Abstract
Background:
Studies show residents of sober living recovery houses (SLHs) make improvements in a variety of areas including alcohol and drug use, arrests, and employment. Longitudinal measures of motivation (assessed as costs and benefits of continuing sobriety) have been shown to be associated with alcohol and drug outcomes in SLHs. However, how motivation interacts with other potentially important factors, such as psychiatric severity, is unclear.
Objective:
The present study aimed to assess how perceived costs and benefits of sobriety among residents of SLHs differed by psychiatric severity. The study also aimed to assess how costs and benefits interacted with psychiatric severity to influence outcome.
Methods:
Two hundred forty-five residents of SLHs were assessed at baseline and 6, 12, and 18 months.
Results:
High psychiatric severity was associated with higher severity of alcohol and drug problems and higher perceived costs of sobriety at all data collection time points. Perceived costs and benefits of sobriety were strong predictors of alcohol and drug problems for participants with low psychiatric severity. Perceived costs, but not perceived benefits, predicted outcomes for residents with high psychiatric severity.
Conclusions/Importance:
High psychiatric severity is a serious impediment for some residents in SLHs. These individuals perceive sobriety as difficult and that perception is associated with worse outcome. Finding ways to decrease perceived costs and challenges to sustained sobriety among these individuals is essential as is collaboration with local mental health services. SLHs should consider whether additional onsite services or modifications of SLH operations might help this population.
Keywords: Sober Living House, Residential Treatment, Recovery House, Psychiatric
The plethora of literature on mental health disorders in substance abusing populations is testament to the high prevalence of the rates observed. Indeed, the National Survey of Alcohol and Related Conditions (NESARC) found that 60% of adults seeking treatment for substance use disorders reported at least mild mood or anxiety disorders (Clark, Power, Le Fauve, & Lopez, 2008). Moreover, comparisons between individuals seeking mental health and substance abuse services found few differences on measures of diagnosis, drug use, and problem severity (Havassy, Alvidrez, & Owen, 2004).
A large body of work substantiates that severity of psychiatric problems are associated with poorer treatment outcomes (Compton, Cottler, Jacobs, Ben-Abdallah, & Spitznagel, 2003; Ritsher, McKellar, Finney, Otilingam, & Moos, 2002). For example, a study of male alcoholics (n=460) and drug addicts (n=282) in various types of treatment programs found patients with low psychiatric severity at admission showed improvement at 6-month follow-up but those with high severity did not (McLellan, Luborsky, Woody, O’Brien, & Druley, 1983) . More recent studies have also shown that co-occurrence of mental health and substance use problems can impede effective treatment. In a review of outcomes among substance abuse clients in treatment McNulty and Kouimtsidis (2001) concluded that depression at entry into treatment is associated with lower treatment engagement and poorer substance use outcomes. Using data from 526 adults in a large clinical trial of persons with methamphetamine disorders researchers Glasner-Edwards et al (2010) found the presence of various psychiatric disorders at post treatment was associated with more methamphetamine use. However, psychiatric disorders were only assessed at 3-year follow-up and the analyses reported did not show how changes in psychiatric symptoms were associated with changes in MA use over time. The lack of studies assessing longitudinal effects of psychiatric severity represents a limitation in the current literature.
Few studies have assessed how the relationship between psychiatric severity and outcome might be affected by a variety of factors, such as motivation for change. The transtheoretical model of motivation (DiClemente, Schlundt, & Gemmell, 2004) has received considerable attention as a way to describe motivation among substance users. Five stages are described, beginning with pre-contemplation (little of no motivation) and proceeding through contemplation, preparation, action and maintenance. Consideration of what has been termed “decisional balance,” or the anticipated pros and cons of making a change weighs heavily in determining level of motivation. Cunningham and colleagues (Cunningham, Sobell, Gavin, Sobell, & Breslin, 1997) capitalized on this notion of pros and cons by developing the Alcohol and Drug Consequences Questionnaire (ADCQ), which quantifies reasons for making a change in substance use (benefits) and the reasons to not make a change (costs). Although motivation at treatment entry has been studied extensively, the magnitude of association between motivation and outcome at follow-up is typically small (Cunningham, et al., 1997; Project MATCH Research Group, 1998).
Motivation for changing substance use behavior among selected samples of comorbid substance abusers has been given some attention (Carey, 1996; Zhang, Harmon, Werkner, & McCormick, 2004), yet how motivation and the process of change works for comorbid substance abusers is still underdeveloped (DiClemente, Nidecker, & Bellack, 2008). We are aware of no studies assessing how measures of motivation and psychiatric severity interact to influence outcome. As with psychiatric severity, there are only a few studies (e.g., (Korcha, Polcin, Bond, Lapp, & Galloway, 2011) that examine the impact of motivation longitudinally rather than at baseline only. There are no studies that we know of that assess interactive effects of psychiatric severity and motivation.
