Abstract
BACKGROUND/OBJECTIVES
Although preclinical studies suggest that garlic has potential preventive effects on cardiovascular disease (CVD) risk factors, clinical trials and reports from systematic reviews or meta-analyses present inconsistent results. The contradiction might be attributed to variations in the manufacturing process that can markedly influence the composition of garlic products. To investigate this issue further, we performed a meta-analysis of the effects of garlic powder on CVD risk factors.
MATERIALS/METHODS
We searched PubMed, Cochrane, Science Direct and EMBASE through May 2014. A random-effects meta-analysis was performed on 22 trials reporting total cholesterol (TC), 17 trials reporting LDL cholesterol (LDL-C), 18 trials reporting HDL cholesterol (HDL-C), 4 trials reporting fasting blood glucose (FBG), 9 trials reporting systolic blood pressure (SBP) and 10 trials reporting diastolic blood pressure (DBP).
RESULTS
The overall garlic powder intake significantly reduced blood TC and LDL-C by -0.41 mmol/L (95% confidence interval [CI], -0.69, -0.12) (-15.83 mg/dL [95% CI, -26.64, -4.63]) and -0.21 mmol/L (95% CI, -0.40, -0.03) (-8.11 mg/dL [95% CI, -15.44, -1.16]), respectively. The mean difference in the reduction of FBG levels was -0.96 mmol/L (95% CI, -1.91, -0.01) (-17.30 mg/dL [95% CI, -34.41, -0.18]). Evidence for SBP and DBP reduction in the garlic supplementation group was also demonstrated by decreases of -4.34 mmHg (95% CI, -8.38, -0.29) and -2.36 mmHg (95% CI, -4.56, -0.15), respectively.
CONCLUSIONS
This meta-analysis provides consistent evidence that garlic powder intake reduces the CVD risk factors of TC, LDL-C, FBG and BP.
Keywords: Allium sativum, garlic, CVD risk factor, meta-analysis, systematic review
INTRODUCTION
Cardiovascular disease (CVD) is a prominent global public health problem. The etiology of CVD is multifactorial and exemplified by hypercholesterolemia, hypertension and diabetes mellitus (DM). Various major CVD risk factors cannot be controlled, including age, gender and family history. However, CVD is predominantly caused by risk factors that can be controlled, treated or modified, such as cholesterol, high blood pressure (BP) and diabetes [1,2].
Allium sativum, commonly known as garlic, is a plant of the family Alliaceae and is widely consumed as a spice in Korea. Garlic contains high levels of organosulfur compounds and flavonoids as well as a variety of compounds that function synergistically to provide various health benefits [3]. The body of evidence on garlic continues to grow, and numerous clinical trials have been published [4,5,6,7]. Animal studies suggest that garlic has potential antilipidemic, antihypertensive, antiglycemic, antithrombotic and antiatherogenic properties [8,9,10]. However, clinical trials and reports from systematic reviews or meta-analyses present inconsistent results despite preclinical studies that suggest that garlic has potential preventive effects on CVD risk factors [4,5,6,7,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37]. The contradiction may be attributed to variations the manufacturing process that can markedly influence the composition of garlic products. As a dietary supplement, garlic is available as dehydrated garlic powder, aged garlic extract (AGE), garlic oil (steam-distilled), garlic essential oil (etherextracted) and garlic oil macerate, and each form contains a markedly different set of compounds [38]. Among these garlic products, dehydrated preparations are most commonly used and reportedly contain most of the constituents found naturally in whole garlic. According to a recent meta-analysis of randomized controlled clinical trials, garlic powder appeared to be more effective for reducing LDL cholesterol (LDL-C) in their subgroup analysis of garlic preparation types [4].
In the present study, we systemically reviewed randomized clinical trials (RCTs) to assess the effects of a garlic powder or dehydrated garlic preparation on CVD biomarkers. Specifically, we examined the effects of these preparations on the classic modifiable Framingham risk measures, including systolic BP (SBP), diastolic BP (DBP), total cholesterol (TC) and LDL-C and HDL cholesterol (HDL-C) [39,40]. Additionally, given the reciprocal relationship between insulin resistance and cardiovascular risk [41], we also examined fasting blood glucose (FBG) levels. The effect of other potential confounders, such as the duration of treatment, intake level, subject type and location where the study was performed, were explored in the subgroup analyses.
MATERIALS AND METHODS
Search strategy
The study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA checklist) [42]. In this analysis, RCTs that included clinical outcomes related to CVD risk factors, such as blood cholesterol, glucose levels and BPs, were eligible. Only garlic powder intake studies were included in this analysis. Databases, such as PubMed, Cochrane, Science Direct and EMBASE, were searched for studies that were published from January 1995 to May 2014 and examined the effects of garlic powder on cholesterol, blood glucose or BP compared with placebo or positive control. The search terms used were Allium sativum and garlic in combination with cardiovascular-related factors, such as cholesterol, blood glucose, BP and blood circulation. The search was limited to human studies published in English, Japanese and Korean. No studies published in Korean or Japanese were identified. A manual search using the reference lists of original articles and recent reviews was also performed. Each publication was independently reviewed, and the relevant information was extracted by two authors (JSK and JYK).
Data extraction and quality assessment
Data were extracted, and quality was assessed independently by two investigators (JSK and JYK) on the basis of the quality assessment tool used for our previous systematic review and the Cochrane Collaboration [43,44]. This quality rating was based on several criteria related to study design (e.g., use of placebo control versus a non-placebo control group), data collection (e.g., the method of dietary assessment), the quality of the statistical analysis, the type of outcome measured and the characteristics of the study populations (e.g., whether selection bias was present or whether important information about the study subjects, such as age and smoking status, was gathered and reported). We assigned a score from -1 to 1 point for each quality item to yield a score ranging from -20 to 11 for a completely valid study. If the scientific study adequately addressed all or most of the criteria, it received a high methodological quality rating. The risk of bias for this analysis was assessed based on the risk of bias assessment tool for RCTs provided by the Cochrane Collaboration [43]. The risk of bias domains, such as selection bias (random sequence generation and allocation concealment), performance/detection bias (blinding of participants and personnel/blinding of outcome assessment), attrition bias (incomplete data outcome) and reporting bias (selective reporting), were identified [43].
Statistical analysis
The mean changes in biomarkers from baseline were treated as continuous variables, and the mean difference was calculated as the difference between the means in the garlic powder and the control material supplementation groups. The mean changes were calculated using the methods described in the Cochrane Handbook [43]. Briefly, the mean of the differences was equal to the difference in the means. If information was not available from the study on the standard deviations (SD) of the differences, imputation of standard deviations could be achieved by assuming a particular correlation coefficient. Forest plots were produced to visually assess the changes for each variable and the corresponding 95% confidence intervals (CIs) across the studies. A random-effect model was used to calculate the combined effect size to provide a more conservative estimation. Heterogeneity among the studies was assessed using the I2 statistic, and considered low if I2 < 30%, moderate if I2 = 30-75%, and high if I2 > 75% [43]. Publication bias was assessed using funnel plots and Egger's regression. Additionally, subgroup analyses were performed to investigate the potential moderator, and the groups were classified according to dosage, duration, subject and location based on median values for continuous variables. To evaluate the influence of each study on the overall effect size, a sensitivity analysis was conducted using the study removal approach. The secondary analysis was limited to studies that demonstrated high compliance; high quality or a placebo-control design; were published recently; were conducted with dietary management or were supplemented with standardized garlic powder. Furthermore, the relationships between effect size and moderators, such as dose, duration, quality of study, baseline value of risk factor and subject number, were investigated using random effects meta-regression analyses. The statistical analyses were performed using Comprehensive Meta-analysis Version 2.2, Biostat (Englewood, NJ, USA), and a P-value of < 0.05 was considered statistically significant.
