Abstract
Introduction
The seeds of Abrus precatorius contain the highly toxic plant protein abrin. There is no antidote for abrin poisoning. Management, largely supportive, may consist of administering intravenous fluids, anti-emetics, and activated charcoal depending on the time of exposure. We report the presentation of a single case of unintentional abrin poisoning confirmed by the quantitation of l-abrine biomarker.
Case Report
A previously healthy 22-month-old, 11.5-kg female presented to the hospital after ingesting approximately 20 rosary peas (A. precatorius) sold as a “peace bracelet”. Her primary manifestations were episodes of forceful emesis that included food particles progressing to clear gastric fluid. The patient was tachycardic (HR = 134 bpm) but had brisk capillary refill and normal blood pressure (96/60 mmHg). Laboratory testing revealed elevated blood urea nitrogen (16 mg/dL) and serum creatinine (0.4 mg/dL). In the emergency department, the patient was resuscitated with 40 mL/kg normal saline via peripheral IV and received ondansetron (0.15 mg/kg IV) to control retching. The patient was discharged well 24 h after the ingestion.
Discussion
This is the first case of human abrin toxin poisoning confirmed by the quantitation of l-abrine as a biomarker. Quantifying the levels of abrin toxin in the body after exposure can help clinicians make informed decisions when managing patients with symptomatic exposures to seeds of A. precatorius.
Keywords: Abrin, Mechanisms of toxicity, Poisoning, Ribosome-inactivating proteins
Introduction
The seeds of Abrus precatorius (also known as rosary peas) are often incorporated into costume jewelry. These peas, however, contain the highly toxic plant protein abrin, which has a reported fatal dose of 0.1–1 μg/kg in humans [2]. The abrin protein contains two polypeptide chains (designated α and β) that are water soluble. When masticated rosary peas are ingested, abrin is released into the digestive fluids and absorbed by the body. After absorption, the β-chain of the protein binds to cell membranes and aids entry of the α-chain into the cell. Inside the cell, the α-chain attaches to 28S rRNA by removing adenine bases from vital positions on the ribosomal chain [3]. The abrin-rRNA attachment inhibits mRNA decoding, leading to extreme reduction in protein synthesis and subsequent cell death. Children with access to rosary pea jewelry can accidentally ingest the peas, exposing them to the abrin toxin which can lead to life-threatening conditions such as gastrointestinal bleeding, dehydration, seizures, and organ failure. We report the presentation of a 22-month-old patient poisoned by abrin after unintentional ingestion of rosary peas and describe briefly the method of confirmatory diagnosis through the quantitation of the urinary biomarker l-abrine (N-methyl-l-tryptophan) using liquid chromatography mass spectrometry. This is the first confirmed case of abrin poisoning in humans where the level of toxin exposure is quantified by the l-abrine biomarker. This case report provides useful information for management of future abrin exposures.
Case Report
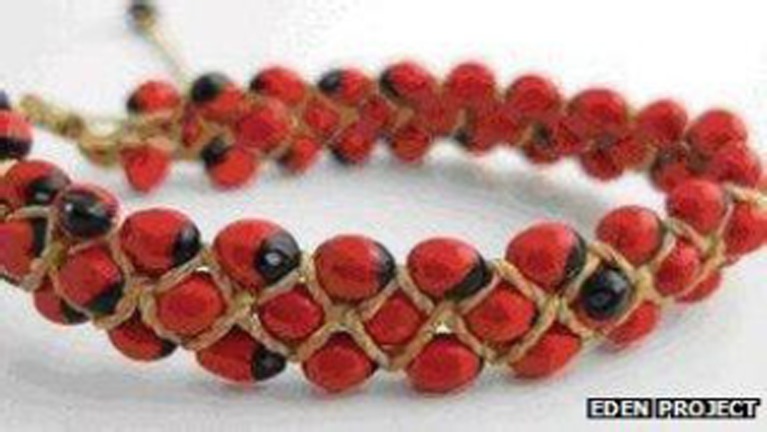
A previously healthy 22-month-old, 11.5-kg female ingested approximately 20 rosary peas (A. precatorius) sold as a “peace bracelet” (Fig. 1). When the parents noticed the child coughing, only one intact pea remained. The child spit out several chewed pea fragments; however, it is unknown how many peas were swallowed intact and how many were chewed. The child appeared to have a normal appetite and activity level through the remainder of the afternoon. Approximately 6 h after ingestion, the patient began vomiting. The parents reported five episodes of forceful emesis that included food particles progressing to clear gastric fluid, and ultimately to retching without emesis. No rosary peas, pea fragments or blood were noted in the vomitus, which was the more prominent feature. She was transported by private vehicle to the emergency department of the local children’s hospital. Upon arrival, the patient was lethargic but awake and smiling. She was tachycardic (HR = 134 bpm) but had brisk capillary refill and normal blood pressure (96/60 mmHg). Complete blood count, coagulation profile, blood chemistries, and liver function tests were all normal except for slightly elevated blood urea nitrogen (BUN; 16 mg/dL) and serum creatinine (0.4 mg/dL). Urine analysis was unremarkable except for elevated specific gravity (1.020). Urine and serum toxicology screens were negative for amphetamines, barbiturates, benzodiazepines, cocaine metabolites, opiates, THC, PCP, methadone, propoxyphen, tricyclic antidepressants, acetaminophen, ASA, and ethanol. In addition, a 12-lead EKG test was normal. Examination of the patient’s stool revealed no blood or diarrhea; however, the patient had one loose, not watery stool.