Purpose
This paper addresses these gaps in the current literature by assessing how motivation interacts with psychiatric severity to impact substance abuse outcomes over an 18-month period. Data were drawn from a previous study of sober living recovery houses (SLHs) for alcohol and drug problems (Polcin, Korcha, Bond, & Galloway, 2010). Understanding factors associated with outcome in SLHs is important because research has demonstrated strong favorable outcomes. (Polcin, et al., 2010) studied N=245 residents of SLHs and found they significantly reduced or stopped their substance use between baseline and 6-month follow-up and then maintained those improvements at 12 and 18 months after the baseline interview. It was noteworthy that a wide variety of individuals had positive outcomes and improvements were maintained at the 18-month follow-up even though the average length of stay at the SLH was approximately 5 months (mean=166 days, sd=11 days). Also observed was an association between motivation, which was measured as costs and benefits of sobriety, and substance use outcomes (Korcha, et al., 2011). Although we found initial improvement on psychiatric severity, these improvements were not maintained at the final follow-up (18 months) and psychiatric severity remained relatively high at all study time points.
Study Aims
The primary aims of the analyses reported here were first to understand how psychiatric symptoms were associated with alcohol and drug outcome over time and second to understand whether psychiatric severity interacted with motivation to impact outcome. Consistent with a variety of findings in the substance abuse field, we expected to find that higher psychiatric severity would be associated with worse alcohol and drug outcome. We also expected that motivation might be less influential among individuals with higher psychiatric severity. We surmised even if they were motivated for maintaining sobriety (high perceived benefits and low perceived costs) their psychiatric issues might undermine progress.
Methods
Sober Living Houses
SLHs are a type of residential recovery service that offers long-term, alcohol- and drug-free housing for persons with alcohol and drug problems. They are not licensed as treatment and do not offer formal services such as case management, individual counseling, or group counseling. However, all residents are required to attend 12-step meetings and abide by house rules, such as abstaining from substance use and attending house meetings. The houses are financially self-sufficient through resident fees. In addition to substance abuse problems, a majority experience some level of difficulty with psychiatric symptoms such as anxiety or depression. For a more complete description of the structure and operations of SLHs see (Polcin & Henderson, 2008).
Data Collection Site
All study participants were recruited from Clean and Sober Transitional Living (CSTL) in Sacramento County California between January 2004 and July 2006. At the time the data were collected CSLT operated 16 freestanding SLHs with a 136 bed capacity. The program offered no onsite treatment services, but residents were required to attend mutual help 12-step meetings. Unlike halfway houses affiliated with treatment, CSTL residents were free to stay as long as they wished provided they abided by house rules (e.g., no use of substances).
For the most part the program was financed through resident fees. CSLT houses were divided into two phases. Phase I houses were for entering residents and they were designed to orient the resident to the program and help them establish a recovery program. Phase II houses were for residents wh0 had successfully completed phase I and allowed for more autonomy in the community. A more complete description of CSTL can be found in Polcin and Henderson (2008) or (Wittman & Polcin, in press).
Sample
Two hundred forty five residents of CSLT were recruited into the study during their first week after entering the house. In order to maximize our ability to generalize results we employed few inclusion/exclusion criteria: all study participants were age 18 or older and competent to provide informed consent. No individuals were exclude using these criteria and very few (<5) who entered the program during the study period opted to not participate. Most participants were men (77%), never married (50%) and most were white (73%). Resident age ranged from 18 to 71 with a mean of 37 years (sd=10). Nearly half (49%) of the residents met DSM IV dependence criteria for poly-substances while the remainder were dependent on singular substances of amphetamines (16%), alcohol (12%), cocaine (4%), opiates (5%) and marijuana (1%). Approximately 12% did not met DSM IV criteria for past 12-month substance dependence. The vast majority of residents had a prior history of receiving formal alcohol or drug treatment and about a quarter were referred through the criminal justice system.
Measures
Demographic Characteristics included standard demographic questions such as age, gender, ethnicity, marital status, and education.
DSM IV Checklist for Past 12 Month Alcohol and Drug Dependence was used to assess substance use disorders over the past 12 months. Items are based on DSM IV diagnostic criteria (American Psychiatric Association, 2000). Wu et al (2009) reported Crobach’s alphas > 0.8 when used to assess opioid and cocaine dependence.
Addiction Severity Index Lite (ASI): The ASI is a standardized, structured interview that assesses problem severity in six areas: medical, employment/support, drug/alcohol, legal, family/social and psychological. The ASI measures a 30 day time period and provides composite scores between 0 and 1 for each problem area. The ASI has demonstrated good to excellent reliability and validity in numerous studies (McLellan et al., 1992). Cronback’s alphas for composite scores range from 0.68 to 0.87 and test retest reliability ranges from o.88 to 0.99. Although the instrument includes a measure of psychiatric severity as well, we opted to identify psychiatric severity based on a multi-dimensional scale, the Brief Symptom Inventory.
Psychiatric symptoms: To assess current psychiatric severity we used the Brief Symptom Inventory (Derogatis & Melisaratos, 1983). This 53-item measure assesses severity of psychiatric symptoms on nine clinical scales as well as three global indices. Assessments of internal consistency resulted in Cronbach’s alphas ranging from 0.71 to 0.85 across the clinical scales. We used one of the global indices, the Global Severity Index (GSI) as our measure of psychiatric severity, which has a test-retest reliability of 0.90. Items are rated on a 5-point scale and ask about symptoms over the past 7 days. Higher psychiatric symptomatology was indicated if a resident scored two standard deviations or more above the normed mean established for non-psychiatric patient populations (Derogatis & Melisaratos, 1983).
