Abstract
Objective:
This study examines patient factors to identify risks of 12-month mortality following periprosthetic femur fractures. Hospital charges were analyzed to quantify the financial burden for treatment modalities.
Methods:
Data were retrospectively analyzed from a prospective database at a university hospital setting. One-hundred and thirteen patients with a periprosthetic fracture of the proximal or distal femur were identified. Risk factors for 12-month mortality were analyzed, and financial data were compared between the various treatment modalities.
Results:
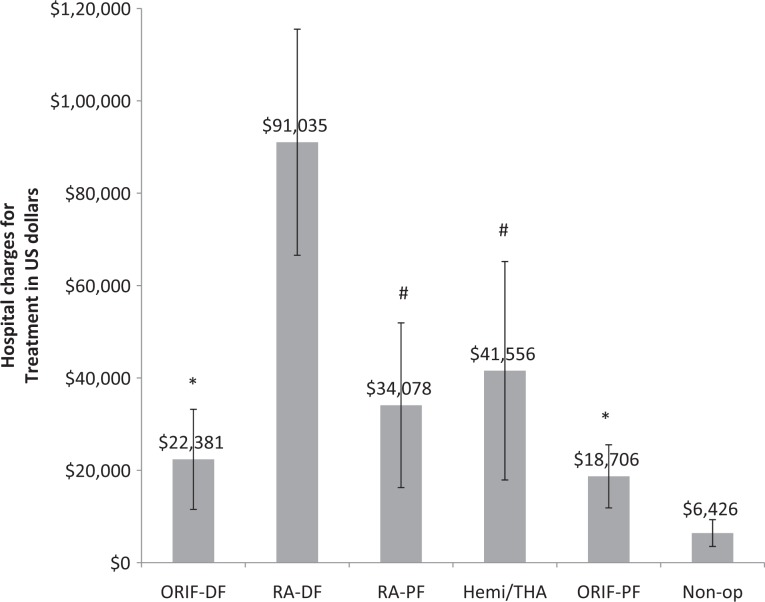
In all, 14% of patients died (16 of 113) within 3 months and the 1-year mortality was 17.7% (20 of 113). Patients who died within 1 year had higher hospital charges (US$33 880 ± 25 051 vs US$22 886 ± 16 841; P = .01) and were older (87.6 ± 8.5 vs 81.5 ± 8.6; P = .004). Logistic regression analysis revealed age was the only significant predictor of 1-year mortality (P = .029, odds ratio 1.1). Analysis of financial data revealed 4 distinct groups (P < .05 between groups). Distal femoral revision arthroplasty (RA-DF) generated the highest hospital charges of US$91 035 ± 25 579 (n = 3). The second most highly charged group included proximal femoral fractures treated with revision arthroplasty (US$34 078 ± 17 832; n = 20) and hemi/total hip arthroplasty (THA; US$41 556 ± 23 651; n = 8). The third most charged group underwent open reduction internal fixation of the proximal (US$18 706 ± 6829; n = 35) and distal (US$22 381 ± 10 835; n = 35) femur. Nonoperative treatment generated the lowest charges (US$6426 ± 2899; n = 11). On average, the hospital lost money treating patients with RA-DF (US$−19 080 ± 2022 per patient) and hemi/THA (US$−6594 ± 9305 per patient), while all other treatment groups were profitable.
Conclusion:
One-year mortality after periprosthetic femur fractures was 17.7%, is mostly influenced by age, and 80% of deaths occur within 3 months. Patients treated with primary/revision arthroplasty generate more hospital charges than internal fixation. The average patient treated with revision arthroplasty of the distal femur or hemi/THA for a periprosthetic femur fractures resulted in net financial losses for the hospital.