RESULTS
Literature search and study characteristics
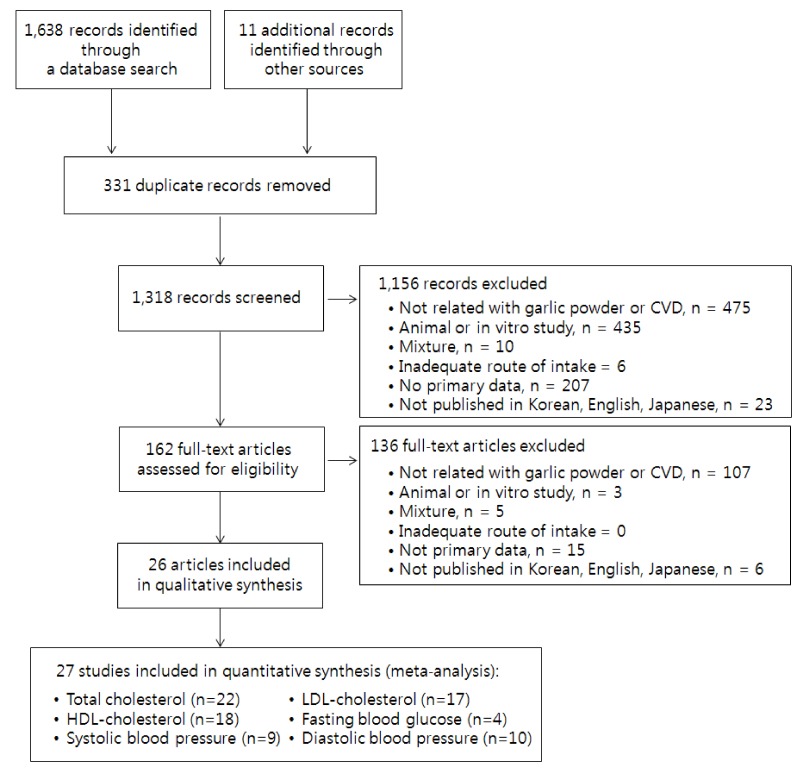
A total of 1,649 potentially relevant titles and abstracts were identified from searches on PubMed, Cochrane, Science Direct and EMBASE together with other reference sources. Of the 162 articles that were collected as full text and assessed for inclusion, 27 studies met the inclusion criteria for meta-analysis (Fig. 1). The characteristics of the 27 included RCTs and their quality are described in Table 1. Twenty-two trials reported sufficient data on TC, 17 trials reported LDL-C data, 18 trials reported HDL-C data, 4 trials reported FBG data, 9 trials reported SBP data and 10 trials reported DBP data (Fig. 1). The majority of trials employed a parallel study design (n = 26); however, 1 trial used a crossover design. Among the 27 identified studies, 14 [12,13,14,16,17,18,21,23,24,25,28,29,31,36] reported that the garlic powder used in each trial was standardized to contain 2.5-13 µg/mg allicin or 13 µg/mg alliin, whereas the remaining studies did not provide any information about standardization. The trials ranged from 7 days to one year in duration. The studies were generally from the United States or European countries; five studies were based in Asia, and one was conducted in Australia.
Fig. 1.
Flow diagram of the article selection process.
Table 1.
Details of trials included in this meta-analysis
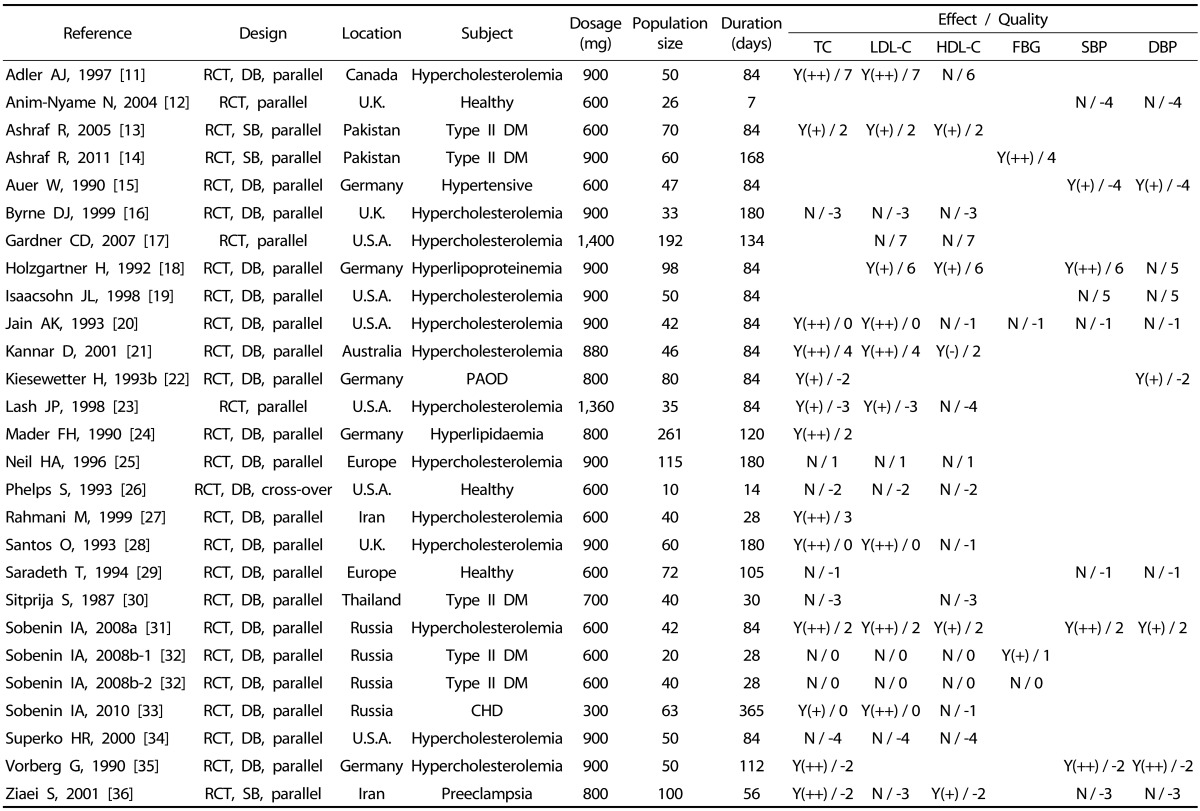
TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; FBG, fasting blood glucose; SBP, systolic blood pressure; DBP, diastolic blood pressure; RCT, randomized controlled trial; DB, double-blind; SB, single-blind; Y(++), significant improvement in the biomarker compared to control; Y(+), significant improvement in the biomarker compared to before the treatment; N, no significant improvement in the biomarker; DM, diabetes mellitus; PAOD, Peripheral arterial occlusive disease; CHD, coronary heart disease
The quality of the trials was generally adequate (score range: -4-7; median score: 0). (Table 1). Six trials reported adequate randomization [17,18,19,24,25,29], and all but six trials were double-blind, placebo-controlled trials [11,14,15,16,18,19,20,21,22,24,25,26,27,28,29,30,32,33,34,35]. Eight trials did not provide information on the dietary intervention [15,16,22,24,25,33,35,36]. Compliance was assessed and reported as high in 20 trials [11,12,13,14,17,18,19,21,22,24,25,27,28,29,30,32,33,34,35,36], and all trials applied adequate statistical analyses.