Six month measures of alcohol and drug use: These measures were modifications of measures taken from (Gerstein et al., 1994) and labeled Peak Density and 6-month abstinence. Peak Density is the number of days of any substance use (i.e., any alcohol or drug) during the month of highest use over the past 6 months. Six-month abstinence was a dichotomous yes/no regarding any use of alcohol of drugs over the past 6 months.
Alcohol and Drug Consequences Questionnaire (ADCQ): Motivation was assessed using the ADCQ. This instrument was developed as part of a treatment evaluation of a brief cognitive-behavioural intervention for alcohol and drug abusers (Cunningham, 1997). Items draw on decision making theory (Janis, 1977) and assess the ’pros’ and ‘cons’ about alcohol and drug use. The ADCQ has 29 items and two scales, one assessing costs and the other assessing benefits. Responses are measured on a 6-point Likert scale ranging from zero to five. Examples of costs include items such as “I will have difficulty relaxing,” “I will get depressed,” and “I will feel bored.” Examples of benefits include items such as “I will have a better relationship with my family,” “I will feel better about myself,” and “I will be more active and alert.” The two ADCQ mean scale scores for the perceived benefits and perceived costs were calculated at each interview. The lowest response selection was “Probably will not happen to me” and rated ‘0’ while other responses were rated from 1 (“not important”) to 5 (“extremely important”).
The questionnaire was administered by interviewers at every time point. Because this instrument was administered several times over the course of the study and many study participants had established abstinence from substance use, participants were asked to consider and choose one of two options: (1) “if I keep my sobriety” or (2) “if I stop or cut down.” Questions were asked based on the motivation toward substance use (e.g. “If I stop or cut down, I will have fewer problems with friends” or “If I keep my sobriety, I will have fewer problems with friends”). The vast majority of participants at each data collection time point chose the “keep my sobriety” option: 97% at baseline, 81% at 6 months, 80% at 12 months and 77% at 18 months. Subscales of perceived costs consisted of 15 items and the perceived benefits subscale was inclusive of 14 items. Two scales were created by summing scores and dividing by the number of items. Cronbach’s alphas for our adapted way of using the instrument (the keep my sobriety preface) were excellent, 0.88 for costs and 0.84 for benefits
Procedures
Study participants completed a baseline interview within their first week of entering a SLH and were interviewed again at 6-, 12-, and 18-month follow-ups. Interviews required about 2 hours and participants were paid $30 for their time completing a baseline interview and $50 for their time completing each of the follow up interviews. All participants signed an informed consent to take part in the study and all were informed that their responses were confidential. Study procedures were approved by the Public Health Institute Institutional Review Board and a federal certificate of confidentiality was obtained, adding further protection to confidentiality.
Among the sample of 245, 89% (N=218) participated in at least one follow up interview. Follow up rates for each time point included 72% at 6 months, 71% at 12 months and 73% at 18 months. As described below, we used generalized estimating equations (GEE) for our main analyses, which enabled all participants to be included in analyses even if they have missed follow up interviews.
To assess whether individuals that we located and interviewed at follow up differed from those whom we were not able to locate we conducted baseline comparisons. Separate baseline comparisons were made for individuals interviewed and not interviewed at each time point. On each of these 3 comparisons we found no differences in terms of demographic characteristics, Addiction Severity Index scales (i.e., medical, legal, alcohol, drug, family, and vocational), psychiatric symptoms, and maximum number of days of substance use (alcohol or drugs) per month during the previous 6 months. Thus, the demographic characteristics and problem severity of individuals successfully followed up and lost at follow up were not significantly different. We did find that individuals located and interviewed spent on average more time in the SLHs than individuals lost to follow up.
Analysis Plan
To investigate the role psychiatric severity and motivation play in alcohol and drug severity outcomes across time, longitudinal profiles were estimated using latent class analysis (LCA) in Mplus (Muthén & Muthén, 2013). The number of classes was determined by examining the Bayesian Information Criteria (BIC), the Vuong-Lo-Mendell-Rubin likelihood ratio test, model entropy, class sample distribution, and interpretability of resulting class trajectories. ANOVA was used to test for differences in alcohol and drug outcomes as well as motivation scales across resulting psychiatric severity groups separately for each interview (baseline and 6, 12, and 18 months). Controlling for gender, age, education, and marital status, generalized estimating equation (GEE) (Diggle, Heagerty, Liang, & Zeger, 2002) modeling using an exchangeable error correlation structure was then used to estimate longitudinal change from baseline in alcohol and drug outcomes across psychiatric severity groups, using indicator variables for each of the 6, 12, and 18-month follow-up interviews. Finally, the relationship between motivation measures and alcohol and drug severity outcomes was estimated using lagged longitudinal GEE models, predicting alcohol and drug severity 6, 12, and 18 months from motivation at the prior interview and its interaction with the psychiatric severity group measure.
