Abstract
Hip and spine fractures represent just a portion of the burden of osteoporosis; however, these fractures require treatment and often represent a major change in lifestyle for the patient and their family. The orthopedic surgeon plays a crucial role, not only in the treatment of these injuries but also providing guidance in prevention of future osteoporotic fractures. This review provides a brief epidemiology of the fractures, details the surgical techniques, and outlines the current treatment guidelines for orthopedic surgeons.
Keywords: fragility fractures, geriatric trauma, osteoporosis, spine surgery, trauma, surgery
Osteoporotic Hip and Spine Fractures
Hip and spine fractures represent just a portion of the burden of osteoporosis. However, these fractures require treatment and often represent a major change in lifestyle for the patient and their family. The orthopedic surgeon plays a crucial role, not only in the treatment of these injuries but also providing guidance in prevention of future osteoporotic fractures.
Hip Fractures—Epidemiology
Hip fractures in the elderly patients are a growing epidemic as the population ages. This, in part, is likely due to the greater prevalence of osteoporosis.1 There are no boundaries with hip fractures as they affect individuals regardless of age, gender, or race. Although these fractures represent only a small portion of osteoporotic fractures (14%), hip fractures represent 72% of the cost expenditure or are projected to cost over 18.2 billion dollars by 2025.1 It is not just the burden of hip fracture fixation affecting health care costs. The aftercare and subsequent decline in independence and heath come into the picture. The underlying cause of the fracture needs to be addressed with the patient and their family. By treating osteoporosis in patients with prior fractures, there was a 50% reduction in risk of future fractures.2
Patients and their families need to be counseled appropriately before surgery regarding return to prefracture mobility. The risk of not regaining mobility was noted to be highest in those independent ambulators without use of assistive devices.3 Information regarding outcomes after hip fracture surgery should be discussed prior to the surgery with the patient and their family.
It is well known that hip fractures represent an injury with increased morbidities and mortality. The complications after hip fracture range from admission to an intensive care unit, deep venous thrombosis, wound dehiscence, bedsores, pneumonia, failure of fixation, and death.4–6 Pugely et al developed a 30-day risk calculator for morbidity and mortality following hip fracture surgery.7 Those factors associated with an increased morbidity and mortality included age greater than 80 and male sex.7 This model supported previous studies regarding increased mortality after hip fractures in the male gender.
The Surgical Treatment of Osteoporotic Hip Fractures
With rare exception, the treatment of an osteoporotic hip fracture requires surgery. At times, there are conflicting opinions regarding preoperative clearance. A few studies have documented that preoperative cardiac testing in patients with hip fracture delays surgery and increases costs without improving morbidity or mortality.8,9 It is important there not be excessive tests that will not impact the outcome and instead contribute to a significant delay in surgery. There should be identification of treatable risk factors prior to surgery and optimization of the patient. Management of the elderly patients with hip fracture requires communication and group effort between anesthesia, the surgeon, and the medicine team.10 With the increased burden of hip fractures due to the aging population, the establishment of a geriatric fracture service should be considered. Not only can the outcomes of patients with fracture be improved, the protocols in place provide guidance for common issues. A goal of fracture fixation in the geriatric patient should be avoidance of complications and need for reoperation by adhering to solid surgical principles.10–17
The implant selection for the treatment of geriatric proximal femur fractures should include evaluation of the fracture pattern, preexisting bone quality, mobility, and mental status, presence of arthritis, and surgeon experience. In addition, there should be consideration of implant cost and outcomes of specific implants.
Femoral neck fractures
Femoral neck fracture treatment should consider the fracture type, patient physiologic age, and presence of symptomatic arthritis. Nondisplaced fractures and valgus-impacted fractures can be treated with cannulated screw fixation. It is the displaced fractures that include more options: closed reduction and percutaneous pinning, closed/open reduction and fixation with a sliding hip screw (with or without a derotation screw), hemiarthroplasty (HA), or total hip arthroplasty (THA). The basic tenets of fixation of femoral neck and peritrochanteric fractures with a sliding hip screw, including preoperative planning to use the correct angle implant, anatomic reduction in the fracture, and having a tip apex distance of 25 mm or less, are important details for success with these fractures18,19 (Figures 1 and 2).
