Abstract
This study examined the association between restrictive eating behaviors and binge eating in anorexia nervosa (AN) using data collected in the natural environment. Women (N = 118) with DSM-IV full or sub-threshold AN reported eating disorder behaviors, including binge eating episodes, going ≥ 8 waking hours without eating, and skipping meals, during 2 weeks of ecological momentary assessment (EMA). Time-lagged generalized estimating equations tested the following hypotheses: 1) dietary restriction would predict binge eating while controlling for binge eating the previous day; 2) binge eating would predict restriction the subsequent day while controlling for restriction the previous day. After controlling for relevant covariates, the hypotheses were not supported; however, there appeared to be a cumulative effect of repeatedly going 8 consecutive hours without eating (i.e. fasting) on the risk of binge eating among individuals who recently engaged in binge eating. In addition, skipping meals was associated with a lower risk of same day binge eating. The relationship between binge eating and dietary restriction appears to be complex and may vary by type of restrictive eating behavior. Future research should aim to further clarify the nature of the interaction of binge eating and restrictive eating among individuals with AN in order to effectively eliminate these behaviors in treatment.
Keywords: Binge eating, Restriction, Anorexia nervosa
Introduction
The eating behaviors that characterize eating disorders are generally restrictive, appetitive, or purgative (American Psychiatric Association, 2013). Restrictive and purgative eating behaviors can be further described as compensatory when an individual engages in them in response to an eating episode (e.g., binge eating), although these behaviors also may occur independently of specific eating episodes (e.g., a day of fasting). Multiple converging sources of evidence suggest that restrictive eating behaviors (e.g., fasting, avoiding certain types of foods, and limiting the amount of foods eaten) may promote binge eating. For instance, prospective studies in adolescents demonstrate that restrictive eating predicts the onset of binge eating during the high school years (e.g., Stice, Killen, Hayward, & Taylor, 1998; Stice, Presnell, & Spangler, 2002); in animal studies, acute caloric restriction precipitates binge-like eating behavior (e.g., Mathes, Brownley, Mo, & Bulik, 2009); and in a naturalistic study of women with bulimia nervosa, restrictive eating behaviors predicted the next day occurrence of binge eating episodes (Zunker et al., 2011). However, an opposing line of research suggests that dietary restriction may actually reduce binge eating. Studies of weight loss interventions in overweight individuals have found that caloric restriction results in decreases in binge eating frequency (e.g., Goodrick, Poston, Kimball, Reeves, & Foreyt, 1998). Similarly, a weight maintenance intervention that included caloric restriction resulted in decreased binge eating in adolescent girls (Stice, Presnell, Groesz, & Shaw, 2005), and a 6-week weight loss diet in normal-weight women produced decreased binge eating (Presnell & Stice, 2003). Thus, findings regarding the relationship between restrictive eating behaviors and binge eating are mixed and may differ across populations.
Some of these inconsistencies may stem from confusion regarding two related but distinct constructs: dietary restriction and dietary restraint. Dietary restriction is the behavior of limiting caloric intake below energy requirements, and dietary restraint is the cognitive intent to do so (Stice, Fisher, & Lowe, 2004). Individuals may engage in dietary restriction through the cognitively mediated process of dietary restraint. In other words, individuals may restrict their intake below their needs purposely by attempting to (and succeeding at) restraining themselves from eating as much as they otherwise would. However, there are also other reasons individuals may engage in dietary restriction. For instance, forgetting to eat, experiencing an illness that interferes with appetite, poor planning leading to the unavailability of food, or economic limitations that impinge upon the ability to purchase food may each lead to dietary restriction. At the same time, dietary restraint need not lead to dietary restriction, and indeed dietary restraint does not predict short-term dietary restriction as measured by the actual amount of calories consumed (Stice et al., 2004). This may result from the difficulty of executing the intention to limit intake in the context of the modern environment in which food is generally plentiful and highly palatable (Lowe, 2003). Further, dietary restraint itself may actually increase the risk of binge eating by enhancing disinhibition around food after violations of the intention to limit intake (Johnson, Pratt, & Wardle, 2012). Some individuals, particularly those with eating psychopathology (Stice, Presnell, & Shaw, 2012), often aspire to unrealistic goals when it comes to limiting their intake; aspirations that they inevitably fail to accomplish. In the context of such failures, individuals may experience increased negative affect, disinhibition, and all-or-nothing thinking that lead to a binge eating episode, after which they recommit to their unrealistic goals and set the stage for the process to repeat (e.g., Herman & Mack, 1975). Thus, the intention to limit intake (i.e., dietary restraint) appears to be an important construct for understanding eating psychopathology but a poor proxy for dietary restriction. To avoid introducing further confusion to the literature, research on the relationship between binge eating and restrictive eating behaviors must be careful to ensure that measures of dietary restriction are not actually measures of restraint.