The effect of garlic powder on CVD risk factors
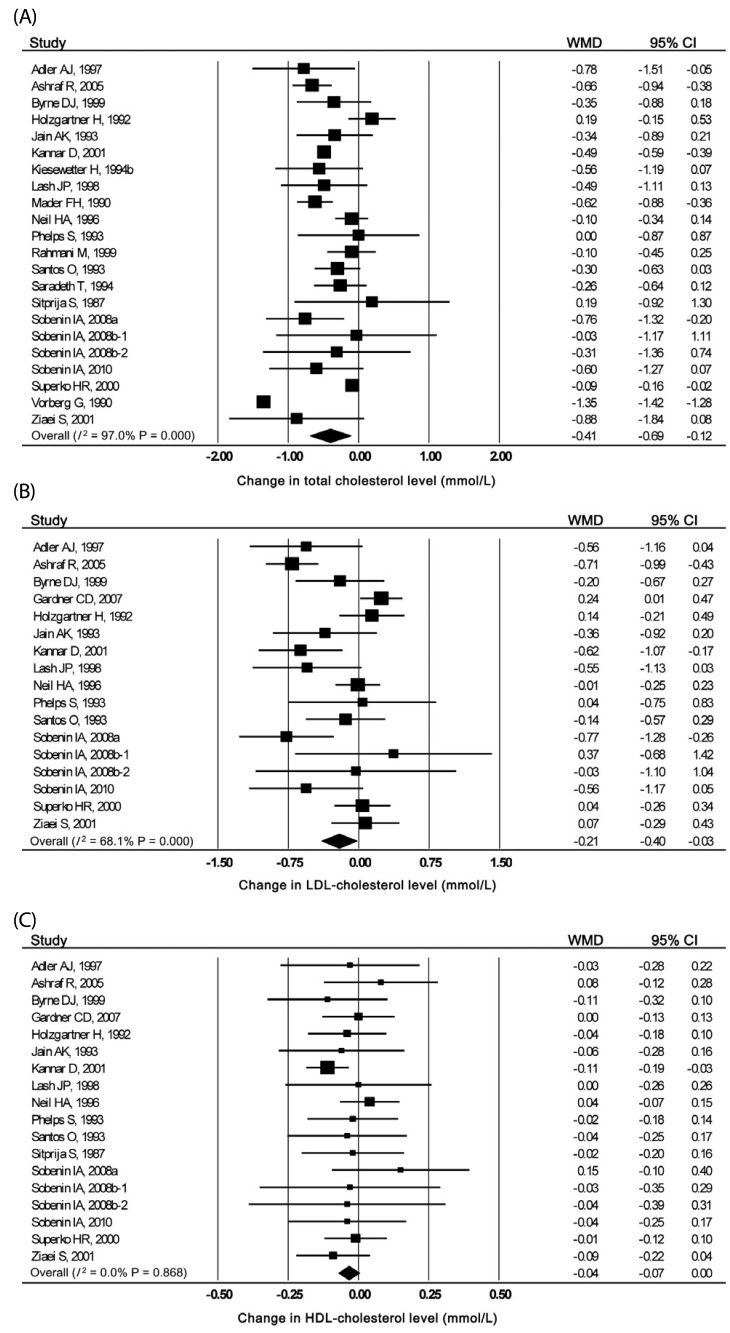
A total of 22 studies for TC (n = 1,442), 17 for LDL-C (n = 1,083) and 18 for HDL-C (n = 1,123) were reviewed for garlic powder (Table 1). The effects of garlic on the levels of TC, LDL-C and HDL-C are presented in Fig. 2. Overall, garlic powder intake significantly reduced blood TC and LDL-C by -0.41 mmol/L (95% CI, -0.69, -0.12, P = 0.005) (-15.83 mg/dL [95% CI, -26.64, -4.63]) and -0.21 mmol/L (95% CI, -0.40, -0.03, P = 0.024) (-8.11 mg/dL [95% CI, -15.44, -1.16]), respectively. Heterogeneity among the studies on TC or LDL-C levels was observed (I2 = 97.0 or 68.1%). However, the HDL-C level was not significantly modified by garlic supplementation (P = 0.057).
Fig. 2.
Forest plot results of the effect of garlic powder on cholesterol. (A) Total cholesterol, (B) LDL-cholesterol and (C) HDL-cholesterol; WMD, weighted mean difference
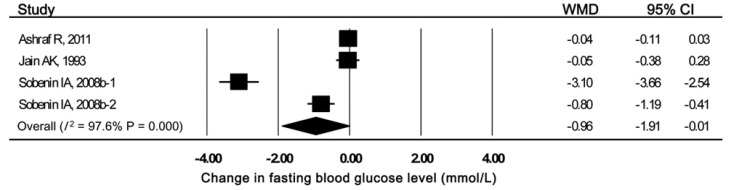
The mean difference in the reduction of FBG levels between the garlic powder-treated subjects and those receiving control substances was -0.96 mmol/L (95% CI, -1.91, -0.01) (-17.30 mg/dL [95% CI, -34.41, -0.18]) in 4 trials that included 162 subjects. This effect was significant (P = 0.047) with high heterogeneity (I2 = 97.6%, Fig. 3).
Fig. 3.
Forest plot results of the effect of garlic powder on fasting blood glucose; WMD, weighted mean difference
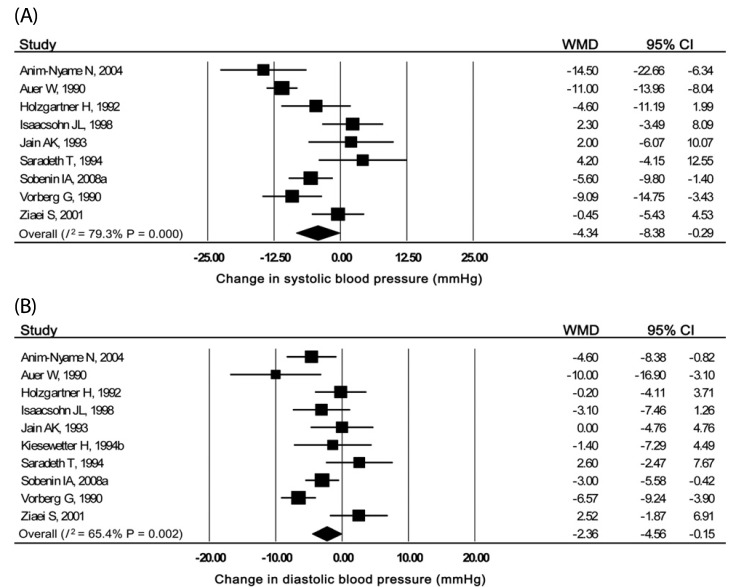
A total of nine (n = 470) or ten (n = 550) studies were appropriate for the meta-analysis evaluation on whether garlic powder intake reduced SBP or DBP (Table 1). SBP was reduced by -4.34 mmHg (95% CI, -8.38, -0.29, P = 0.036) with significant heterogeneity (I2 = 79.3%) in the garlic supplementation group compared with the control group (Fig. 4(A)). The overall pooled estimate of the effect of garlic powder on DBP was -2.36 mmHg (95% CI, -4.56, -0.15, P = 0.036), and the heterogeneity across studies was significant (I2 = 65.4%) (Fig. 4(B)).
Fig. 4.