Fig. 1.
Rosary pea bracelet; courtesy of Cornwell Council [1]
In the emergency department, the patient was resuscitated with 40 mL/kg normal saline via peripheral IV, administered as two 20 mL/kg blouses in rapid succession over approximately 1 h; she also received ondansetron (0.15 mg/kg IV) to control retching. Her heart rate decreased to 110 bpm after fluid resuscitation; urine output was normal. She was admitted to a monitored bed in the Intermediate Care Unit for observation. She remained awake and alert with normal vital signs. She was given clear liquids and advanced to a regular diet when emesis ceased. By the following morning, she continued to look well; laboratory results were improved: BUN 8 mg/dL and creatinine <0.3 mg/dL. The patient was discharged in good condition 24 h after the ingestion. During follow-up, no further episodes of emesis were reported after discharge.
Following preliminary consultation with the US Centers for Disease Control and Prevention (CDC), the diagnosis of abrin poisoning was confirmed. After informed consent, approximately 500 μL of fresh urine was obtained from the patient within 24 h and sent to the CDC, where the diagnosis of abrin poisoning was confirmed by quantitation of l-abrine, a small molecule biomarker of abrin exposure, using a previously reported liquid chromatography tandem mass spectrometry (LC-MS/MS) assay [4]. Briefly, the assay consisted of enriching 200 μL of the patient’s urine sample with 30 μL of labeled 13CD3-l-abrine internal standard. The l-abrine toxin was extracted from the urine mixture by solid phase extraction techniques, and quantitated by high performance liquid chromatography mass spectrometry analysis. The range of the method calibration curve was 5–500 ng/mL, which is where most exposures are expected to occur, and the limit of detection is 5.0 ng/mL. In addition to l-abrine quantitation, creatinine measurements were also performed on the patient’s urine sample. After hospital admittance, the patient’s lab results showed serum creatinine of 0.4 mg/dL which dropped to <0.3 mg/dL by the following morning. In contrast, we measured the urine creatinine level as 42.6 mg/dL in the sample provided. Moreover, the analysis of the patient’s sample showed that the concentration of l-abrine was 726 ng/mL, which was above the highest point on the calibration curve. After a 5:1 dilution of the original sample with high-performance liquid chromatography-grade water, the analysis was repeated. Using the urine sample creatinine concentration (0.426 g/L) measured in-house on the new results, the creatinine-adjusted l-abrine concentration was 1,703 μg l-abrine/g creatinine.
Discussion
One of the most toxic plants found in nature is jequirity (Abrus precatourius) [4, 5]. The plant produces seeds known as rosary peas which, because of their attractive appearance, are often made into inexpensive costume jewelry [6, 7]. Occasionally, children with access to rosary pea jewelry accidentally swallow masticated peas and are exposed to the toxin abrin. Because there is no antidote for abrin poisoning, it should be removed from the body as quickly as possible. Patient management can consist of resuscitation with intravenous fluids, medications to treat emerging symptoms, and activated charcoal for early presentations if tolerated. We have described the first application of a previously developed clinical assay for the quantitative detection of l-abrine [4] to a 22-month-old patient unintentionally poisoned by the toxin abrin while chewing rosary peas found in a bracelet.