The risk for binge eating that is theoretically potentiated by restrictive eating is generally conceptualized as occurring over shorter (e.g., hours or days) versus longer (e.g., weeks, months, years) intervals, although other mechanisms function in long term appetite regulation (e.g., fat mass and leptin concentrations; Gil-Campos, Aguilera, Cañete, & Gil, 2006). Restrictive eating behaviors may lead to a state of acute caloric/nutrient deprivation that induces physiological hunger and results in a homeostatic drive to eat (Gil-Campos et al., 2006). Thus, consistent with the nature of the hypothesized bi-directional relationship between restriction and binge eating in eating disorder maintenance models (e.g., Fairburn, Cooper, & Shafran, 2003), restrictive eating behaviors may have dual functions, both precipitating the occurrence of binge eating episodes and compensating for their occurrence.
Prospective, momentary research is well-suited to examine the relationship between behaviors that occur within close proximity, including restrictive eating and binge eating. Ecological momentary assessment (EMA) is one such data collection strategy in which individuals monitor and report on experiences in their natural environment in real-time. Data collected via EMA have a number of benefits over data collected using more traditional methods of assessment, which include reduced error attributable to bias in retrospective recall and increased generalizability of findings to the natural environment (Wheeler & Reis, 1991). Recently, Zunker et al. (2011) reported results from an EMA study of restrictive eating behaviors and binge eating in women with bulimia nervosa, in which restrictive eating behaviors predicted binge eating both on the same day and on the subsequent day. Restrictive eating behaviors two days prior did not improve the prediction of binge eating, indicating that acute restrictive eating behaviors (≈24 hours or less) were specifically predictive of binge eating. These results support contemporary models of the maintenance of bulimic pathology (e.g., Fairburn, 2008; Fairburn et al., 2003).
In the present study, we aimed to examine the temporal nature of the relationships between restrictive eating behaviors and binge eating in individuals with anorexia nervosa (AN) using data collected via EMA. No studies to our knowledge have examined this relationship in AN, which is characterized by restrictive eating behaviors associated with chronic caloric intake that is below energy needs (American Psychiatric Association, 2013). Although recent evidence suggests that restrictive eating behaviors and binge eating episodes do not appear to be significantly associated when examined as summed frequencies over a two-week period in AN (De Young et al., 2013), the extent to which there may be bidirectional relationships between these behaviors, including possible cumulative effects of repeated restrictive eating behaviors, remains unclear. Consistent with treatment models that target binge eating and the findings of Zunker et al. (2011), we hypothesized that restrictive eating would function in a compensatory fashion, such that the presence of binge eating on a given day (controlling for the presence of restrictive eating that day) would predict restrictive eating behavior on the subsequent day. Second, consistent with evidence suggesting that restrictive eating may potentiate the risk of binge eating, we hypothesized that restrictive eating on a given day (controlling for the presence of binge eating that day) would predict binge eating the subsequent day. In addition, we conducted an exploratory analysis to examine the cumulative effect of restrictive eating over multiple days on the risk of binge eating, which would be consistent with the chronic caloric deprivation characterizing AN.
Method
Participants
A total of 118 women who were at least 18 years old with full (n = 59) or sub-threshold (n = 59) AN participated in this study. Individuals with full AN met all DSM-IV (American Psychiatric Association, 1994) criteria; individuals with sub-threshold AN met all DSM-IV criteria except one of the following: (1) body mass index (BMI) of 17.6–18.5 kg/m2, (2) no amenorrhea, or (3) no body image disturbance and intense fear of fatness. Research generally supports the clinical significance of an AN syndrome that presents without fear of fatness (Becker, Thomas, & Pike, 2009; Wildes, Forbush, & Markon, 2013). Only three of the 118 individuals in this sample met criteria for sub-threshold AN in this way. A study examining differences between the full and sub-threshold AN samples noted no difference across measures of anxiety, depression, personality, eating pathology, or comorbid psychopathology. The only differences were more frequent binge eating and purging in the full-threshold and more frequent checking of the thighs and joints in the sub-threshold sample when assessed via EMA (Le Grange et al., 2013). Participants were recruited through referrals from treatment providers and advertisements in the community, treatment centers, and college campuses in three locations in the Midwestern U.S. (Fargo, Minneapolis, and Chicago). Demographics can be found in Table 1.
Table 1.
