Abstract
Introduction and Objective:
Drug-induced thrombocytopenia is a common adverse effect reported in the literature. Typically patients present with a low platelet count with signs and symptoms ranging from bruising to bleeding, and major organ damage. Penicillin-induced thrombocytopenia previously reported in the literature is explained primarily through the hapten-dependent antibody process. The goal of this report is to present a case of an amoxicillin/clavulanic acid-induced thrombocytopenia.
Case Presentation:
A 23-year-old male presented to the emergency department with bruises on his arms and legs after completing a full course of amoxicillin/clavulanic acid of 625 mg twice a day for 5 days for tonsillitis. After several tests, the patient was diagnosed with thrombocytopenia induced by amoxicillin/clavulanic acid. The patient was treated with a corticosteroids taper regimen for 3 weeks. He was discharged after 3 days of inpatient treatment with instructions to avoid physical activity for 2 weeks. Two weeks post discharge, the follow-up showed that the platelet count had increased.
Discussion:
Penicillin-induced thrombocytopenia has been previously reported in the inpatient setting where bleeding was observed. However, the patient in this case report presented with bruises on his arms and legs. The diagnosis was made by the process of elimination; not all possible tests were conducted. The patient was prescribed corticosteroids that are not indicated for drug-induced thrombocytopenia. The Naranjo scale showed that this is a probable adverse event of amoxicillin/clavulanic acid.
Conclusion:
This is a unique case where amoxicillin/clavulanic acid was reported to be a probable cause of thrombocytopenia in an outpatient setting without signs of bleeding and without concomitant medications.
Keywords: amoxicillin/clavulanic acid, drug-induced, platelets, thrombocytopenia
Drug-induced thrombocytopenia (DIT) is among the most frequently reported fatal adverse drug reactions.1 Although the definition of thrombocytopenia is not consistent in the literature, it is usually considered when a platelet count is less than 100 x 109/L or the patient experiences a greater than 50% drop in the platelet count from baseline.2,3 Patients with DIT can present with a wide range of signs and symptoms, from bruising, petechiae, epistaxis, and purpura to major organ bleeding, depending on the severity of thrombocytopenia. Excluding chemotherapeutic agents and heparin, major drug classes that have been implicated in DIT include anticonvulsants, beta-lactams, cinchona alkaloid derivatives, disease-modifying anti-rheumatic drugs (DMARDs), diuretics, sulfonamide antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and tuberculostatics.4 Beta-lactam antimicrobials have been reported to cause several blood dyscrasias.5 The use of beta-lactams is associated with a 7-fold increased risk of thrombocytopenia in the general population, whereas penicillins are associated with an almost 2-fold increase.6
We conducted a PubMed search using the key terms drug-induced thrombocytopenia, penicillin-induced thrombocytopenia, amoxicillin-clavulanic acid induced thrombocytopenia, amoxicillin, thrombocytopenia, B-lactams, and B-lactams-induced thrombocytopenia. Evidence documenting this adverse drug event comes mostly from case reports and case studies; none had reported on amoxicillin/ clavulanic acid-induced thrombocytopenia.4
The postulated mechanisms for antimicrobialassociated thrombocytopenia and bleeding include hapten-dependent antibody, quinine-type antibody, autoantibody, bone marrow suppression or toxicity, and prolonged international normalized ratio (INR) of prothrombin time (PT). Of these mechanisms, penicillin-induced thrombocytopenia is mostly explained through the hapten-dependent antibody process.3
To the best of our knowledge, the following is the first report of possible amoxicillin/clavulanic acid-induced thrombocytopenia.
Case Presentation
A 23-year-old Caucasian male presented with bluish spots on the arms, legs, and buccal mucosa. Those bruises were not the result of physical trauma. Upon physical examination, the patient weighed 80 kg, was 183 cm tall, afebrile, and had no known drug allergies. His blood pressure measured 90/70 mm Hg and his heart rate was 77 bpm. Ecchymoses on the arms, legs, and buccal mucosa were noticed. He reported being a nonsmoker, drinking alcohol occasionally, and experiencing 1 episode of epistaxis 1 week prior to presentation.