Keywords: periprosthetic femur fracture, mortality, geriatric fracture, hospital charges
Introduction
Periprosthetic fractures occur around or adjacent to prosthetic joints or orthopedic implants.1 Currently, 0.8% to 1.1% of total hip arthroplasty (THA) and 0.5% to 1.1% of total knee arthroplasty (TKA) patients will experience a periprosthetic fracture in the first 5 years from surgery, and these numbers are expected to increase.2–6 The indications for THA are expanding, leading to more implants in younger patients, as well as in older adults. The number of TKAs is also projected to increase continuously.4,7 Increased life expectancy combined with the increased numbers of arthroplasties is contributing to an increase in the number of periprosthetic fractures both in the United States and worldwide.3
Periprosthetic fractures are associated with significant morbidity and mortality.8,9 Recent literature suggests an 11% 1-year mortality rate after periprosthetic femur fractures, with age and type of surgery potentially influencing mortality risk.8,9 However, an investigation specifically looking for patient factors influencing risks of 1-year mortality has not been undertaken. Furthermore, many treatment options exist for periprosthetic fractures including nonoperative management, surgical management with plate fixation or intramedullary fixation, and revision arthroplasty.10 The financial burden related to these various treatments has not been reported in the United States. Analysis of the hospital charges for these treatments and factors associated with increased 1-year mortality may help define the highest value procedures, assist with prognostic counseling, and help guide preoperative decision making.
The lack of published data on these aspects of care has prompted us to undertake this investigation. The purpose of this study is to report 1-year mortality rates after periprosthetic fractures of the femur, to investigate patient factors associated with increased risk of mortality and to examine the financial burden of various treatment modalities.
Methods
The Geriatric Fracture registry at our center was reviewed from July 2008 through July 2011 for patients presenting with periprosthetic fractures of the proximal or distal femur. The registry contains demographic and clinical outcomes data for all patients hospitalized with a fracture at our hospital, which is affiliated with the university medical center. Data are collected on all major fractures prospectively for quality management. Periprosthetic fractures were defined as fractures around or adjacent to prosthetic joints or existing orthopedic hardware. Patients admitted with a low-energy femoral periprosthetic fracture were included in this study; patients with incomplete data or high-energy mechanisms were excluded. Fractures involving total hip implants were classified as proximal femur, and if around total knee implants, they were grouped as distal femur. In general, stable implants underwent open reduction with internal fixation, while loose or broken implants were treated with revision surgery.
For each patient in the registry, data were collected prospectively beginning at the time of admission and continuing through hospital discharge (or death). Follow-up data were collected at 1 month, 3 months, and 12 months posttreatment as part of a hospital quality management program. Parameters included Parker mobility score, Katz activities of daily living (ADL; scored 1 point for independently performing each of the following bathing, ambulation, transfers, eating, grooming, and toileting), place of residence prior to injury (home, home with assistance, assisted living home, skilled nursing facility [SNF], and other), and mortality date (obtained by chart review or telephone contact with patient’s caregivers). Charlson comorbidity index, in-hospital complications, basic demographic information, admission date, surgery date, fracture location, treatment rendered, and discharge date were also included in the database. If a patient died during admission, length of stay was calculated from admission date until date of death.
During analysis, patient primary residence was grouped into independent living (home) and dependent living (home with nursing services, assisted living home, SNF, and other). Treatments evaluated in the multivariate analysis included amputation (n = 1), hip hemiarthroplasty (n = 7), nonoperative treatment of the proximal femur (n = 6), nonoperative treatment of the distal femur (n = 5), open reduction internal fixation (ORIF) proximal femur (n = 35), ORIF of distal femur (n = 35), revision arthroplasty (n = 23; included 3 distal femoral revision arthroplasty [RA-DF] and 20 proximal femur revision arthroplasty cases), and THA (n = 1).
