Abstract
Aims
The present study examined whether lifetime cocaine use consequences mediate the relationship between trait impulsiveness and current depression symptoms among regular cocaine users.
Methods
Regular cocaine users (N = 108) were assessed using: Barratt Impulsiveness Scale subscales (non-planning, attentional, motor sub-scales) to measure trait impulsiveness; a standardized Drug History and Use Questionnaire to measure cocaine use and related consequences; and Beck Depression Inventory to measure current depression symptoms.
Results
All impulsiveness subscales were positively associated with an earlier age of first cocaine use, a higher degree of current depression symptoms and a greater number of lifetime cocaine use consequences. In three separate simple mediation tests, lifetime cocaine use consequences partially mediated the relationship between each of the impulsiveness subscales (non-planning: R2 = .42; attentional: R2 = .40; motor: R2 = .24) and current depression symptoms. Separate moderated mediation analyses failed to demonstrate an interaction between lifetime cocaine use and cocaine-related consequences predicting depression symptoms for the mediation models.
Conclusions
Cocaine-related consequences function in a more nuanced manner than just an outcome of impulsiveness or cocaine use, but as a pathway between trait impulsiveness and current depression symptoms.
Keywords: cocaine, impulsiveness, depression, cocaine use consequences, pathways
1. Introduction
Regular cocaine users report higher levels of trait impulsiveness than non-users (Coffey, Gudleski, Saladin, & Brady, 2003; Patkar et al., 2004b; Poling, Kosten, & Sofuoglu, 2007; Vonmoos et al., 2013). More importantly from the standpoint of clinical prediction, high trait impulsiveness is associated with increased cocaine use quantity and long-term cocaine consumption (Moeller et al., 2001; Vonmoos et al., 2013), increased craving (Tziortis, Mahoney, Kalechstein, Newton, & De La Garza, 2011), fewer days of treatment attendance (Moeller et al., 2001; Patkar et al., 2004a, 2004b), greater withdrawal symptom severity (Moeller et al., 2001), and a greater number of depression symptoms (Vonmoos et al., 2013).
Regular cocaine users also report substantially higher rates of lifetime major depression (Falck, Wang, Siegal, & Carlson, 2004; Herrero, Domingo-Salvany, Torrens, & Brugal, 2008) and current major depression (Rounsaville et al., 1991) than non-users. Hasin and colleagues (2002) examined the time sequence of depression and cocaine and substance dependence; participants demonstrated nearly four times the likelihood of substance-induced or abstinence-induced major depression compared to prior-onset major depression. Comorbid depression among regular cocaine users has been associated with greater urges to use cocaine during treatment (Brown et al., 1998), increased subjective high when using cocaine and increased depressive symptoms during initial abstinence (Uslaner, Kalechstein, Richter, Ling, & Newton 1999), greater likelihood of relapse (Hasin et al., 2002; McKay et al., 2002), and poorer medication response aimed at reducing cocaine use (Gonzalez, Feingold, Oliveto, Gonsai, & Kosten, 2003).
Impulsiveness is a multi-dimensional construct tied to antecedents and consequences of cocaine and other drug dependence (de Wit, 2009; Perry & Carroll, 2008; Winstanley, Olausson, Taylor, & Jentsch, 2010), making it important to distinguish mechanisms of influence. There are several pathways through which impulsiveness might alter the expression (e.g. course, severity) of cocaine use, abuse, and dependence. For instance, recent data indicate that cocaine users with higher (vs. lower) trait impulsiveness have reduced frontal-cortical gray matter (Crunelle et al., 2014; Moreno-Lopez et al., 2012), which may perpetuate cocaine use and exacerbate its long-term adverse consequences via reduced executive control of behavior (Jentsch & Taylor, 1999) and/or emotion dysregulation (Fox, Axelrod, Paliwal, & Sinha, 2007). One pathway that may connect impulsiveness to depression is through chronic cocaine use-related adverse consequences. In a recent study, higher trait impulsiveness among recreational and dependent cocaine users was correlated with greater depression symptoms and long-term cocaine consumption (Vonmoos et al., 2013).
High levels of trait impulsiveness among regular cocaine users seem to increase risk of greater cocaine-use consequences and comorbid depression symptoms (Moeller et al., 2001; Vonmoos et al., 2013). Although clinically relevant, it is not clear how trait impulsiveness exerts an influence on depression symptoms among chronic cocaine users. Thus, the aim of the present investigation was to examine the psychological mechanisms and outcomes associated with regular cocaine use. To accomplish this aim, we assessed trait impulsiveness, lifetime cocaine use and related consequences, and current depression symptoms among a sample of regular cocaine users. We specifically evaluated whether lifetime cocaine use consequences might mediate the relationship between trait impulsiveness and current depression symptoms. A variable can be considered a mediator, “to the extent that it accounts for the relation between predictor and criterion” (Baron & Kenny, 1986, p. 1176). Mediation analyses are advantageous because causality can be prioritized with the independent variable (i.e., trait impulsiveness) preceding the mediator (i.e., lifetime cocaine use consequences) in temporal sequence to predict the criterion (i.e., current depression symptoms; Baron & Kenny, 1986).
