Abstract
Background
To determine the prevalence and severity of oral submucous fibrosis (OSMF) among habitual gutkha, areca nut and pan chewers of Moradabad, India.
Method
A survey was conducted for a period of one year in east, west, north and south zones of Moradabad district, Uttar Pradesh. One thousand habitual chewers were selected as study participants, using a stratified random sampling technique, between the ages of 11–40 yrs, with a habit of chewing gutkha, areca nut, pan for over a year. A detailed history was recorded and meticulous clinical examination was conducted. Evaluation of taste sensation, hearing, interincisal distance, clinical staging was done in the OSMF patients found amongst habitual chewers. The obtained data was statistically analyzed using an SPSS 16.5 version soft ware.
Results
The prevalence of OSMF was 6.3% (63/1000) and gutkha chewing was the most common abusive habit (42/63) amongst OSMF patients. Stage 1, Stage 2, Stage 3 OSMF was seen in 28, 19 and 16 patients respectively. Restricted mouth opening, altered taste perception and defective hearing was observed in 37/63 (58.7%), 24/63 (38.09%) and 14/63 (22.22%) respectively.
Conclusion
Our study shows a prevalence of 6.3% OSMF among habitual chewers of Moradabad. Prevalence and severity were more in urban and rural patients respectively.
Keywords: Oral submucous fibrosis, Moradabad, Gutkha chewers, Areca nut
1. Introduction
Oral submucous fibrosis (OSMF) is a chronic, progressive, scarring precancerous condition of the oral cavity seen predominantly in the Indian subcontinent and South East Asia.1 In India, the prevalence increased over the past four decades from 0.03% to 6.42%.2,3 Data published earlier reported an estimate of 5 million OSMF patients in India.4 OSMF is seen commonly in males between 20 and 40 yrs age. The common sites involved are buccal mucosa, labial mucosa, retromolar pads, soft palate and floor of the mouth. Rarely fibrotic changes of the pharynx, esophagus and paratubal muscles of eustachian tubes have also been observed. Early features of OSMF include burning sensation, hypersalivation/xerostomia and mucosal blanching with marble like appearance.5 Later on, the mucosa becomes leathery and inelastic with palpable fibrous bands resulting in restricted mouth opening. Eventually, OSMF leads to difficulty in swallowing, speech & hearing defects and defective gustatory sensation.5–7
The pathogenesis of OSMF is multifactorial and enigmatic. The etiological factors implicated are excessive chilly consumption, areca nut chewing, vitamin B complex & iron deficiency, autoimmunity, genetic and environmental factors.5,8,9 However, the most consistent factor identified through epidemiological studies is areca nut consumption in form of quid.5,8,9 Quid is defined as “ a substance, or mixture of substances, placed in the mouth or chewed and remaining in contact with the mucosa, usually containing one or both of the two basic ingredients, tobacco and/or areca nut, in raw or any manufactured or processed form”.10 Areca nut or betel nut is the endosperm of the fruit of Areca catechu. Areca nut contains alkaloids like arecoline, arecaidine, guvacine and guvacoline, flavanoids and copper. The alkaloids stimulate fibroblasts to produce collagen and flavanoids inhibit collagenase, thus decreasing collagen degradation.4 Reasons for using areca nut primarily are attaining euphoria, satiation, thus making the habit, addictive. Areca nut is consumed either alone or in combination with other constituents. Paan or betel quid contains areca nut and slaked lime wrapped in a betel leaf (Piper betel).10 Gutkha is a mixture of powdered areca nut and tobacco, marketed in pre packaged pouches of 5–10 g.4 There is a sudden upsurge in the use of gutkha recently, due to easy availability, attractive colorful packs, longer shelf life and low cost. Babu et al reported that habitual chewing of gutkha/pan masala resulted in the early occurrence of OSMF than areca nut chewing.9,11 The earlier presentation may be due to the synergistic action of nicotine on the cytotoxicity induced by arecoline.12
Though, paan and gutkha chewing are the most common abusive habits of northern India, very few studies were conducted among this population.13,14 The present study was hence conducted to determine and compare the prevalence and severity of OSMF among areca nut, gutkha and pan chewers of the urban and rural population of Moradabad district, in Uttar Pradesh located in North India. The clinical profile and staging of OSMF patients among the study population was also recorded. Association between the severity of OSMF and the various chewing habits was also assessed.