Figure 1.
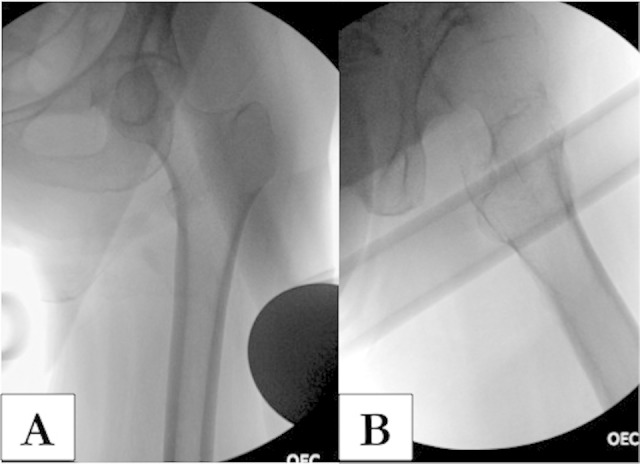
A and B, Intraoperative fluoroscopic imaging of acceptable anterior–posterior (AP) and lateral views of the proximal femur prior to starting the procedure.
Figure 2.
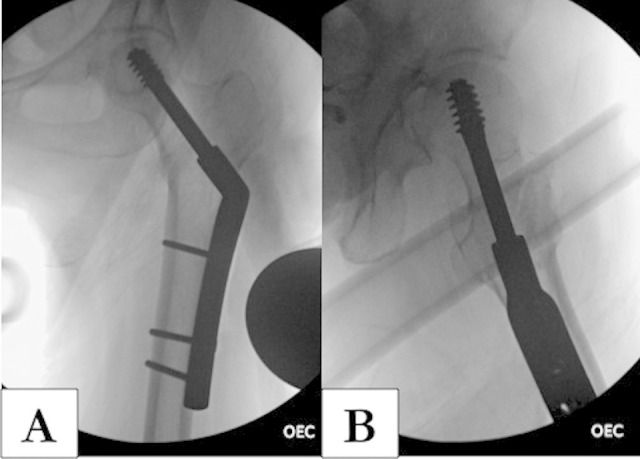
A and B, Anterior–posterior (AP) and lateral images of the proximal femur demonstrating a tip apex distance (TAD) of less than 25 mm.
The choice between HA and THA is a topic generating significant discussion. The Displaced Femoral Neck Fracture Arthroplasty Consortium for Treatment and Outcomes found significant improved outcome scores on the SF-36 and Western Ontario and McMaster Universities Arthritis Index (WOMAC) function for the THA group in a prospective randomized trial of 40 patients.20 There was not a significant increased risk of complications, thus, the authors concluded THA is a valuable treatment option.20 Better outcomes in terms of function and quality of life were also found after THA in a study of 120 patients with 4-year follow-up.21 In a meta-analysis that reviewed 8 randomized trials including 986 patients, patients with a THA achieved improved outcome scores and had less pain but had a higher dislocation rate.22 If choosing THA for treatment of a femoral neck fracture, the optimal patient is an active, lucid patient, with some preexisting degenerative changes. If torn between primary THA versus open reduction internal fixation (ORIF), it is better to choose THA as conversion to THA after failed ORIF has a higher complication rate and lower functional outcome scores.23
For those individuals who are treated with a hemiarthoplasty, the surgeon is faced with the choice of a unipolar versus a bipolar arthroplasty. There were equivalent clinical outcomes after 1 year in a randomized study of unipolar versus bipolar arthroplasty, but noted a higher incidence of acetabular erosion in the unipolar patients.24
Intertrochanteric/subtrochanteric Fractures
Just like with femoral neck fractures, one should approach implant selection based on fracture pattern stability. Stable intertrochanteric fractures can be treated with a sliding hip screw device or an intramedullary nail (IMN). For unstable fracture patterns, an IMN is the preferred treatment.25,26 There are several surgical details important for success in IMN of the elderly patients with hip fracture. Preoperative full-length femur films are important no matter what the fixation choice. Some considerations in fixation with a long IMN include the femoral bow. Most nail systems have