Results
Results from the LCA of psychiatric severity measures are shown in Table 1. The VLMR chi-square rejected the 1 class solution in favor of the 2-class solution and although it indicated marginal support for 3 compared to 2-classes, both the BIC and AIC indicated better fit for the 2 compared to the 3 and 4-class models. Entropy was similar for each of the models examined. Examination of the sample distribution across the solutions favored the 2-class solution as both the 3 and 4- class solutions produced additional classes with small proportions of the sample.
Table 1.
Latent class analysis solutions for psychiatric severity
| 2-Class Solution |
3-Class Solution |
4-Class Solution |
|
|---|---|---|---|
| BIC | 856.11 | 878.59 | 902.48 |
| AIC | 824.68 | 829.57 | 835.95 |
| VLMR p-value | < .001 | .03 | .06 |
| Entropy | .80 | .79 | .80 |
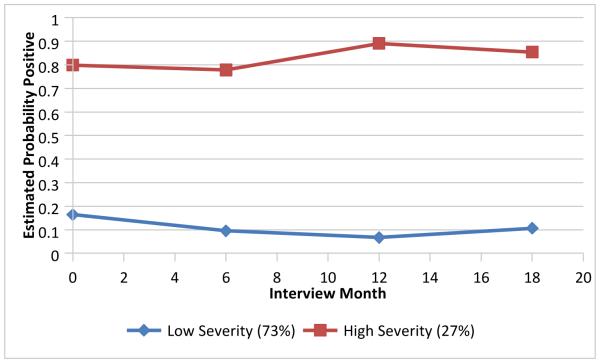
Plots of the estimated proportions within each class favored the 2-class solution (Figure 1), which was characterized by a class with low (ranging from about .10-.20) and fairly constant severity across interviews comprising about 73% of the sample and the second characterized by a high (ranging from .8-.9) and also fairly constant severity across interviews comprising about 27% of the sample. In subsequent analyses, these two classes will be referred to as low and high psychiatric severity groups, respectively.
Figure 1.
LCA Estimates of the proportion positive on psychiatric severity
When we compared demographic characteristics between the low and high psychiatric severity groups we found few differences. While there were no differences in age, education, race, marital status, or length of stay in the SLH, those in the higher psychiatric severity group had a higher proportion of women (33%) than those with lower psychiatric severity (19%). Table 2 shows comparisons of low and high psychiatric severity groups on measures of alcohol and drug severity and peak density at each data collection time point. Results from ANOVA models indicated ASI alcohol scores at each of the four time points were significantly higher for participants with high psychiatric severity compared to those with low severity. In terms of drug severity, mean ASI drug scores were higher among participants with high psychiatric severity for three of the four interviews with no significant differences found for peak density between groups at any interview.
Table 2.
Mean AST scores, peak density, costs of sobriety, and benefits of sobriety&.
|
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASI Alcohol | ASI Drag | Peak Density | Costs of sobriety | Benefits of sobriety | ||||||||||||||||
|
|
||||||||||||||||||||
| Low psych | High psych | Low psych | High psych | Low psych | High psych | Low psych | High psych | Low psych | High psych | |||||||||||
| mean | sd | Mean | sd | mean | sd | mean | sd | mean | sd | mean | sd | mean | sd | mean | sd | mean | sd | mean | sd | |
|
|
||||||||||||||||||||
| Baseline | 0.11 | 0.22 | 0.29 | 0.33*** | 0.07 | .10 | 0.08 | 0.11** | 18.5 | 13.0 | 19.7 | 12.7 | 1.03 | 1.04 | 1.49 | 1.16** | 4.31 | 0.75 | 4.23 | 0.77 |
| 6-month | 0.07 | 0.14 | 0.20 | 0.29*** | 0.05 | .09 | 0.05 | 0.09 | 9.9 | 12.7 | 11.7 | 12.3 | 0.78 | 0.99 | 1.30 | 1.10** | 3.88 | 1.26 | 4.05 | 1.01 |
| 12-month | 0.06 | 0.13 | 0.20 | 0.24*** | 0.04 | .08 | 0.05 | 0.09* | 8.6 | 12.3 | 12.2 | 13.0 | 0.63 | 0.78 | 1.41 | 1.25*** | 3.95 | 1.24 | 4.26 | 0.78 |
| 18-month | 0.07 | 0.15 | 0.17 | 0.24** | 0.04 | .07 | 0.06 | 0.09*** | 11.2 | 13.0 | 13.2 | 13.8 | 0.64 | 0.86 | 1.35 | 1.20*** | 3.99 | 1.14 | 4.33 | 0.73 |
|
| ||||||||||||||||||||
P values reflect ANOVA comparisons between psychiatric distress groups.
p < 0.05 ;
p < 0.01 ;
p < 0.001
In addition to comparisons of drug and alcohol outcomes by psychiatric severity, Table 2 shows how motivation as measured by the two ADCQ scales: costs and benefits of sobriety differed by psychiatric severity. Compared to participants with low psychiatric severity, those with high severity perceived higher costs associated with sobriety at all interviews. No differences between groups were found for the benefits scale.
