Abstract
Background
We assessed the contribution of reverse shoulder arthroplasty to overall utilization of primary shoulder arthroplasty, and present age and sex stratified national rates of shoulder arthroplasty. We also assessed contemporary complication rates, mortality, and indications for shoulder arthroplasty, as well as estimates and indications for revision arthroplasty.
Methods
We used the Nationwide Inpatient Samples for 2009–2011 to calculate estimates of shoulder arthroplasty and assessed trends using joinpoint regression.
Results
The cumulative estimated utilization of primary shoulder arthroplasty (total anatomical, hemi, and reverse) increased significantly from 52,397 procedures (95% CI=47,093–57,701) in 2009 to 67,184 cases (95% CI=60,638–73,731) in 2011. Reverse shoulder arthroplasty accounted for 42% of all primary shoulder arthroplasty procedures in 2011. The diagnosis of concomitant diagnosis of osteoarthritis and rotator cuff impairment was found in only 29.8% of reverse shoulder arthroplasty cases. The highest rate of reverse shoulder arthroplasty was in the 75–84 year female sub-group (77; 95% CI=67–87). Revision cases were 8.8% and 8.2% of all shoulder arthroplasties in 2009 and 2011, respectively, and 35% of revision cases were secondary to mechanical complications/loosening while 18% were due to dislocation.
Conclusions
The utilization of primary shoulder arthroplasty significantly increased in just a three year time span, with a major contribution from reverse shoulder arthroplasty in 2011. Indications appear to have expanded as a large percentage of patients did not have rotator cuff pathology. The burden from revision arthroplasties was also substantial and efforts to optimize outcomes and longevity of primary shoulder arthroplasty are needed.
Level of evidence
Epidemiology Study, Database Analysis
Keywords: reverse shoulder arthroplasty, utilization
INTRODUCTION
An increasing utilization of shoulder arthroplasty has been reported in the United States from 1993 to 2008.18,19 This increase in utilization is disproportionate to the increase in population. The recent increase in utilization of total shoulder arthroplasty is likely partly attributable to the approval of reverse shoulder arthroplasty device by the United States Food and Drug Administration (FDA) in 200312. However, national estimates on contribution of reverse shoulder arthroplasty to the overall utilization of shoulder arthroplasty are not available. This data will assist patients, clinicians, and policy makers who are stakeholders in understanding the burden of shoulder arthropathies requiring surgical intervention and perform appropriate resource allocation.
The objectives of our study were to assess the contribution of reverse shoulder arthroplasty to overall utilization of primary shoulder arthroplasty, and present age and sex stratified national rates of shoulder arthroplasty. We also assessed contemporary complication rates, mortality, and indications for shoulder arthroplasty, and estimates and indications for revision arthroplasty.
MATERIALS AND METHODS
Databases
We used the Nationwide Inpatient Sample databases for 2009 through 2011. The Nationwide Inpatient Sample is part of the Healthcare Cost and Utilization Project and is sponsored by the Agency for Healthcare Research and Quality (AHRQ)17. It is the largest all-payer inpatient database available in the United States17. The Nationwide Inpatient Sample used sampling techniques to enable nationally representative estimates17. The Nationwide Inpatient Sample has been validated by an independent contractor and against the National Hospital Discharge Survey31, 43. Further details on the database, sampling techniques, and validation can be found elsewhere17, 31, 43.
Shoulder Arthroplasty Procedures and Associated Diagnoses Codes
There is one principal International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) diagnosis and procedure code for each record in the Nationwide Inpatient Sample. There are up to an additional 24 diagnoses and 14 procedure codes. Each record in the Nationwide Inpatient Sample represents an in-patient admission (and not a unique patient). We used ICD-9-CM procedure codes to ascertain cases of primary total shoulder arthroplasty (81.80), hemiarthroplasty (81.81), and total elbow arthroplasty (81.84). Cases of revision arthroplasty were determined using the ICD-9-CM procedure code of 81.9711. However, this code is not specific to the shoulder and is described as revision arthroplasty of the upper extremity (henceforth referred to as revision arthroplasty). We calculated the number of primary total elbow arthroplasty, wrist, hand, and finger arthroplasty procedures during our study period to validate our assumption that most upper extremity arthroplasty procedures were performed for the shoulder. Reverse shoulder arthroplasty was not assigned an ICD-9-CM procedure code (81.88) until October 1, 20109. Hence, national estimates for reverse shoulder arthroplasty can be calculated for the first time using ICD-9-CM codes for 2011. Although reverse shoulder arthroplasty national estimates were only calculated for the year 2011, we used data from 2010 (after FDA approval of reverse shoulder arthroplasty) when assessing characteristics and complications of reverse shoulder arthroplasty. Since reverse shoulder arthroplasty has a specific ICD-9-CM procedure code for the year 2011, it is reasonable to assume that the code 81.80 was assigned to cases of anatomic total shoulder arthroplasty for this year.
