Abstract
Purpose:
This prospective study was designed to evaluate the effect of American Society of Anaesthesiologists (ASA) score on time to surgery, length of hospital stay, and 30-day mortality in elderly patients with femoral neck fracture.
Methods:
A total of 249 patients admitted with femoral neck fracture were included in the study. Mean age was 84 years (95% confidence interval 83 to 85). Two patients were ASA I, 110 patients were ASA II, 125 were ASA III, and 12 were ASA IV.
Results:
The mean time to surgery was 18.9 hours for ASA I patients, 34.4 hours for ASA II patients, 42.8 hours for ASA III patients, and 61 hours for ASA IV patients (P = .005). The mean hospital stay was 11.5 days (6.3-15.2) for ASA I patients, 17.6 days (4.2-98.8) for ASA II patients, 22.9 days (4.1-120.3) for ASA III patients, and 29 days (2.4-86.0) for ASA IV patients (P = .026); 85% of the patients who died within 30 days of admission were of ASA III-IV.
Conclusion:
Our study shows that patients with higher ASA score have delay in surgery, longer hospital stay, and increase in 30-day mortality. We conclude that ASA grade is a simple and effective tool to predict the above-mentioned outcomes in these patients.
Keywords: ASA, neck of femur fracture, predictor
Introduction
In 2008, 70 000 patients sustained hip fracture in the United Kingdom. There is an estimated 2% rise per year. The estimated figures predict that there will be 91 500 hip fractures in 2015 and 101 000 in 2020.1 Hip fractures in elderly individuals are associated with high morbidity and mortality. There is a great emphasis on improving the outcome by focusing on anesthetic and surgical techniques, nursing care, early surgery, and multidisciplinary approach, but it still remains a significant source of morbidity and mortality for the elderly population.
American Society of Anaesthesiologists (ASA) score was introduced to assess one’s overall physical fitness or sickness preoperatively and regarded as a scale to predict risk.2 The ASA scores divide patients undergoing a surgical procedure into the following categories: I, healthy patient; II, patient with mild systemic disease; III, patient with severe systemic disease not incapacitating; IV, patient with incapacitating systemic disease; and V, moribund patient.3 The ASA score determines physical state of the patient prior to anesthetic and surgery. It is a useful tool for communication, record keeping, and statistical analysis. The aim of our study was to determine the relationship between time to surgery, length of hospital stay, and 30-day mortality in elderly patients with femoral neck fracture and ASA score.
It is well known that the delay in surgery is associated with increased risk of morbidity and mortality in patients with hip fracture.4–8 Although previous literatures use ASA score as a predictor of mortality, there are no reports of it being used as for time to surgery, length of stay, and 30-day mortality.5,9,10 The duration of stay in the hospital of such patients is an important issue, especially in the current economic environment.
Materials and Methods
It is a single-center study performed at a district hospital; data were collected prospectively. Between April 2010 and May 2011, 252 patients were admitted to hospital with femoral neck fracture. Mean age was 84 years (95% confidence interval [CI] 83-85). The time to surgery was defined as the difference between the time of admission and the time of starting the surgery (in hours). The length of stay is defined as the time from hospital admission to the time of discharge from the hospital (in days). Delay in surgery was defined as patient having surgery after 36 hours of the admission.
Three patients died before surgery and were not included in the study and 18 patients died in hospital before discharge, hence 231 patients were considered in the length of stay.
The senior anesthetist in charge of the operating list evaluated the ASA grade of the patient. Two patients were ASA I, 110 patients were ASA II, 125 were ASA III, and 12 were ASA IV. The data were collected using Microsoft Office Excel 2007 and analyzed using PASW Statistics v.18 computer package (SPSS Inc, Chicago, Illinois). The use of power analysis enabled us to decide on sample size needed for statistical judgments that was reliable and how likely the statistical test will be to detect effects of a given sample size. The analysis showed that at least 194 patients were needed to detect 10% difference in hospital stays, using significance level of 5% and power of 80%. Using normal plot of residuals, the samples proved to be normally distributed. The variants of time to surgery were compared with the categorized ASA grades using parametric 1-way analysis of variance test. A Pearson correlation 2-tailed test was used to determine the association of the time to surgery with the length of stay.
