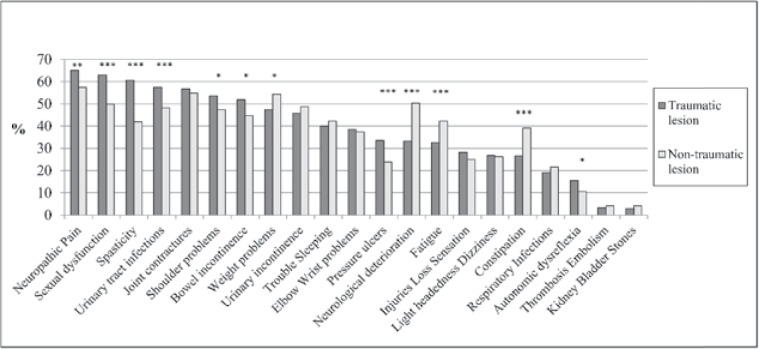
Secondary health conditions
The occurrence of SHCs (Figure 3) is noticeable in both subsamples (TR and NT). Neuropathic pain is the most common complication, but the occurrence of several complications exceeds 50%, mostly in the TR group (sexual dysfunction, spasticity, urinary tract infections, joint contractures, shoulder problems, bowel incontinence). Several differences were apparent between the TR and NT subsamples; prevalence was usually higher in the TR group, but a few SHCs were more prevalent in the NT group (weight problems, neurological deterioration, fatigue, constipation).
Figure 3. Occurrence of secondary health complications in the previous 12 months for participants with a traumatic or nontraumatic SCI. Significant difference between traumatic and nontraumatic lesion determined by chi-square test. * P ≤ .05; ** P ≤ .01; *** P ≤ .001.
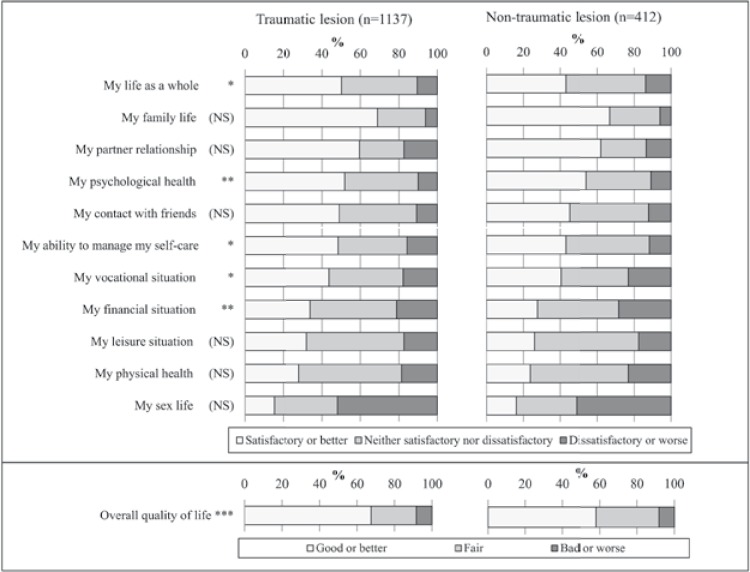
Quality of life and life satisfaction
When quality of life was considered as an overall concept, about 60% (NT group) and 70% (TR group) of the participants reported good or very good quality of life (Figure 4). Inspection of data based on dimensions of life satisfaction suggested a variation by domains. A higher proportion of participants expressed satisfaction with family life, partner relationships, psychological health, and contacts with friends, but a significant proportion expressed dissatisfaction with domains such as their vocational and financial situation, recreation or physical health, and particularly with their sex life. Slight differences between the TR and NT groups were observed in a few life domains that had a potential influence on overall quality of life, as indicated by a higher proportion of people in the TR group who indicated good quality of life.
Figure 4. Bar graphs of the satisfaction with life domains as measured by the Life Satisfaction Questionnaire (LiSAT-11) and a single question rating overall quality of life in participants with a traumatic or nontraumatic SCI. Significant difference between traumatic and nontraumatic lesion determined by chi-square test. * P ≤ .05; ** P ≤ .01; NS = not significant.