We theorized that depression symptoms would primarily function as an outcome of impulsive cocaine use-related consequences (see Hasin et al., 2002). To test this possibility, we hypothesized that the number of lifetime cocaine use negative consequences would mediate the relationship between trait impulsiveness and acute depression symptoms. Specifically, we predicted that regular cocaine users with a higher degree of trait impulsiveness would experience a greater number of lifetime cocaine use consequences and, as a result, experience a higher degree of current depression symptoms.
2. Material and methods
The local Institutional Review Board approved this study, which was conducted according to the Declaration of Helsinki. A Certificate of Confidentiality was obtained from the National Institutes of Health to provide further legal protection against forced disclosure of confidential study data.
2.1. Participants and Procedure
Cocaine users (N = 108), ages 18-55 years who were not seeking treatment for their substance use were recruited via newspaper advertisements and word-of-mouth referral in the Detroit/metropolitan area for possible participation in one of two experimental laboratory-based cocaine self-administration studies, registered on www.clinicaltrials.gov as NCT 00946660 (Greenwald et al., 2014) and NCT 01392092.
Individuals who passed an initial telephone-screening interview were invited to undergo in-person comprehensive screening procedures. All participants were remunerated $25 for attending the screening session, during which they provided written informed consent for all screening assessments. In the event their screening session required additional time, participants were remunerated an additional $10 to complete the screening during a second session.
2.2. Measures
Alcohol-free breath samples (< .002%; Alco Sensor III breathalyzer) and no evidence of cognitive impairment based on estimated IQ score > 80 (Shipley Institute of Living Scale; Zachary, 1991) were required for informed consent. Volunteers provided a urine sample that was analyzed on-site for cocaine metabolites, benzodiazepines, opioids (positive cutoff ≥ 300 ng/ml), amphetamines (≥ 1000 ng/ml), barbiturates (≥ 200 ng/ml), and THC metabolites (≥ 50 ng/ml). However, urinalysis results did not determine inclusion in this analysis.
2.2.1. Cocaine use
Substance use screening included a locally developed, standardized, comprehensive Drug History and Use Questionnaire [DHUQ, routinely used in our laboratory studies, e.g. Greenwald, Steinmiller, Śliwerska, Lundahl, & Burmeister, 2013]. Cocaine use data obtained from the DHUQ included: Age of first cocaine use, age of first regular (three times a week or more) cocaine use, number of days using cocaine in the past month, number of days using cocaine in the past week, average number of cocaine uses/day during the past week, and the number of days using cocaine in the past week multiplied by the average number of cocaine uses/day during the past week. We also used DHUQ data to estimate the number of lifetime cocaine uses (ordinal response). For this analysis, we focused on the number of lifetime cocaine uses and cocaine-related consequences outlined in the questionnaire. Finally, the DHUQ lists 18 different types of potential consequences of lifetime cocaine use: overdose, seizure, shake/tremor, tolerance, impaired control, legal problem, accident/injury, health problem, intoxicated at work, missed work, lost job, intoxicated at school, missed school, fight, driving under the influence, family problem, financial problem, and emergency department visit. The participant checked whether s/he had ever experienced each event (scored present/absent); the total score reflects the number of different types of lifetime consequences endorsed.
2.2.2. Trait impulsiveness
The Barratt Impulsiveness Scale (BIS-11; Barratt & Patton, 1983; Patton, Stanford, &Barratt, 1995; Zaparniuk & Taylor 1997) is a 30-item standardized self-report measure of trait impulsiveness; the scale includes 3 second-order subscales: attentional (impulsive decision making), motor (propensity to engage in spontaneous behavior) and non-planning (lack of concern for the consequences of one's future actions).
2.2.3. Current depression symptoms
Current depression symptoms were assessed using the second version of the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996), a 21-item measure that assesses past 14-day neurovegetative depressive symptoms. Participants who scored in the range of moderate to severe depression were provided a referral for treatment. In the event suicidal thoughts were reported, a licensed clinical psychologist met with the participant to conduct a risk assessment and arrange for hospitalization if deemed necessary.