2. Materials and methods
2.1. Study design
2.1.1. Study area
After obtaining consent from the Institutional Review Board, a cross sectional study was conducted in Moradabad district, Uttar Pradesh. It has both rural and urban areas in close proximity. Census of India15 defines an urban area as (a) All statutory places with a municipality, corporation, cantonment board or notified town area committee, etc. (b) A place satisfying the following three criteria simultaneously: i) a minimum population of 5000; ii) at least 75 per cent of male working population engaged in non-agricultural pursuits; and iii) a density of population of at least 400 per sq. km (1000 per sq. mile). Moradabad district has a population of 3,810,983. It has 1793 villages and is bordered by Bijnor district on the north, Badaun district on the south, Rampur district on the east and JP Nagar district on the west.
2.1.2. Sample size & technique
One thousand subjects were selected using a stratified random sampling technique from the rural and urban populations using 3 stage design (Fig. 1). Line listing of the villages and urban areas of Moradabad district was done initially. In the first stage, 4 villages and Moradabad city proper were randomly selected representing rural and urban population respectively. Next stage comprised of selecting 3 colonies from each village and dividing Moradabad city into east, west, north and south zones. Third stage consists of selecting a sampling unit, a colony comprising of 40–50 houses from each village/zone. Dental health care camps were conducted in the rural areas of Moradabad district to attend to the basic dental needs of these patients like restorations of carious teeth, extraction of grossly carious teeth and oral prophylaxis. 125 subjects belonging to each village (rural) and each zone (urban) were selected from sampling unit and dental health care camps.
Fig. 1.
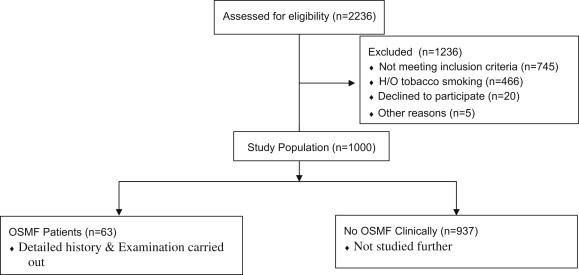
Flow chart of the survey.
2.2. Study population
1000 habitual chewers were selected with the following inclusion and exclusion criteria:
Inclusion criteria:
-
•
habit of chewing areca nut/pan/gutkha for ≥1 year
-
•
frequency of ≥3 units per day
-
•
age group of 11–40 yrs
Exclusion criteria:
-
•
with limitation of mouth opening due to other causes like odontogenic infections and joint disorders
-
•
History of tobacco smoking
The habits, clinical characteristics and severity of OSMF were compared among the rural (Group 1) and urban (Group 2) groups. The study population was not grouped as per the chewing product (areca nut/pan/gutkha) for analysis.
2.3. Data collection technique & tools
All study participants were screened for presence of OSMF by first 2 authors independently. In case of disagreement, a third opinion from last author was taken. The examiners were not blinded to the chewing habit of the study participant.
In the OSMF patients, a detailed history was recorded including duration, type and frequency of the chewing habit. Severity of burning sensation and pain were recorded on a self assessment descriptive rating scale (Absent, mild, moderate and severe). Presence of pain and its severity due to ulcerations, difficulty in mouth opening especially during eating was noted.