Discussion
As much as possible, rehabilitation prepares people with SCI to face challenges related to returning to community living, but this process requires resilience, effort, and adequate support. In some cases, despite essential support from caregivers, other formal sources of support are needed. The SCICS is one the first studies to simultaneously describe and analyze needs for services expressed by people with TR and NT SCI throughout the course of community integration and to document the state of community living (eg, SHCs, community participation, quality of life). Initial findings of this study suggest that (a) some expressed needs to support community living are met to a great extent for a substantial proportion of people with SCI; (b) SHCs remain highly prevalent (≥50% in the previous 12 months) particularly in pain, sexual dysfunction, and musculoskeletal disorders; (c) the extent of community participation based on values and preference varies tremendously among daily activities and social roles; and (d) some dimensions of quality of life are rated positively (eg, family life) while others are greatly disrupted (eg, sex life and physical health).
Characteristics of the sample were compared to the Canadian population as described in the Canadian Community Health Survey (CCHS, n = 57,462 adults).18 Not surprisingly, the current sample contained more males (71% vs 49%), more middle-aged adults (52% vs 36%), fewer people living with spouse/partner/children (50% vs 57%), fewer people with income from wages/salary (31% vs 72%), and a similar proportion of people with postsecondary education (64% vs 60%). However, data from a subsample of the CCHS18 comprising 355 adults with a neurological condition caused by SCI had numbers similar to the current sample for many variables (living arrangement, marital status, salary as source of income, education), suggesting representativeness of the sample in Canada, although the current sample contained slightly more males (71% vs 60%) and fewer people aged 65 years or over (11% vs 27%).
Comparisons with the SCI Models in the United States showed important differences between the US cohort and the current sample. Although these might be explained by methodological considerations (eg, differences in study design and data collection method, sampling biases), some should be considered as actual differences between Canada and the United States. On the one hand, neither sample is population-based; the rehabilitation facilities associated with the US Model Systems record about 15% of all people with a new injury and probably those with a more severe injury, whereas such a data collection system does not exist in Canada and the SCICS participants might be representative of a broader group of individuals receiving care at different institutions. Moreover, the current sample is based on self-selected participation rather than recruitment from a clinical point of entry (the basis of the SCI Model Systems), which could have created a selection bias. On the other hand, actual differences between the 2 countries must be acknowledged, such as the cause of injury (significantly more violence in the US cohort), severity of injury, and ethnicity between the cohorts, which makes it difficult to determine whether the characteristics of the 2 samples allow generalization or comparisons of results between the 2 countries.
Expressed vs met needs
Previous studies provided insight into the needs for community integration or participation, but these needs were mostly identified as a combination of services (eg, recreational programs) and influencing factors (eg accessible infrastructure). Studies on SCI-related needs4,5,19 identified the nature and extent of unmet needs in various dimensions, including health and participation issues (eg, work and occupation, sexual activity, and pain relief) similar to previous studies in Canada6,7 that also included the lack of resources to meet critical needs (income support, attendant care, and equipment). Transportation and accessible infrastructure were also top priority needs to support community living.
The current survey has the merit of identifying categories of needs for services and differentiating between expressed and met needs among people with traumatic and nontraumatic injury. Although the results indicate the fulfillment of some needs in a satisfactory manner among a majority of people with SCI, this would occur gradually over the course of community living. A study using mixed methods with a similar measure of expressed and met needs20 reported that in the first year post discharge, the fulfilment of critical needs (eg, accessible housing, transportation, home support) was under 60%. Differences in the TR versus NT groups for expressed needs might be explained by multiple factors related to demographics and living arrangement and to a difference in the etiology leading to sudden versus progressive impairments, which seem to generate limitations requiring more support and corresponding needs after a traumatic lesion. Nonetheless, only a few differences exist between the TR and NT groups in the proportion of people reporting met needs.