2.3. Data Analysis
Participants with DHUQ, BIS-11, and BDI-II data from the screening phase (regardless of whether they qualified for the above-noted laboratory studies) were included in the present analysis. All statistical tests were conducted using SPSS v. 22. Preliminary correlations (Pearson r), were conducted to assess the relationships the BIS-11 impulsiveness subscales, current depression symptoms [BDI-II], lifetime cocaine uses [DHUQ], and lifetime cocaine use consequences [DHUQ]. We chose to examine the BIS-11 subscales instead of the BIS-11 total score to gain a more precise understanding of the differential effects of different types of impulsiveness on cocaine use and consequences and current depression. Variables that were non-normally distributed were transformed as appropriate prior to analysis (age of cocaine use onset, age of regular cocaine use, and current depression scores were square root transformed; lifetime cocaine uses [DHUQ] was reflected and then inverse transformed) (Tabachnick & Fidell, 2013).
Mediation analyses were conducted to assess the mechanistic influence of lifetime cocaine use consequences on the relationship between trait impulsiveness and current depression symptoms. Previous studies have identified trait impulsiveness (X) as a risk factor (causal precedent) for both regular cocaine use (Coffey et al., 2003; Vonmoos et al., 2013) and lifetime cocaine use consequences (M) (Moeller et al., 2001). In addition, Baron and Kenny (1986) recommend that the dependent variable (Y) should not cause the mediator variable (M). That is, current depression symptoms cannot cause lifetime cocaine use consequences. In sum, this project followed the recommended guidelines (Baron & Kenny, 1986; Preacher & Hayes, 2004) for mediation analyses, thus allowing for tests that prioritize the causal relationships between trait impulsiveness (X), lifetime cocaine use consequences (M), and current depression symptoms (Y). In addition, we conducted moderated mediation analyses (Preacher, Rucker, & Hayes, 2007), which examined whether lifetime cocaine use (W: moderator) interacted with the number of lifetime cocaine use consequences (M) to predict current depression symptoms (Y) when controlling for trait impulsiveness (X)
After estimating the direct effects of the simple mediation models, a bootstrapping technique (Preacher & Hayes, 2004) was applied to estimate indirect effects. Bootstrapping (with 1000 iterations) was used to offset the limitation of using Baron and Kenny's recommended Sobel (1982) test to estimate indirect effects. The Sobel test was designed for large sample sizes, and is more likely (than bootstrapping) to produce Type II errors when using small samples (Preacher & Hayes, 2004). In contrast, bootstrapping allows for testing indirect effects with almost any sample size (Preacher et al., 2007). In addition to direct and indirect effects, we also derived effect size (R2) for all three simple mediation models. For the three moderated mediation analyses, we examined the interaction between lifetime cocaine use and lifetime cocaine use consequences (on the b path) predicting current depression symptoms (Preacher et al., 2007).
3. Results
3.1. Sample demographics, cocaine use, trait impulsiveness, and current depression symptoms
The sample (N = 108) was primarily male (n = 88, 81.5%) and African-American (n = 87, 80.6%). Age of participants ranged from 24 – 57 years old (M = 45.5, SD = 7.1). Forty-two percent (n = 45) of participants completed some high school or a high school degree (or equivalent), nearly half (n = 53, 49.1%) had attended college, and the remaining participants (n = 10, 9.3%) completed a bachelor's degree or more.
Participants typically used cocaine for the first time during their mid-20's (M = 25.1, SD = 7.2), with regular use beginning on average less than three years later (M = 27.6, SD = 7.2). Participants' duration of time since first cocaine use was about 20 years (M = 20.4, SD = 8.2), with duration of regular use roughly three years fewer (M = 17.9, SD = 8.0). Participants reported using cocaine roughly half the days over the past month (M = 15.2, SD = 8.8) and using cocaine, on average, every other day during the past week (M = 3.5, SD = 2.1). Participants reported using cocaine about four times per day (M = 4.0, SD = 3.7). Smoking crack cocaine (n = 91, 84.3%) was the most common current route of administration; all remaining participants reported snorting (n = 15, 13.9%) as current route. Most participants (n = 79, 73.1%) provided a cocaine positive urine sample at screening, and roughly a third of participants (n = 34, 32.1%) had a THC positive urine sample. Total scores on the DHUQ consequences scale ranged from 0 – 17 (maximum possible score = 18), with participants reporting an average of about five lifetime cocaine use negative consequences (M = 4.9, SD = 4.2).
Scores for the BIS-11 impulsiveness subscales were as follows: attentional (M = 15.1, SD = 4.1), motor (M = 23.4, SD = 5.0), and non-planning (M = 26.4, SD = 5.8). Participants' current depression symptom total scores ranged from 0 – 39 (M = 12.3, SD = 10.0). BDI-II scores of 14 or more indicate clinically relevant symptoms of depression (Beck et al., 1996) (n = 42, 38.9%). Within this sample, approximately one in six participants reported mild depression (scores of 14 – 19; n = 17, 15.7%), nearly one in ten reported moderate depression symptoms (scores of 20 – 28; n = 10, 9.3%), and approximately one in eight participants reported severe depression symptoms (scores of 29 – 63; n = 13, 12.0%).