Financial data were also available for each hospital stay. “Charges” refer to the amount the patient’s insurance provider was billed, while “costs” refer to the financial burden carried by the hospital. During financial analysis, the amputation case (n = 1) was excluded. The final groups consisted of nonoperative treatment (n = 11; combined proximal femur and distal femur cases), ORIF proximal femur (n = 35), ORIF distal femur (n = 35), revision arthroplasty distal femur (n = 3), revision arthroplasty proximal femur (n = 20; included all cases with femoral, acetabular, or both component revision), and the hemiarthroplasty (n = 7) and THA (n = 1) cases were grouped together (hemi/THA; n = 8). Combined operating room and implant costs to the hospital were also calculated from these data. Net margin (profit/loss) was defined as total revenue collected by the hospital minus the costs associated with care of the patient to the hospital.
Binomial logistic regression analysis, student t test, Mann-Whitney U, and analysis of variance (ANOVA) for multiple groups were performed using SPSS v.20 (IBM, Chicago, Illinois). The data were tested for normality and equal variance as appropriate. Statistical significance was set as P < .05. All values are presented as mean ± standard deviation. The University Research Subjects Review Board approved this study.
Results
One hundred and thirteen patients met inclusion criteria and had follow-up through 12 months or time of death. The average patient age was 83 ± 8.88 (range 61-102 years), 22% were men (n = 25) and 78% were women (n = 88). There were 70 proximal femur fractures and 43 distal femur fractures. Racially, 93% of patients were caucasian (n = 105), 5.3% were African American (n = 6), 0.90% were Asian (n = 1), and 0.90% were other (n = 1; Table 1).
Table 1.
Basic Demographics Summary of Patients With Distal and Proximal Periprosthetic Femur Fractures.
| Patient Demographics | All Periprosthetic Fractures (n = 113) | Distal Femur (n = 43) | Proximal Femur (n = 70) |
|---|---|---|---|
| Age | 83 ± 8.8 | 81 ± 8.0 | 84 ± 9.2 |
| Sex | |||
| Male | 22% (n = 25) | 16% (n = 7) | 25.7% (n = 18) |
| Female | 78% (n = 88) | 84% (n = 36) | 74.3% (n = 52) |
| Race | |||
| White | 93% (n = 105) | 88.4% (n = 38) | 95.7% (n = 67) |
| African American | 5.3% (n = 6) | 9.3% (n = 4) | 2.9% (n = 2) |
| Asian | 0.9% (n = 1) | 2.3% (n = 1) | 0% (n = 0) |
| Other | 0.9% (n = 1) | 0% (n = 0) | 1.4% (n = 1) |
| Preinjury residence | |||
| Home | 53% (n = 60) | 67% (n = 28) | 45.7% (n = 32) |
| SNF | 26.5% (n = 30) | 16.7% (n = 7) | 33% (n = 23) |
| Home with services | 8.8% (n = 10) | 12% (n = 5) | 7.1% (n = 5) |
| Assisted living | 8.0% (n = 9) | 4.8% (n = 2) | 10% (n = 7) |
| Other | 3.5% (n = 4) | 2.3% (n = 1) | 4% (n = 3) |
Abbreviation: SNF, skilled nursing facility.
The majority of patients were admitted from home (53%, n = 60), while 26.5% of patients came from a SNF (n = 30), 8.8% lived at home with services (n = 10), 8.0% resided in an assisted living facility (n = 9), and 3.5% lived in other arrangements (n = 4; Table 1).
One-year mortality of the entire group was 17.7% (n = 20 of 113). Of these patients, 80% died within the first 3 months following their fracture (n = 16). The average hospital length of stay was 6.3 ± 8.8 days, and the average hospital charges were US$24 831 ± 18 739 (Table 2). Patients who died had their date of death used as the end of the hospital stay. In-hospital causes of death included acute renal failure (n = 3), respiratory failure (n = 1), and septic shock (n = 1). Causes of death in the first 3 months after hospital discharge included respiratory failure (n = 3), sepsis (n = 2), unclear (n = 2), pulmonary embolism (n = 1), and cancer (n = 1). Deaths between 3 and 12 months were caused by cancer (n = 2), congestive heart failure (n = 1), and coronary artery disease (n = 1).
Table 2.