Forest plot results of the effect of garlic powder on blood pressure. (A) SBP and (B) DBP; WMD, weighted mean difference
Meta-regression
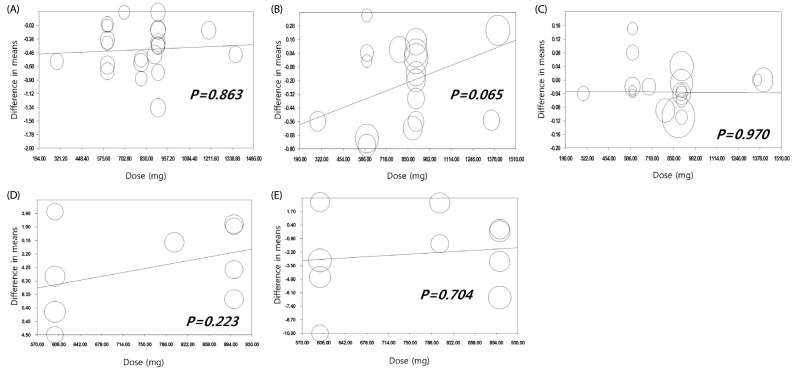
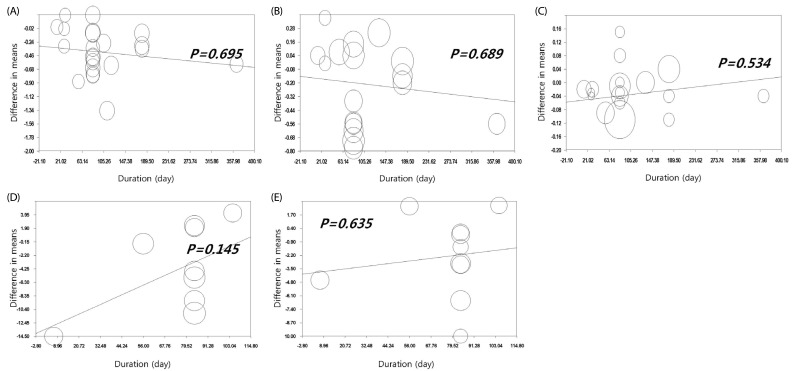
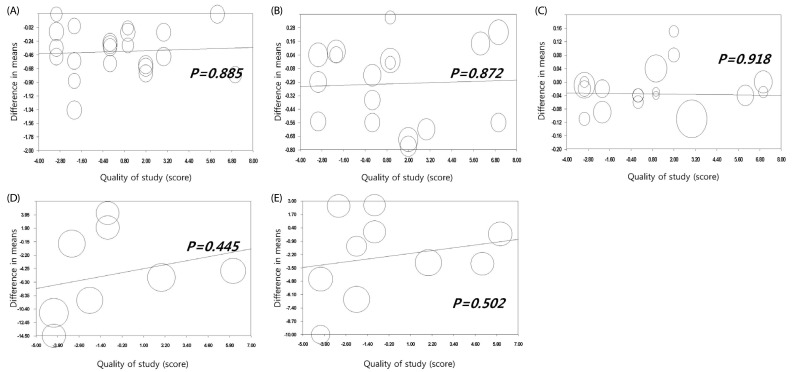
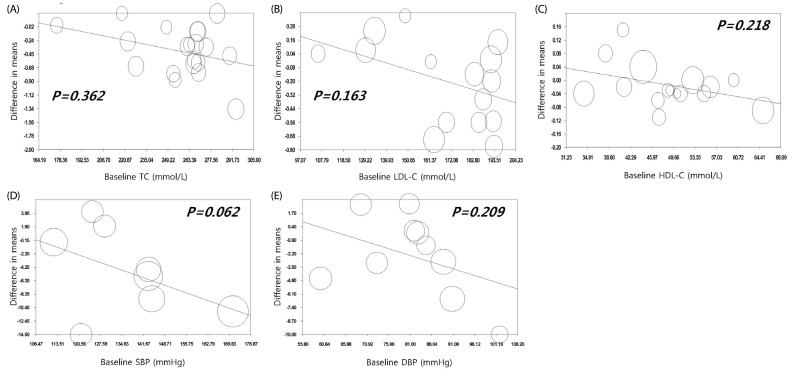
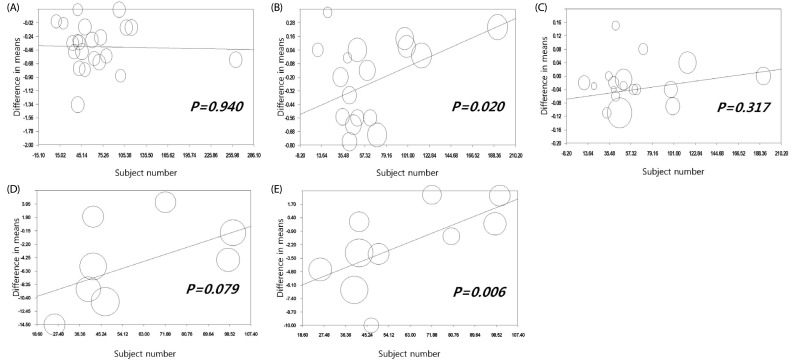
The effect of moderators, such as dosage, intervention duration, quality of study, baseline value or participant number, was analyzed using meta-regression. FBG was not included in these analyses given the limited number of studies. In addition, with regard to the cholesterol metabolism biomarkers, two studies [21,34] were excluded from the analysis of baseline values for TC, LDL-C and HDL-C due to lack of information. Our meta-regression analyses suggest that the effects of garlic on all of the variables were not moderated by the dosage, duration, quality or baseline value (Fig. 5,6,7,8). However, participant number was inversely associated with the effect size of LDL-C (slope = 0.004, P = 0.020) and DBP (slope = 0.093, P = 0.006) (Fig. 9).
Fig. 5.
Meta-regression analysis between changes in cardiovascular disease risk factors and garlic powder dosage. (A) Total cholesterol, (B) LDL-cholesterol, (C) HDL-cholesterol, (D) systolic blood pressure and (E) diastolic blood pressure.
Fig. 6.
Meta-regression analysis between changes in cardiovascular disease risk factors and duration of garlic powder supplementation. (A) Total cholesterol, (B) LDL-cholesterol, (C) HDL-cholesterol, (D) systolic blood pressure and (E) diastolic blood pressure.
Fig. 7.
Meta-regression analysis between changes in cardiovascular disease risk factors and study quality regarding garlic powder supplementation. (A) Total cholesterol, (B) LDL-cholesterol, (C) HDL-cholesterol, (D) systolic blood pressure and E) diastolic blood pressure.
Fig. 8.
Meta-regression analysis between changes in cardiovascular disease risk factors and baseline values of (A) total cholesterol, (B) LDL-cholesterol, (C) HDL-cholesterol, (D) systolic blood pressure and (E) diastolic blood pressure.
Fig. 9.
Meta-regression analysis between changes in cardiovascular disease risk factors and number of participants. (A) Total cholesterol, (B) LDL-cholesterol, (C) HDL-cholesterol, (D) systolic blood pressure and (E) diastolic blood pressure.
Sensitivity / subgroup analyses
We conducted a sensitivity analysis to ascertain whether the results were driven by a single study by sequentially omitting one study at a time (data not shown). No substantial change in the effect of garlic intake on TC, LDL-C, HDL-C, SBP or DBP was noted. In the case of FBG, the effect size was largely decreased after the omission of one study [31] and became non-significant, although between-study heterogeneity was markedly decreased (from 97.6 to 86.1%).
The results of the subgroup analyses are also presented in Table 2. Garlic supplementation was significantly effective in the reduction of TC levels in both the lower- and higher-dose groups (P < 0.000 and P = 0.018, respectively). In the other subgroups, garlic's effect on TC was significant in studies of longer duration (≥ 84 days, P = 0.006), in subjects with hypercholesterolemia (P = 0.009) and in other types of patients, such as those with type 2 diabetes (P = 0.046) or in non-Asian countries (P = 0.012). In contrast, the studies that were short-term (< 84 days), performed in healthy subjects or performed in Asia did not exhibit these changes. The LDL-C values were more striking in studies that used a lower dose (≤ 800 mg, P = 0.003), were of long-term duration (≥ 84 days, P = 0.012) or involved hypercholesterolemic subjects (P = 0.012). No significant change in HDL-C level was demonstrated in any subgroup for dose, subject and location, however, a small increase in higher-dose groups (≥ 800 mg, P = 0.024) was noted. The net change in SBP for garlic supplements compared with the control material was significant for the trials that were conducted in Europe or America (P = 0.028), administered a daily dose ≤ 800 mg (P = 0.019) and involved populations at high-risk for hypertension (P = 0.002). No significant effects were observed in all of the subgroups categorized by the intervention period. No group stratified by dosage exhibited a significant change in DBP. A significant DBP reduction was observed in the subgroups with a longer intervention duration (P = 0.031), hypertensive patients (P = 0.010) and locations in Europe or America (P = 0.008). FBG subgroup analysis was excluded given the small number of trials.