a radius of curvature greater than the femur.27 This means the nail is straighter than the femur and there may be a risk of anterior cortical penetration. Appropriate preoperative fluoroscopic imaging to obtain a true anterior–posterior and lateral view is important. On the lateral fluoroscopic images, the ideal starting position should be in the middle one-third of the greater trochanter to minimize the risk of anterior cortical penetration and ensure a mid-axial position of the femoral nail distally on both the anteroposterior and lateral views. There are reduction aids, depending on manufacturer, to assist with aligning the guidewire to the mid portion of the femur (Figure 3). In osteoporotic bone, the use of an implant traversing the full length of the bone can help prevent stress risers at the tip of a short nail and provide a wide buttress of support in the bone.28,29
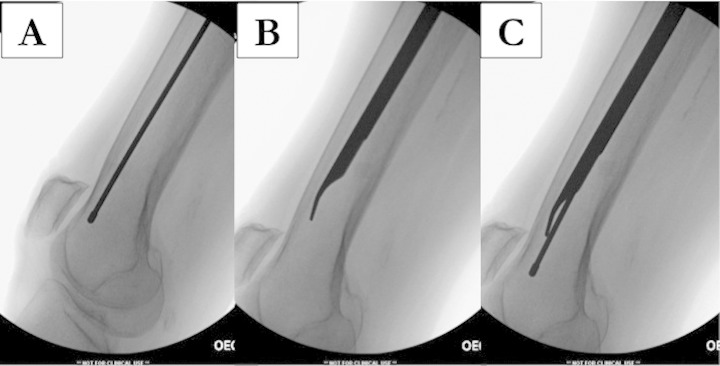
Figure 3.
When the guide wire initially travels too anterior distally in subtrochanteric femur fractures (A), reduction aids (B and C) are useful to obtain proper positioning of the guidewire for proper nail position.
Atypical femur fractures
Atypical femur fractures are those group of fractures occurring with a low-energy mechanism and often associated with use of bisphosphonates.30–33 These fractures are located below the lesser trochanter in the proximal femur and typically have characteristic radiographic features: cortical beaking, focal lateral cortical thickening, short oblique, or transverse in nature.31,34,35 In evaluation of bone biomechanical properties, changes have been noted with the prolonged use of bisphosphonates. The bone has demonstrated changes in crystallinity (lower mineral crystallinity), higher collagen maturity, a lower elastic modulus, and contact hardness compared to untreated women.36 It is important to understand that this is a pathologic type of fracture and fixation should reflect this.37 Preoperatively, one should also obtain images of the contralateral side as there may already be a stress reaction present30,33 (Figure 4). If a contralateral stress fracture is identified, one should recommend prophylactic fixation.30,32 In one case series, Banffy et al33 identified 6 nondisplaced stress fractures after bisphosphonate use managed nonoperatively. Of the 6 fractures, 5 eventually displaced and required subsequent fixation and had a statistically significant longer hospital stay when compared with the patients the authors treated prophylactically.
Figure 4.
