Abstract
Background
The rampant tobacco abuse is escalating the Indian health sector towards a future overburdened with high prevalence of cancer and potentially malignant conditions. Thus manifestations of tobacco abuse have become a widely recognized but poorly tackled public health issue. To understand the same, a study was conducted in a dental college of Bhopal, India.
Methodology
A hospital based cross sectional study was done over a period of 1.5 years. Patients giving history of deleterious habits were included in the study. The form of tobacco/areca nut used, duration and frequency of usage and awareness regarding their ill-effects were recorded. All documented data was subjected to statistical analysis using chi-square test.
Results
Out of 2033 individuals studied 21% were below the age of 25 years, 53% in 26–50 years, 20% in 51–75 years and 6% above 76 years of age with 85% being males. 67% used smokeless form, 21% smoked and 12% used tobacco in both smokeless and smoking form. 58% of the individuals had tobacco associated lesions, of which oral submucous fibrosis (OSMF) was the most prevalent. The relation between duration and frequency of abuse and occurrence of lesion was found to be statistically significant (p < 0.05).
Conclusion
The smokeless form was most widely abused in this part of the country especially the younger population. OSMF, a premalignant condition with debilitating effects on the lifestyle, was the most prevalent lesion associated with tobacco use. These findings call for early and aggressive intervention methods be put into action.
Keywords: Smokeless tobacco, Oral submucous fibrosis, Oral leukoplakia
1. Introduction
The World Health Organization (WHO) predicts that India will have an accelerated rise in deaths attributable to tobacco in the first two decades of the present century. Tobacco addiction will hasten deaths in the productive life of young adults due to habits acquired in youth. India occupies a very special place in the world tobacco map. As the second most populous country in the world, India's share of the global burden of tobacco-induced disease and death is substantial.1
There are several forms in which tobacco is consumed in India. Among smokers, it is consumed in the form of cigarettes, and other indigenous forms like bidis, chuttas, chilam, hooklis, hookah, which are to name a few. The smokeless form of tobacco include khaini, Guthka, maipuri tobacco, mawa, snuff where tobacco is used in confluence with several other substances like areca nut, lime, catechu and flavoring agents.2
Regular use of these lead to manifestation of oral cancer and potentially malignant conditions and lesions.3 To add to this, in India 180 million tobacco users are present and 8 lakh deaths per year attributed to tobacco use have been reported.4 The tobacco associated lesions with serious outcome are oral cancer, leukoplakia, oral submucous fibrosis, erythroplakia and carcinoma in situ.2 Several studies have shown the prevalence of leukoplakia in India to be 0.02–5.2%.5,6 Surveys about tobacco use have been carried out in different parts of the world which have yielded results with immense geographic variation. Reliable prevalence data on tobacco use and their manifestation in India is scarce. Socio-demographic determinants influencing tobacco use is poorly understood which propelled us to conduct this study. The study was conducted to estimate the prevalence of tobacco users reporting to the OPD of a dental college in Bhopal. The objectives of this study were to record the demographic factors of tobacco usage, types of tobacco used and associated lesions with frequency/duration of substance abused and relate the reasons for the abuse.
2. Materials and methods
A cross sectional study was conducted over a period of 1.5 years where 56,472 patients reported to the OPD, where those with the habit of tobacco and areca nut chewing and tobacco smoking were included (2033). The demographic data of each patient and detailed history were recorded and chair side examination of the patients was done. The individuals included in the study were segregated into categories according to age, gender, form of tobacco consumed, duration and frequency of tobacco usage, presence and type of oral lesions associated with tobacco usage. All the data were documented, tabulated and analyzed statistically using Chi-square test and Correlation Coefficient calculated.