Secondary health conditions
Not surprisingly, people with SCI identify SHCs as major issues that need more attention. Their deleterious effects impact quality of life,21 their prevalence tends to increase over time,22 and there are potential interactions between some complications (eg, being overweight is more likely to lead to upper limb overuse and fatigue) that may affect life satisfaction.23 The high prevalence of SHCs reported in the survey is of concern. This prevalence is comparable to that in studies in the early 1990s24 and more recently in Canada,22,23 including studies reporting a high prevalence of pain in various countries25–27 (NT lesion).28 Sexual dysfunction was also reported to be a major issue,29 affecting social participation and quality of life, and is one of the most deleterious complications for many people with SCI. Among various needs for services to enhance community living, the study findings suggest that health care and services aimed at decreasing the incidence of SHCs remain a priority, given their association with mortality and life expectancy.30
Participation and quality of life
Participation can be described from a societal or personal perspective, and measures can focus on subconstructs such as accommodation, importance, assistance required, difficulty encountered, and satisfaction with involvement in daily activities or social roles.31,32 This implies that information must be captured by appropriate measures for a definite purpose. The current survey focused on a particular concept, that is, extent of participation, a subconcept relying on the person-perceived approach to participation and measured by the PADQ.13 Based on individual preferences and values, the survey results suggest that many people with SCI can carry out activities and achieve social roles as much as they want. They also indicate that some people do not want to participate in specific activities, by choice or due to a contextual situation (eg, retired from work, not living with a partner or children), and therefore an intervention to change their situation might not be necessary or a priority. However, interventions might be required for people who do not participate as much as they want or who do not participate but would like to be involved in daily activities or roles (respectively 40% and 20% of survey participants on some PDAQ items). This approach is supported by research suggesting that people with disabilities want to define participation by themselves rather than meeting various social norms,33 usually based on a more quantitative approach (eg, hours spent on activities).
Quality of life can be seen as a surrogate for appraisal of satisfaction with participation. The survey findings suggest an important parallel between satisfaction with life domains and social participation; they showed that the lowest life satisfaction was observed in domains with disruption in participation, such as the vocational or leisure situation, or were related to physical health and especially to sex life, the latter being associated with the second most prevalent SHC (sexual dysfunction). Previous studies support this finding, reporting that perceived participation and problems in participation are determinants of life satisfaction in people with SCI21,34 and dissatisfaction stems from various types of social disadvantages.35
Limitations
There are several limitations in this survey that must be acknowledged. First, the recruitment process did not allow for the selection of participants through a randomized process and the level of participation was uneven across Canada, creating a potential selection bias and a nonresponse bias. Although the geographical distribution of participants approaches the distribution of the adult population within Canada, it was not possible to calculate a representational weight for each observation. Second, the study is based on self-reported data that cannot be validated by external data, and the high number of sections and questions may have induced fatigue or boredom in participants leading to an under- or overestimation of behaviors, beliefs, and knowledge and consequently to a potential information bias. Likewise, there is a subjective component in the assessment of a need (expressed and met) influenced by personal beliefs and social norms that can also create potential upward or downward bias. Associated with such a bias is the 12-month retrospective time period to determine the occurrence of SHCs that might have been unequally estimated by participants compared to a more recent situation. Third, several questions offered predefined ordinal or Likert scale responses, and participants might have been constrained by these predefined categories; this might have led to potential central tendency (avoiding to use extreme response categories) or acquiescence (agreement with a statement when in doubt) biases. Fourth, the period to complete the survey lasted more than a week or a month for 25% and 15% of participants, respectively, which might have created a form of recall bias. Fifth, the estimation of the severity of injury relied on self-report information about motor and sensation recovery that is not as accurate as an actual medical assessment, leading to a potential misclassification of the AIS grade.
Conclusion
The SCICS sheds light on many facets of the lives of Canadians with SCI who are living in the community, including those with an NT lesion. Detailed data on met and unmet needs and main obstacles to meeting needs are reported for the first time. The study findings should help service providers understand the reality experienced by people with SCI, not only regarding unmet needs for services but also the difficulties encountered in life situations with respect to the occurrence of health conditions or reduced social participation, both of which have the potential to influence quality of life. Despite specific characteristics in the Canadian cohort depicted by the survey results, this information could be compared to findings addressing similar issues in other countries. In line with expectancies embodied in the UN Convention on the Rights of Persons with Disabilities concerning effective community participation and full citizenship for people with disabilities, the survey results should help alert policy makers to a potential gap between the living conditions of people with SCI and the services they need to ensure that such societal objectives are achieved.