Subjective alterations of salivation were recorded. The patient was asked whether he needed frequent sipping of water to swallow food or wet his mouth or whether there was any pooling of saliva in his mouth necessitating frequent spitting. An increase or decrease in the amount of salivation, as per the patient's response, was recorded accordingly in the case proforma. Alterations in taste perceptions were assessed using sweet and salt solution. After mouth rinsing, 2 ml of sucrose solution (0.25% saccharine solution), salty solutions (1% sodium chloride) or water were given to the patient, which he swished in the mouth for 1 min and spitted out. The patient's gustation was considered normal, if both the solutions were identified correctly. Gustatory sensation was considered decreased, if the subject was unable to identify either or none of them. Tuning fork tests were used to assess conductive hearing loss.
Presence of blanching, fibrous bands was noted for each subject. Labial, buccal mucosae, retromolar areas, fauces and soft palate were palpated for the presence of fibrous bands. A thick, vertical, continuous band like structure felt in the buccal mucosa was considered as a fibrous band. Interincisal distance was measured between maxillary and mandibular right/left central incisors with vernier calipers. A distance of >30 mm is considered normal and <30 mm as restricted mouth opening.
Severity of OSMF was assessed as per the clinical staging given below16:
Stage 1: Early OSMF – mild blanching, no restriction of mouth opening or tongue protrusion and burning sensation only on taking spicy food or hot food.
Stage 2: Moderate OSMF – moderate to severe blanching, mouth opening reduced by 33%, burning sensation even in the absence of stimuli, presence of palpable fibrous bands
Stage 3: Severe OSMF – severe burning sensation, interfering with patient's routine, more than 66% reduction of mouth opening, tongue may be fixed (impaired tongue movements), ulcerations on the oral mucosa and the presence of thick palpable fibrous bands.
2.3.1. Data analysis
The obtained data was analyzed using SPSS (Statistical Package for Social Services) 16.5 version. Fisher's exact test was used to compare the frequency of variables among two groups and a probability value of less than 0.05 was considered to be statistically significant.
3. Results
In the 1000 habitual chewers (678 males and 322 females), the prevalence of OSMF was found to be 6.3% (63 out of 1000) with a male to female ratio of 6.88:1 (55:8) (P = 0.0004). Out of 63 OSMF patients, 28 (44.44%) had Stage 1, 19 (30.16%) Stage 2 and 16 (25.40%) had Stage 3 disease. 27 out of the 63 (42.85%) patients were from rural areas and remaining 36 (57.14%) were from urban areas (P = 0.2977). Significant difference (P = 0.0461) was seen in the clinical staging of urban and rural patients, with 22.22% of rural patients being affected by Stage 2 OSMF, where as 31.75% of urban patients were affected by Stage 1 OSMF (Fig. 2). The demographic data of OSMF patients is given in Table 1. The study participants were divided into 6 cohorts (5 yr age interval) to assess the age wise prevalence. Majority of OSMF patients were males in the 36–40 yr age group.
Fig. 2.
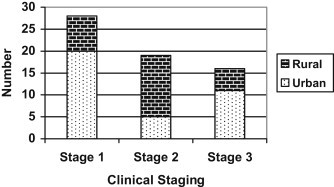
Distribution of clinical staging among urban and rural population.
Table 1.
Demographic data of OSMF patients.
| Group | Distribution (age in yrs) | Males (n = 55) | Females (n = 8) |
|---|---|---|---|
| 1. | 11–15 | 0 | 0 |
| 2. | 16–20 | 5 | 0 |
| 3. | 21–25 | 12 | 2 |
| 4. | 26–30 | 12 | 0 |
| 5. | 31–35 | 8 | 0 |
| 6. | 36–40 | 18 | 6 |
| Total | 55 | 8 |
With regard to chewing habits, out of 63 OSMF patients, 42 (66.66%) were gutkha chewers, 14 (22.22%) were pan chewers and 7 (11.11%) were areca nut chewers. None of the patients had mixed chewing habits. The salient clinical findings of OSMF patients according to the clinical staging are summarized in Table 2. 26 OSMF patients had mouth opening greater than 30 mm and remaining 37 patients had restricted mouth opening. 38.09% (24/63) had altered taste perception and 22.22% (14/63) had defective hearing. Defective hearing was seen more commonly in Stage 1 disease than in later stages.