3. Results
The total number of individuals included in this study was 2033. The individuals were categorized into 4 age groups: group I: <25 years, group II: 26–50 years, group III: 51–75 years and group IV: 76–100 years. 21% (427) of patients belonged to group I, 53% (1078) of the patients belonged to the group II, 20% (406) to group III and 6% (122) to group IV (Fig. 1). 85% (1728) of the patients were males and 15% (305) were females. 67% (1374) of the patients used smokeless form of tobacco, 21% (426) smoke form and 12% (233) of the patients used tobacco in both smokeless and smoking form (Fig. 2). Out of the total number individuals using tobacco, it was found that maximum individuals i.e. 29% (598) preferred using “Guthka” while areca nut alone was used by 7% (143) of the individuals. Smokeless tobacco products other than Guthka were consumed by 31% (638) of the study population. The form of tobacco preferred in both the genders have been shown in Table 1. 58% (1189) of the patients presented with oral lesions associated strongly with the use of tobacco and rest (844) were lesion-free. It was found that the appearance of lesion was influenced by duration of tobacco use and with the increase in duration of tobacco usage, the occurrence of tobacco associated lesions have significantly increased which was confirmed statistically using Chi square test (p < 0.05). On the basis of frequency of habits, subjects were stratified into following groups: group A: <5 times/day, group B: 5–10 times/day, group C: 11–15 times/day, group D: 16–20 times/day, group E: 21–25 times/day and group F: 25–30 times/day. On assessing the frequency of appearance of lesion to frequency of tobacco usage, it was found that in Group A 47%, in group B 68.5%, in group C 69.6%, in group D 96 80% and in group E and F 100% of individuals had lesions (Table 2). It was observed that with increase in the frequency of daily tobacco consumption, there was a rise in the incidence of associated lesions in the oral cavity which was depicted using correlation coefficient of 0.97 (Fig. 3). Amongst the individuals who had tobacco–induced lesions, it was found that oral submucous fibrosis (OSMF) was the most prevalent lesion being present in 16.3% subjects. This was closely followed by leukoplakia (13.1%). The most striking finding was the relatively high prevalence of oral cancer (1.6%) in tobacco using patients reporting to the dental OPD. 56% of the individuals stated that they resorted to these habits to alleviate stress, 23.7% blamed it on peer pressure, 11.7% to subside tooth ache and 9.2% used it to prevent halitosis. Chi square test revealed that the awareness of ill effects of tobacco and areca nut was more in younger age group which was statistically significant (p < 0.05).
Fig. 1.

Pie distribution of age group of tobacco users.
Fig. 2.
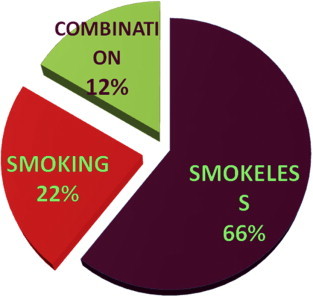
Distribution of form of tobacco used in the region.
Table 1.
Distribution of tobacco users according to forms of tobacco in the 2 gender groups.
| Forms | Male (85%) | Female (15%) |
|---|---|---|
| Areca nut | 6% | 0.7% |
| Guthka | 26.6% | 2.7% |
| Other smokeless forms | 20.7% | 10.6% |
| Smoking | 21.06% | 1.3% |
| Guthka + smoking | 8.3% | – |
| Areca nut + smoking | 2.03% | – |
| Other smokeless + smoking | 0.6% | – |
Table 2.
Describes the distribution of lesion free individuals and those afflicted with lesions in relation to habit frequency.
| Frequency (times/day) | <5 | 5–10 | 11–15 | 16–20 | 21–25 | 26–30 |
|---|---|---|---|---|---|---|
| With lesions [n (%)] | 511 (47) | 418 (69) | 115 (69) | 77 (80) | 49 (100) | 19 (100) |
| Without lesions [n (%)] | 583 (53) | 192 (31) | 50 (31) | 19 (20) | 0 | 0 |
| Total | 1094 | 610 | 165 | 96 | 49 | 19 |
Fig. 3.
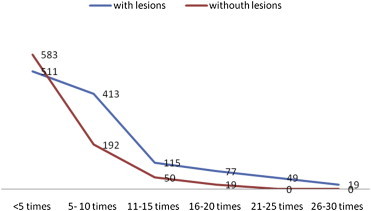
Graph depicting the relation between frequency of tobacco usage with occurrence of lesions.
4. Discussion
The prevalence of tobacco and areca-nut users reporting to the OPD was 3.6% (2033/56,472). Through this survey we put forward an estimate of the demographic aspects of tobacco usage and extensive exploration of the tobacco-associated disease burden.
Tobacco contains several deleterious compounds, a large group of which have been found to be carcinogenic.1 Nicotine is the addictive alkaloid component. This is accompanied by several potent carcinogens like polycyclic aromatic hydrocarbons, tobacco specific nitrosamines,2 heterocyclic amines, aldehydes, inorganic compounds, and miscellaneous organic chemicals (e.g., styrene, benzene, and vinyl chloride) which are classified as Group 1 carcinogens by the International Agency for Research on Cancer.7 The carcinogen present in the smokeless form of tobacco is nitrosamines especially tobacco specific vareity.8 In India areca nut/betel nut is another psychoactive substance, which is frequently abused. The use of betel nut itself or along with tobacco results in several mucosal lesions. Areca nut also contains several carcinogenic components like tannins, some polyphenols like safrole, hydroxychavicol, and catechins, and most of the alkaloids.8–10 The frequently encountered oral lesions associated with tobacco abuse include the various forms of leukoplakia, oral submucous fibrosis, erythroplakia, tobacco chewer's keratosis, smoking induced palatal lesions and finally oral cancer.