Acknowledgments
The study was supported by the Rick Hansen Institute (grant number: 2010-03) and the Ontario Neurotrauma Foundation (grant number: 2010-RHI-SURVEY-812). The authors are indebted to all participants who took the survey and to the members of the Community Integration Practice Network (RHI) for their invaluable comments during the initial phase of the survey design and development. We particularly thank Ms. Cathy McGuinness and Lydia Cartar from RHI for their support throughout the survey development phases.
The authors do not have any conflicts of interest to disclose.
References
- 1.United Nations Convention on the Rights of Persons with Disabilities. http://www.un.org/disabilities/convention/conventionfull.shtml2006. [DOI] [PubMed]
- 2.World Health Organization. World report on disability. http://www.who.int/disabilities/world_report/2011/report/en/2011.
- 3.Heinemann AW, Sokol K, Garvin L, Bode RK.Measuring unmet needs and services among persons with traumatic brain injury. Arch Phys Med Rehabil. 2002;83(8):1052–1059. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy P, Lude P, Taylor N.Quality of life, social participation, appraisals and coping post spinal cord injury: A review of four community samples. Spinal Cord. 2006;44(2):95–105. [DOI] [PubMed] [Google Scholar]
- 5.Cox RJ, Amsters DI, Pershouse KJ.The need for a multidisciplinary outreach service for people with spinal cord injury living in the community. Clin Rehabil. 2001;15(6):600–606. [DOI] [PubMed] [Google Scholar]
- 6.Rick Hansen Man-in-Motion Foundation (RHMIMF). SCI Community Survey overall results. Ipsos Reid. 2004:56. [Google Scholar]
- 7.Rick Hansen Man-in-Motion Foundation (RHMIMF). SCI Forum report. Ipsos Reid. 2005:66. [Google Scholar]
- 8.Barker RN, Kendall MD, Amsters DI, Pershouse KJ, Haines TP, Kuipers P.The relationship between quality of life and disability across the lifespan for people with spinal cord injury. Spinal Cord. 2009;47(2):149–155. [DOI] [PubMed] [Google Scholar]
- 9.Noreau L, Fougeyrollas P.Long-term consequences of spinal cord injury on social participation: The occurrence of handicap situations. Disabil Rehabil. 2000;22(4):170–180. [DOI] [PubMed] [Google Scholar]
- 10.Cardol M, de Jong BA, van den Bos GA, Beelem A, de Groot IJ, de Haan RJ.Beyond disability: Perceived participation in people with a chronic disabling condition. Clin Rehabil. 2002;16(1):2735. [DOI] [PubMed] [Google Scholar]
- 11.Larsson Lund M, Nordlund A, Nygard L, Lexell J, Bernspang B.Perceptions of participation and predictors of perceived problems with participation in persons with spinal cord injury. J Rehabil Med. 2005;37(1):3–8. [DOI] [PubMed] [Google Scholar]
- 12.Post MW, de Witte LP, van Asbeck FW, van Dijk AJ, Schrijvers AJ.Predictors of health status and life satisfaction in spinal cord injury. Arch Phys Med Rehabil. 1998;79(4):395–401. [DOI] [PubMed] [Google Scholar]
- 13.Noreau L, Cobb J, Belanger LM, Dvorak MF, Leblond J, Noonan VK.Development and assessment of a community follow-up questionnaire for the Rick Hansen Spinal Cord Injury Registry. Arch Phys Med Rehabil. 2013;94(9):1753–1765. [DOI] [PubMed] [Google Scholar]
- 14.Fugl-Meyer AR, Melin R, Fugl-Meyer KS.Life satisfaction in 18- to 64-year-old Swedes: In relation to gender, age, partner and immigrant status. J Rehabil Med. 2002;34(5):239–246. [DOI] [PubMed] [Google Scholar]
- 15.Statistic Canada. Canadian Community Health Survey (CCHS) - Cycle 3.1. 2005. http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SurvId=1630&InstaId=22642&SDDS=3226
- 16.Ware J, Jr, Kosinski M, Keller SD.A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 17.DeVivo MJ, Chen Y.Trends in new injuries, prevalent cases, and aging with spinal cord injury. Arch Phys Med Rehabil. 2011;92(3):332–338. [DOI] [PubMed] [Google Scholar]