Participant demographics.
| M | SD | Range | |
|---|---|---|---|
| Age (years) | 25.4 | 8.4 | 18–58 |
| BMI (kg/m2) | 17.2 | 1.0 | 13.4–18.5 |
| EDE Global | 2.75 | 1.29 | 0.13–5.31 |
| n | % | |
|---|---|---|
| Ethnicity (White) | 114 | 96.6 |
| Marital status (single/never married) | 89 | 75.4 |
| Education (college degree) | 40 | 33.9 |
Note: BMI = body mass index; EDE = Eating Disorder Examination interview.
Measures
Baseline interviews
AN diagnosis was established using the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P; First, Spitzer, Gibbon, & Williams, 1995). An independent assessor rated a random sample of 30 of these audiotaped interviews to gauge the reliability of the AN diagnosis (i.e., full versus subthreshold), which yielded a kappa coefficient of .929.
The Eating Disorder Examination (EDE; Fairburn & Cooper, 1993) is a semi-structured interview used to asses eating psychopathology. It includes a global score and four subscales (restraint, eating concern, shape concern, and weight concern) and assesses the frequency of several ED behaviors including binge eating and purging for the 3 months prior to the interview. An independent assessor rated a random sample of 31 audiotaped interviews for reliability, which yielded intraclass correlation coefficients ranging from .894 to .997 for the subscale scores.
EMA measures
Participants reported the occurrence of a number of eating behaviors over the course of the day using palmtop computers as described below. Included among these behaviors were binge eating episodes, compensatory behaviors (e.g., self-induced vomiting), and restrictive eating behaviors (e.g., skipping a meal; limiting calories, carbohydrates, or fat grams; and eating as little as possible). At the end of each day, participants also reported whether they had gone for 8 or more waking hours without eating and whether they limited their total caloric intake that day to fewer than 1200 kilocalories.
Skipping meals and fasting, defined as going at least 8 consecutive waking hours without eating, indicate dietary restriction for the purposes of the present study because they are the most objective and discrete of the available restrictive eating behaviors and are behavioral measures rather than cognitive variables, the latter of which may be more indicative of dietary restraint than restriction. Skipping a meal and going at least 8 waking hours without eating are clear markers of restriction (i.e., eating less than what is required for energy balance), especially as measured momentarily.
Procedure
Individuals first completed a telephone screen to determine eligibility. Eligible individuals attended an informational meeting about the study during which they provided written informed consent. Baseline assessments (semi-structured interviews and self-report questionnaires) took place over two visits at which participants were also screened for medical stability. At the first visit, research assistants instructed participants on the use of the palmtop computers for EMA recordings. Participants then practiced making ratings over the next two days before returning for the second assessment visit at which time they received feedback regarding their compliance with EMA recordings and received further instruction, if necessary. Participants then began the two week EMA protocol. Participants were compensated with $100 per EMA week and received a $50 bonus if they responded to at least 80% of random signals.
Participants made three types of EMA recordings: signal contingent, interval contingent, and event contingent (Wheeler & Reis, 1991). Alerts from the palmtop computers occurred within 20 minutes of six times spread throughout the waking hours of the day (8:30 a.m., 11:10 a.m., 1:50 p.m., 4:30 p.m., 7:10 p.m., and 9:50 p.m.) and prompted participants to make signal contingent recordings. Participants initiated interval contingent recordings at the end of each day, and initiated event contingent recordings immediately following the occurrence of specific pre-identified behaviors including binge eating, self-induced vomiting, and certain restrictive eating behaviors. Participants could also record the occurrence of such behaviors at signal-contingent recordings, if they had been unable or had forgotten to initiate an event contingent recording. The Institutional Review Boards at all three data collection sites approved this protocol.
Statistical analyses
Time-lagged general estimating equations (GEE; Liang & Zeger, 1986) with a binary logit link function tested (a) whether binge eating predicted restrictive eating the following day while controlling for restrictive eating the previous day, (b) whether restrictive eating predicted binge eating the following day while controlling for binge eating the previous day, and (c) whether restricting predicted binge eating later the same day. Controlling for the previous day dependent variable (e.g., restricting) was necessary because it is possible that this behavior influences the likelihood of the independent variable on the previous day (e.g., binge eating) which could then confound the prediction of the dependent variable on the next day (e.g., restricting). Thus, without controlling for the previous day dependent variable, it may appear as though the independent variable predicts the dependent variable when the relationship is better accounted for by the dependent variable predicting the dependent variable the next day.
In addition, an interaction term (independent variable × previous day dependent variable) separated the main effects of each behavior from potentially moderating effects of the behaviors on one another that may be present when both behaviors occur on the same day. This term tested for the possibility that previous day behavior predicts next day behavior only in the context of ongoing behavior (e.g., restrictive behavior predicting next day binge eating only when individuals binge ate the day before). The presence of such an interaction would indicate that the ability of the independent variable to predict the next day dependent variable depends upon the presence of the dependent variable the same day.