The patient had no medical problems and was not taking any chronic medications. However, 1 month earlier, he reported taking oral Augmentin 625 mg (amoxicillin/clavulanic acid) twice daily for 5 days for tonsillitis. A week later, the patient noticed purple spots on his arms and legs while playing soccer. At first, he suspected that these spots were from playing soccer and he abstained from physical activity. However, the spots persisted and darkened in color, which led the patient to present to the emergency department. This happened over the span of a 2-week period. A complete blood count (CBC) and a comprehensive metabolic panel were performed. A platelet count of 17,200 cells/μL was detected; the rest of the laboratory data were normal including aspartate aminotranferase (AST), alanine aminotransferase (ALT), serum albumin, PT, and INR. Tests including HIV, monospot, EBV antibody, hepatitis B and C, and a bone marrow aspirate were negative. Cytomegalovirus (CMV) and toxoplasmosis IgG(s) were positive with negative IgM(s). Figure 1 summarizes the platelets trend during hospitalization and after discharge.
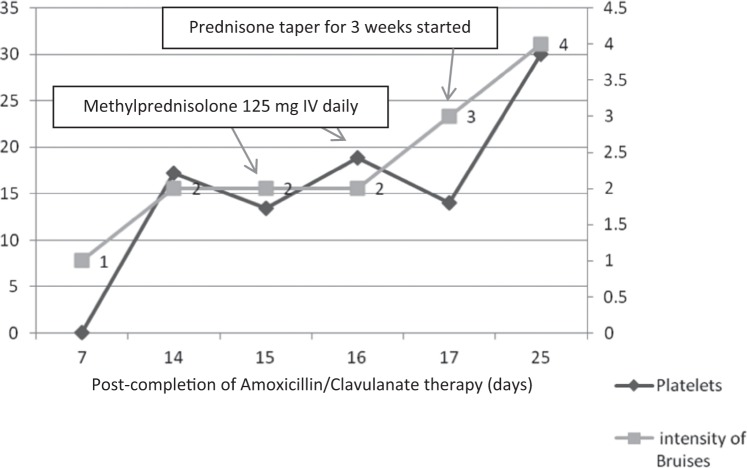
Figure 1.
Platelets trend and intensity of bruises after exposure to Augmentin. On the left y axis, platelets are counted in 103 cells/mm3. On the right y axis, color intensity of the bruises range from reddish-blush (1), purple (2), green (3), to yellow-brown (4).
Based on the available data, the patient was diagnosed with drug-induced thrombocytopenia. The patient was admitted to the hospital for follow-up and management. During the hospital stay, the patient received steroids (Figure 1).
Upon discharge, the patient was instructed to stay home and avoid physical activity for 2 weeks. One week after hospital discharge, the patient showed an increased platelet count of 30,000 cells/μL.