To study how alcohol and drug use changed over time, GEE models assuming an exchangeable error correlation were estimated separately for each of the low and high psychiatric severity groups. Table 3 shows estimated differences in outcomes between each follow-up interview and baseline. For individuals with low psychiatric severity, there were significantly lower scores on the ASI alcohol and drug scales and less substance use as measured by peak density at every follow-up interview. The one exception was for alcohol severity at 18 months. Thus, participants with low psychiatric severity were able to maintain reductions in ASI drug and peak density measures from baseline to the 6-month interview were maintained throughout the follow-up time period of the study.
Table 3.
Generalized estimating equation models predicting ASI alcohol, ASI drug use and peak density by psychiatric severity~.
|
|
||||||
|---|---|---|---|---|---|---|
| Low psych severity | High psych severity | |||||
| (n=177) | (n=67) | |||||
|
|
||||||
|
Coefficien
t |
95% CI |
Coefficien
t |
95% CI | |||
|
|
||||||
| ASI alcohol(ref=baseline) | ||||||
| Baseline | ||||||
| 6-month | −0.03* | −0.06 | −0.01 | −0.06^ | −0.13 | −0.00 |
| 12-month | −0.03* | −0.06 | −0.01 | −0.06^ | −0.13 | −0.00 |
| 18-month | −0.02 | −0.05 | −0.01 | −0.08* | −0.13 | −0.00 |
| ASI drug (ref=baseline) | ||||||
| Baseline | ||||||
| 6-month | −0.02* | −0.04 | −0.00 | −0.04* | −0.08 | −0.01 |
| 12-month | −0.02* | −0.04 | −0.00 | −0.02 | −0.06 | 0.01 |
| 18-month | −0.02* | −0.04 | −0.00 | −0.02 | −0.01 | 0.06 |
| Peak Density (ref=baseline) |
||||||
| Baseline | ||||||
| 6-month | −8.9*** | −11.5 | −6.4 | −8.0*** | −12.1 | −3.9 |
| 12-month | −9.6*** | −12.1 | −7.0 | −7.3** | −11.4 | −3.1 |
| 18-month | −7.6*** | −10.4 | −4.9 | −5.5* | −10.0 | −0.9 |
|
| ||||||
p< 0.10;
p < 0.05 ;
p < 0.01 ;
p < 0.001
models control for age, sex, education and marital status.
For individuals with high psychiatric severity the pattern and magnitude of outcomes over time were similar. Improvements between baseline and follow up time points were noted for ASI alcohol, ASI drug and peak density measures. However, even though the coefficients were similar to those for individuals with low psychiatric severity there were differences in the significance levels. Comparison of baseline ASI drug scores with follow-up time points was significant for 6-months but not for 12 and 18 months. Comparison of baseline ASI alcohol scores with follow-up time point was significant at 18 months but only statistical trends at 6 and 12 months (p<.10). The lower significance levels for the high psychiatric severity group appeared to largely be a result of lower statistical power for detecting differences. Only the measure of peak density, which assessed a 6-month time period, showed significant reductions at follow-up for both the low and high psychiatric severity groups.
Longitudinal relationships between motivation (costs and benefits of sobriety) and substance use outcomes were examined using lagged GEE models separately for low and high psychiatric severity groups (Table 4). For participants with low psychiatric severity, increases in costs and decreases in benefits were associated with higher alcohol and drug severity and use measures. However, for participants with high psychiatric severity only costs predicted outcomes and only for ASI alcohol severity and peak density, not ASI drug severity. Because these analyses were conducted separately for low and high psychiatric severity and the N for high severity was lower, there was lower statistical power to detect significant differences within the high severity group.
Table 4.
Lagged generalized estimating equation (GEE) models of costs and benefits predicting ASI outcomes and peak density, by psychiatric severity~
|
|
|||||||
|---|---|---|---|---|---|---|---|
| Low psych severity | High psych severity | ||||||
|
|
|||||||
| Coefficient | 95% CI | Coefficient | 95% CI | P value interaction | |||
|
psych severity by
costs/benefits |
|||||||
|
|
|||||||
| ASI alcohol | |||||||
| Costs | 0.03*** | 0.02 | 0.05 | 0.07*** | 0.04 | 0.11 | 0.04 |
| Benefits | −0.02* | −0.03 | −0.01 | −0.00 | −0.05 | 0.05 | ns |
| ASI drug | |||||||
| Costs | 0.02*** | 0.01 | 0.03 | 0.01 | −0.00 | 0.03 | ns |
| Benefits | −0.01* | −0.02 | −0.00 | −0.00 | −0.03 | 0.01 | ns |
| Peak Density | |||||||
| Costs | 3.2** | 1.8 | 4.6 | 3.3*** | 1.5 | 5.2 | ns |
| Benefits | −1.5* | −2.5 | −0.4 | −2.0 | −4.5 | 0.5 | ns |
|
| |||||||
models control for age, sex, education and marital status.