3.2. Correlations among trait impulsiveness, cocaine use and cocaine-related consequences, and current depression symptoms
Table 1 presents correlations among the major study variables (trait impulsiveness subscales, lifetime cocaine use, lifetime cocaine use consequences, current depression symptoms) that were used in mediation analyses, as well as age of cocaine use onset and age of regular cocaine use. Positive relationships were observed between scores for all three impulsiveness subscales and current depression symptoms. All three impulsiveness subscales were positively associated with lifetime cocaine use consequences. A higher total number of lifetime cocaine use consequences were associated with higher current depression symptom scores. A greater number of lifetime cocaine uses was positively associated with a greater number of lifetime cocaine use consequences but unrelated to current depression symptoms. Higher non-planning impulsiveness was associated with a greater number of lifetime cocaine uses. Because lifetime cocaine use was not associated with current depression symptoms, mediation analysis was not conducted with this variable.
Table 1.
Correlations among trait impulsiveness, cocaine use and cocaine-related consequences, and current depression symptoms
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| Mediation Variables | 1 BIS-11 Attentional | .57*** | .66*** | .20* | .53*** | .05 | −.21* | −.09 | |
| 2 BIS-11 Motor | .45*** | .36*** | .35*** | .06 | −.30** | −.25** | |||
| 3 BIS-11 Non-Planning | .36*** | .60*** | .19* | −.20* | −.10 | ||||
| 4 DHUQ Lifetime Consequences | .44*** | .27** | −.24* | −.20* | |||||
| 5 BDI-II | .17 | −.21* | −.23* | ||||||
| 6 DHUQ Lifetime Cocaine Uses | −.19* | −.28* | |||||||
| Other Variables | 7 DHUQ Age of Cocaine Use Onset | .82*** | |||||||
| 8 DHUQ Age of Regular Cocaine Use |
Note.
p <.05
p <.01
p <.001.
Note. (1) Barratt Impulsiveness Attentional Scale; (2) Barratt Impulsiveness Motor Scale; (3) Barratt Impulsiveness Non-Planning Scale; (4) Drug History and Use Questionnaire Number of Lifetime Cocaine Use Consequences; (5) Beck Depression Inventory-II; (6) Drug History and Use Questionnaire Number of Lifetime Cocaine Uses (7) Drug History and Use Questionnaire Age of Cocaine Use Onset; and (8) Drug History and Use Questionnaire Age of Regular Cocaine Use (3 or more times a week).
All three impulsiveness subscales were associated with a younger age of first cocaine use. Higher scores for motor impulsiveness were associated with an earlier age of regular cocaine use. Both an earlier age at initial cocaine use and earlier onset of regular cocaine use were associated with a greater number of lifetime cocaine uses, lifetime cocaine use consequences, and current depression symptoms.
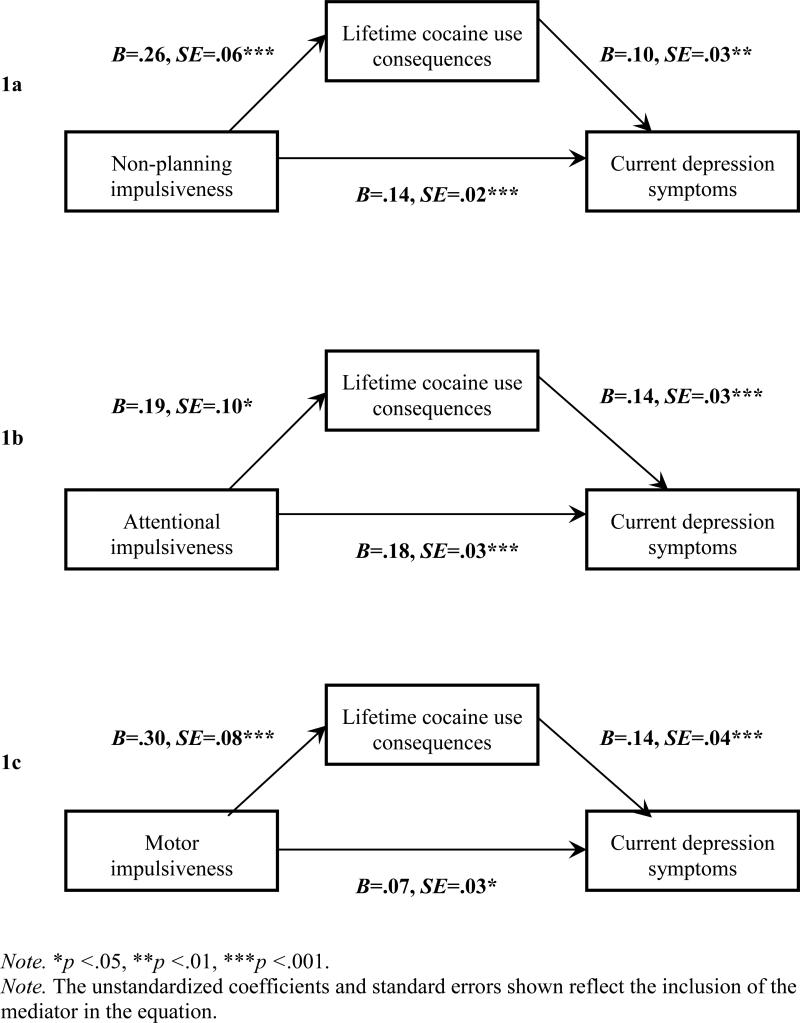
3.3. Mediation models explain current depression symptoms
Three simple mediation analyses were conducted (presented in Figures 1a, 1b, 1c) based on Baron and Kenny's (1986) recommended series of regression equations to test mediation. The first simple mediation model was tested to determine whether the indirect effect of non-planning impulsiveness on current depression symptoms via lifetime cocaine use consequences was significantly different from zero (Figure 1a). The direct effect of X (non-planning impulsiveness) on Y (current depression symptoms) (B = .14, SE = .02) was significant (p < .001). The indirect effect through lifetime cocaine use consequences was estimated to lie between .01 and .05 with 95% confidence, which is significantly different from zero at p < .05 (two tailed). Both the direct and indirect effects were significant, indicating that lifetime cocaine use consequences partially mediated the relationship between non-planning impulsiveness and current depression symptoms (R2 = .42)