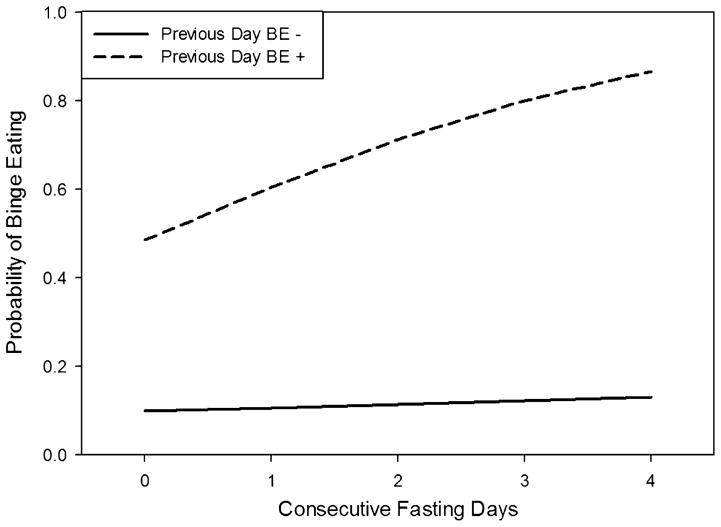
The cumulative effect of restrictive eating on the likelihood of binge eating was examined by calculating a running total of consecutive days that individuals reported going at least 8 consecutive waking hours without eating (i.e., fasting). For example, if an individual engaged in fasting on the first day of data collection, her value for this variable would be “1.” If she did so again the next day, her value would be “2.” If individuals experienced a day during which they did not fast, their running total returned to zero. This running total was used to predict binge eating on the following day while controlling for binge eating the previous day, and included the interaction of cumulative fasting days and previous day binge eating. AN subtype was added as a covariate in all analyses due to research indicating that individuals classified as having the binge-eating/purging subtype of AN endorse higher rates of both binge eating and restrictive eating behaviors (De Young et al., 2013).
Finally, due to heterogeneity in the reported occurrence of binge eating and restrictive eating behaviors in the sample, the analyses were re-run while excluding participants who did not report an instance of the independent variable in order to determine whether this heterogeneity impacted the findings. For instance, participants who never reported an instance of binge eating during the study period were excluded in the first analysis in which binge eating was used to predict next day restrictive eating. All analyses were conducted using SPSS Version 21.
Results
Binge eating predicting restriction
The mean (SD) number of binge eating episodes per day among individuals with the binge eating/purging type of AN was 0.35 (0.45), and it was 0.05 (0.13) among individuals with the restricting type. To test the hypothesis that binge eating leads to compensatory restrictive eating, binge eating was used as an independent variable to predict next day fasting. Results revealed that the presence of binge eating predicted the occurrence of fasting the following day (Wald X2(1) = 4.13, p = .042). However, after including fasting the previous day and AN subtype as covariates, binge eating was neither a significant predictor of next day fasting, nor was the interaction term of binge eating and previous day fasting significant, suggesting that fasting did not function in a compensatory fashion in response to binge eating (Table 2). Excluding participants who never reported binge eating (n = 68) did not alter these findings.
Table 2.
Generalized estimating equation results involving binge eating and fasting (N = 118).
| Parameter | Predicting fasting
|
Predicting binge eating
|
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Wald X2 (1) | p | OR (95% CI) | Wald X2 (1) | p | |
| Intercept | 0.08 (0.05, 0.13) | 100.59 | <.001 | 0.18 (0.12,0.26) | 85.01 | <.001 |
| Lag binge eating | 1.20 (0.62, 2.33) | 0.28 | .595 | 5.48 (3.13,9.59) | 35.58 | <.001 |
| Lag fasting | 10.98 (5.83,20.66) | 55.12 | <.001 | 0.79 (0.34,1.83) | 0.30 | .584 |
| Lag binge eating × lag fasting | 1.59 (0.52, 4.86) | 0.67 | .415 | 2.80 (0.92,8.50) | 3.29 | .070 |
| AN subtype | 1.67 (1.02, 2.83) | 3.57 | .059 | 3.99 (2.30,6.90) | 24.45 | <.001 |
Note: AN subtype coded 0 for restricting type and 1 for binge eating/purging type; significance evaluated at a p-value of .05, represented by bold type; OR = odds ratio; CI = confidence interval.