Discussion
Case reports of drug-induced, especially penicillins, thrombocytic purpura have been reported, including ampicillin, methicillin, amoxicillin, and piperacillin and ceftriaxone and second-generation cephalosporins.6–8 Amoxicillin-clavulanic acid (Augmentin) has been associated with some hematological disorders, mainly purpura. One case of severe neutropenia after prolonged treatment with amoxicillin-clavulanic acid has been reported, however, we found little information related to thrombocytopenia.9–13 For instance, prolongation of PT, purpura, thrombocytopenia, agranulocytosis, granulocytopenia, and leucopenia are listed as rare side effects in the package insert.14
The patient in this case report developed ecchymosis of the skin and buccal mucosa soon after taking amoxicillin/clavulanic acid for the treatment of tonsillitis. The case is unique, as it was an isolated case of thrombocytopenia that was diagnosed by the process of elimination. A workup to rule out possible causes of thrombocytopenia was conducted, and no correlation between the investigated diseases and low platelets has been confirmed. The Naranjo scale was used to establish the probability of causality.15 A score of 5 was obtained, and drug-induced thrombocytopenia was shown to be a probable adverse event of amoxicillin/clavulanic acid. Because the thrombocytopenia occurred due to a penicillin derivative, similar cases with penicillin- and cephalosporin-induced thrombocytopenia were reviewed. The incidence of bleeding, antibodies detection, the time for the thrombocytopenia to occur from the time of exposure, and the recovery time were reported. In this case, the patient did not complain of any bleeding side effects. However, the occurrence of bruises motivated him to seek medical attention. Several cases of idiopathic thrombocytic purpura were reported in which 79.3% of the patients presented with bruises.6 Ampicillin-induced thrombocytopenia was reported in 2 case reports and was associated with minor or major bleeding. 7 Methicillin-induced thrombocytopenia was described in a case report in which it was associated with minor bleeding.7
In some reported cases, drug-specific antibodies were tested. Although the mechanism of DIT is not fully understood, it has been linked to the presence of antibodies. For instance, hapten-dependent antibodies appear to be present in beta-lactam–induced thrombocytopenia where hapten (drug) binds covalently to platelet membrane resulting in a drug-specific immune response (Figure 2).16–18 In this case report, no drug antibodies or hapten-dependent antibodies were tested. In one case of piperacillin-induced thrombocytopenia, IgG results were positive.8,19 Ceftriaxone has been shown to induce antibody formation and platelet destruction.20
Figure 2.
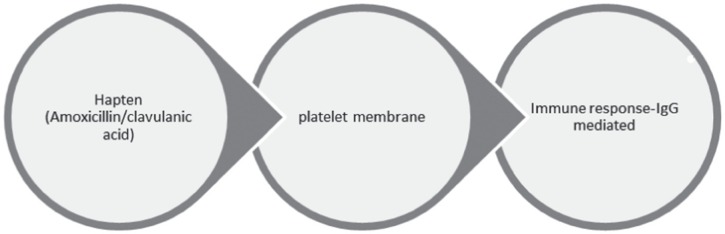
Suspected mechanism of action of the amoxicillin/clavulanic acid immune response.
Of note, some of the patients who developed beta-lactam–induced thrombocytopenia were exposed to the same antibiotic class. Current use of an antibiotic class was defined as exposure to the drug in the 4-week period before the occurrence of thrombocytopenia.21 In the case of piperacillin-induced thrombocytopenia, the decrease in the platelets count started on day 4 of therapy.8 In that case, the patient was also on heparin and vancomcyin. Vancomcyin and heparin were discontinued because they were suspected to be the causative agents, but the platelets continued to decrease on day 12 of piperacillin treatment. On day 14 of piperacillin treatment, piperacillin was stopped and the platelets started to increase. Piperacillininduced thrombocytopenia is reported to be severe but reversible within 3 to 5 days after stopping the antibiotic.8,22–24 These findings concur with reports of the occurrence of thrombocytopenia within 3 days of exposure to the causative agent and a recovery with a median of 7 days.7 In the present case, thrombocytopenia was detected after hospitalization and the appearance of the purpura and increase in the intensity of the bruises. This explains the relationship between the low platelet count and the exposure to amoxicillin/clavulanic acid, however, the reason behind the continued decrease in the platelet count 1 month after stopping amoxicillin/clavulanic acid remains unclear.
This case has few limitations. For instance, heptan antibodies were not tested, so we cannot confirm the causality between thrombocytopenia and amoxicillin/clavulanic acid. There is also no information on whether the patient was previously exposed to Augmentin. The hypercoagulable state was not ruled out.