This study revealed that the age group most frequently involved in the practice of tobacco usage was between 25 and 50 years (53%), followed by individuals of age group of <25 years (21%). This was concurrent with the findings of Keluskar and Kale4 and of Desai et al,11 where most of the patients with habit of tobacco belonged to the age groups of 20–60 years and 21–50 years respectively. This finding was of grave concern as it was an indicator of the productive population and the youth falling prey to the vicious habit. There are several factors which could be thought to influence the youth to make this choice which could include idolization of close family members of the older influential age group as well as media personalities. Easy availability of the tobacco products and economic prices could be catalysts in establishment of such habits.
We found a clear cut male predominance (85%) of the subjects which was consistent with those in studies carried out by Rani et al12 (2003) and Saraswathi et al13 (2006). However this data might not be completely indicative of the male:female ratio of tobacco users. Social prejudice more so in rural areas could inhibit females from availing dental treatment. This puts them at higher risks of developing oral lesions and greater potential for these lesions to undergo malignant transformation.
It was found the smokeless form of tobacco was most preferred in this region (67%) followed by 21% of smoking, which was in contrast to the findings of tobacco using population in the state of Uttar Pradesh who were smokers.1 Guthka was the most frequently used smokeless form of tobacco in the present study (29%). This was comparable to the findings reported by the GATS India report, which stated that 27% of the men in Madhya Pradesh used “Guthka”.14 The female population was found to be almost exclusively chewers. The product used commonly by the female population of tobacco users was “zarda” (90%), a smokeless form of tobacco used frequently by the rural and lower economic strata. These data give us a peek at the popular usage of smokeless tobacco products like “Guthka”, where it seems the addition of the flavoring agents make the taste and essence of these products more favorable, have played a key role in popularizing the use of “Guthka” especially in the younger population. The finding that the female population using smokeless tobacco products usually belonged to the lower economic strata pointed a finger at the role of education and awareness regarding tobacco usage was unable to reach the grass root levels.
A myriad of manifestations ranging from extrinsic stains to invasion of the mucosa represent the injurious effects of these agents. The potentially malignant states are of prime concern as they present with increased risks of malignant transformations at accelerated rates when the patients continue to use tobacco even after development of the lesions. In this study we found that 58% of the subjects had developed tobacco related lesions. The most commonly encountered oral lesion was found to be Oral Submucous Fibrosis (OSMF), affecting 16.3%. Although it is predominantly widespread in the South-East Asian subcontinent, its incidence has gained notice in the East African countries as well.15 The overall prevalence of OSMF in India is 0.03–3.2%.3,5 The relative risk of malignant transformation among individuals with OSMF was found to be 397.3 times, reason being the generalized epithelial atrophy, which increases the penetration of carcinogens into the subepithelial layers.1
This was followed by 13.10% of the individuals suffering from leukoplakia amongst whom 74% used smokeless tobacco followed by users of both smoking and smokeless tobacco products (18%) and the rest were smokers. In India, leukoplakia is almost always tobacco induced and its prevalence ranges from 0.2 to 5.2%.1,3,5,6 Leukoplakia has a wide variety of clinical presentation varying greatly with site and habits practiced. In smokers commonly speckled leukoplakia is seen occurring in the commisures and in chewers homogenous leukoplakia is usually associated at the site of quid placement.2 These lesions maybe persistent, regress spontaneously or progress to result in oral cancer. The worldwide rate of malignant transformation of leukoplakia is 3.6% while in Indian studies these rates varied from 0.13% to 10%. Speckled leukoplakia is the most severe form of leukoplakia with maximum risks of developing into oral cancers.1 In smokers the most common oral lesion was found to be smoker's palate. It is a common lesion, usually asymptomatic and has no significant risks of malignant transformation.