Next, the association between binge eating and subsequent meal skipping was examined. The occurrence of binge eating did not predict skipping meals the next day (Wald X2(1) = 2.07, p = .151). This remained the case after AN subtype, previous day meal skipping, and same day fasting were entered as covariates. The interaction term of binge eating and previous day meal skipping was also not a significant predictor of next day meal skipping (Table 3). Fasting was included as a covariate because skipping meals and fasting were significantly associated with one another (Wald X2(1) = 20.53, p < .001), which is logically consistent with the likelihood of skipping meals in order to fast for at least 8 consecutive waking hours. Thus, controlling for fasting ensured that any relationship between skipping meals and binge eating would not be better accounted for by a relationship between binge eating and fasting. Excluding participants who never reported binge eating (n = 68) did not alter these findings.
Table 3.
Generalized estimating equation results involving binge eating and meal skipping (N = 118).
| Parameter | Predicting meal skipping
|
Predicting binge eating
|
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Wald X2 (1) | p | OR (95% CI) | Wald X2 (1) | p | |
| Intercept | 0.18 (0.14, 0.23) | 174.38 | <.001 | 0.80 (0.05, 0.12) | 145.65 | <.001 |
| Lag binge eating | 1.33 (0.73, 2.44) | 0.86 | .354 | 7.78 (3.91,15.46) | 34.26 | <.001 |
| Lag meal skipping | 8.01 (5.29,12.15) | 96.42 | <.001 | |||
| Lag binge eating × lag meal skipping | 1.00 (0.40, 2.52) | 0.000005 | .994 | |||
| AN subtype | 1.34 (0.90, 1.98) | 2.12 | .146 | 4.15 (2.47, 6.98) | 28.94 | <.001 |
| Same day meal skipping | 0.58 (0.32, 1.04) | 3.33 | .068 | |||
| Same day fasting | 3.33 (1.92, 5.80) | 18.15 | <.001 | 1.84 (0.91, 3.71) | 2.92 | .087 |
| Lag binge eating × same day meal skipping | 0.58 (0.25, 1.35) | 1.60 | .206 | |||
Note: AN subtype coded 0 for restricting type and 1 for binge eating/purging type; significance evaluated at a p-value of .05, represented by bold type; OR = odds ratio; CI = confidence interval.
Restriction predicting binge eating
To test the hypothesis that restrictive eating potentiates the risk of binge eating, fasting was used as an independent variable to predict next day binge eating. Fasting did not predict the occurrence of binge eating the following day (Wald X2(1) = 2.15, p = .143), and fasting remained a nonsignificant predictor after controlling for AN subtype and binge eating the day before. The interaction term of fasting and previous day binge eating was also not a significant predictor of next day binge eating (Table 2), although it was in the direction of indicating that fasting increased the risk of binge eating the next day among individuals who engaged in binge eating the previous day. Excluding participants who never fasted (n = 70) did not alter these findings.
With regard to meal skipping predicting binge eating, fasting was included as a covariate for the same reasons described above. Fasting emerged as a significant predictor of same day binge eating (Wald X2(1) = 4.43, p = .035) such that engaging in fasting was associated with a higher likelihood of engaging in binge eating; however, meal skipping was not predictive of binge eating later that same day (Wald X2(1) = 2.05, p = .152). After subtype was included as a covariate (Wald X2(1) = 34.35, p < .001), meal skipping emerged as a significant negative predictor of binge eating later the same day (Wald X2(1) = 4.70, p = .030), and same day fasting became non-significant (Wald X2(1) = 2.443, p = .118). The addition of the interaction term of meal skipping and previous day binge eating was not a significant predictor of later binge eating (Table 3). Excluding participants who never skipped a meal (n = 26) did not alter these findings.
Cumulative effects of restriction on risk of binge eating
Finally, an exploratory analysis was conducted to evaluate the cumulative effect of restricting on the risk of binge eating, as indicated by consecutive days during which individuals reported going at least 8 waking hours without eating. There was a significant interaction of consecutive days of fasting and previous day binge eating (Wald X2(1) = 4.34, p = .037; Fig. 1) that remained (Wald X2(1) = 4.01, p = .045) after controlling for AN subtype (Wald X2(1) = 23.54, p < .001). The likelihood of binge eating increased as the number of consecutive days of fasting increased for individuals who engaged in binge eating the previous day, but not for individuals who did not engage in binge eating the previous day. Thus, it appears that the risk of next day binge eating was potentiated not simply by repeatedly engaging in fasting but by doing so in the context of having recently engaged in binge eating. Importantly, previous day binge eating did not appear to be a proxy for the tendency to engage in binge eating in general, as the same analysis using average frequency of binge eating over the 2-week protocol in place of previous day binge eating did not replicate the interaction effect (Wald X2(1) = 1.16, p = .281). Thus, the relationship between the cumulative effect of fasting and binge eating appears to be particular to previous day binge eating and not binge eating in general. Excluding participants who never fasted (n = 70) did not alter these findings.