Results
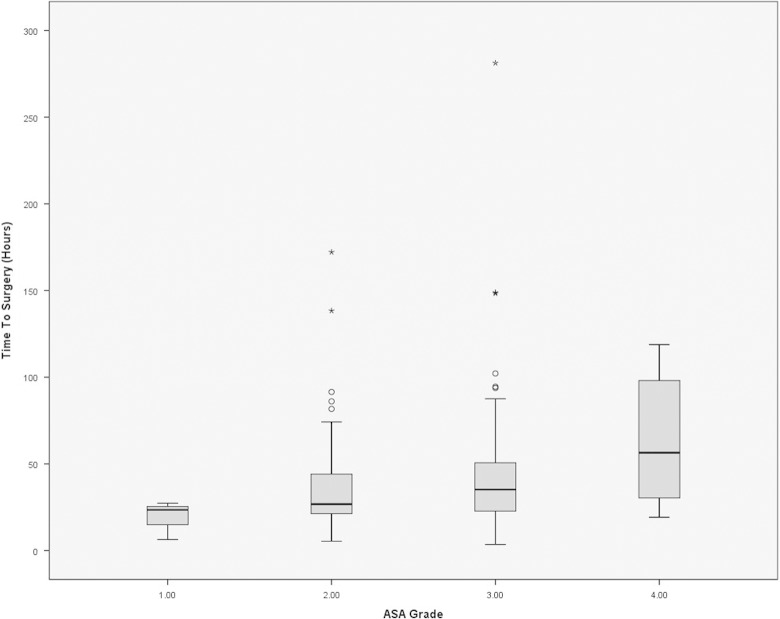
The mean time to surgery was 18.9 hours for ASA I patients (95% CI −8.8-46.6), 34.4 hours (95% CI 29.9-38.8) for ASA II patients, 42.8 hours (95% CI 36.9-48.7) for ASA III patients, and 61 hours (95% CI 38.8-83.3) in ASA IV patients. A total of 145 (58.2%) patients had their operation within 36 hours of admission to hospital, mean time to surgery in this group was 22.7 hours (95% CI 21.7-23.7) and 41.8% of the patients were not operated within 36 hours of admission and mean time to surgery in this group was 62.6 hours (95% CI 56.1-69). The results show that higher the ASA grade, longer the time to surgery (Figure 1) and a significant difference in the mean time to surgery in these 4 groups (P = .005).
Figure 1.
Box plot with standard error showing time to surgery with American Society of Anaesthesiologist (ASA) grading.
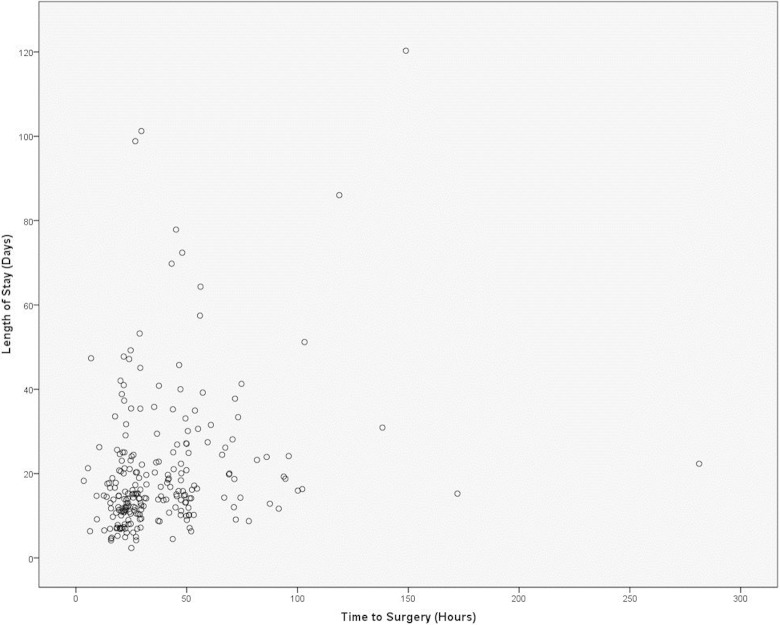
The mean hospital stay was 11.5 days (6.3-15.2) for ASA I patients, 17.6 days (4.2-98.8) for ASA II patients, 22.9 days (4.1-120.3) for ASA III patients, and 29 days (2.4-86.0) for ASA IV patients (P = .026). There is evidence of linear association between time to surgery and length of stay with Pearson correlation coefficient, r = .178 (95% CI 0.001-0.397) with P < .01. The scatter graph showed the delay in surgery increased the hospital stay thus delaying patient discharge (Figure 2).
Figure 2.
Scatter plots showing length of stay (in days) with time to surgery (in hours).
Sixty-one patients were operated after 36 hours due to being quite sick and need for further imaging; 18 patients had their surgery delayed due to hematological reasons; 14 patients had their surgery postponed due to pulmonary problems such as severe acute on chronic obstructive pulmonary disease, pneumonia, and pulmonary embolism; 12 patients needed further imaging, as radiographs did not show obvious hip fractures; 7 patients were septic due to urinary tract infection; 7 patients had delay due to cardiovascular problem including atrial fibrillation, heart block, and severe heart failure; and 3 patients had severe cellulitis with sepsis. In this group, 49 patients were quite unwell on admission and needed medical input prior to surgery. Of these, 27 patients were of ASA III while 6 were of ASA IV. Figure 3 gives a breakdown of delays due to medical reasons versus ASA grades and shows that majority of the patients in whom surgery was delayed were of higher ASA grades; 39 patients were surgery delayed due to lack of operating time and 4 patients had their operation delayed due to problems in theater equipment; 34 (14%) patients died within 30 days of the admission; 5 patients were ASA II; 26 were ASA III, and 3 were ASA IV; 15 of these 34 patients were operated after 36 hours of their hospital admission due to medical reasons; and 14 of these patients were of ASA III and 1 was of ASA IV.