- 18.Statistics Canada, Canadian Community Health Survey (CCHS). 2010. http://www23.statcan.gc.ca/imdb-bmdi/document/3226_D7_T9_V8-eng.htm
- 19.Kennedy P, Sherlock O, McClelland M, Short D, Royle J, Wilson C.A multi-centre study of the community needs of people with spinal cord injuries: The first 18 months. Spinal Cord. 2010;48(1):15–20. [DOI] [PubMed] [Google Scholar]
- 20.Beauregard L, Guindon A, Noreau L, Lefebvre H, Boucher N.Community needs of people living with spinal cord injury and their family. Top Spinal Cord Inj Rehabil. 2012;18(2):122–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammell KRW.Spinal cord injury rehabilitation research: Patient priorities, current deficiencies and potential directions. Disabil Rehabil. 2010;32(14):1209–1218. [DOI] [PubMed] [Google Scholar]
- 22.Hitzig SL, Campbell KA, McGillivray CF, Boschen KA, Craven BC.Understanding age effects associated with changes in secondary health conditions in a Canadian spinal cord injury cohort. Spinal Cord. 2010;48(4):330–335. [DOI] [PubMed] [Google Scholar]
- 23.Hetz SP, Latimer AE, Arbour-Nicitopoulos KP, Martin Ginis KA.Secondary complications and subjective well-being in individuals with chronic spinal cord injury: Associations with self-reported adiposity. Spinal Cord. 2011;49(2):266–272. [DOI] [PubMed] [Google Scholar]
- 24.Levi R, Hultling C, Nash MS, Seiger A.The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia. 1995;33(6):308–315. [DOI] [PubMed] [Google Scholar]
- 25.Ataoglu E, Tiftik T, Kara M, Tunc H, Ersoz M, Akkus S.Effects of chronic pain on quality of life and depression in patients with spinal cord injury. Spinal Cord. 2013;51(1):23–6 [DOI] [PubMed] [Google Scholar]
- 26.Budh CN, Osteraker AL.Life satisfaction in individuals with a spinal cord injury and pain. Clin Rehabil. 2007;21(1):89–96. [DOI] [PubMed] [Google Scholar]
- 27.Modirian E, Pirouzi P, Soroush M, Karbalaei-Esmaeili S, Shojaei H, Zamani H.Chronic pain after spinal cord injury: Results of a long-term study. Pain Med. 2010;11(7):1037–1043. [DOI] [PubMed] [Google Scholar]
- 28.Werhagen L, Hultling C, Molander C.The prevalence of neuropathic pain after non-traumatic spinal cord lesion. Spinal Cord. 2007;45(9):609–615. [DOI] [PubMed] [Google Scholar]
- 29.Anderson KD, Borisoff JF, Johnson RD, Stiens SA, Elliott SL.The impact of spinal cord injury on sexual function: Concerns of the general population. Spinal Cord. 2007;45(5):328–337. [DOI] [PubMed] [Google Scholar]
- 30.Krause JS, Saunders LL.Health, secondary conditions, and life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2011;92(11):1770–1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Noreau L, Fougeyrollas P, Post M, Asano M.Participation after spinal cord injury: The evolution of conceptualization and measurement. J Neurol Phys Ther. 2005;29(3):147–156. [DOI] [PubMed] [Google Scholar]
- 32.Gray DB, Hollingsworth HH, Stark SL, Morgan KA.Participation survey/mobility: Psychometric properties of a measure of participation for people with mobility impairments and limitations. Arch Phys Med Rehabil. 2006;87(2):189–197. [DOI] [PubMed] [Google Scholar]
- 33.Hammel J, Magasi S, Heinemann A, Whiteneck G, Bogner J, Rodriguez E.What does participation mean? An insider perspective from people with disabilities. Disabil Rehabil. 2008;30(19):1445–1460. [DOI] [PubMed] [Google Scholar]
- 34.Lund ML, Nordlund A, Bernspang B, Lexell J.Perceived participation and problems in participation are determinants of life satisfaction in people with spinal cord injury. Disabil Rehabil. 2007;29(18):1417–1422. [DOI] [PubMed] [Google Scholar]
- 35.Hammell KW.Exploring quality of life following high spinal cord injury: A review and critique. Spinal Cord. 2004;42(9):491–502. [DOI] [PubMed] [Google Scholar]