Figure 1.
Mediation models with non-planning (1a), attentional (1b) and motor (1c) impulsiveness (X), lifetime cocaine use consequences (M), and current depression symptoms (Y)
The second simple mediation model was tested to determine whether the indirect effect of attentional impulsiveness on current depression symptoms via lifetime cocaine use consequences was significantly different from zero (Figure 1b). The direct effect of X (attentional impulsiveness) on Y (current depression symptoms) (B = .18, SE = .03) was significant (p < .001). The indirect effect through lifetime cocaine use consequences was estimated to lie between .01 and .06 with 95% confidence, which is significantly different from zero at p < .05 (two tailed). Both the direct and indirect effects were significant, indicating that lifetime cocaine use consequences partially mediated the relationship between attentional impulsiveness and current depression symptoms (R2 = .40)
The third simple mediation model was tested to determine whether the indirect effect of motor impulsiveness on current depression symptoms via lifetime cocaine use consequences was significantly different from zero (Figure 1c). The direct effect of X (motor impulsiveness) on Y (current depression symptoms) (B = .07, SE = .03) was significant (p < .05). The indirect effect through lifetime cocaine use consequences was estimated to lie between .02 and .08 with 95% confidence, which is significantly different from zero (p < .05). Both the direct and indirect effects were significant, indicating that lifetime cocaine use consequences partially mediated the relationship between motor impulsiveness and current depression symptoms (R2 = .24).
We considered whether specific or subsets of cocaine-related consequences might differentially influence the relationship between impulsiveness and depression. All items were dichotomous; therefore mediation analyses could not be conducted with single items. The strongest relationships (in bivariate analyses) between specific cocaine-related consequences, impulsiveness subscales, and current depression were observed for financial problems, family problems, and job loss. Reliability and dimension reduction analyses determined that examining subsets (dimensions) of the [DHUQ] cocaine use consequence scale was unwarranted (i.e., a single-factor scale was indicated following internal consistency and item analyses, and scree plot, Eigenvalue, and factor loading interpretation).
We also considered the influence of lifetime cocaine use as a moderator of the relationship between cocaine use consequences and current depression (when controlling for impulsiveness subscales) in three separate moderated mediation models. All moderated mediation analyses failed to reveal a significant interaction between lifetime cocaine use and cocaine use consequences predicting depression symptoms (when controlling for each of the three impulsiveness subscales).
4. Discussion
This study examined causal pathways involving three constructs that have been associated with regular cocaine use in prior research, in an effort to clarify the complex relationship between impulsiveness, cocaine use consequences, and depression symptoms.