Management
No pharmacological treatment is recommended for the management of DIT. Corticosteroids have not been shown to be beneficial in the treatment of DIT, although they have shown an effect in idiopathic thrombocytic purpura.2 Hence, in cases where the distinction between drug-induced and iodiopathic purpura is difficult to make, prednisone 1 to 2 mg/kg/ day over 2 to 4 weeks or intravenous immunoglobulin (1 g/kg/day for 2 consecutive days) may be administered. Platelets transfusion might be considered in the occurrence of bleeding.25–29
In the present case, the patient was given methylprednisolone 125 mg (1.5 mg/kg/day) for 2 days on day 2 of hospitalization and was discharged on a taper regimen over 3 weeks of prednisone. Based on the literature review, the case was managed as an idiopathic thrombocytic purpura and not as drug-induced thrombocytopenia, as the diagnosis was confirmed on day 3 of hospitalization. Even though corticosteroids were no longer indicated following the final diagnosis, methylprednisolone was continued because platelets count increased by 5,500 cells/μL following steroid therapy.
Conclusion
This case suggests a probable relationship between thrombocytopenia and recent exposure to amoxicillin/clavulanic acid. Previous case reports suggested this causality between beta-lactams and thrombocytopenia where antibodies were detected. In the future, when DIT is suspected, the necessary antibody tests should be ordered to help with the diagnosis and guide the treatment.
Acknowledgments
The authors have no conflicts of interest.
References
- 1.De Keulenaer BL, Cheah CY.Comment on “Drug-Induced Thrombocytopenia: An Updated Systematic Review.” Drug Saf. 2009;32:707–708. [DOI] [PubMed] [Google Scholar]
- 2.Van den bemt PMLA, Meyboom RHB, Egberts ACG. Drug-induced thrombocytopenia. Drug Saf. 2004;27:1243–1252. [DOI] [PubMed] [Google Scholar]
- 3.Loo A, Gerzenshtein L, Ison M.Antimicrobial drug-induced thrombocytopenia: A review of the literature. Semin Thromb Hemost. 2012;38:818–829. [DOI] [PubMed] [Google Scholar]
- 4.Ten Berg M, Huisman A, Souverein P, et al. Drug-induced thrombocytopenia. Drug Saf. 2006;29:713–721. [DOI] [PubMed] [Google Scholar]
- 5.Huerta C, Garcia Rodruguez LA.Risk of clinical blood dyscrasia in a cohort of antibiotic users. Pharmacotherapy. 2002;22:630–636. [DOI] [PubMed] [Google Scholar]
- 6.Bertuola F, Morando C, Menniti-Ippolito F, et al. Association between drug and vaccine use and acute immune thrombocytopenia in childhood. A case-control study in Italy. Drug Saf. 2010;33:65–72. [DOI] [PubMed] [Google Scholar]
- 7.George J, Raskob G, Rizvi Shah S, et al. Drug-induced thrombocytopenia: A systematic review of published case reports. Ann Intern Med. 1998;129:886–890. [DOI] [PubMed] [Google Scholar]
- 8.Anand A, Chauhan H.Piperacillin and vancomycin induced severe thrombocytopenia in a hospitalized patient. Platelet. 2011;22:294–301. [DOI] [PubMed] [Google Scholar]
- 9.Hartleb M, Biernat L, Kochel A.Drug-induced liver damage—a three-year study of patients from one gastroenterological department. Med Sci Monit. 2002; 8:292–296. [PubMed] [Google Scholar]
- 10.Rouveix B, Lassoued K, Vittecoq D, et al. Neutropenia due to b-lactamine antibodies. Br Med J. 1983;287:1832–1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polimeri G, Salvo F, Cutroneo PMet al. Adverse reactions induced by NSAIDs and antibacterials: Analysis of spontaneous reports from the Sicilian regional database. Drug Saf. 2006;29:449–459. [DOI] [PubMed] [Google Scholar]