Table 2.
Clinical signs and symptoms of OSMF patients.
| Stage of OSMF | Taste perception |
Hearing |
Salivation |
Blanching |
Mouth opening (IID) |
Pain during mastication |
Burning sensation |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n | n | n | n | n | n | ||||||||
| Stage1 | Normal | 19 | Normal | 20 | Normal | 17 | Absent | 0 | >30 mm | 16 | Absent | 01 | Absent | 10 |
| n = 28 | Altered | 09 | Defective | 08 | Increased | 02 | Bilateral | 18 | 15–30 mm | 12 | Mild | 04 | Mild | 09 |
| Decreased | 09 | Unilateral | 10 | <15 mm | 0 | Moderate | 07 | Moderate | 06 | |||||
| Severe | 16 | Severe | 03 | |||||||||||
| Stage2 | Normal | 12 | Normal | 15 | Normal | 11 | Absent | 0 | >30 mm | 09 | Absent | 01 | Absent | 04 |
| n = 19 | Altered | 07 | Defective | 04 | Increased | 02 | Bilateral | 13 | 15–30 mm | 10 | Mild | 01 | Mild | 10 |
| Decreased | 06 | Unilateral | 06 | <15 mm | 0 | Moderate | 08 | Moderate | 05 | |||||
| Severe | 09 | Severe | 0 | |||||||||||
| Stage3 | Normal | 08 | Normal | 14 | Normal | 06 | Absent | 0 | >30 mm | 01 | Absent | 0 | Absent | 09 |
| n = 16 | Altered | 08 | Defective | 02 | Increased | 01 | Bilateral | 11 | 15–30 mm | 13 | Mild | 14 | Mild | 02 |
| Decreased | 09 | Unilateral | 05 | <15 mm | 02 | Moderate | 01 | Moderate | 01 | |||||
| Severe | 01 | Severe | 04 | |||||||||||
| Total | Normal | 39 | Normal | 49 | Normal | 34 | Absent | 0 | >30 mm | 26 | Absent | 02 | Absent | 23 |
| n = 63 | Altered | 24 | Defective | 14 | Increased | 05 | Bilateral | 42 | 15–30 mm | 35 | Mild | 19 | Mild | 21 |
| Decreased | 24 | Unilateral | 21 | <15 mm | 02 | Moderate | 16 | Moderate | 12 | |||||
| Severe | 26 | Severe | 07 | |||||||||||
A total 35 out of 63 patients had fibrous bands. Fibrous band locations differed as per the severity of the disease. In Stage 2 patients they were common in buccal mucosa, where as retromolar area had more fibrous bands in Stage 3 patients. Chewing habits of all 3 products according to the clinical stages is given in Table 3. Gutkha consumption is observed to be most prevalent in all stages of the disease. Pan and areca nut chewing was observed in almost equal proportion of OSMF patients in Stages 2 &3.
Table 3.
Chewing habits in various clinical stages of OSMF patients.