Prior research identified impulsiveness as a risk factor for cocaine use, cocaine-related consequences, and depression (Falck et al., 2004). In addition, cocaine users with co-morbid depression symptoms have demonstrated worse treatment response (e.g., stronger urges to use during treatment; Brown et al., 1998), higher rates of relapse (Hasin et al., 2003), and poorer medication response aimed at reducing cocaine use (Gonzalez et al., 2003). We found support for impulsiveness as a risk factor for lifetime cocaine use, cocaine use consequences, recent depression symptoms, and a relationship between co-morbid depression symptoms and cocaine use consequences. This project provides a novel understanding of the possible pathways for these relationships with two key additions to the literature: 1) depression symptoms accrue as a distal outcome of high trait impulsiveness, which exerts a persistent (lifetime) effect on cocaine use consequences independent of the amount of lifetime cocaine use, and 2) depression symptoms are engendered more proximally in response to cocaine use consequences and not simply as a result of the level of cocaine used over one„s lifetime. Taken together, these findings strengthen the existing literature by addressing these important gaps.
These results may inform clinical practice such that clinicians will better understand the relationship between impulsiveness, cocaine use and consequences, and depression. Specifically, our findings support the conceptualization that depressive symptoms may primarily result from and are proportional to lifetime cocaine use-related consequences (financial problems, family discord, and job loss). This viewpoint is in line with substance-induced depressive disorders, which radically differs from the conceptualization outlined by major depressive symptoms, which are primarily related to negative thoughts and beliefs that are independent of cocaine use consequences. Future research could examine the impact of consequence-induced depression symptoms on prospective cocaine use and cocaine use consequences, e.g., using longitudinal assessments of these indices, and analyzing the data with growth models or structural equation models. Using a prospective design could serve to gain an even clearer understanding of the vicious cycle between cocaine use, consequences, and depression. Future research should also examine these causal relationships among different demographic populations. We did not find a moderating role for gender or age, but it is possible these relationships would be influenced by other demographic variables.
This study has some limitations. It is possible that the recruitment strategy and/or sample characteristics influenced our findings; and our study relied on self-report measures. We did not find a relationship between impulsiveness and recent cocaine use quantity/frequency although this null finding is consistent with prior work (Vonmoos et al., 2013). However, we did find a relationship between impulsiveness and a higher number of lifetime cocaine uses. Our findings build on prior research that has demonstrated impulsiveness as a discriminating factor between controls and regular users (Vonmoos et al., 2013). In the current sample of regular cocaine users, impulsiveness was a key risk factor for experiencing a greater number of cocaine use consequences.
In summary, this study sought to explore the relationship between impulsiveness, cocaine use consequences, and depression symptoms among regular cocaine users. Previous research has demonstrated that chronic users are more likely to report a higher degree of impulsiveness, comorbid depression, and a greater number of consequences related to their cocaine use. This study sought to proxy the causative sequence of each of these factors, and in doing so, contributes to a better understanding of the relationships between these factors. We found that cocaine use consequences mediated the relationship between impulsiveness and depression symptoms, and remained a significant mediator independent of the amount of lifetime cocaine use of participants. These findings indicate that depression functions primarily as a response to impulsiveness and the level of cocaine use consequences experienced by among regular cocaine users.
Highlights.
Examined impulsiveness, cocaine use consequences and depression among cocaine users
Depression occurs as outcome of impulsiveness, which exerts effect on consequences
Cocaine use consequences function as pathway between impulsiveness and depression
Higher trait impulsiveness associated with earlier age of cocaine use onset
Cocaine use did not moderate the relationship between consequences and depression
Acknowledgements
The authors thank Ken Bates for participant recruitment, and Elorie Eggleston, Debra Kish, Joi Moore, Lisa Sulkowski and Melissa Williams for assistance with data collection and management.
Role of Funding Sources
This research was supported by a grant (Joe Young Sr./Helene Lycacki Funds) from the State of Michigan, the Detroit Wayne Mental Health Authority, NIH R01 DA026861 from the National Institute on Drug Abuse (to M.K.G.), and a postdoctoral research fellowship award (to J.J.L., with mentorship by D.M.L.) from the Wayne State University Office of the Vice President supported this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
All authors contributed to the writing and data analysis processes during the preparation of this manuscript. All authors have read and approved of this manuscript.
Conflict of Interest
There are no conflicts of interest to report.