Indications for shoulder arthroplasty were determined using ICD-9-CM diagnosis codes. The diagnosis of osteoarthritis was determined if the record contained a diagnosis code for primary or secondary osteoarthritis of the shoulder or arm. Proximal humeral fractures included fractures of the humeral head, surgical neck, anatomical neck, and greater tuberosity. ICD-9-CM codes were also used to identify patients with rotator cuff disorders such as rotator cuff tear/strain/syndrome. ICD-9-CM diagnoses codes were used to determine complications such as pulmonary embolism, post-operative infections, and potential causes for revision arthroplasty such as loosening, dislocation, prosthetic or peri-prosthetic fracture, osteolysis, and other mechanical complications. Further details on ICD-9-CM codes used for our analysis are included in the Appendix. The Nationwide Inpatient Sample databases only permit assessment of inhospital complications and mortality.
Statistical Analysis
We estimated population-based number of patients undergoing anatomic total shoulder arthroplasty, hemiarthroplasty, reverse shoulder arthroplasty, and total elbow arthroplasty, and revision arthroplasty in the United States for the years 2009, 2010, and 2011 by using sampling weights provided by the Nationwide Inpatient Sample. The sampling weights in Nationwide Inpatient Sample were calculated within each sampling stratum as the ratio of discharges in the American Hospital Association survey data for non-rehabilitation community hospitals to discharges in the sample17. We calculated confidence intervals around the point estimates using strata and cluster variables.
We calculated age and sex stratified procedural rates per 100,000 persons by using 2009–2011 population estimates for a given age-group by sex and year from the U.S. Census Bureau6–8. Since, a separate code for reverse shoulder arthroplasty did not exist prior to October 1, 20109, it is likely that cases of reverse shoulder arthroplasty were coded as total shoulder arthroplasty or hemiarthroplasty in 2009 and 2010. Hence, we report cumulative primary shoulder arthroplasty (henceforth also referred to as shoulder arthroplasty) rates per 100,000 persons stratified by age and sex for the years 2009 to 2011. We used joinpoint regression analysis to assess changes in utilization of primary shoulder arthroplasty. A software developed by the Surveillance Research Program of the National Cancer Institute was used for this purpose28. Joinpoint regression permits assessment of significant changes in slopes of linear trend and provides an average annual percent change that summarizes trend over a period of time27.
We also present unweighted proportion of patients by diagnosis, in-hospital complications, and in-hospital mortality for all three years of the study combined. Statistical analyses were conducted using SAS for Windows (version 9.3), SAS Institute Inc., (Cary, NC, USA).
RESULTS
The utilization of primary shoulder arthroplasty (anatomic total, hemi, and reverse) increased significantly from 52,397 procedures (95% CI=47,093–57,701) in 2009 to 67,184 procedures (95% CI=60,638–73,731) in 2011 (Table 1). Joinpoint regression identified one significant phase of increase in utilization of primary shoulder arthroplasty with an average annual percent change of 13.2. The estimates for reverse shoulder arthroplasty were only calculated for 2011 when 21,916 (95% CI=18,796–25,035) procedures were performed, accounting for 42% of all primary shoulder arthroplasty procedures in 2011. There was an increase in the overall number of upper extremity revision procedures performed from 2009 to 2011 (increased from 5,070 procedures to 6,028 procedures). However, revision arthroplasty procedures as a proportion of all shoulder arthroplasty procedures remained stable during the study period (8.8% in 2009 versus 8.2% in 2011). Our assumption that a majority of upper extremity procedures were performed for the shoulder was valid since only 7% of all primary upper extremity arthroplasty procedures were performed for the elbow, wrist, hand, and fingers between 2009 and 2011.
Table 1.