1.6% of the subjects were affected by oral cancer, the commonest being oral squamous cell carcinoma. In our study maximum of individuals suffering from oral cancer belonged to age group of 21–30 years and 72.2% were males. 87.7% of these patients used smokeless form of tobacco namely Guthka and areca nut while rest were smokers. Paradoxically majority of such individuals had used tobacco and their products for less than 10 years and with a frequency of about 5–10 times per day. The most commonly involved sites were vestibular and buccal mucosae. A thorough investigation of other risk factors like nutritional status, trauma, viruses and genetic mutations as co-risk factors would definitely shed more light on process of carcinogenesis.
56% attributed their habit alleviation from stressful situations as their reason while the second common reason was peer pressure.
5. Conclusion
Old habits die hard and abstinence from these injurious agents will require strong motivation. Potentially malignant disorders are on the rise in central India due to the easy availability of these products. Though oral cancer had been considered as an age dependant disease, increasing evidence points to a change in trend. As responsible health care providers we not only detect it early but help in spreading awareness and thus promote prevention.
Conflicts of interest
All authors have none to declare.
References
- 1.Reddy K.S., Gupta P.C. Ministry Health & Fam Welf (India); New Delhi: 25 November 2004. (Report on Tobacco Control). [Google Scholar]
- 2.Mehta F.S., Hammer J.E. Basic Dental Research Unit; Bombay: 1993. Tobacco-Related Oral Mucosal Lesions and Conditions In India. [Google Scholar]
- 3.Murti, Bhonsle, Pindborg Johnson, Ranasinghe, Warnakulasuriya, Mehta Betel-quid and areca-nut chewing and some areca-nut derived nitrosamines. IARC Monogr Eval Carcinog Risks Hum. 2004;85:1–334. [PMC free article] [PubMed] [Google Scholar]
- 4.Keluskar V., Kale A. An epidemiological study for evaluation of oral precancerous lesions, conditions and oral cancer among Belgaum population with tobacco habits. Biosci Biotech Res Comm. 2010;3(1):50–54. [Google Scholar]
- 5.Mehta F.S., Gupta P.C., Daftary D.K., Pindborg J.J., Choksi S.K. An epidemiological study of oral cancer and precancerous conditions among 101, 761 villagers in Maharashtra, India. Intermit J Cancer. 1972;10:134–141. doi: 10.1002/ijc.2910100118. [DOI] [PubMed] [Google Scholar]
- 6.Pindborg J.J., Chavla T.N., Mishra R.K., Nagpaul R.K., Gupta V.K. Frequency of oral carcinoma, leukokeratosis, leukoedema, submucous fibrosis and lichen planus in 10,000 Indians in Lucknow, Uttar Pradesh, India Report. J Dent Res. 1965;44:625. doi: 10.1177/00220345650440032901. [DOI] [PubMed] [Google Scholar]
- 7.Phillips D.H. DNA adducts in human tissues: biomarkers of exposure to carcinogens in tobacco smoke. Environ Health Persp. 1996;104(3):453–458. doi: 10.1289/ehp.96104s3453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hecht S.S. Tobacco carcinogens, their biomarkers and tobacco induced cancer. Nat Rev Cancer. 2003;3:733–744. doi: 10.1038/nrc1190. [DOI] [PubMed] [Google Scholar]
- 9.Blank M., Deshpande L., Balster R.L. Availability and characteristics of betel products in the US. J Psychoact Drugs. 2008;40(3):309–313. doi: 10.1080/02791072.2008.10400646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta P.C., Ray C.S. Epidemiology of betel quid usage. Ann Acad Med Singapore. 2004;33(suppl l):31S–36S. [PubMed] [Google Scholar]
- 11.Desai V., Gill R.K., Sharma R. Prevalence of habit of tobacco and its deleterious effects in general population of district Jaipur, Rajasthan. J Indian Aca Oral Med Radiol. 2012;24(2):113–116. [Google Scholar]
- 12.Rani M., Bonu S., Jha P., Ngyuen S.N., Jamjoum L. Tobacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tob Control. 2003;12:e4 2. doi: 10.1136/tc.12.4.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saraswathi T.R., Ranganathan K., Shanmugam S., Ramesh S., Narsimhan P.D., Gunaseelan R. Prevalence of oral lesion in relation to habits-cross sectional study in South India. Ind J Dent Res. 2006;17(3):121–125. doi: 10.4103/0970-9290.29877. [DOI] [PubMed] [Google Scholar]
- 14.Global Adult Tobacco Survey India Report 2009–10. International Institute of Population Sciences; Mumbai: 2010. [Google Scholar]
- 15.Venkataraman B.K. Wolters Kluwer India pvt.ltd; New Delhi: 2013. Diagnostic Oral Medicine. [Google Scholar]