Table 2.
Results of subgroup analyses by dosage, duration, population and location
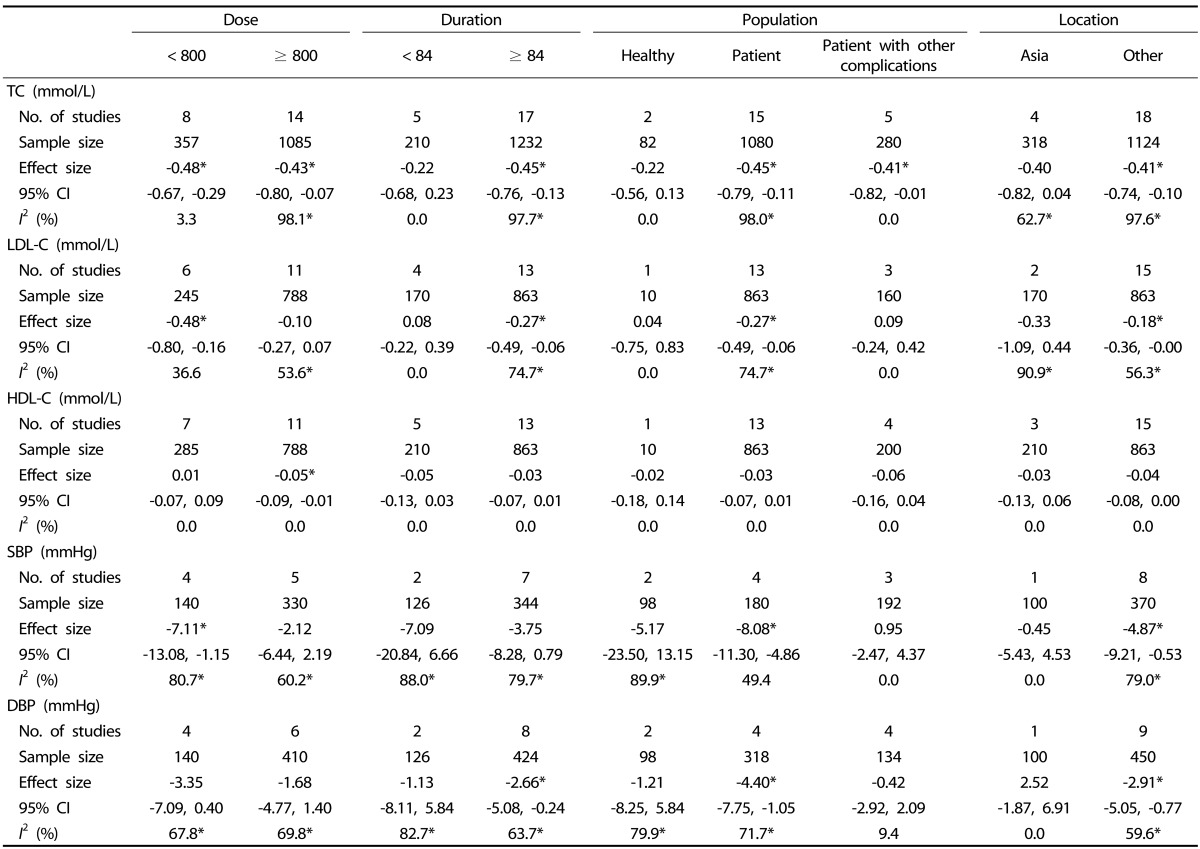
CI, confidence interval; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; FBG, fasting blood glucose; SBP, systolic blood pressure; DBP, diastolic blood pressure;
*P < 0.05
An additional sensitivity analysis limited to studies that demonstrated high compliance, high quality or placebo-control design; were published recently; were conducted with dietary management or supplemented with standardized garlic powder was performed (Table 3). The primary analysis on TC was confirmed, and the heterogeneity was improved in the analysis of high quality trials or supplemented with standardized materials (I2: from 96.9 to 62.3 or 67.2, respectively). The significant effect on LDL-C or DBP value was not significantly different from the effect demonstrated by the comprehensive meta-analyses restricted to studies that demonstrated high compliance, were recently published, were supplemented with standardized materials or used garlic powder with a high alliin content. The pooled effects of garlic on HDL-C were not altered when analyses were limited, with the exception of recently published studies. Contrary to the pooled results, the sensitivity test revealed no significant effect on FBG or SBP in all restricted categories.
Table 3.
Restriction sensitivity and heterogeneity analyses
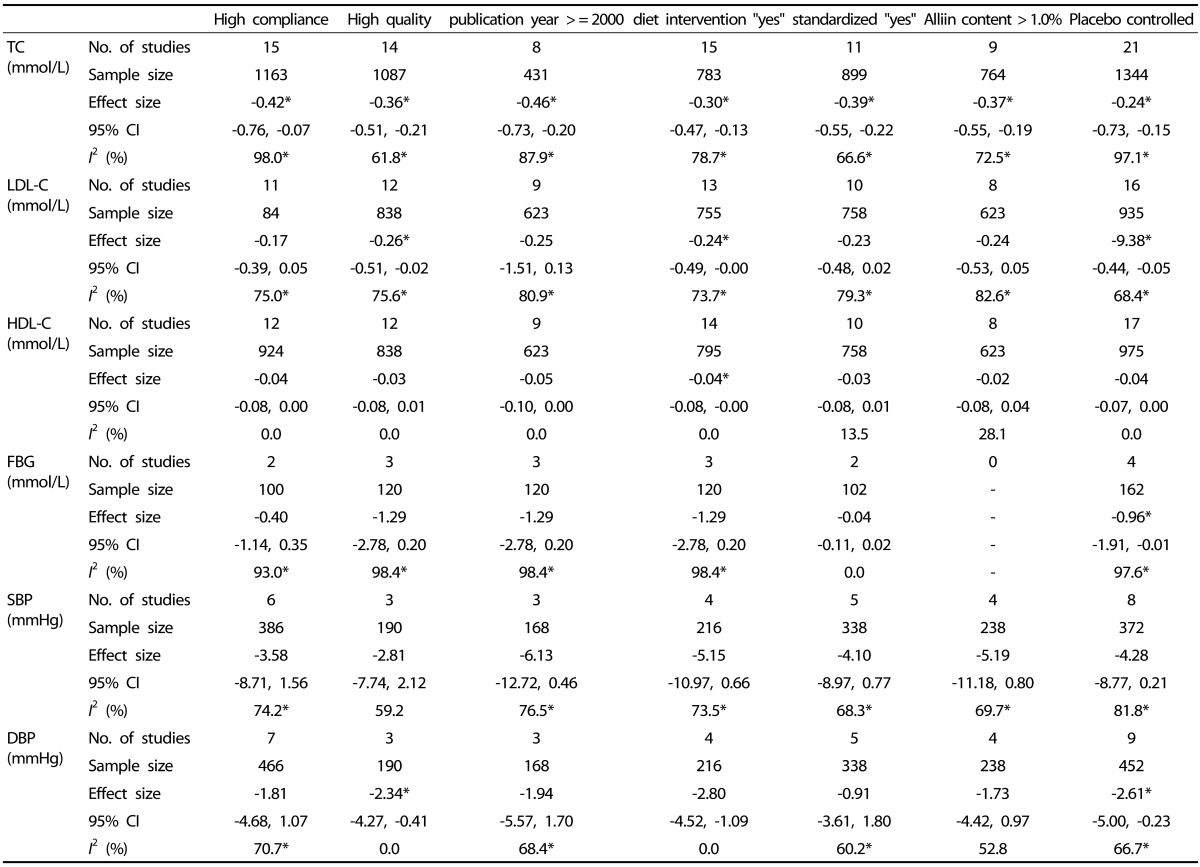
*P < 0.05
We conducted an additional analysis to investigate the gender-specific effects of garlic powder on blood lipid values with 2 trials (n = 163) for females and 3 trials (n = 155) for males (data not shown). The effect size of TC was greater in both the female (-0.81 mmol/L [-31.27 mg/dL], P = 0.018) and male groups (-0.72 mmol/L [-27.80 mg/dL], P = 0.000) than in the primary analysis, with improved heterogeneity (I2 = 0.0). Garlic's effect on LDL-C was significant only in the male group (-0.63 mmol/L [-24.32 mg/dL], P = 0.000), showing low heterogeneity (I2 = 0.0). However, no significant change in HDL-C level was demonstrated for either gender, which was consistent with the primary analysis. Blood pressure and FBG were not evaluated in the gender-specific analysis, as limited numbers were obtained for this part of the study.