Primary Residence Before Injury, Mortality Rates, Hospital Length of Stay, and Average Hospital Charges for Patients With Proximal and Distal Femoral Periprosthetic Femur Fractures.
| 12 Month Mortality, Hospital Length of Stay, and Hospital Charges | All Periprosthetic Fractures (n = 113) | Distal Femur (n = 43) | Proximal Femur (n = 70) |
|---|---|---|---|
| Mortality | |||
| By 3 months | 14.1% (n = 16) | 14.0% (n = 6) | 14.2% (n = 10) |
| By 12 months | 17.7% (n = 20) | 18.6% (n = 8) | 17.1% (n = 12) |
| Length of hospital stay, days | 6.3 ± 8.8 | 8.4 ± 13.8 | 4.97 ± 2.4 |
| Average hospital charges | US$24 831 ± 18 739 | US$25 479 ± 21 800 | US$24 434 ± 16 741 |
Patients who died within 1 year were older (87.65 ± 8.47 vs 81.5 ± 8.6; P = .004) and had higher hospital charges (US$33 880 ± 25 051 vs US$22 886 ± 16 841; P = .01) compared to patients who survived greater than 12 months. Preinjury Parker scores (alive 3.8 ± 3.01 vs died 3.75 ± 2.51; P = .89), preinjury ADL score (alive 4.45 ± 1.9 vs died 3.7 ± 2.15; P = .14), Charlson comorbidity index score (alive 2.84 ± 2.2 vs died 2.8 ± 2.02; P = .95), and hospital length of stay in days (alive 6.18 ± 9.57 vs died 6.9 ± 4.04; P = .059) did not significantly differ between patients who survived and those who were Dead within 1 year (Table 3). Patients admitted from a dependent living situation were more likely to die within 1 year compared to patients admitted from independent situations (home; 26.4%, n = 14/53 vs 10%, n = 6/60; P = .02). Patients admitted from dependent living situations were also older than patients admitted who were living independently (85.2 ± 8.32 vs 80.23 ± 8.7; P = .002). Death rates from all preinjury living situations are presented in Table 4. Two (8%) of the 25 men and 18 of the 88 women (20%) in this study died within 1 year (P = .15).
Table 3.
Patients Who Were Dead at 12 Months After Injury Were Older (P < .05) and Accrued More Hospital Charges on Average (P < .05).a
| Comparisons Between Patients Died at 12 Months After Fracture Versus Living | Alive at 12 Months (n = 93) | Died at 12 Months (n = 20) | P Value |
|---|---|---|---|
| Age | 81.5 ± 8.6 | 87.65 ± 8.47 | .004 |
| Hospital charges | US$22 886 ± 16 841 | US$33 880 ± 25 051 | .01 |
| Preinjury Parker mobility score | 3.8 ± 3.01 | 3.75 ±2.51 | .89 |
| Preinjury ADL score | 4.45 ±1.9 | 3.7 ± 2.15 | .14 |
| Charlson comorbidity index | 2.84 ± 2.2 | 2.8 ± 2.02 | .95 |
| Hospital length of stay | 6.18 ± 9.57 | 6.9 ± 4.04 | .059 |
Abbreviation: ADL, activities of daily living.
aThere were no differences in preinjury Parker mobility scores, preinjury ADL scores, Charlson scores, and hospital length of stay between patients who survived the first 12 months, and those who did not (P > .05).
Table 4.
Mortality Rates for Patients From All Living Facilities Individually.
| Primary Residence | Percentage of Dead at 12 Months | Total Number Dead at 12 Months |
|---|---|---|
| Home (n = 60) | 10 | 6 |
| Skilled nursing facility (N = 30) | 22.6 | 7 |
| Home with services (N = 10) | 20 | 2 |
| Assisted living (N = 9) | 33 | 3 |
| Other (N = 4) | 50 | 2 |
Binomial logistic regression analysis revealed that, when analyzed individually, 12-month mortality was not influenced by hospital length of stay, Charlson comorbidity index, preinjury Parker mobility score, preinjury ADL score, fracture location (proximal or distal), delirium or renal insufficiency during the hospital stay, or treatment type (P > .05 for all). Univariate analysis revealed significant interactions between living situation (P = .012), age (P = .004), and hospital cost (P = .016) as predictors of 12-month mortality. However, multivariate analysis revealed age (P = .029) to be the only significant predictor of 12-month mortality when controlling for all other factors (Table 5).