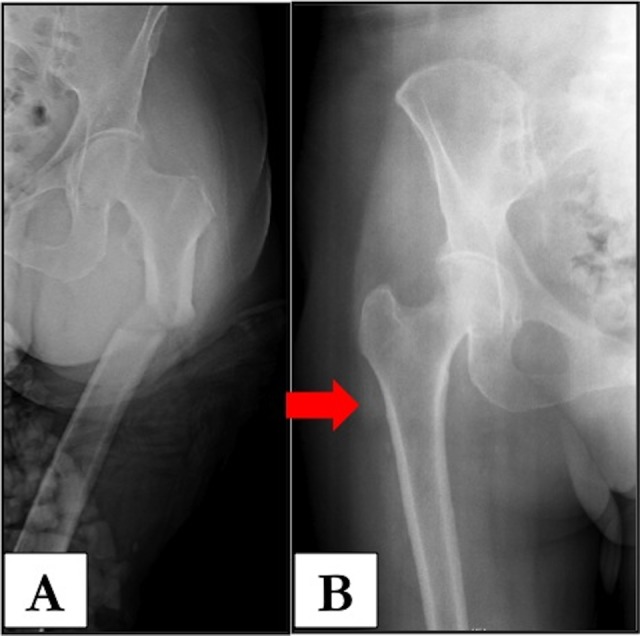
A, Anterior–posterior (AP) hip of a patient with an atypical femur fracture. Note the short oblique fracture and cortical beaking. B, Contralateral hip of the same patient. Note the stress reaction present with increased lateral cortical thickening. She underwent prophylactic intramedullary nailing of the right femur.
Vertebral Compression Fractures
Vertebral compression fractures (VCFs) are a common cause of pain and morbidity in the elderly patients. One may not realize how common these fractures are in postmenopausal women. In the United States alone, there is an estimate of 500 000 fractures annually.1 The treatment costs of these fractures are also tremendous, estimated to be greater than of US$15 billion.1
The VCF may just signal the beginning of a downhill spiral if the underlying etiology is not addressed. Patients often complain of pain, which may be disabling. There may be progressive spinal deformity. This affects lung function, decreasing vital capacity and functional levels, which affects mortality.38 There is also increased risk of additional compression fractures.39 The presentation of a patient with a VCF often is just with pain, which may be poorly localized, and without a direct etiology or traumatic event. Neurologic symptoms are rare. Complete evaluation of these patients should include a clinical examination, radiographic studies, and laboratory evaluation. It is important to rule out a metastatic process and infection. Advanced radiographic imaging may be helpful (Figure 5).
Figure 5.
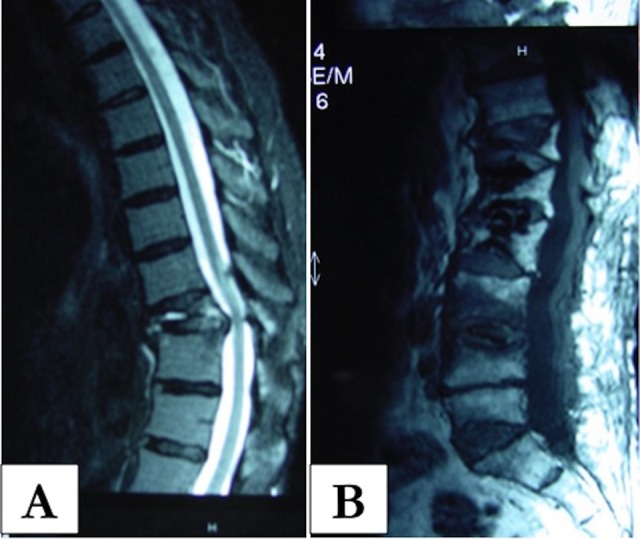
A and B, Magnetic resonance imaging (MRI) of a patient with vertebral compression fracture. Note the marrow edema and increased signal on the T2 image. One should also evaluate the MRI for other areas of involvement. (Images courtesy of Dr Howard Place.)