| Stage of OSMF | Habit |
||
|---|---|---|---|
| Types | n | Percentage (out of total patients) | |
| Stage 1 (n = 28) | Gutkha | 21 | 33.33 |
| Pan | 6 | 9.52 | |
| Areca nut | 1 | 1.59 | |
| Stage 2 (n = 19) | Gutkha | 10 | 15.87 |
| Pan | 5 | 7.94 | |
| Areca nut | 4 | 6.35 | |
| Stage 3 (n = 16) | Gutkha | 11 | 17.46 |
| Pan | 3 | 4.76 | |
| Areca nut | 2 | 3.17 | |
| Total (n = 63) | Gutkha | 42 | 66.66 |
| Pan | 14 | 22.22 | |
| Areca nut | 07 | 11.11 | |
4. Discussion
Our study found a prevalence of 6.3% OSMF among habitual chewers of the Moradabad population. Previous reports from other states of India and neighboring Asian countries revealed similar prevalence.3,14,17 Stage 1 disease (45%) was common in our study, followed by Stage 2 (30%) and Stage 3 (25%) respectively. Other study from India involving 50 patients, found Grade I disease in 9%, 39% in Grade II and 52% in Grade III OSMF.18 The difference could be due to the fact that ours is a population screening study which revealed majority of patients in asymptomatic stage where as Raina et al studied the OSMF patients attending hospital. There is increased prevalence noted in United States recently due to increase in number of immigrant population from India/Africa.4
Our study reports a variation in clinical staging between urban and rural population. Rural population had Stage 2 commonly, where as urban population had Stage 1 OSMF predominantly (P = 0.0461). Advanced disease among rural population could be due to lack of awareness and paucity of adequate professional care. Other social & environmental factors like nutritional deficiency, deprived socio-economic status, poor education, duration and frequency of areca nut or gutkha chewing habit may act cumulatively on the severity of OSMF.12 However, we did not study the effect of these factors in our study population.
Our study found that OSMF was common in 36–40 yr of both sexes followed by 21–25 yr age group. Previous reports from Indian Subcontinent revealed maximum number of patients in the 21–30 yrs and 21–40 yrs age groups.15,19 Male–female ratio, in our study is 6.9:1, is in accordance with a 6.8:1 ratio in a series of 239 patients reported by Pandya et al and other studies.3,17,20 The higher involvement of males in all studies, reflects their easy access to the abusive habits when compared with females.
Our study involving 63 OSMF patients showed that 66.66% were gutkha users, 22.22% were pan users and only 11.11% were areca nut users. Ranganathan et al reported that 69% of their OSMF patients were gutkha users in a study population of 185.1 However Murti et al in their review stated that 98% of OSMF patients used areca nut either alone or in combination.3 Increase in gutkha chewing over areca nut recently could be due to the easy availability of attractive, tiny, multicolored gutkha packets.
Babu et al and others reported that OSMF presents early in gutkha chewers than betel quid chewers.4,11 This could be due to its tobacco content, absence of betel leaf (has beta carotene which acts as antioxidant) and the increased dry weight of areca nut in gutkha.4 The areca nut grains cause mechanical injury, cytotoxicity of the oral mucosa and produces collagen crosslinks. The cytotoxicity induced by arecholine is augmented by nicotine leading to production of damaged collagen.12
The clinical profile of our patients was similar to other studies from India in most of the features.14,18,21 Pain was present in 62% in our patients. Pain was reported to occur while eating, probably due to surface ulcerations or difficulty in opening the mouth. Our study showed higher percentage of people (38%) with altered taste perception than 11% from previous report.18 This is because, we objectively tested for the taste sensation where as other authors relied on the subjective report. Defective hearing was seen in 22% (14/63) of our OSMF patients. Stage 1 OSMF patients had more hearing defects than other stages. Paramhans et al included OSMF patients with speech and hearing defects as Stage 3 disease.22 Hearing defects are reported to be common in the later stages of the disease.7 However, the early occurrence of defective hearing in our study could be due to other factors like ear infections and wax.
In our study, we observed restricted mouth opening in 58.7%. Kiran Kumar et al in their series found that 6.66%patients had IID >40 mm, 76% had IID between 20 & 40 mm and 17.33% patients had IID less than 20 mm.23 This variation can be explained by the difference in cut off defined for IID in both the studies. The fibrous bands were palpable mostly in the buccal mucosa in Stage 2 OSMF patients and retromolar area in Stage 3 OSMF patients. Ahmad et al also reported that fibrosis was more in the buccal vestibule followed by retromolar area and the soft palate.14 The patterns of blanching or formation of fibrous bands depend largely on the style of chewing (whether it is swallowed or spitted out), duration of addiction and the period of contact of the quid with the specific site. The quid remains in contact for a longer time with the buccal mucosa rather than the retromolar area, soft palate or labial mucosa, causing localized irritation, thus explaining the findings.