Table 5.
Univariate and Multivariate Analyses of Available Factors.a
| Predictors of 12-Month Mortality After Periprosthetic Femur Fractures | Univariate Analysis P Value | Multivariate Adjusted P Value | Odds Ratio With 95% Confidence Interval |
|---|---|---|---|
| Treatment | .827 | .888 | NS |
| Amputation (n = 1) | >.05 | >.05 | NS |
| Hemiarthroplasty of hip (n = 7) | >.05 | >.05 | NS |
| Nonoperative proximal femur (n = 6) | >.05 | >.05 | NS |
| Nonoperative distal femur (n = 5) | >.05 | >.05 | NS |
| ORIF proximal femur (n = 35) | >.05 | >.05 | NS |
| ORIF distal femur (n = 35) | >.05 | >.05 | NS |
| bRevision arthroplasty (n = 23) | >.05 | >.05 | NS |
| Total hip arthroplasty (n = 1) | >.05 | >.05 | NS |
| Renal insufficiency while hospitalized | .42 | .393 | NS |
| Delirium while hospitalized | .075 | .364 | NS |
| Hospital cost | .016 | .068 | NS |
| Age | .004 | .029 | 1.1 (1.01-1.25) |
| Fracture location (proximal vs distal | .87 | .933 | NS |
| Preinjury living situation | .012 | >.999 | NS |
| Independent (Home) | .025 | >.05 | NS |
| Dependent (all others combined) | .066 | >.05 | NS |
| Preinjury ADL score | .385 | .375 | NS |
| Preinjury Parker mobility score | .855 | .244 | NS |
| Charlson comorbidity score | .912 | .959 | NS |
| Hospital length of stay | .720 | .496 | NS |
Abbreviations: ADL, activities of daily living; NS, not significant; ORIF, open reduction internal fixation.
aIn multivariate analysis, age was the only significant predictor of 1-year mortality.
bThe revision arthroplasty group included 3 distal femur revision arthroplasty cases and 20 proximal femur cases.
Analysis of financial data for the different treatments revealed 4 distinct groups with regard to hospital charges, after ANOVA and post hoc statistics. Distal femoral revision arthroplasty generated higher hospital charges of US$91 035 ± 25 579 (n = 3) than all other treatments (ANOVA P < .05, post hoc P < .05 for all). Proximal femoral fractures treated with revision arthroplasty (US$34 078 ± 17 832; n = 20) or hemi/THA (US$41 556 ± 23 651; n = 8) had similar charges to each other (post hoc P > .05) but generated less charges than RA-DF, but higher than ORIF and nonoperative groups. Open reduction internal fixation of the proximal femur (US$18 706 ± 6829; n = 35) and distal femur (US$22 381 ± 10 835; n = 35) had similar hospital charges to each other (post hoc P > .05) but generated more charges than nonoperative treatment and less than the previous groups. The nonoperative group (US$6426 ± 2899; n = 11) generated less hospital charges than all other groups (post hoc P < .05 for all; Figure 1). The combined operating room and implant costs incurred by the hospital for the various treatment groups followed a similar pattern to overall hospital charges (Table 6). The few patients (n = 3) in this study treated with RA-DF had significantly longer hospital stays (39 ± 44 days) versus all other treatments (P < .0001). The average net margin per patient treated was positive for all treatments except RA-DF and revision hemi/THA groups (Table 7).
Figure 1.