Publication bias
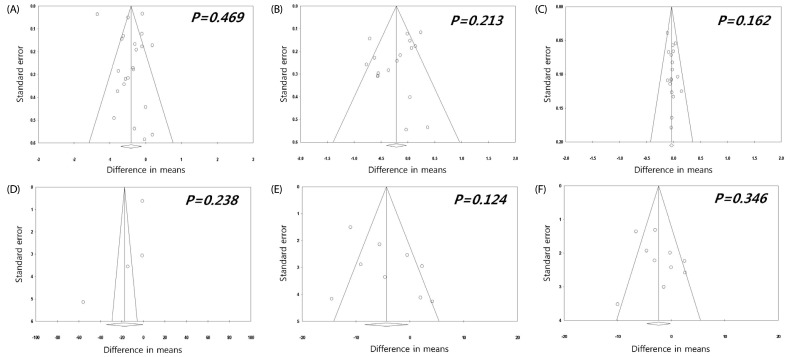
Publication bias was evaluated by funnel plots and Egger's regression test. The plots exhibited a typical funnel shape, and Egger's regression test suggested no evidence of substantial publication bias (P > 0.05) (Fig. 10).
Fig. 10.
Funnel plot showing the effects of the garlic powder intervention on changes in (A) total cholesterol, (B) LDL-cholesterol, (C) HDL-cholesterol, (D) fasting blood glucose, (E) systolic blood pressure and (F) diastolic blood pressure.
DISCUSSION
This meta-analysis demonstrated the efficacy of garlic powder intake on CVD risk factors using 27 RCTs that collectively included 1,649 participants. To the best of our knowledge, this meta-analysis is the first to present the finding that garlic consumed as a powder preparation improved multiple CVD risk factors. Garlic powder supplementation significantly reduced blood TC, LDL-C and FBG levels, along with SBP and DBP compared with control substances. Although the HDL-C data did not achieve statistical significance, overall these data support the potential cardiovascular benefits of garlic powder. Garlic contains various sulfur compounds, such as γ-glutamyl-S-allyl-L-cysteines and S-allyl-L-cysteine sulfoxide, which are organosulfur compounds that are processed or metabolized into diallyl sulfide, diallyl disulfide, diallyl trisulfide, diallyl tetrasulfide, ajoene and S-allyl cysteines; these compounds have been shown to exert cardiovascular effects/benefits [45]. Garlic preparations may be categorized as powders, oils, AGE or raw (not processed), and the chemical profile may vary according to these preparation types, including the active compounds. S-allyl cysteine has been identified as the active and stable component of AGE. However, the active component in garlic powder is less well established given that the commonly named allicin, an alliin derivative, is volatile [6,45,46]. The strength of our analysis is derived from the meta-analysis that exclusively focused on garlic powder and therefore excluded a major confounder attributed to garlic product preparation variability.
We demonstrated a -0.41 mmol/L (-15.83 mg/dL) and -0.21 mmol/L (-8.11 mg/dL) reduction in blood TC and LDL-C levels, respectively, in subjects who received garlic powder compared with the controls. An elevated blood cholesterol level is one of the major risk factors for CVD. Roberts [47] reviewed evidence regarding the 10 factors identified by the National Cholesterol Education Program (NCEP) and concluded that elevated serum TC levels (> 3.9 mmol/L (150 mg/dL)), specifically an elevated serum LDL-C level, is the only absolute, unequivocal, independent atherosclerotic risk factor. Serum cholesterol levels are frequently used as secondary/surrogate outcome measures of CVD disease progression. In the case of blood TC levels, our findings were consistent with those of previous meta-analyses that evaluated the hypocholesterolemic effect of garlic and resulted in an effect size ranging from -0.77 to -0.19 mmol/L (-29.73 ~ -7.33 mg/dL) for the TC level [4,6,37]. The results of the sub-analyses of garlic preparations in previous studies support the consistency with which "garlic powder" intake significantly reduced blood TC levels by -0.36 to -0.31 mmol/L (-13.90 ~ -11.97 mg/dL) [4,6,37]. Recently, meta-analyses investigating garlic consumption with respect to blood LDL-C or HDL-C levels reported conflicting findings. Ried et al. [4] demonstrated that garlic intake significantly improved these end points, whereas three meta-analyses questioned the robustness of such findings and the reported clinical effectiveness [6,7,37]. In contrast to the previous meta-analyses, our meta-analysis exclusively included garlic powder intake to avoid confounders. Furthermore, the amount of garlic powder intake could be compared in the present study. Interestingly, a lower dosage (< 800 mg/day) demonstrated a more profound effect on LDL-C in the subgroup analysis. In agreement with the previous meta-analysis, a longer duration was more effective in improving blood cholesterol levels.
This study is the first to conduct a meta-analysis of the effects of garlic powder intake on blood glucose metabolism. In the four included studies in which the subjects had type II DM or hypercholesterolemia, the FBG level was significantly decreased by -0.96 mmol/L (95% CI, -1.91, -0.01; P = 0.047) (-17.30 mg/dL [95% CI, -34.41, -0.18]). Garlic powder supplementation also exerted a small but significant hypotensive effect on both SBP (-4.34 mmHg, P = 0.036) and DBP (-2.36 mmHg, P = 0.036). The effect size for all subjects was -7.7 ~ -4.6 mmHg for the SBP levels and -5.0 ~ -2.4 mmHg for the DBP levels, which were similar to the decreased levels reported in previous meta-analyses [5,48]. However, the meta-analysis of hypertensive subjects (SBP ≥ 140 mmHg) demonstrated a potent effect size with a -16.33 mmHg decrease for SBP and -9.28 mmHg for DBP [49]. We also observed more profound effect sizes than were observed for the total analysis in our subgroup analysis, which demonstrated a -8.08 mmHg decrease for SBP and -4.40 mmHg for DBP. In agreement with the meta-analysis results of blood lipid levels, the lower dosage group exhibited a higher effect size for SBP; however, the duration of intake did not appear to be a potent moderator of BP levels in the subgroup analysis. Although a significant reduction of LDL-C was observed only in the male group, it is difficult to generalize that garlic is more effective in males than females due to the limited number of study in this analysis.