p < 0.05 ;
p < 0.01 ;
p < 0.001
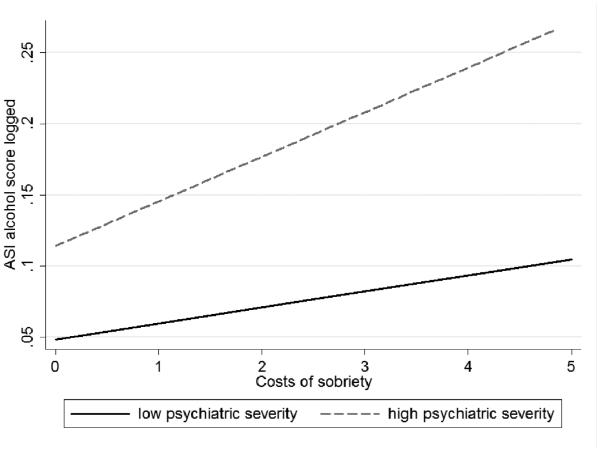
In order to formally test whether coefficients differed significantly between low and high psychiatric severity the samples were combined and main and interactive effects were calculated (Table 4). These analyses showed psychiatric severity interacted with costs as a predictor of alcohol outcome. Figure 2 depicts this relationship. For participants with high psychiatric severity, increases in costs over time were associated with increased severity of alcohol problems and the slope for this group was found to be significantly steeper than for the low severity group. No other interactions were found to be significant.
Figure 2.
Interactive Effects of Psychiatric Severity and Costs of Sobriety on ASI Alcohol Outcome.
Discussion
Study findings constitute a number of distinct contributions to the alcohol and drug literature. First, results represent one of very few studies examining psychiatric severity from a longitudinal perspective rather than at treatment entry. Second, it represents one of the first to examine the impact of psychiatric severity outside the context of formal treatment settings (i.e., sober living houses). Third, it assesses motivation over time. Typically, motivation is assessed at treatment entry in terms of desire to stop substance use. Our study assessed it over the course of 18 months and included assessment of motivation to maintain sobriety once abstinent, a topic largely ignored in the addiction treatment literature. Finally, the study is one of the first to assess how motivation and psychiatric severity interact to impact alcohol and drug outcome. Each of these issues is discussed below along with recommendations for operators of SLHs.
Psychiatric Severity in Sober Living Houses
There were striking differences between participants with high versus low psychiatric severity. Comparisons within time points showed persons with more severe psychiatric problems had higher alcohol and drug severity on ASI scales. Although comparisons of peak density between high and low psychiatric severity groups did not reach significance, the mean peak density of substance use was higher at each time point for individuals in the high psychiatric group. Part of the reason for lack of more robust findings could be that peak density measures a 6-month period of time whereas our measure of psychiatric symptoms, the Brief Symptom Inventory, only measures symptoms the past two weeks. There may have been stronger findings for comparisons of the ASI alcohol and drug scales between psychiatric severity groups because the ASI measures the past 30 days.
Despite higher severity of alcohol and drug problems among the high psychiatric group there was evidence that they made improvements in their substance use between baseline and follow-up time points. The finding of fewer significant improvements relative to the low psychiatric severity group may be due to lower statistical power to detect differences. GEE analyses assessing within group improvements resulted in similar coefficients.
The finding that alcohol and drug problems were more severe among the high psychiatric group is consistent with a variety of reports in the alcohol and drug treatment literature (Broome, Flynn, & Simpson, 1999; McLellan, et al., 1983; Ritsher, McKeller, Finney, Otilingam, & Moos, 2002). However, our study adds to the literature by accounting for psychiatric symptoms over time rather than at treatment entry only. Study findings also constitute a unique contribution in that most studies have been conducted on samples of persons receiving formal treatment. Polcin and Henderson (2008) have described how long-term services that support ongoing recovery, such as SLHs, are gaining increased recognition in the substance abuse literature, but have receive limited attention in terms of formal research. Our study is the first to examine the impact of psychiatric severity in SLHs.
Our finding that persons with high psychiatric severity have more problems with alcohol and drug use is consistent with a study examining perceptions of SLH managers (Polcin, Henderson, Trocki, Evans, & Wittman, 2012). They noted that persons with more significant psychiatric problems had difficulty maximizing the benefits of interpersonal support in the SLH environment. However, our findings were different from a study of psychiatric severity among residents in Oxford Houses (Majer et al., 2008). Similar to SLHs, Oxford Houses are peer focused, residentially based facilities for persons with alcohol and drug problems. Majer et al (2008) did not find alcohol and drug differences by level of psychiatric severity. However, they used the Addiction Severity Index (ASI) Psychiatric Severity Scale as a measure of psychiatric severity, which has far fewer items than the measure we used, the GSI score from the Brief Symptom Inventory. There are no subscales on the ASI Psychiatric Scale, while there are 10 clinical scales on the Brief Symptom Inventory used to generate the GSI score.
The other significant difference is the Oxford house study did not use an “intent to treat” study design, where individuals are interviewed at entry into the house and then tracked over time. Rather, they enrolled individuals who had been residing at an Oxford House between one day and 122 months and then interviewed that sample at four-month intervals. There could be significant variability in the impact of psychiatric severity among individuals with these widely varying lengths of time in the residence.