Treatment hospital charges statistically fell into 4 distinct groups (analysis of variance [ANOVA] P < .05). Revision arthroplasty of the distal femur (RA-DF; n = 3) generated the most charges (P < .05). The nonoperative group (n = 11) generated the least charges (P < .05). *The second most costly group included revision arthroplasty of the proximal femur (n = 20) and the hemi/total hip arthroplasty (THA; n = 8) groups (P < .05). #The third most costly group was ORIF of the distal (ORIF-DF; n = 35) and proximal femur (ORIF-PF; n = 35; P < .05). ORIF indicates open reduction internal fixation.
Table 6.
Operating Room and Implant Costs Incurred by the Hospital.a
| Treatment | Operating Room/Implant Costs | Treatment Number | Post Hoc P Values |
|---|---|---|---|
| Revision arthroplasty—distal femur | US$22 377 ± 3995 | 1 | <.05 vs 2, 3, 4, 5, 6 |
| Revision arthroplasty—proximal femur | US$8691 ± 6106 | 2 | <.05 vs 1, 4, 5, 6 >.05 vs 3 |
| Hemiarthroplasty/total hip arthroplasty | US$11 144 ± 9042 | 3 | <.05 vs 1, 4, 5, 6 >.05 vs 2 |
| ORIF proximal femur | US$3722 ± 4329 | 4 | <.05 vs 1, 2, 3, 6 >.05 vs 5 |
| ORIF distal femur | US$3478 ± 1676 | 5 | <.05 vs 1, 2, 3, 6 >.05 vs 4 |
| Nonoperative treatment | US$0 ± 0 | 6 | <.05 vs 1, 2, 3, 4, 5 |
Abbreviations: ANOVA, analysis of variance; ORIF, open reduction internal fixation.
aOne-way ANOVA P < .0001. Post hoc analysis revealed 4 distinct groups based on P values <.05. Group 1: revision arthroplasty of the distal femur was more costly than every other treatment. Group 2: revision arthroplasty of the proximal femur and the hemiarthroplasty/total hip arthroplasty groups were similar to each other, but different from all other groups. Group 3: ORIF of the proximal and distal femur groups has similar costs to each other but were different from all other groups. Group 4: nonoperative treatment resulted in no implant or operating room cost to the hospital. Average operating room and implant costs accrued by the hospital for each treatment per patient.
Table 7.
Average Hospital Length of Stay and Average Net Margin (Profit/Loss) Per Patient Treated by Treatment Type.a
| Treatment | Average Hospital Length of Stay, days | Average Net Marginal Profit per Patient Treated, US$ |
|---|---|---|
| Revision arthroplasty—distal femur | 39.3 ± 45b | −19 080 ± 2022c |
| Revision arthroplasty—proximal femur | 5.5 ± 2.0 | 2838 ± 6864 |
| Hemiarthroplasty/total hip arthroplasty | 6.9 ± 3.3 | −6594 ± 9305d |
| ORIF proximal femur | 4.6 ± 2.4 | 1897 ± 3980 |
| ORIF distal femur | 6.4 ± 5.0 | 428 ± 5709 |
| Nonoperative treatment | 3.3 ± 1.2 | 1405 ± 1904 |
Abbreviations: ANOVA, analysis of variance; ORIF, open reduction internal fixation.
aProfit and length of stay for patients undergoing various treatment modalities for periprosthetic femur fractures
bPatients treated with revision arthroplasty of the distal femur had significantly longer hospital stays than all other treatments (ANOVA P < .05, post hoc P < .05 vs all other treatments).
cPatients treated with revision arthroplasty of the distal femur on average resulted in the most financial losses for the hospital (ANOVA P < .05, post hoc P < .05 vs all other treatments).
dPatients treated with revision hemi/total hip arthroplasty of the distal femur on average resulted in more financial losses than all other treatments, except distal femoral revision arthroplasty (ANOVA P < .05, post hoc P < .05 vs all other treatments).