Fig. 1.
Depicts the interaction between consecutive fasting days and the likelihood of a subsequent binge eating episode.
Discussion
The purpose of this study was to test two hypothesized temporal relationships between restrictive eating and binge eating. The first, that binge eating would increase the likelihood of restrictive eating (presumably in a compensatory fashion), was tested by predicting next day fasting and meal skipping using previous day binge eating. In neither case was binge eating a significant predictor after controlling for covariates (i.e., previous day dependent variables and AN subtype). The second hypothesis, that restrictive eating would increase the likelihood of binge eating, was tested by (a) predicting next day binge eating with previous day fasting and (b) predicting binge eating later in the day with meal skipping earlier in the day. Again, the hypotheses were not directly supported; however, meal skipping was a negative predictor of binge eating. Finally, the exploratory analysis revealed that fasting for consecutive days increased the odds of next day binge eating among individuals who engaged in binge eating the previous day.
At the bivariate level, fasting predicted same day binge eating, which replicated findings from an EMA study in bulimia nervosa (Zunker et al., 2011). This was not used to test the hypothesis about the temporal prediction of restrictive eating and binge eating in the present study because fasting was assessed only at the end of the day. Thus, it is unknown in what order same-day binge eating and fasting occurred. Also at the bivariate level, binge eating predicted next day fasting, which is consistent with theoretical models (e.g., cognitive behavior therapy) and nosologies (e.g., DSM-5) that include fasting as a possible inappropriate compensatory behavior. However, both of these bivariate relationships were accounted for by AN subtype.
Two other findings deserve further elaboration. It may seem counterintuitive that skipping meals was a negative predictor of binge eating. Further, this relationship only emerged after controlling for fasting and AN subtype. Thus, although the binge eating/purging subtype engaged in both meal skipping and binge eating more often than the restricting type, and fasting and skipping meals were strongly positively associated with one another, skipping meals was found to uniquely reduce the likelihood of binge eating later the same day. It is possible that this highlights the “good day/bad day” dichotomous thinking observed in this population (Byrne, Allen, Dove, Watt, & Nathan, 2008), such that when one skips meals, she is encouraged by her successful restriction and bolstered against binge eating later that day. It is also possible that skipping meals coincides with other eating behaviors (e.g., increased snacking) that may reduce the likelihood of binge eating. Another possibility is that meals themselves serve as triggers for binge eating in this population, such that skipping meals reduces one’s exposure to binge eating triggers. This last possibility is particularly troubling as it would highlight the pernicious nature of these behaviors in AN. These findings, together with those from Zunker et al. (2011), are consistent with the laboratory findings of Hetherington, Stoner, Andersen, and Rolls (2000) who found that 19 hours of food deprivation (i.e., an overnight fast combined with skipping breakfast and lunch the following day) increased consumption at a dinner meal in individuals with bulimia nervosa but not in individuals with binge eating/purging AN. They concluded that “short-term food deprivation may have a relatively weak influence on eating behavior in the eating disorders, compared to cumulative and chronic periods of caloric restriction” (p. 282). Future research should aim to replicate this finding and further identify and explain the mechanism responsible for this relationship.
The second notable finding was that there appears to be a cumulative effect of repeatedly fasting on the risk of binge eating, but only among individuals who engaged in binge eating the previous day. If individuals were not actively engaged in binge eating, repeatedly fasting did not increase their likelihood of binge eating. This finding may be evidence of a transient binge eating-fasting cycle that may occur intermittently. Additional evidence supporting this possibility comes from the lack of such a relationship when substituting average frequency of binge eating for previous day binge eating. This indicates that the observed relationship between the cumulative effects of fasting and risk of binge eating is not dependent upon a person-level variable (e.g., AN subtype or one’s propensity to binge eat) but rather upon the recent occurrence of specific behavior (i.e., a binge eating episode). Additional research will be needed to replicate this finding and should examine this relationship in individuals who are of normal body weight or overweight status and to investigate whether physiological changes induced by short-term weight loss result in compensatory binge eating.