Interaction of Motivation and Psychiatric Severity
In previous analyses of the data used in our study (Korcha, et al., 2011) we found motivation, measured as perceived costs and benefits of sobriety on the ADCQ, had a strong relationship with alcohol and drug use. Specifically, low costs and high benefits were significant predictors of abstinence over an 18-month period. However, the analyses performed here suggest that perceived benefits of sobriety primarily impact individuals with low psychiatric severity. We found no effect of benefits for the high psychiatric severity group. These findings suggest that interventions designed to enhance perceptions about the benefits of abstinence might be best directed toward persons with lower psychiatric severity.
Study findings suggest interventions designed to decrease perceived costs of sobriety might be useful for both groups. Our assessment of the impact of costs on substance use showed main effects for both high and low levels of psychiatric symptoms. However, for individuals with high psychiatric severity we found perceived consequences only impacted measures that targeted or included assessments of drinking (ASI alcohol scale and peak density), not drugs (ASI drug scale). Interventions targeting costs of sobriety for this group might be best directed toward those with primarily drinking problems. Additional support for this recommendation can be seen in the interactive effect we found: costs were significantly more impactful on alcohol severity outcome for the high severity group. Therefore, helping residents in SLHs address the challenges (i.e., perceived costs) they face in recovery is important for all residents, but it appears to be especially critical for those with high psychiatric severity. Creating a sense of confidence that they will be able to manage the challenges they encounter in sobriety is critically important.
Implications for Sober Living Houses
Despite the problems associated with high psychiatric severity there was limited involvement in outside mental health services. Previous analyses of the data used for this study showed only 12% of the residents who entered the sober living residence received any outpatient psychotherapy between baseline and 6 months (Polcin & Henderson, 2008). About 3o% reported receiving some type of psychiatric medication during this period. More efforts could be directed toward coordination with these services.
There may be additional considerations for on-site services as well. SLHs are not licensed to deliver services to residents. However, there is no reason they could not contract with outside professionals to come on-site and provide interventions that help manage psychiatric symptoms such as anxiety, depression, and trauma. Motivational interviewing (MI) interventions that address the “pros and cons” of substance use would seem to a good way to address and impact perceived costs and benefits. Typically, MI is delivered as a brief intervention at the beginning of treatment. However, novel methods of conducting it over longer periods of time (e.g., Polcin et al., in press) might be a way to impact motivation to maintain sobriety.
Another idea would be to generate peer support interventions for residents suffering from these types of disorders. Peers could help each other by providing encouragement, suggestions, and guidance through periods of crises. Additionally, house managers could be given skills training to assist those residents with psychiatric problems to find outside services and support.
More research is needed to assess whether there are types of psychiatric disorders that suggest SLHs are not an appropriate referral source. For example, some individuals with substance use disorders who also have more serious types of mental illness may do better in houses specifically designed for this population. On the other hand, it should be noted that the high psychiatric severity group made significant improvements in substance use despite the existence of their symptoms, demonstrating that SLHs can be a viable option for a variety of individuals.
Limitations
There are a number of limitations that bear noting. First, the parent study did not include a control or comparison group, so improvements seen over time could have been influenced by extraneous factors other than residence in the SLH. To some extent this concern is mitigated by previous findings showing variables central to the philosophy of recovery in these settings (e.g., 12-step involvement and social networks supportive of recovery) were associated with outcome (Polcin et al, 2010). Another limitation is potential bias associated with self-report data. Finally, the research interviewers were not blind to participants or results from their previous interview (e.g., responses to questions assessing psychiatric problems) and there is a possibility that their prior knowledge about participants may have potentially influence their ratings. However, all interviewers received extensive training on research instruments and standard research practices.
Acknowledgements
This work was supported by the National Institute on Drug Abuse grant R03 DA034961 and the National Association of Alcohol Abuse and Alcoholism grant R01AA014030.