Discussion
The 17.1% 1-year mortality rate in this study was similar to previously reported rates in patients who have been treated for native hip fractures from this registry of 21.2%11 and other published data.12 This is consistent with previous reports also suggesting that these 2 injuries have similar 1-year mortality rates.9 One-year mortality rates specifically for distal femur periprosthetic fractures have also been previously reported, with a majority occurring within 6 months.13 Proximal and distal femoral periprosthetic fractures had similar mortality rates at 1 year in our study, which was higher than proximal periprosthetic femoral fracture mortality rates of 11% reported by Bhattacharyya et al and lower than distal femoral periprosthetic 1-year mortality rates of 27% reported by Streubel et al .9,13 We also examined death rates at 3 months instead of 6 months, which revealed a large majority (80%) of these deaths occur in the time period immediately following injury and surgery. Patients surviving the first 3 months are more likely to survive the first year. These death rates are significantly higher than the expected death rates for uninjured 80-year old adults—about 6% per year.14
Although previous reports have suggested that there are lower mortality rates with revision arthroplasty versus ORIF of the proximal femur in periprosthetic femur fractures, we saw no such relationship in our study.9 One-year mortality also did not appear to be influenced by Parker mobility score, preinjury ADL score, or Charlson comorbidity index, which was surprising. When reviewing patients with Charlson scores of 1 through 4 only, there was a small, linear increase in the percentage of deaths as Charlson score increased, but it was not large enough to reach statistical significance. A larger study population may be necessary to detect these differences.
Age was the only significant factor predicting 1-year mortality when controlling for other variables, which has been reported previously as being a significant predictor.11 Also interesting was that 8% of men and 20% of women with periprosthetic femur fractures were dead at 1 year. This difference was not statistically significant, but it differs from published literature suggesting that male sex represents a significant risk factor for 1-year mortality in native hip fractures.11,15
We initially saw a relationship between different types of preinjury residence and 1-year mortality. Patients who were admitted from a dependent living situation had higher mortality rates than patients living at home independently. However, these results were confounded by age, which was significantly higher in patients living in dependent situations.
This is the first study in the United States to review hospital charges for care of periprosthetic femur fractures. In the United Kingdom, average charges have been estimated at US$30 509 but include hospital lengths of stay over 30 days.16 Our charges appear to be lower, although our hospital stays are much shorter. However, the majority of patients were discharged to skilled rehabilitation facilities, and we did not analyze the charges of rehabilitation in this study.
The charges of revision arthroplasty for distal femoral fractures should be interpreted with caution. Only 3 patients were in this group, and all 3 had prolonged hospital stays. Revision arthroplasty in general appears to be more costly than ORIF in the proximal or distal femur.
Hospital charges for primary hip fracture are influenced by many variables, including ASA class.17 Charges of care for primary hip fractures have been previously published from our center with average hospital charges being US$15 188,18 which is lower than government publications of US$42 567.19 These charges are lower than the averages in this study but may be due to variations in treatment modality, as our results demonstrate there are clear differences in hospital charges depending on the treatment.
The differences in hospital charges between treatment groups are likely multifactorial. The revision arthroplasty distal femur treatment group did have significantly higher operating room and implant costs; however, these patients also had prolonged hospital stays. Operating room/implant costs to the hospital were higher for revision arthroplasty in general compared to ORIF groups, but the differences are not large enough to account for the differences in hospital charges to payers. Generally speaking, the revision arthroplasty Diagnosis-Related Groups result in higher charges than ORIF. We did not analyze complications or ICU days between the different treatment groups in the present study.
Weaknesses of this study include its retrospective nature. The number of different treatments that resulted in some groups have a very small number of patients, especially the patients treated with revision arthroplasty of the distal femur (n = 3). Groups with fewer patients may be biased and not represent the true population averages. The number of treatment groups may also have affected our multivariate analysis, with more treatments being analyzed making it more difficult to determine whether any were significantly associated with mortality. Furthermore, financial analysis at 1 institution may not be widely applicable. Hospitals charge different amounts for the same procedures. We also do not have local or national comparison data to confirm our findings.