Estimates of Shoulder Arthroplasty Procedures in the United States
| Year | ||||||
|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | ||||
| Estimate | 95% Confidence Intervals | Estimate | 95% Confidence Intervals | Estimate | 95% Confidence Intervals | |
| Hemiarthroplasty | 19,394 | (17,777 – 21,012) | 18,713 | (17,053 – 20,373) | 15,860 | (14,484 – 17,236) |
| Anatomic Total Shoulder Arthroplasty | N/A* | N/A | N/A | N/A | 29,414 | (26,145 – 32,682) |
| Reverse Shoulder Arthroplasty | N/A** | N/A | N/A | N/A | 21,916 | (18,796 – 25,035) |
| Cumulative Primary Shoulder Arthroplasty | 52,397 | (47,093 – 57,701) | 62,695 | (55,971 – 69,419) | 67,184 | (60,638 – 73,731) |
| Elbow Arthroplasty | 2,775 | (2,386 – 3,164) | 2,973 | (2,507 – 3,439) | 2,987 | (2,551 – 3,423) |
| Revision Upper Extremity Arthroplasty | 5,070 | (3,977 – 6,162) | 5,970 | (4,650 – 7,290) | 6,028 | (4,990 – 7,065) |
N/A since total shoulder arthroplasty codes are the same for anatomic and reverse total shoulder arthroplasty in 2009 and until October 1, 2010
N/A since an ICD-9-CM code for reverse shoulder arthroplasty was not implemented until October 1, 2010
The rate of primary shoulder arthroplasty was highest in the 75–84 year female age-group (133 per 100,000 persons in 2009, 95% CI=120–146, and; 170 per 100,000 persons in 2011, 95% CI=154–186; Figure 1). Females in the 65–74 age-group had the next highest rate of primary shoulder arthroplasty (96 per 100,000 persons in 2009, 95% CI=86–1050, and; 119 per 100,000 persons in 2011, 95% CI=108–131). Among males, 75–84 year old persons had the highest utilization of primary shoulder arthroplasty with a rate of 79 per 100,000 persons in 2009 (95% CI=69–90) and 113 per 100,000 persons in 2011 (95% CI=101–125). The highest rate of reverse shoulder arthroplasty in 2011 was in the 75–84 year female sub-group (77 per 100,000 persons, 95% CI=67–87; Table 2).
Figure 1. Yearly Estimates of Primary Shoulder Arthroplasty* per 100,000 Persons in the United States by Age-Groups and Sex.
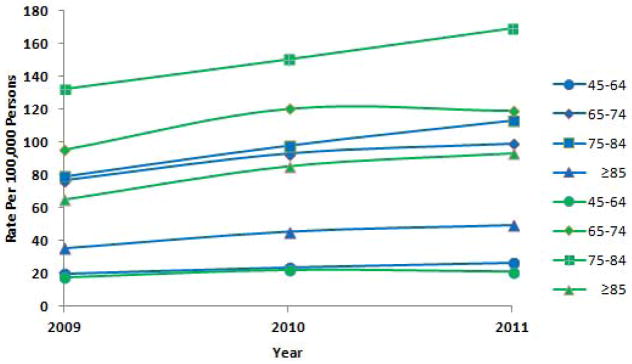
Note: Green lines in the figure represent females and blue lines represent males
*Shoulder arthroplasty includes anatomic total shoulder arthroplasty, hemiarthroplasty, and reverse shoulder arthroplasty
Table 2.
2011 Estimates for Reverse Shoulder Arthroplasty per 100,000 persons in the United States by Sex and Age-Groups
| Estimate | 95% Confidence Intervals | |
|---|---|---|
| Male | ||
| 45–64 | 5 | (3 – 6) |
| 65–74 | 29 | (24 – 34) |
| 75–84 | 51 | (44 – 57) |
| ≥85 | 24 | (18 – 30) |
| Female | ||
| 45–64 | 5 | (4 – 6) |
| 65–74 | 42 | (36 – 47) |
| 75–84 | 77 | (67 – 87) |
| ≥85 | 41 | (33 – 48) |
The rate of revision arthroplasty was highest in the 75–84 age-group in females in 2009 (10 per 100,000 persons; 95% CI=8–12) but decreased to 9 (95% CI=7–12) per 100,000 persons in this age-group in 2011 (Figure 2). Among males of age 75–84 years, revision arthroplasty rate increased from 6 (95% CI=4–8) per 100,000 persons in 2009 to 10 (95% CI=7–12) per 100,000 persons in 2011.