References
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. http://dx.doi.org/10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barratt ES, Patton JH. Impulsivity: Cognitive, behavioral, and psychophysiological correlates. In: Zuckerman M, editor. Biological bases of sensation seeking, impulsivity, and anxiety. Erlbaum; Hillsdale, NJ: 1983. pp. 77–116. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Brown RA, Monti PM, Myers MG, Martin RA, Rivinus T, Dubreuil ME, Rohsenow DJ. Depression among cocaine abusers in treatment: Relation to cocaine and alcohol use and treatment outcome. The American Journal of Psychiatry. 1998;155:220–225. doi: 10.1176/ajp.155.2.220. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Gudleski GD, Saladin ME, Brady KT. Impulsivity and rapid discounting of delayed hypothetical rewards in cocaine-dependent individuals. Experimental and Clinical Psychopharmacology. 2003;11:18–25. doi: 10.1037//1064-1297.11.1.18. http://dx.doi.org/10.1037/1064-1297.11.1.18. [DOI] [PubMed] [Google Scholar]
- Crunelle CL, Kaag AM, van Wingen G, van den Munkhof HE, Homberg JR, Reneman L, van den Brink W. Reduced frontal brain volume in non-treatment-seeking cocaine-dependent individuals: Exploring the role of impulsivity, depression, and smoking. Frontiers in Human Neuroscience. 2014 doi: 10.3389/fnhum.2014.00007. http://dx.doi.org/10.3389/fnhum.2014.00007. [DOI] [PMC free article] [PubMed]
- de Wit H. Impulsivity as a determinant and consequence of drug use: A review of underlying processes. Addiction Biology. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. http://dx.doi.org/10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falck RS, Wang J, Siegal HA, Carlson RG. The prevalence of psychiatric disorder among a community sample of crack cocaine users: An exploratory study with practical implications. The Journal of Nervous and Mental Disease. 2004;192:503–507. doi: 10.1097/01.nmd.0000131913.94916.d5. http://dx.doi.org/10.1097/01.nmd.0000131913.94916.d5. [DOI] [PubMed] [Google Scholar]
- Fox HC, Axelrod SR, Paliwal P, Sinha SR. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug and Alcohol Dependence. 2007;89:298–301. doi: 10.1016/j.drugalcdep.2006.12.026. http://dx.doi.org/10.1016/j.drugalcdep.2006.12.026. [DOI] [PubMed] [Google Scholar]
- Gonzalez G, Feingold A, Oliveto A, Gonsai K, Kosten TR. Comorbid major depressive disorder as a prognostic factor in cocaine-abusing buprenorphine-maintained patients treated with desipramine and contingency management. The American Journal of Drug and Alcohol Abuse. 2003;29:497–514. doi: 10.1081/ada-120023455. http://dx.doi.org/10.1081/ADA-120023455. [DOI] [PubMed] [Google Scholar]
- Greenwald MK, Steinmiller CL, Śliwerska E, Lundahl LH, Burmeister M. BDNF Val66Met genotype is associated with drug-seeking phenotypes in heroin-dependent individuals: a pilot study. Addiction Biology. 2013;18:836–845. doi: 10.1111/j.1369-1600.2011.00431.x. http://dx.doi.org/10.1111/j.1369-1600.2011.00431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald MK, Ledgerwood DM, Lundahl LH, Steinmiller CL. Effect of experimental analogs of contingency management treatment on cocaine seeking behavior. Drug and Alcohol Dependence. doi: 10.1016/j.drugalcdep.2014.03.009. Epub 19 March 2014 http://dx.doi.org/10.1016/j.drugalcdep.2014.03.009. [DOI] [PMC free article] [PubMed]
- Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Archives of General Psychiatry. 2002;59:375–380. doi: 10.1001/archpsyc.59.4.375. http://dx.doi.org/10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Herrero MJ, Domingo-Salvany A, Torrens M, Brugal MT. Psychiatric comorbidity in young cocaine users: induced versus independent disorders. Addiction. 2008;193:284–293. doi: 10.1111/j.1360-0443.2007.02076.x. http://dx.doi.org/10.1111/j.1360-0443.2007.02076.x. [DOI] [PubMed] [Google Scholar]
- Jentsch JD, Taylor JR. Impulsivity resulting from frontostriatal dysfunction in drug abuse: Implications for the control of behavior by reward-related stimuli. Psychopharmacology. 1999;146:373–390. doi: 10.1007/pl00005483. http://dx.doi.org/10.1007/PL00005483. [DOI] [PubMed] [Google Scholar]
- McKay JR, Pettinati HM, Morrison R, Feeley M, Mulvaney FD, Gallop R. Relation of depression diagnoses to 2-year outcomes in cocaine-dependent patients in a randomized continuing care study. Psychology of Addictive Behaviors. 2002;16:225–235. http://dx.doi.org/10.1037/0893-164X.16.3.225. [PubMed] [Google Scholar]