This systematic review, the most comprehensive to date, included moderate- to high-quality RCTs that investigated the effect of garlic powder on cardiovascular risk factors, such as blood lipids, FBG and BP, thereby allowing for meaningful subgroup analyses by dosage, trial duration and baseline levels. Certain limitations of this analysis should be noted. Due to the high heterogeneity in meta-analyses, the resulting effect sizes should be interpreted with some degree of caution despite the lack of publication bias. The reason for the heterogeneity was explored using meta-regression, subgroup analyses and sensitivity analyses. However, no factors, such as dose, duration, subject type, location and study quality, significantly changed heterogeneity, implying the presence of additional factors that might explain the high variability between the studies. How a lower dose of garlic powder affects LDL-C and SBP is still unclear. Additionally, a number of trials with short duration or with a limited number of included participants might influence the results of the present meta-analysis. The available data were insufficient to establish conclusive effects on FBG given the inclusion criterion of studies exclusively limited to garlic powder.
In summary, the present analysis revealed that garlic powder preparations could be considered a general heart and cardiovascular tonic with cholesterol (particularly LDL-C), FBG and BP regulatory properties. Thus, these preparations might be considered a healthy functional food and a dietary supplement for conventional diets. Because the Korean mean daily intake of garlic powder (1.9 g, which is equivalent to 4.7 g of fresh garlic) covers the effective dosage (0.3 - 1.4 g), clinical benefits on ordinary dietary intake of garlic is suggested. However, the 33% of the Korean population whose consumption level of garlic is below the effective dosage should take an additional dietary, garlic supplement. Further trials on the effects of garlic on cardiovascular risk factors should include information on the active ingredients in standardized garlic preparations. Additionally, meta-analyses examining other garlic preparations, such as AGE or garlic oil, and cardiovascular risk factors might be needed to explore the preventive effects of garlic intake.
Footnotes
This study was performed with the support of the Cooperative Research Program for Agriculture Science & Technology Development funded by the Rural Development Administration (Project No. PJ008450022014), Republic of Korea.
References
- 1.World Health Organization; World Heart Federation; World Stroke Organization. Global Atlas on Cardiovascular Disease Prevention and Control. Geneva: World Health Organization; 2011. [Google Scholar]
- 2.Verschuren WM, Jacobs DR, Bloemberg BP, Kromhout D, Menotti A, Aravanis C, Blackburn H, Buzina R, Dontas AS, Fidanza F, Karvonen MJ, Nedelijković S, Nissinen A, Toshima H. Serum total cholesterol and long-term coronary heart disease mortality in different cultures. Twenty-five-year follow-up of the seven countries study. JAMA. 1995;274:131–136. [PubMed] [Google Scholar]
- 3.Amagase H. Clarifying the real bioactive constituents of garlic. J Nutr. 2006;136:716S–725S. doi: 10.1093/jn/136.3.716S. [DOI] [PubMed] [Google Scholar]
- 4.Ried K, Toben C, Fakler P. Effect of garlic on serum lipids: an updated meta-analysis. Nutr Rev. 2013;71:282–299. doi: 10.1111/nure.12012. [DOI] [PubMed] [Google Scholar]
- 5.Silagy CA, Neil HA. A meta-analysis of the effect of garlic on blood pressure. J Hypertens. 1994;12:463–468. [PubMed] [Google Scholar]
- 6.Zeng T, Guo FF, Zhang CL, Song FY, Zhao XL, Xie KQ. A metaanalysis of randomized, double-blind, placebo-controlled trials for the effects of garlic on serum lipid profiles. J Sci Food Agric. 2012;92:1892–1902. doi: 10.1002/jsfa.5557. [DOI] [PubMed] [Google Scholar]
- 7.Khoo YS, Aziz Z. Garlic supplementation and serum cholesterol: a meta-analysis. J Clin Pharm Ther. 2009;34:133–145. doi: 10.1111/j.1365-2710.2008.00998.x. [DOI] [PubMed] [Google Scholar]
- 8.You SJ, Ahn BK, Kang CW. Effects of dietary garlic powder on growth performance and mRNA expression of hepatic HMG-CoA reductase in broiler chickens. J Anim Sci Technol. 2009;51:307–314. [Google Scholar]
- 9.Kim-Park S, Ku DD. Garlic elicits a nitric oxide-dependent relaxation and inhibits hypoxic pulmonary vasoconstriction in rats. Clin Exp Pharmacol Physiol. 2000;27:780–786. doi: 10.1046/j.1440-1681.2000.03333.x. [DOI] [PubMed] [Google Scholar]
- 10.Al-Qattan KK, Thomson M, Al-Mutawa'a S, Al-Hajeri D, Drobiova H, Ali M. Nitric oxide mediates the blood-pressure lowering effect of garlic in the rat two-kidney, one-clip model of hypertension. J Nutr. 2006;136:774S–776S. doi: 10.1093/jn/136.3.774S. [DOI] [PubMed] [Google Scholar]
- 11.Adler AJ, Holub BJ. Effect of garlic and fish-oil supplementation on serum lipid and lipoprotein concentrations in hypercholesterolemic men. Am J Clin Nutr. 1997;65:445–450. doi: 10.1093/ajcn/65.2.445. [DOI] [PubMed] [Google Scholar]
- 12.Anim-Nyame N, Sooranna SR, Johnson MR, Gamble J, Steer PJ. Garlic supplementation increases peripheral blood flow: a role for interleukin-6? J Nutr Biochem. 2004;15:30–36. doi: 10.1016/j.jnutbio.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Ashraf R, Aamir K, Shaikh AR, Ahmed T. Effects of garlic on dyslipidemia in patients with type 2 diabetes mellitus. J Ayub Med Coll Abbottabad. 2005;17:60–64. [PubMed] [Google Scholar]
- 14.Ashraf R, Khan RA, Ashraf I. Garlic (Allium sativum) supplementation with standard antidiabetic agent provides better diabetic control in type 2 diabetes patients. Pak J Pharm Sci. 2011;24:565–570. [PubMed] [Google Scholar]
- 15.Auer W, Eiber A, Hertkorn E, Hoehfeld E, Koehrle U, Lorenz A, Mader F, Merx W, Otto G, Schmid-Otto B. Hypertension and hyperlipidaemia: garlic helps in mild cases. Br J Clin Pract Suppl. 1990;69:3–6. [PubMed] [Google Scholar]
- 16.Byrne DJ, Neil HA, Vallance DT, Winder AF. A pilot study of garlic consumption shows no significant effect on markers of oxidation or sub-fraction composition of low-density lipoprotein including lipoprotein(a) after allowance for non-compliance and the placebo effect. Clin Chim Acta. 1999;285:21–33. doi: 10.1016/s0009-8981(99)00063-7. [DOI] [PubMed] [Google Scholar]
- 17.Gardner CD, Lawson LD, Block E, Chatterjee LM, Kiazand A, Balise RR, Kraemer HC. Effect of raw garlic vs commercial garlic supplements on plasma lipid concentrations in adults with moderate hypercholesterolemia: a randomized clinical trial. Arch Intern Med. 2007;167:346–353. doi: 10.1001/archinte.167.4.346. [DOI] [PubMed] [Google Scholar]
- 18.Holzgartner H, Schmidt U, Kuhn U. Comparison of the efficacy and tolerance of a garlic preparation vs. bezafibrate. Arzneimittelforschung. 1992;42:1473–1477. [PubMed] [Google Scholar]