Noninvasive treatment should be the initial treatment. Medications are used to control the pain and/or spasm. It is important to minimize the use of narcotics due to the sedating effects on older individuals. Additional treatment options include activity modification and physical therapy with an emphasis on core strengthening. The use of a brace in older individuals is controversial. There is question as to its efficacy, and the ability for the patient to comply is another concern. If prescribed, close follow-up should ensue to ensure that the brace is providing support and/or preventing flexion. Should conservative measures fail or the patient have difficulty in mobilizing, vertebral augmentation represents an attractive option. Operative treatment of vertebral collapse includes vertebral augmentation with vertebroplasty (VP) or kyphoplasty (KP). Both procedures are performed under fluoroscopic imaging and use cement. The end results of the procedures are slightly different in terms of restoration of vertebral height.
Vertebroplasty is performed by placing a trocar and needle in the vertebral body, followed by the injection of cement. The advantages of VP include a faster procedure time, less invasive technique, and durability.40,41 Disadvantages include that the fractures are fixed in position without restoration of vertebral height and/or correction of kyphotic deformity. There also remains the risk of cement leakage and neurologic compromise.40
Kyphoplasty is a procedure in which a balloon is placed into the vertebral body and inflated to restore vertebral height, followed by the injection of cement. Like VP, KP is minimally invasive and cement complications remain a risk.42–44 The advantages of KP include subjective and objective improvement in quality of life and function.44–46 It is important to have careful patient selection as those with pain from a fixed deformity, instability, or both are not candidates for KP.47
The AAOS guidelines (reference: www.aaos.org/guidelines) recommend against VP and offer weak support for KP based on the clinical and scientific literature. It is important the physician be able to provide objective information to the patient as a basis of their decision making. In addition, since VCF are the end result of osteoporosis, as in hip fractures, one should provide evaluation and treatment/referral for the underlying disease process.47
In conclusion, osteoporotic fractures of the hip and spine are a major health problem with increasing occurrence as the population ages and a significant cost burden to society. When a patient sustains an osteoporotic hip or spine fracture, prompt evaluation and treatment with a team approach is critical. There is less tolerance for repeat procedures in the elderly patients, so minimizing complications and morbidities is paramount. The orthopedic surgeon should be proactive in recognizing the underlying etiology and have a system in place for treatment plans and/or referrals as ultimately evaluation and treatment of osteoporosis can help save lives.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22 (3):465–475. [DOI] [PubMed] [Google Scholar]
- 2. Edwards BJ, Bunta AD, Simonelli C, Bolander M, Fitzpatrick LA. Prior fractures are common in patients with subsequent hip fractures. Clin Orthop Relat Res. 2007;461:226–230. [DOI] [PubMed] [Google Scholar]
- 3. Vochteloo AJ, van Vliet-Koppert ST, Maier AB, et al. Risk factors for failure to return to the pre-fracture place of residence after hip fracture: a prospective longitudinal study of 444 patients. Arch Orthop Trauma Surg. 2012;132 (6):823–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Donegan DJ, Gay AN, Baldwin K, Morales EE, Esterhai JL, Jr, Mehta S. Use of medical comorbidities to predict complications after hip fracture surgery in the elderly. J Bone Joint Surg. 2010;92 (4):807–813. [DOI] [PubMed] [Google Scholar]