- Moeller FG, Dougherty DM, Barratt ES, Schmitz JM, Swann AC, Grabowski J. The impact of impulsivity on cocaine use and retention in treatment. Journal of Substance Abuse Treatment. 2001;21:193–198. doi: 10.1016/s0740-5472(01)00202-1. http://dx.doi.org/10.1016/S0740-5472(01)00202-1. [DOI] [PubMed] [Google Scholar]
- Moreno-Lopez L, Catena A, Fernandez-Serrano MJ, Delgado-Rico E, Stamatakis EA, Perez-Garcia M, Verdejo-Garcia A. Trait impulsivity and prefrontal gray matter reductions in cocaine dependent individuals. Drug and Alcohol Dependence. 2012;125:208–214. doi: 10.1016/j.drugalcdep.2012.02.012. http://dx.doi.org/10.1016/j.drugalcdep.2012.02.012. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. http://dx.doi.org/10.1002/1097-4679(199511)51:6768::AID-JCLP22705106073.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Mannelli P, Certa KM, Peindl K, Murray H, Vergare MJ, Berrettini WH. Relationship of serum prolactin with severity of drug use and treatment outcome in cocaine dependence. Psychopharmacology. 2004a;176:74–81. doi: 10.1007/s00213-004-1856-0. http://dx.doi.org/10.1007/s00213-004-1856-0. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Murray HW, Mannelli P, Gottheil E, Weinstein SP, Vergare MJ. Pre-treatment measures of impulsivity, aggression, and sensation seeking are associated with treatment outcome for African-American cocaine-dependent patients. Journal of Addictive Diseases. 2004b;23:109–122. doi: 10.1300/J069v23n02_08. http://dx.doi.org/10.1300/J069v23n02_08. [DOI] [PubMed] [Google Scholar]
- Perry JL, Carroll ME. The role of impulsive behavior in drug abuse. Psychopharmacology. 2008;200:1–26. doi: 10.1007/s00213-008-1173-0. http://dx.doi.org/10.1007/s00213-008-1173-0. [DOI] [PubMed] [Google Scholar]
- Poling J, Kosten TR, Sofuoglu M. Treatment outcome predictors for cocaine dependence. The American Journal of Drug and Alcohol Abuse. 2007;33:191–206. doi: 10.1080/00952990701199416. http://dx.doi.org/10.1080/00952990701199416. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. http://dx.doi.org/10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. http://dx.doi.org/10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Anton SF, Carroll K, Budde D, Prusoff BA, Gawin F. Psychiatric diagnosis of treatment-seeking cocaine abusers. Archives of General Psychiatry. 1991;18:43–51. doi: 10.1001/archpsyc.1991.01810250045005. http://dx.doi.org/10.1001/archpsyc.1991.01810250045005. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological methodology 1982. Jossey-Bass; San Francisco: 1982. pp. 290–312. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed. Pearson Education; Upper Saddle River, NJ: 2013. [Google Scholar]
- Tziortis D, Mahoney JJ, Kalechstein AD, Newton TF, De La Garza R. The relationship between impulsivity and craving in cocaine-and methamphetamine-dependent volunteers. Pharmacology, Biochemistry and Behavior. 2011;98:196–202. doi: 10.1016/j.pbb.2010.12.022. http://dx.doi.org/10.1016/j.pbb.2010.12.022. [DOI] [PubMed] [Google Scholar]
- Ulsaner J, Kalechstein A, Richter T, Ling W, Newton T. Association of depressive symptoms during abstinence with the subjective high produced by cocaine. The American Journal of Psychiatry. 1999;156:1444–1446. doi: 10.1176/ajp.156.9.1444. [DOI] [PubMed] [Google Scholar]
- Vonmoos M, Hulka LM, Preller KH, Jenni D, Schulz C, Baumgartner MB, Quednow BB. Differences in self-reported and behavioral measures of impulsivity in recreational and dependent cocaine users. Drug and Alcohol Dependence. 2013;133:61–70. doi: 10.1016/j.drugalcdep.2013.05.032. http://dx.doi.org/10.1016/j.drugalcdep.2013.05.032. [DOI] [PubMed] [Google Scholar]
- Winstanley CA, Olausson P, Taylor JR, Jentsch JD. Insight into the relationship between impulsivity and substance abuse from studies using animal models. Alcoholism: Clinical and Experimental Research. 2010;34:1306–1318. doi: 10.1111/j.1530-0277.2010.01215.x. http://dx.doi.org/10.1111/j.1530-0277.2010.01215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachary RA. The manual of the Shipley Institute of Living Scale. Western Psychological Services; Los Angeles, CA: 1991. [Google Scholar]
- Zaparniuk J, Taylor S. Impulsivity in children and adolescents. In: Webster CD, Jackson MA, editors. Impulsivity: Theory, assessment, and treatment. Guilford Press; New York, NY: 1997. pp. 158–179. [Google Scholar]