- 19.Isaacsohn JL, Moser M, Stein EA, Dudley K, Davey JA, Liskov E, Black HR. Garlic powder and plasma lipids and lipoproteins: a multicenter, randomized, placebo-controlled trial. Arch Intern Med. 1998;158:1189–1194. doi: 10.1001/archinte.158.11.1189. [DOI] [PubMed] [Google Scholar]
- 20.Jain AK, Vargas R, Gotzkowsky S, McMahon FG. Can garlic reduce levels of serum lipids? A controlled clinical study. Am J Med. 1993;94:632–635. doi: 10.1016/0002-9343(93)90216-c. [DOI] [PubMed] [Google Scholar]
- 21.Kannar D, Wattanapenpaiboon N, Savige GS, Wahlqvist ML. Hypocholesterolemic effect of an enteric-coated garlic supplement. J Am Coll Nutr. 2001;20:225–231. doi: 10.1080/07315724.2001.10719036. [DOI] [PubMed] [Google Scholar]
- 22.Kiesewetter H, Jung F, Jung EM, Blume J, Mrowietz C, Birk A, Koscielny J, Wenzel E. Effects of garlic coated tablets in peripheral arterial occlusive disease. Clin Investig. 1993;71:383–386. doi: 10.1007/BF00186628. [DOI] [PubMed] [Google Scholar]
- 23.Lash JP, Cardoso LR, Mesler PM, Walczak DA, Pollak R. The effect of garlic on hypercholesterolemia in renal transplant patients. Transplant Proc. 1998;30:189–191. doi: 10.1016/s0041-1345(97)01227-x. [DOI] [PubMed] [Google Scholar]
- 24.Mader FH. Treatment of hyperlipidaemia with garlic-powder tablets. Evidence from the German Association of General Practitioners' multicentric placebo-controlled double-blind study. Arzneimittelforschung. 1990;40:1111–1116. [PubMed] [Google Scholar]
- 25.Neil HA, Silagy CA, Lancaster T, Hodgeman J, Vos K, Moore JW, Jones L, Cahill J, Fowler GH. Garlic powder in the treatment of moderate hyperlipidaemia: a controlled trial and meta-analysis. J R Coll Physicians Lond. 1996;30:329–334. [PMC free article] [PubMed] [Google Scholar]
- 26.Phelps S, Harris WS. Garlic supplementation and lipoprotein oxidation susceptibility. Lipids. 1993;28:475–477. doi: 10.1007/BF02535949. [DOI] [PubMed] [Google Scholar]
- 27.Rahmani M, Tabari AK, Niaki K, Allahaverdian S, Sheikholeslami M. Effect of dried garlic supplementation on blood lipids in mild and moderate hypercholesterolemic patients. Arch Iran Med. 1999;2:19–23. [Google Scholar]
- 28.De A, Gruenwald J. Effect of garlic powder tablets on blood lipids and blood pressure: a six month placebo controlled, double blind study. Br J Clin Res. 1993;4:37–44. [Google Scholar]
- 29.Saradeth T, Seidl S, Resch KL, Ernst E. Does garlic alter the lipid pattern in normal volunteers? Phytomedicine. 1994;1:183–185. doi: 10.1016/S0944-7113(11)80062-0. [DOI] [PubMed] [Google Scholar]
- 30.Sitprija S, Plengvidhya C, Kangkaya V, Bhuvapanich S, Tunkayoon M. Garlic and diabetes mellitus phase II clinical trial. J Med Assoc Thai. 1987;70(Suppl 2):223–227. [PubMed] [Google Scholar]
- 31.Sobenin IA, Andrianova IV, Demidova ON, Gorchakova T, Orekhov AN. Lipid-lowering effects of time-released garlic powder tablets in double-blinded placebo-controlled randomized study. J Atheroscler Thromb. 2008;15:334–338. doi: 10.5551/jat.e550. [DOI] [PubMed] [Google Scholar]
- 32.Sobenin IA, Nedosugova LV, Filatova LV, Balabolkin MI, Gorchakova TV, Orekhov AN. Metabolic effects of time-released garlic powder tablets in type 2 diabetes mellitus: the results of double-blinded placebo-controlled study. Acta Diabetol. 2008;45:1–6. doi: 10.1007/s00592-007-0011-x. [DOI] [PubMed] [Google Scholar]
- 33.Sobenin IA, Pryanishnikov VV, Kunnova LM, Rabinovich YA, Martirosyan DM, Orekhov AN. The effects of time-released garlic powder tablets on multifunctional cardiovascular risk in patients with coronary artery disease. Lipids Health Dis. 2010;9:119. doi: 10.1186/1476-511X-9-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Superko HR, Krauss RM. Garlic powder, effect on plasma lipids, postprandial lipemia, low-density lipoprotein particle size, high-density lipoprotein subclass distribution and lipoprotein(a) J Am Coll Cardiol. 2000;35:321–326. doi: 10.1016/s0735-1097(99)90541-7. [DOI] [PubMed] [Google Scholar]
- 35.Vorberg G, Schneider B. Therapy with garlic: results of a placebo-controlled, double-blind study. Br J Clin Pract Suppl. 1990;69:7–11. [PubMed] [Google Scholar]
- 36.Ziaei S, Hantoshzadeh S, Rezasoltani P, Lamyian M. The effect of garlic tablet on plasma lipids and platelet aggregation in nulliparous pregnants at high risk of preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2001;99:201–206. doi: 10.1016/s0301-2115(01)00384-0. [DOI] [PubMed] [Google Scholar]
- 37.Reinhart KM, Talati R, White CM, Coleman CI. The impact of garlic on lipid parameters: a systematic review and meta-analysis. Nutr Res Rev. 2009;22:39–48. doi: 10.1017/S0954422409350003. [DOI] [PubMed] [Google Scholar]
- 38.Staba EJ, Lash L, Staba JE. A commentary on the effects of garlic extraction and formulation on product composition. J Nutr. 2001;131:1118S–1119S. doi: 10.1093/jn/131.3.1118S. [DOI] [PubMed] [Google Scholar]
- 39.D'Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 40.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 41.Kim JA, Montagnani M, Koh KK, Quon MJ. Reciprocal relationships between insulin resistance and endothelial dysfunction: molecular and pathophysiological mechanisms. Circulation. 2006;113:1888–1904. doi: 10.1161/CIRCULATIONAHA.105.563213. [DOI] [PubMed] [Google Scholar]
- 42.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [Internet] Oxford: The Cochrane Collaboration; 2011. [updated 2011 March]. [cited 2014 June 1]. Available from: www.cochrane-handbook.org. [Google Scholar]
- 44.Kim JY, Kwon O. Garlic intake and cancer risk: an analysis using the Food and Drug Administration's evidence-based review system for the scientific evaluation of health claims. Am J Clin Nutr. 2009;89:257–264. doi: 10.3945/ajcn.2008.26142. [DOI] [PubMed] [Google Scholar]
- 45.Zeng T, Zhang CL, Zhao XL, Xie KQ. The roles of garlic on the lipid parameters: a systematic review of the literature. Crit Rev Food Sci Nutr. 2013;53:215–230. doi: 10.1080/10408398.2010.523148. [DOI] [PubMed] [Google Scholar]
- 46.Rahman K, Lowe GM. Garlic and cardiovascular disease: a critical review. J Nutr. 2006;136:736S–740S. doi: 10.1093/jn/136.3.736S. [DOI] [PubMed] [Google Scholar]
- 47.Roberts WC. Atherosclerotic risk factors--are there ten or is there only one? Am J Cardiol. 1989;64:552–554. doi: 10.1016/0002-9149(89)90444-x. [DOI] [PubMed] [Google Scholar]
- 48.Ried K, Frank OR, Stocks NP, Fakler P, Sullivan T. Effect of garlic on blood pressure: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2008;8:13. doi: 10.1186/1471-2261-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reinhart KM, Coleman CI, Teevan C, Vachhani P, White CM. Effects of garlic on blood pressure in patients with and without systolic hypertension: a meta-analysis. Ann Pharmacother. 2008;42:1766–1771. doi: 10.1345/aph.1L319. [DOI] [PubMed] [Google Scholar]