5. Conclusion
Our study shows a prevalence of 6.3% OSMF among habitual chewers of Moradabad district. Prevalence was more in urban patients and severity of disease was more in rural population. Gutkha chewing habit was common over pan and areca nut chewing amongst OSMF patients. Our patients had high incidence of taste and hearing alterations. Public health measures to quit areca nut and gutkha use must be strictly imposed.
Conflicts of interest
All authors have none to declare.
References
- 1.Ranganathan K., Devi M.U., Joshua E., Kirankumar K., Saraswati T.R. Oral submucous fibrosis: a case control study in Chennai, South India. J Oral Pathol Med. 2004;33(5):274–277. doi: 10.1111/j.0904-2512.2004.00116.x. [DOI] [PubMed] [Google Scholar]
- 2.Pindborg J.J., Mehta F.S., Gupta P.C., Daftary D.K. Prevalence of oral submucous fibrosis among 50,915 Indian villagers. Br J Cancer. 1968;22(4):646–654. doi: 10.1038/bjc.1968.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hazarey V.K., Erlewad D.M., Mundhe K.A., Ughade S.N. Oral submucous fibrosis: a study of 1000 cases from central India. J Oral Pathol Med. 2007;36(1):12–17. doi: 10.1111/j.1600-0714.2006.00485.x. [DOI] [PubMed] [Google Scholar]
- 4.Shahid R.A. Coming to America: betel nut and oral sub mucous fibrosis. JADA. 2010;141(4):423–428. doi: 10.14219/jada.archive.2010.0194. [DOI] [PubMed] [Google Scholar]
- 5.Rajendran R. Oral submucous fibrosis: etiology, pathogenesis and future research. WHO Bull OMS. 1994;72(6):986–996. [PMC free article] [PubMed] [Google Scholar]
- 6.Eipe Naveen. The chewing of betel quid and oral submucous fibrosis and Anesthesia. Anesth Analg. 2005;100:1210–1213. doi: 10.1213/01.ANE.0000146434.36989.34. [DOI] [PubMed] [Google Scholar]
- 7.Gupta S.C., Singh Mangal, Khanna Sanjay, Jain Sachin. Oral submucous fibrosis with its possible effect on Eustachian tube functions: a tympanometric study. Indian J Otolaryngol Head Neck Surg. 2004;56(3):183–185. doi: 10.1007/BF02974346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murti P.R., Bhonsle R.B., Gupta P.C., Daftary D.K., Pindborg J.J., Mehta F.S. Etiology of oral submucous fibrosis with special reference to the role of areca nut chewing. J Oral Pathol Med. 1995;24(4):145–152. doi: 10.1111/j.1600-0714.1995.tb01156.x. [DOI] [PubMed] [Google Scholar]
- 9.Babu S., Bhat R.V., Kumar P.U. A comparative clinico-pathological study of oral submucous fibrosis in habitual chewers of pan masala and betel quid. Clin Toxicol. 1996;34:317–322. doi: 10.3109/15563659609013796. [DOI] [PubMed] [Google Scholar]
- 10.Zain R.B., Ikeda N., Gupta P.C. Oral mucosal changes related to betel quid, areca nut and tobacco chewing habits: consensus from a workshop held at Kuala Lumpur, Malaysia, November 25–27, 1996. J Oral Pathol Med. 1999;28(1):1–4. doi: 10.1111/j.1600-0714.1999.tb01985.x. [DOI] [PubMed] [Google Scholar]
- 11.Shah N., Sharma P.P. Role of chewing and smoking habits in the etiology of oral submucous fibrosis (OSF): a case control study. J Oral Pathol Med. 1998;27(10):475–479. doi: 10.1111/j.1600-0714.1998.tb01915.x. [DOI] [PubMed] [Google Scholar]