- 12.Odio CM, Kusmiez H, Shelton S, et al. Comparative treatment trial of augmentin versus cefaclor for acute otitis media with effusion. Pediatrics. 1985;75:819–825. [PubMed] [Google Scholar]
- 13.Desgrandchamps D, Schnyder C.Severe neutropenia in prolonged treatment with orally augmentin (amoxicillin/clavulanic acid) [letter to the editor]. Infection. 1987;15:260–261. [DOI] [PubMed] [Google Scholar]
- 14.Augmentin XRFIRST, amoxicillin/clavulanate potassium extended release tablets [product information]. Research Triangle Park, NC: GlaxoSmithKline; 2006. [Google Scholar]
- 15.Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–245. [DOI] [PubMed] [Google Scholar]
- 16.Drug reactions and interactions. Drug-induced immune thrombocytopenia that increases platelet destruction results from antibody-related mechanisms. Drugs Ther Perspect. 2005;21:12 [Google Scholar]
- 17.Kenney B, Stack G.Drug-induced thrombocytopenia. Arch Pathol Lab Med. 2009;133:309–314. [DOI] [PubMed] [Google Scholar]
- 18.Aster RH, Curtis BR, McFarland JG, Bougie DW.Drug-induced immune thrombocytopenia: Pathogenesis, diagnosis, and management. J Thromb Haemost. 2009;7:911–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leger RM, Arndt PA, Garratty G.Serological studies of piperacillin antibodies. Transfusion. 2008;48:2429–2434. [DOI] [PubMed] [Google Scholar]
- 20.Grossjohann B, Eichler P, Greinacher A, et al. Ceftriaxone causes drug-induced immune thrombocytopenia and hemolytic anemia: Characterization of targets on platelets and red blood cells. Transfusion. 2004;44:1033–1040. [DOI] [PubMed] [Google Scholar]
- 21.Ten Berg MJ, van den Bemt PMLA, Shantakumar S, et al. Thrombocytopenia in adult cancer patients receiving cytotoxic chemotherapy: Results from a retrospective hospitalbased cohort study. Drug Saf. 2011;34:1151–1160. [DOI] [PubMed] [Google Scholar]
- 22.Perez-Vasquez A, Pastor JM, Riancho JA.Immune thrombocytopenia caused by piperacillin/tazobactam. Clin Infect Dis. 1998;27:650–651. [DOI] [PubMed] [Google Scholar]
- 23.Olivera E, Lakhani P, Watanakunakorn C.Isolated severe thrombocytopenia and bleeding caused by piperacillin. Scand J Infect Dis. 1998;27:650–651. [DOI] [PubMed] [Google Scholar]
- 24.Rousan TA, Aldoss IT, Cowley BD, et al. Recurrent acute thrombocytopenia in the hospitalized patient: Sepsis, DIC, HIT, or antibiotic-induced thrombocytopenia. Am J Hematol. 2009;85:71–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pedersen-Bjergaard U, Andersen M, Hansen PB.Drug-induced thrombocytopenia: Clinical data on 309 cases and the effect of corticosteroid therapy. Eur J Clin Pharmacol. 1997;52:183–189. [DOI] [PubMed] [Google Scholar]
- 26.Wazny LD, Ariano RE.Evaluation and management of drug-induced thrombocytopenia in the acutely ill patient. Pharmacotherapy. 200;20:292–307. [DOI] [PubMed] [Google Scholar]
- 27.George JN, Woolf SH, Raskob GE, et al. Idiopathic thrombocytopenic purpura: A practice guideline developed by explicit methods for the American Society of Hematology. Blood. 1996;88:3–40. [PubMed] [Google Scholar]
- 28.Kojouri K, Perdue JJ, Medina PJ, et al. Occult quinine-induced thrombocytopenia. J Okla State Med Assoc. 2000;93:519–521. [PubMed] [Google Scholar]
- 29.Kereiakes DJ, Essell JH, Abbottsmith CW, et al. Abciximab-associated profound thrombocytopenia: Therapy with immunoglobulin and platelet transfusion. Am J Cardiol. 1996;78:1161–1163. [DOI] [PubMed] [Google Scholar]