Figure 3.
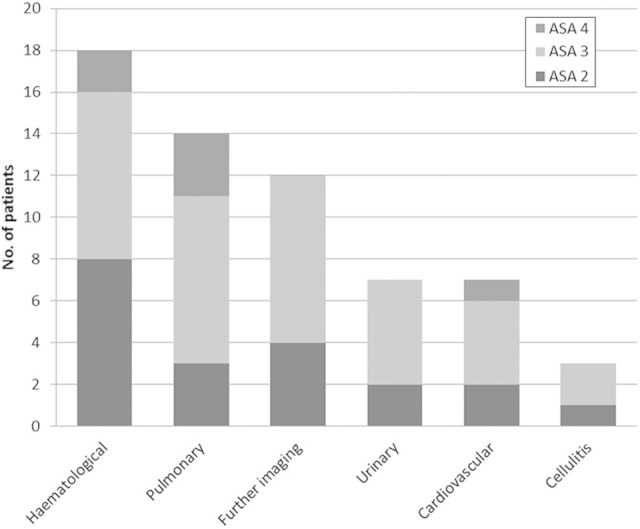
Type of delays due to medical cause versus American Society of Anaesthesiologist (ASA) scores.
Discussion
The management of hip fractures requires multidisciplinary approach from admission in accident and emergency department through to the departments of radiology, anesthetics, orthopaedic surgery, medicine, and rehabilitation. The gold standard is to resuscitate the patient and surgery as soon as possible. The National Institute for health and Clinical Excellence guidelines recommend early surgery within 36 hours of the admission would improve the patient outcome.11 All the patients with hip fractures undergo preoperative assessment soon after the admission by an anesthetist and are graded according to ASA grade. Higher ASA scores indicate significant preoperative morbidity and need for appropriate early resuscitation of these patients. It enables the clinicians to counsel the patient and family accordingly. To our knowledge, there is very limited studies describing the effect of ASA grade on delay in surgery, length of stay, and 30-day mortality in patients with femoral neck fractures hence the reason of our study.12–16
Table 1 summarizes the relationship between ASA grades, mortality, delayin surgery, and length of stay. Our results show that about 25% of the patients had their operation deferred because of medical reasons; 33% of these were of ASA II, 57% of ASA III, 10% of ASA IV, and none from ASA I indicating that higher ASA grades are associated with delay in surgery. Delay in surgery contributes to prolonged hospital stay and has been shown to some extent in previous studies.17 The hospital stay was longer in patients with higher ASA score in our study. We observed that patients with higher ASA grades were often slow to rehabilitate and delay in surgery led to prolonged stay in bed, slow mobilization, and a delayed hospital discharge. There was some delay due to lack of operating time. Dedicated trauma operating sessions for patients with femoral neck fracture will be ideal and are likely to improve the productivity by allowing more cases to be performed during working hours with senior supervision and reduce the postoperative complication.11
Table 1.
Table summarizing the relationship between American Society of Anaesthesiologist (ASA) grades, mortality, delay in time to surgery, and length of stay.
The average 30-day mortality following hip fracture surgery has been reported to be about 9% from admission.18 In our series, it was about 14% and reflects the group of patients being treated at our institution; 85% of the patients who died within 30 days of admission were of ASA III and IV, and 41% of these patients were operated within 36 hours of admission while 44% of the patients needed medical stabilization and were operated after 36 hours of admission and all these patients were of ASA III and IV. There was some delay in this group for resuscitation; however, it seems that mortality in these cases was related to the medical condition rather than minor delay in surgery. Lefaivre et al have shown in their study that delay in surgery was not a significant predictor of 30-day mortality.19 Our results show that high ASA grade is associated with increased risk of early mortality.
The ASA grade is determined preoperatively and is a reliable assessment of physical status of an individual prior to the surgical procedure. Higher ASA grade indicates significant preoperative comorbidity. In cases of neck of femur fracture, these comorbidities when coupled with old age present a management challenge to the clinicians and demand timely aggressive approach for a favorable outcome. The results of our study have shown that higher ASA grades are associated with delay in surgery, longer hospital stay, and high 30-day mortality. We believe that early recognition is a key along with a multi disciplinary input starting on admission, particularly a close collaboration between geriatricians, anesthetists, orthopedic surgeons, intensive care physician, and support services will help to minimize the delay in surgery, early mobilization, reduce hospital stay, and improve patient care.