- 12.Javed F., Chotai M., Mehmood A., Almas K. Oral mucosal disorders associated with habitual gutka usage: a review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:857–864. doi: 10.1016/j.tripleo.2009.12.038. [DOI] [PubMed] [Google Scholar]
- 13.Pindborg J.J., Chawla T.N., Misra R.K., Nagpaul R.K., Gupta V.K. Frequency of oral carcinoma, leukoplakia, leukokeratosis, leukoedema, submucous fibrosis and Lichen planus in 10,000 Indians in Lucknow, Uttar Pradesh, India, preliminary report. J Dent Res. 1965;44(3):615. doi: 10.1177/00220345650440032901. [DOI] [PubMed] [Google Scholar]
- 14.Ahmad M.S., Ali S.A., Ali A.S., Chaubey K.K. Epidemiological and etiological study of oral submucous fibrosis among gutkha chewers of Patna, Bihar, India. J Indian Soc Pedod Prev Dent. 2006;24:84–89. doi: 10.4103/0970-4388.26022. [DOI] [PubMed] [Google Scholar]
- 15.censusindiagov.in [Internet]. Census of India, Office of the Registrar General & Census Commissioner, India. [cited 20 Jul 2011]. Available from: http://www.censusindiagov.in.
- 16.Bailoor D.N., Nagesh K.S. 3rd ed. Jaypee Bros; 2005. Fundamentals of Oral Medicine and Radiology; pp. 282–289. [Google Scholar]
- 17.Yang Y.H., Lee H.Y., Tung S., Shieh T.Y. Epidemiological survey of oral submucous fibrosis and leukoplakia in aboriginies of Taiwan. J Oral Pathol Med. 2001;30(4):213–219. doi: 10.1034/j.1600-0714.2001.300404.x. [DOI] [PubMed] [Google Scholar]
- 18.Raina C., Raizada R.M., Chaturvedi V.N., Harinath B.C., Puttewar M.P., Kennedy A.K. Clinical profile and serum beta carotene levels in oral sub mucous fibrosis. J Otolaryngology Head Neck Surgery. 2005;57(3):191–195. doi: 10.1007/BF03008011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar A., Bagewadi A., Keluskar V., Singh M. Efficacy of lycopene in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Oral Endod. 2007;103(2):207–213. doi: 10.1016/j.tripleo.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Pandya S., Chaudhary A.K., Singh M., Mehrotra R. Correlation of histopathological diagnosis with habits and clinical findings in oral sub mucous fibrosis. Head Neck Oncol. 2009;1(1):10. doi: 10.1186/1758-3284-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tupkari J.V., Bhavthankar J.D., Mandale M.S. Oral submucous fibrosis: a study of 101 cases. JIAOMR. 2007;97(02):311–318. [Google Scholar]
- 22.Paramhans D., Mathur R.K., Newaskar V., Shukla S., Sudrania M.K. Role of collagen membrane for reconstruction of buccal defects following fibrotic band excision and coronoidectomy in oral submucous fibrosis. World Artic Ear Nose Throat. 2010;3(1) http://www.waent.org/archives/2010/Vol3-1/20100120-oral-submucous-fibrosis/osmf.htm [Internet] Available from: [Google Scholar]
- 23.Kiran Kumar K., Saraswathi T.R., Ranganathan K., Uma Devi M., Elizabeth J. Oral submucous fibrosis: a clinico-histopathological study in Chennai. Indian J Dent Res. 2007;18:106–111. doi: 10.4103/0970-9290.33785. [DOI] [PubMed] [Google Scholar]