Footnotes
In Press: Substance Use and Misuse
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. 4th American Psychiatric Publishing, Inc; Washington, DC: 2000. [Google Scholar]
- Broome KM, Flynn PM, Simpson DD. Psychiatric comorbidity measures as predictors of retention in drug abuse treatment programs. Health Services Research. 1999;34(3):791–806. [PMC free article] [PubMed] [Google Scholar]
- Carey KB. Substance use reduction in the context of outpatient psychiatric treatment: a collaborative, motivational, harm reduction approach. Community Mental Health Journal. 1996;32(3):291–306. doi: 10.1007/BF02249430. [DOI] [PubMed] [Google Scholar]
- Clark HW, Power AK, Le Fauve CE, Lopez EI. Policy and practice implications of epidemiological surveys on co-occurring mental and substance use disorders. J Subst Abuse Treat. 2008;34(1):3–13. doi: 10.1016/j.jsat.2006.12.032. doi: S0740-5472(07)00092-X [pii] 10.1016/j.jsat.2006.12.032. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Sobell LC, Gavin DR, Sobell MB, Breslin FC. Assessing motivation for change: preliminary development and evaluation of a scale measuring the costs and benefits of changing alcohol and drug use. Psychology of Addictive Behaviors. 1997;11(2):107–114. [Google Scholar]
- Cunningham JA, Sobell LC, Gavin DR, Sobell MB, Breslin FC. Assessing motivation for change: Preliminary development and evaluation of a scale measuring the costs and benefits of changing alcohol or drug use. Psychology of Addictive Behaviors. 1997;11(2):107–114. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13(3):595–605. [PubMed] [Google Scholar]
- DiClemente CC, Nidecker M, Bellack AS. Motivation and the stages of change among individuals with severe mental illness and substance abuse disorders. Journal of substance abuse treatment. 2008;34(1):25–35. doi: 10.1016/j.jsat.2006.12.034. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. The American Journal on Addictions. 2004;13(2):103–119. doi: 10.1080/10550490490435777. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Heagerty P, Liang K-Y, Zeger SL. Analysis of Longitudinal Data. 2nd Oxford University Press; Oxford, UK: 2002. [Google Scholar]
- Gerstein DR, Johnson RA, Harwood HJ, Fountain D, Sutter N, Malloy KM. Evaluating Recovery Services: The California drug and alcohol treatment assessment. California Department of Alcohol And Drug Problems; Sacramento, CA: 1994. (Contract No. 92-001100) (pp. 90) [Google Scholar]
- Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse MP, Ang A, Rawson RA. Psychopathology in methamphetamine-dependent adults 3 years after treatment. Drug and Alcohol Review. 2010;29(1):12–20. doi: 10.1111/j.1465-3362.2009.00081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havassy BE, Alvidrez J, Owen KK. Comparisons of patients with comorbid psychiatric and substance use disorders: implications for treatment and service delivery. American Journal of Psychiatry. 2004;161(1):139–145. doi: 10.1176/appi.ajp.161.1.139. [DOI] [PubMed] [Google Scholar]
- Janis IL, Mann L. Decision making: A psychological analysis of conflict, choice and commitment. Free Press; New York: 1977. [Google Scholar]
- Korcha RA, Polcin DL, Bond JC, Lapp WM, Galloway G. Substance use and motivation: a longitudinal perspective. The American Journal of Drug and Alcohol Abuse. 2011;37(1):48–53. doi: 10.3109/00952990.2010.535583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majer JM, Jason LA, North CS, Ferrari JR, Porter NS, Olson B, Davis M, Aase D, Molloy JP. A longitudinal analysis of psychiatric severity upon outcomes among substance abusers residing in self-help settings. American Journal of Community Psychology. 2008;42(1-2):145–152. doi: 10.1007/s10464-008-9190-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP, Druley KA. Predicting response to alcohol and drug abuse treatments: role of psychiatric severity. Archives of General Psychiatry. 1983;40(6):620–625. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- McNulty J, Kouimtsidis C. Outcomes of treatment intervention in drug abuse. Current Opinions in Psychiatry. 2001;14(3):201–205. [Google Scholar]
- Muthén LK, Muthén BO. Mplus version 7.1. Muthén & Muthén; Los Angeles, CA: 2013. [Google Scholar]
- Polcin DL, Bond J, Korcha R, Nayak MB, Galloway GP, Evans K. Randomized trial of intensive Motivational Interviewing for methamphetamine dependence. Journal of Addictive Diseases. doi: 10.1080/10550887.2014.950029. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Henderson D, Trocki K, Evans K, Wittman F. Community context of Sober Living Houses. Addiction Research and Theory. 2012;20(6):480–491. doi: 10.3109/16066359.2012.665967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Henderson DM. A clean and sober place to live: philosophy, structure, and purported therapeutic factors in sober living houses. Journal of Psychoactive Drugs. 2008;40(2):153–159. doi: 10.1080/02791072.2008.10400625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Bond J, Galloway G. Eighteen-month outcomes for clients receiving combined outpatient treatment and sober living houses. Journal of Substance Abuse. 2010;15(5):352–366. doi: 10.3109/14659890903531279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: treatment main effects and matching effects on drinking during treatment. Journal of Studies on Alcohol. 1998;59(6):631–639. doi: 10.15288/jsa.1998.59.631. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, McKeller JD, Finney JW, Otilingam PG, Moos RH. Psychiatric comorbidity, continuing care and mutual help as predictors of five-year remission from substance use disorders. Journal of Studies on Alcohol. 2002;63(6):709–715. doi: 10.15288/jsa.2002.63.709. [DOI] [PubMed] [Google Scholar]
- Wittman FD, Polcin DL. The evolution of peer run sober housing as a recovery resource for California communities. International Journal of Self Help and Self Care. doi: 10.2190/SH.8.2.c. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Pan JJ, Blazer DG, Tai B, Brooner RK, Stitzer ML, Blaine JD. The construct and measurement equivalence of cocaine and opioid dependences: a National Drug Abuse Treatment Clinical Trials Network (CTN) study. Drug and alcohol dependence. 2009;103(3):114–123. doi: 10.1016/j.drugalcdep.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang AY, Harmon JA, Werkner J, McCormick RA. Impacts of motivation for change on the severity of alcohol use by patients with severe and persistent mental illness. Journal of Studies on Alcohol and Drugs. 2004;65(3):392. doi: 10.15288/jsa.2004.65.392. [DOI] [PubMed] [Google Scholar]