There are several potential clinical implications of the current findings. For instance, it appears important to conceptualize restrictive eating as occurring in relation to binge eating as well as independent of that behavior, even among individuals who tend to binge eat. Many episodes of restrictive eating may occur independently of a binge eating episode, and may in fact not influence the likelihood of binge eating. At the same time, among individuals who have recently engaged in binge eating, fasting appears to increase their risk of future binge eating. Thus, using momentary interventions (e.g., ecological momentary interventions; Heron & Smyth, 2010) to intervene during a binge eating/fasting/binge eating cycle may be a fruitful direction for future research. Unexpectedly, skipping meals appears to reduce the likelihood of binge eating, perhaps by limiting exposure to food- or eating-related triggers for binge eating, as discussed above. It is possible that this relationship is not dissimilar from weight loss study findings in which dietary restriction leads to reductions in the frequency of binge eating episodes (e.g., Goodrick et al., 1998; Presnell & Stice, 2003; Stice et al., 2005) and findings in individuals with BN dieting for weight loss who report less frequent binge eating than their counterparts who are not dieting (Lowe, Witt, & Grossman, 2013). Although weight loss interventions do not typically advise skipping meals, individuals participating in these interventions are likely eating foods that they are less likely to incorporate into a binge eating episode (e.g., salad versus a hamburger). However, when restricting, one must eventually approach food of some kind, and doing so in a fasted state when binge eating has recently occurred appears to put one at greater risk of it occurring again. Thus, eating regular meals that do not include foods that tend to trigger binge eating may be the strategy most likely to decrease the likelihood of binge eating.
This is the first investigation of the temporal relationships between restrictive eating and binge eating in AN. Of particular note is the use of EMA in the present study, which is a particularly strong methodology for measuring the relationship between behavioral variables assessed in the natural environment. In addition, the sample size is large for studies of this type and in this population, and appropriate statistical controls were used to mitigate spurious findings and certain alternative interpretations. Nevertheless, the findings should be interpreted in light of limitations. First, it is unknown whether participants reported all instances of binge eating, fasting, and meal skipping. If participants did not initiate a report (i.e., an event-contingent recording) after they engaged in binge eating or meal skipping, they had the opportunity to report that these behaviors occurred at the next signal-contingent recording. Even so, some participants may have neglected to report all such behaviors. In addition, the only recording at which to report fasting was the interval-contingent recording at the end of the day. Thus, if participants did not complete this recording for a particular day, it is unknown whether they fasted. Second, it is possible that the nature of binge eating, especially as self-reported, may differ across populations (e.g., bulimia nervosa, overweight, etc.). The extent to which self-reported binge eating in this study reflected the diagnostic criteria as defined for bulimia nervosa and binge eating disorder (American Psychiatric Association, 2013) is unclear and may have included a number of episodes that would be classified as “subjective” by clinical rating (Fairburn, 2008). Similarly, the degree to which self-reported dietary restriction was accurate is unknown, although the use of behavioral indicators may have increased the reliability of this variable. Nonetheless, given the limitations of self-report even in the context of EMA, measurement error may have impacted study results. Future research should aim to clarify the affective, physiological, and environmental determinants of binge eating and the various forms of dietary restriction, noting how each may influence the other and within what period of time, to build complete and accurate maintenance models of these behaviors in AN. For instance, short-term dietary restriction (e.g., meal skipping) may reduce short-term (i.e., same day) risk of binge eating through an avoidance of binge eating cues while leading to longer-term restriction (e.g., fasting), which may increase the risk of binge eating through greater hunger and negative affect. The use of EMA to test these hypothesized relationships between eating disorder behaviors provides the most precise level of analysis to improve our understanding of these problems and our ability to effectively intervene.