- 5. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182 (15):1609–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Burgers PT, Van Lieshout EM, Verhelst J, Dawson I, de Rijcke PA. Implementing a clinical pathway for hip fractures; effects on hospital length of stay and complication rates in five hundred and twenty six patients. Int Orthop. 2014;38 (5):1045–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pugely AJ, Martin CT, Gao Y, Klocke NF, Callaghan JJ, Marsh JL. A risk calculator for short term morbidity and mortality following hip fracture surgery. J Orthop Trauma. 2014;28 (2):63–69. [DOI] [PubMed] [Google Scholar]
- 8. O'HEireamhoin S, Beyer T, Ahmed M, Mulhall KJ. The role of preoperative cardiac investigation in emergency hip surgery. J Trauma. 2011;71 (5):1345–1347. [DOI] [PubMed] [Google Scholar]
- 9. Ricci WM, Della Rocca GJ, Combs C, Borrelli J. The medical and economic impact of preoperative cardiac testing in elderly patients with hip fractures. Injury. 2007;38 (suppl 3):S49–S52. [DOI] [PubMed] [Google Scholar]
- 10. Friedman SM, Mendelson DA, Kates SL, McCann RM. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56 (7):1349–1356. [DOI] [PubMed] [Google Scholar]
- 11. Bukata SV, Digiovanni BF, Friedman SM, et al. A guide to improving the care of patients with fragility fractures. Geriatr Orthop Surg Rehabil. 2011;2 (1):5–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kates SL, Mendelson DA, Friedman SM. Co-managed care for fragility hip fractures (Rochester model). Osteoporos Int. 2010;21 (suppl 4):S621–S625. [DOI] [PubMed] [Google Scholar]
- 13. Menzies IB, Mendelson DA, Kates SL, Friedman SM. Prevention and clinical management of hip fractures in patients with dementia. Geriatr Orthop Surg Rehabil. 2010;1 (2):63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Friedman SM, Menzies IB, Bukata SV, Mendelson DA, Kates SL. Dementia and hip fractures: development of a pathogenic framework for understanding and studying risk. Geriatr Orthop Surg Rehabil. 2010;1 (2):52–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kates SL, Blake D, Bingham KW, Kates OS, Mendelson DA, Friedman SM. Comparison of an organized geriatric fracture program to United States government data. Geriatr Orthop Surg Rehabil. 2010;1 (1):15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010;1 (1):6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged geriatric fracture center on short-term hip fracture outcomes. Arch Intern Med. 2009;169 (18):1712–1717. [DOI] [PubMed] [Google Scholar]
- 18. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg. 1995;77 (7):1058–1064. [DOI] [PubMed] [Google Scholar]
- 19. Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2008 (3):CD000093. [DOI] [PubMed] [Google Scholar]
- 20. Macaulay W, Nellans KW, Garvin KL, et al. Prospective randomized clinical trial comparing hemiarthroplasty to total hip arthroplasty in the treatment of displaced femoral neck fractures: winner of the Dorr Award. J Arthroplasty. 2008;23 (6 suppl 1):2–8. [DOI] [PubMed] [Google Scholar]
- 21. Hedbeck CJ, Enocson A, Lapidus G, et al. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg. 2011;93 (5):445–450. [DOI] [PubMed] [Google Scholar]
- 22. Burgers PT, Van Geene AR, Van den Bekerom MP, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthopaed. 2012;36 (8):1549–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthopaed Surg. 2008;16 (10):596–607. [DOI] [PubMed] [Google Scholar]
- 24. Inngul C, Hedbeck CJ, Blomfeldt R, Lapidus G, Ponzer S, Enocson A. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in patients with displaced femoral neck fractures. A four-year follow-up of a randomised controlled trial. Int Orthop. 2013;37 (12):2457–2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Adams CI, Robinson CM, Court-Brown CM, McQueen MM. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma. 2001;15 (6):394–400. [DOI] [PubMed] [Google Scholar]
- 26. Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg. 2008;90 (4):700–707. [DOI] [PubMed] [Google Scholar]