Conclusion
Patients with a periprosthetic femur fracture had a 17.1% 1-year mortality rate, with 80% of these deaths occurring in the first 3 months after injury in this study. Increasing age was the only significant patient factor that increased risk of mortality on multivariate analysis. Revision arthroplasty of periprosthetic femur fractures generated higher hospital charges compared to ORIF, and the average patient treated with revision arthroplasty of the distal femur or revision hemi/THA for a periprosthetic fracture actually resulted in net financial losses for the hospital. A larger sample size and additional study will be required to further assess this growing problem.
Footnotes
Authors’ Note: The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. Institutional IRB approval was obtained for this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article: Cram is supported by a K24 award from NIAMS (AR062133) and by the Department of Veterans Affairs.
References
- 1. Noor S, Pridham C, Fawcett T, et al. Finite element analysis modelling of proximal femoral fractures, including post-fixation periprosthetic fractures. Injury. 2013;44 (6):791–795. [DOI] [PubMed] [Google Scholar]
- 2. Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011;93 (1):96–101. [DOI] [PubMed] [Google Scholar]
- 3. Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007;38 ( 6 ):651–654. [DOI] [PubMed] [Google Scholar]
- 4. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89 (4):780–785. [DOI] [PubMed] [Google Scholar]
- 5. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30 ( 2 ):183–190. [DOI] [PubMed] [Google Scholar]
- 6. Cook RE, Jenkins PJ, Walmsley PJ, Patton JT, Robinson CM. Risk factors for periprosthetic fractures of the hip: a survivorship analysis. Clin Orthop Relat Res. 2008;466 (7):1652–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012;308 (12):1227–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lindahl H, Oden A, Garellick G, Malchau H. The excess mortality due to periprosthetic femur fracture. A study from the Swedish national hip arthroplasty register. Bone. 2007;40 (5):1294–1298. [DOI] [PubMed] [Google Scholar]
- 9. Bhattacharyya T, Chang D, Meigs JB, Estok DM II, Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007;89 (12):2658–2662. [DOI] [PubMed] [Google Scholar]
- 10. McGraw P, Kumar A. Periprosthetic fractures of the femur after total knee arthroplasty. J Orthop Traumatol. 2010;11 ( 3 ):135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010;1 (1):6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302 (14):1573–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Streubel PN, Ricci WM, Wong A, Gardner MJ. Mortality after distal femur fractures in elderly patients. Clin Orthop Relat Res. 2011;469 (4):1188–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Administration SS. Actuarial Life Table; 2009. www.ssa.gov/oact/STATS/table4c6.html. Accessed June 15, 2013.
- 15. Paksima N, Koval KJ, Aharanoff G, et al. Predictors of mortality after hip fracture: a 10-year prospective study. Bull NYU Hosp Jt Dis. 2008;66 (2):111–117. [PubMed] [Google Scholar]
- 16. Phillips JR, Boulton C, Morac CG, Manktelov AR. What is the financial cost of treating periprosthetic hip fractures? Injury. 2011;42 (2):146–149. [DOI] [PubMed] [Google Scholar]
- 17. Garcia AE, Bonnaig JV, Yoneda ZT, et al. Patient variables which may predict length of stay and hospital costs in elderly patients with hip fracture. J Orthop Trauma. 2012;26 (11):620–623. [DOI] [PubMed] [Google Scholar]
- 18. Kates SL, Blake D, Bingham KW, Kates OS, Mendelson DA, Friedman SM. Comparison of an organized geriatric fracture program to United States government data. Geriatr Orthop Surg Rehabil. 2010;1 (1):15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Barrett M WE, Whalen D. 2007. HCUP Nationwide Inpatient Sample (NIS) Comparison Report. HCUP Methods Series Report # 2010-03. Online; 2010 http://www.hcup-us.ahrq.gov/reports/methods/2010_03.pdf. Accessed June 15, 2013.