There are some limitations to our study as delay in surgery also depends upon theater efficiency, which can be variable due to various factors as theater staff, availability of image intensifier, hardware, recovery staff, and patient turnover time. We are aware that patients who are admitted from a nursing home might conceal a true delay in their time to discharge due to the fact that a maximum care package is already in place for them prior to their admission to hospital. It is also difficult to blind the ASA grade. The strength of this study is that it is prospective with a large number of patients; however, a multicenter randomized controlled clinical trial will be of great value but it may not be possible due to the intention-to-treat issue. Although there is evidence of linear association between time to surgery and length of stay and positive correlation, the results are subjected to other confounding factors such as patient potential for rehabilitation, mental state, input by the occupational health team, and location of discharge.
In our study, higher ASA grade was associated with delay in surgery, longer hospital stay, and higher 30-day mortality. We conclude that ASA grade is a reliable indicator of these parameters and is a simple and effective tool in predicting delay in surgery, hospital stay, and 30-day mortality in elderly patients with femoral neck fracture. The ASA grades are known almost immediately following admission therefore helping clinicians to recognize high-risk cases at a very early stage and recommend aggressive resuscitation of all such cases to minimize morbidity, mortality, and counseling of patients/families.
Acknowledgments
Special thanks to Trauma Coordinator Stella Legg for data collection.
Footnotes
Authors’ Note: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2004;(4):CD000521. [DOI] [PubMed] [Google Scholar]
- 2. Owens WD. American society of anaesthesiologists physical status classification system is not a risk classification system. Anesthesiology. 2001;94 (2):378. [DOI] [PubMed] [Google Scholar]
- 3. Dripps RD. American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24(1):111. [Google Scholar]
- 4. Holt EM, Evans RA, Hindley CJ, Metcalfe JW. 1000 femoral neck fractures: the effect of pre-injury mobility and surgical experience on outcome. Injury. 1994;25(2):91–95. [DOI] [PubMed] [Google Scholar]
- 5. Elliott J, Beringer T, Kee F, Marsh D, Willis C, Stevenson M. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. J Clin Epidemiol. 2003;56(8):788–795. [DOI] [PubMed] [Google Scholar]
- 6. Casaletto JA, Gatt R. Post-operative mortality related to waiting time for hip fracture surgery. Injury. 2004;35 (2):114–120. [DOI] [PubMed] [Google Scholar]
- 7. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77 (10):1551–1556. [DOI] [PubMed] [Google Scholar]
- 8. Doruk H, Mas MR, Yildiz C, Sonmez A, Kýrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39 (2):179–185. [DOI] [PubMed] [Google Scholar]
- 9. Michel JP, Klopfenstein C, Hoffmeyer P, Stern R, Grab B. Hip fracture surgery: is the pre-operative American Society of Anesthesiologists (ASA) score a predictor of functional outcome? Aging Clin Exp Res. 2002;14 (5):389–394. [DOI] [PubMed] [Google Scholar]
- 10. Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17 (1):53–56. [DOI] [PubMed] [Google Scholar]
- 11. NICE clinical guideline 124. Hip fracture: the management of hip fracture in adults. National Institute for health and Clinical Excellence. NICE; 2011. [PubMed] [Google Scholar]
- 12. Brown CA, Olson S, Zura R. Predictors of length of hospital stay in elderly hip fracture patients. J Surg Orthopaed Adv. 2013;22 (2):160–163. [DOI] [PubMed] [Google Scholar]
- 13. Daugaard CL, Jorgensen H, Riis T, Lauritzen JB, Duus BR, Mark SV. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? Acta Orthop. 2012; 83 (6):609–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kang JW, Kim KJ, Lee SK, Kim J, Jeung SW, Choi HG. Predictors of mortality in patients with hip fractures for persons aging more than 65 years old. Int J Bio-Science Bio-Technology. 2013;5 (2):27–34. [Google Scholar]
- 15. Egol K, Strauss EJ. Perioperative considerations in geriatric patients with hip fracture: what is the evidence? J Orthop Trauma. 2009;23 (6):386–394. [DOI] [PubMed] [Google Scholar]
- 16. Kim SD, Park Sj, Lee DH, Jee DL. Rick factors of morbidity and mortality following hip fracture surgery. Korean J Anesthesiol. 2013;64 (6):505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Charalambous CP, Yarwood S, Paschalides C, Siddique I, Hirst P, Paul A. Factors delaying surgical treatment of hip fractures in elderly patients. Ann R Coll Surg Engl. 2003;85 (2):117–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87 (3):483–489. [DOI] [PubMed] [Google Scholar]
- 19. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91 (7):922–927. [DOI] [PubMed] [Google Scholar]