- 27. Egol KA, Chang EY, Cvitkovic J, Kummer FJ, Koval KJ. Mismatch of current intramedullary nails with the anterior bow of the femur. J Orthop Trauma. 2004;18 (7):410–415. [DOI] [PubMed] [Google Scholar]
- 28. Goldhahn J, Suhm N, Goldhahn S, Blauth M, Hanson B. Influence of osteoporosis on fracture fixation—a systematic literature review. Osteoporos Int. 2008;19 (6):761–772. [DOI] [PubMed] [Google Scholar]
- 29. Kuzyk PR, Bhandari M, McKee MD, Russell TA, Schemitsch EH. Intramedullary versus extramedullary fixation for subtrochanteric femur fractures. J Orthop Trauma. 2009;23 (6):465–470. [DOI] [PubMed] [Google Scholar]
- 30. Capeci CM, Tejwani NC. Bilateral low-energy simultaneous or sequential femoral fractures in patients on long-term alendronate therapy. J Bone Joint Surg. 2009;91 (11):2556–2561. [DOI] [PubMed] [Google Scholar]
- 31. Edwards MH, McCrae FC, Young-Min SA. Alendronate-related femoral diaphysis fracture—what should be done to predict and prevent subsequent fracture of the contralateral side? Osteoporos Int. 2010;21 (4):701–703. [DOI] [PubMed] [Google Scholar]
- 32. Goddard MS, Reid KR, Johnston JC, Khanuja HS. Atraumatic bilateral femur fracture in long-term bisphosphonate use. Orthopedics. 2009;32 (8). [DOI] [PubMed] [Google Scholar]
- 33. Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res. 2011;469 (7):2028–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Goh SK, Yang KY, Koh JS, et al. Subtrochanteric insufficiency fractures in patients on alendronate therapy: a caution. J Bone Joint Surg. 2007;89 (3):349–353. [DOI] [PubMed] [Google Scholar]
- 35. Koh JS, Goh SK, Png MA, Kwek EB, Howe TS. Femoral cortical stress lesions in long-term bisphosphonate therapy: a herald of impending fracture? J Orthop Trauma. 2010;24 (2):75–81. [DOI] [PubMed] [Google Scholar]
- 36. Bala Y, Depalle B, Farlay D, et al. Bone micromechanical properties are compromised during long-term alendronate therapy independently of mineralization. J Bone Miner Res. 2012;27 (4):825–834. [DOI] [PubMed] [Google Scholar]
- 37. Grady MK, Watson JT, Cannada LK. Treatment of femoral fracture nonunion after long-term bisphosphonate use. Orthopedics. 2012;35 (6): e991–995. [DOI] [PubMed] [Google Scholar]
- 38. Edidin AA, Ong KL, Lau E, Kurtz SM. Life expectancy following diagnosis of a vertebral compression fracture. Osteoporos Int. 2013;24 (2):451–458. [DOI] [PubMed] [Google Scholar]
- 39. Cauley JA, Hochberg MC, Lui LY, et al. Long-term risk of incident vertebral fractures. JAMA. 2007;298 (23):2761–2767. [DOI] [PubMed] [Google Scholar]
- 40. Kallmes DF, Jarvik JG, Osborne RH, et al. Clinical utility of vertebroplasty: elevating the evidence. Radiology. 2010;255 (3):675–680. [DOI] [PubMed] [Google Scholar]
- 41. Staples MP, Kallmes DF, Comstock BA, et al. Effectiveness of vertebroplasty using individual patient data from two randomised placebo controlled trials: meta-analysis. BMJ. 2011;343:d3952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Boonen S, Van Meirhaeghe J, Bastian L, et al. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res. 2011;26 (7):1627–1637. [DOI] [PubMed] [Google Scholar]
- 43. Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26 (14):1631–1638. [DOI] [PubMed] [Google Scholar]
- 44. Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373 (9668):1016–1024. [DOI] [PubMed] [Google Scholar]
- 45. Gill JB, Kuper M, Chin PC, Zhang Y, Schutt R., Jr Comparing pain reduction following kyphoplasty and vertebroplasty for osteoporotic vertebral compression fractures. Pain Phys. 2007;10 (4):583–590. [PubMed] [Google Scholar]
- 46. Wardlaw D, Van Meirhaeghe J, Ranstam J, Bastian L, Boonen S. Balloon kyphoplasty in patients with osteoporotic vertebral compression fractures. Expert Rev Med Devices. 2012;9 (4):423–436. [DOI] [PubMed] [Google Scholar]
- 47. Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR. Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J. 2009;9 (7):537–544. [DOI] [PubMed] [Google Scholar]