Footnotes
Acknowledgments:Funding provided by the National Institute of Mental Health (2 R01-MH-059674-04A2). Principal Investigator: Stephen A. Wonderlich, Ph.D.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Becker AE, Thomas JJ, Pike KM. Should non-fat-phobic anorexia nervosa be included in DSM-V? International Journal of Eating Disorders. 2009;42:620–635. doi: 10.1002/eat.20727. [DOI] [PubMed] [Google Scholar]
- Byrne SM, Allen KL, Dove ER, Watt FJ, Nathan PR. The reliability and validity of the dichotomous thinking in eating disorders scale. Eating Behaviors. 2008;9:154–162. doi: 10.1016/j.eatbeh.2007.07.002. [DOI] [PubMed] [Google Scholar]
- De Young KP, Lavender JM, Steffen K, Wonderlich SA, Engel SG, et al. Restrictive eating behaviors are a nonweight-based marker of severity in anorexia nervosa. International Journal of Eating Disorders. 2013;46:849–854. doi: 10.1002/eat.22163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive behavior therapy and eating disorders. New York: Guilford Press; 2008. [Google Scholar]
- Fairburn CG, Cooper Z. The eating disorders examination. In: Fairburn CG, Wilson GT, editors. Binge eating. Nature, assessment and treatment. 12. New York: Guilford Press; 1993. pp. 317–331. [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders. A “transdiagnostic” theory and treatment. Behaviour Research and Therapy. 2003;41:509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV axis I disorders. New York: Biometrics; 1995. Patient edition (SCIDI/P) [Google Scholar]
- Gil-Campos M, Aguilera CM, Cañete R, Gil A. Ghrelin. A hormone regulating food intake and energy homeostasis. The British Journal of Nutrition. 2006;96:201–226. doi: 10.1079/bjn20061787. [DOI] [PubMed] [Google Scholar]
- Goodrick GK, Poston WS, Kimball KT, Reeves RS, Foreyt JP. Nondieting versus dieting treatment for overweight binge-eating women. Journal of Consulting and Clinical Psychology. 1998;66:363–368. doi: 10.1037//0022-006x.66.2.363. [DOI] [PubMed] [Google Scholar]
- Herman CP, Mack D. Restrained and unrestrained eating. Journal of Personality. 1975;43:647–660. doi: 10.1111/j.1467-6494.1975.tb00727.x. [DOI] [PubMed] [Google Scholar]
- Heron KE, Smyth JM. Ecological momentary interventions. Incorporating mobile technology into psychosocial and health behavior treatments. British Journal of Health Psychology. 2010;15:1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetherington MM, Stoner SA, Andersen AE, Rolls BJ. Effects of acute food deprivation on eating behavior in eating disorders. International Journal of Eating Disorders. 2000;28:272–283. doi: 10.1002/1098-108x(200011)28:3<272::aid-eat4>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Johnson F, Pratt M, Wardle J. Dietary restraint and self-regulation in eating behavior. International Journal of Obesity. 2012;36:665–674. doi: 10.1038/ijo.2011.156. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Crosby RD, Engel SG, Cao L, Ndungu A, Crow SJ, et al. DSM-IV defined anorexia nervosa versus subthreshold anorexia nervosa (EDNOS-AN) European Eating Disorders Review. 2013;21:1–7. doi: 10.1002/erv.2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Lowe MR. Self-regulation of energy intake in the prevention and treatment of obesity. Is it feasible? Obesity Research. 2003;11:44S–59S. doi: 10.1038/oby.2003.223. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Witt AA, Grossman SL. Dieting in bulimia nervosa in associated with increased food restriction and psychopathology but decreased binge eating. Eating Behaviors. 2013;14:342–347. doi: 10.1016/j.eatbeh.2013.06.011. [DOI] [PubMed] [Google Scholar]
- Mathes WF, Brownley KA, Mo X, Bulik CM. The biology of binge eating. Appetite. 2009;52:545–553. doi: 10.1016/j.appet.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presnell K, Stice E. An experimental test of the effect of weight-loss dieting on bulimic pathology. Tipping the scales in a different direction. Journal of Abnormal Psychology. 2003;112:166–170. [PubMed] [Google Scholar]
- Stice E, Fisher M, Lowe MR. Are dietary restraint scales valid measures of acute dietary restriction? Unobtrusive observational data suggest not. Psychological Assessment. 2004;16:51–59. doi: 10.1037/1040-3590.16.1.51. [DOI] [PubMed] [Google Scholar]
- Stice E, Killen JD, Hayward C, Taylor CB. Age of onset for binge eating and purging during late adolescence. A 4-year survival analysis. Journal of Abnormal Psychology. 1998;107:671–675. doi: 10.1037//0021-843x.107.4.671. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Groesz L, Shaw H. Effects of a weight maintenance diet on bulimic symptoms in adolescent girls. An experimental test of the dietary restraint theory. Health Psychology. 2005;24:402–412. doi: 10.1037/0278-6133.24.4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Shaw H. Relation of dieting to eating pathology. The dance of sleeping and eating among adolescents. In: Latzer Y, Tzischinsky O, editors. Normal and Pathological perspectives. Hauppauge, NY: Nova Biomedical Books; 2012. pp. 27–38. [Google Scholar]
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls. A 2-year prospective investigation. Health Psychology. 2002;21:131–138. [PubMed] [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events. Origins, types, and uses. Journal of Personality. 1991;59:339–354. [Google Scholar]
- Wildes JE, Forbush KT, Markon KE. Characteristics and stability of empirically derived anorexia nervosa subtypes. Towards the identification of homogeneous low-weight eating disorder phenotypes. Journal of Abnormal Psychology. 2013;122:1031–1041. doi: 10.1037/a0034676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunker C, Peterson CB, Crosby RD, Cao L, Engel SG, Mitchell JE, et al. Ecological momentary assessment of bulimia nervosa. Does dietary restriction predict binge eating. Behaviour Research and Therapy. 2011;49:714–717. doi: 10.1016/j.brat.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]