We present a useful detection method for l-abrine, developed for public health emergency response purposes. This method is based on a similar approach for detecting exposure to castor bean product. l-abrine is extracted from rosary peas; it passes through the host after masticated peas are eaten, and can be measured in urine. A previous analysis of 113 individual urine samples showed trace levels of l-abrine in people with no known exposure to the toxin abrin. The origin of the l-abrine in the unexposed population is unknown, but may derive from diet because l-abrine is a tryptophan derivative. Background levels of l-abrine in the individual samples ranged from 0.72 ± 0.51 ng/mL (mean ± 1 standard deviation), and creatinine-corrected values as 0.49 ± 0.44 μg l-abrine/g creatinine [4]. In the exposure case reported here involving a 22-month-old toddler, our results for creatinine-corrected concentration of 1,703 μg l-abrine/g creatinine is well above reported background levels.
Several other diagnostic tests have been previously used to confirm abrin poisoning. Ribosome-inactivation tests can accurately determine if clinical samples test positive for the toxin abrin [3, 8]; however, the test cannot provide a measure of the concentration of abrin in the body which may help in patient management. Abrin antibody detection and radioimmunoassay tests have also been used to detect abrin exposure in clinical samples [2–9]. While these tests are sensitive and can provide quantitative results, they require large sample volume, overnight incubation (in the case of radioimmunoassay test), and more invasive procedures to obtain patient samples [2, 11].
This case illustrates the successful clinical application of this specific analytic method for confirmation of abrin exposure. The procedure described here for the analysis of clinical samples from potentially exposed patients is rapid, sensitive, noninvasive, and requires small sample volumes (200 μL). This method gives quantified results with a limit of detection of 5 ng/mL. In addition to its use in confirming ingestion of rosary pea-containing products, this method is ideally suited for rapid screening of suspected abrin-exposed individuals in the event of a mass abrin exposure and public health emergency.
Acknowledgments
We would like to thank Mr. Stephen Stanfill for technical editing of this manuscript.
Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry.
References
- 1.“Jequirity Bean Bracelet Recall” Cornwall Council. http://www.cornwall.gov.uk/default.aspx?page=30980. October 10, 2012. Web March 23, 2012
- 2.Dickers K J et al (2003) Abrin poisoning. Toxicol Rev 22:137–142 [DOI] [PubMed]
- 3.Refsnes K et al (1973) On the toxic proteins abrin and ricin. J Biol Chem 11:3557–3562 [PubMed]
- 4.Johnson RC, et al. Quantification of l-abrine in human and rat urine: a biomarker for the toxin abrin. J Anal Toxicol. 2009;33:77–84. doi: 10.1093/jat/33.2.77. [DOI] [PubMed] [Google Scholar]
- 5.Yu-Huei L, et al. Involvement of prohibitin upregulation in abrin-triggered apoptosis. Evid Based Complement Alternat Med. 2012;2012:11. doi: 10.1155/2012/605154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patocka J, et al. Abin and ricin—two dangerous poisonous proteins. ASA Newsl. 2001;85:16–20. [Google Scholar]
- 7.Reedman L, et al. Survival after an intentional ingestion of crushed abrus seeds. West J Emerg Med. 2008;9:157–159. [PMC free article] [PubMed] [Google Scholar]
- 8.Goldman ER, et al. LIama-derived single domain antibodies specific for abrus agglutinin. J Toxins. 2011;3:1405–1419. doi: 10.3390/toxins3111405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gao S, et al. Colloidal gold-based immunochromatographic test strip for rapid detection of abrin in food samples. J Food Protect. 2012;75:112–117. doi: 10.4315/0362-028X.JFP-11-252. [DOI] [PubMed] [Google Scholar]
- 10.Xiao-Bing L, et al. Preperation and identification of monoclonal antibody against abrin-a. J Agric Food Chem. 2011;59:9796–9799. doi: 10.1021/jf202534y. [DOI] [PubMed] [Google Scholar]
- 11.Godal A, et al. Radioimmunoassays of arbrin and ricin in blood. J Toxicol Environ Health. 1981;8:409–417. doi: 10.1080/15287398109530079. [DOI] [PubMed] [Google Scholar]