Figure 2. Yearly Estimates of Revision Upper Extremity Arthroplasty per 100,000 Persons in the United States by Age-Groups and Sex.
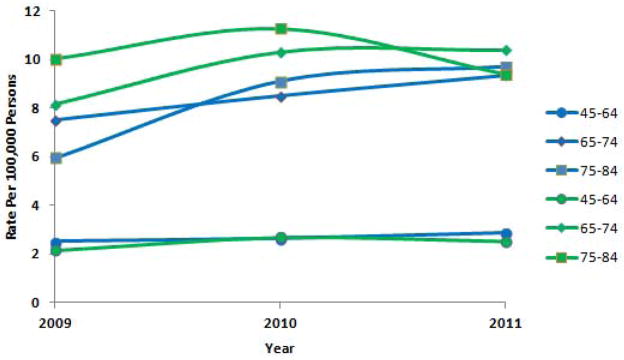
Note: Green lines in the figure represent females and blue lines represent males
≥85 age-group not included because there were <50 patients in this age-group and reliable estimates could not be obtained
Hemiarthroplasty and reverse shoulder arthroplasty had the highest in-hospital mortality rates of 0.28% and 0.24%, respectively (Table 3). In-hospital complication rates were low for all primary and revision arthroplasty procedures and ranged between 0.0% for post-operative infections/wound complications after anatomical total shoulder arthroplasty to 0.78% for postoperative infections/wound complications after reverse shoulder arthroplasty. In-hospital length of stay was 2.6 days (SD=2.4) for primary reverse shoulder arthroplasty as compared with 2.1 days (SD=1.4) for primary anatomic total shoulder arthroplasty.
Table 3.
Outcomes and Complications of Shoulder Arthroplasty in the United States: 2009–2011
| Anatomic Total Shoulder Arthroplasty* | Hemiarthroplasty | Reverse Shoulder Arthroplasty** | Revision Upper Extremity Arthroplasty | |
|---|---|---|---|---|
|
| ||||
| Mortality | 0.03% | 0.28% | 0.24% | 0.06% |
| Length of stay± (days) | 2.1 (1.4) | 3.3 (3.8) | 2.6 (2.4) | 2.7 (2.7) |
| Complications | ||||
| Pulmonary embolism | 0.10% | 0.41% | 0.06% | 0.06% |
| Post-operative infection or would complications | 0.0% | 0.14% | 0.78% | 0.72% |
includes only patients coded as anatomic total shoulder arthroplasty in 2011
includes only patients coded as having reverse shoulder arthroplasty in 2010 and 2011
Mean ± Standard Deviation
n for missing: 9 for mortality for total shoulder arthroplasty; 11 for mortality for hemiarthroplasty; 1 for reverse shoulder arthroplasty
Osteoarthritis was the most common indication for anatomic total shoulder arthroplasty (90.1% of patients), hemiarthroplasty (42.8% of patients), and reverse shoulder arthroplasty (53.2% of patients; Table 4). Patients undergoing reverse shoulder arthroplasty had rotator cuff tear/syndrome in 52.5% of cases. The concomitant diagnosis of osteoarthritis and rotator cuff disorder was found in only 29.8% of cases. The indications for revision arthroplasty included mechanical causes (22% of cases), dislocation (18% of cases), aseptic loosening (13% of cases), and prosthetic or peri-prosthetic fracture (8% of cases) (Figure 3).
Table 4.
Indications for Primary Shoulder Arthroplasty in the United States: 2009–2011
| Anatomic Total Shoulder Arthroplasty* | Hemiarthroplasty | Reverse Shoulder Arthroplasty** | |
|---|---|---|---|
|
| |||
| Osteoarthritis | 90.1% | 42.8% | 53.2% |
| Proximal humeral fracture‡ | 1.2% | 38.5% | 10.1% |
| Rheumatoid arthritis | 4.1% | 3.8% | 5.8% |
| Avascular necrosis of humeral head | 3.1% | 7.0% | 1.8% |
| Rotator cuff syndrome/tear | N/A | N/A | 52.5% |
includes only patients coded as anatomic total shoulder arthroplasty in 2011
includes only patients coded as having reverse shoulder arthroplasty in 2010 and 2011
includes surgical and anatomical neck of humerus
Mean ± Standard Deviation
Figure 3. Select Indications for Revision Upper Extremity Arthroplasty in the United States (2009–11).
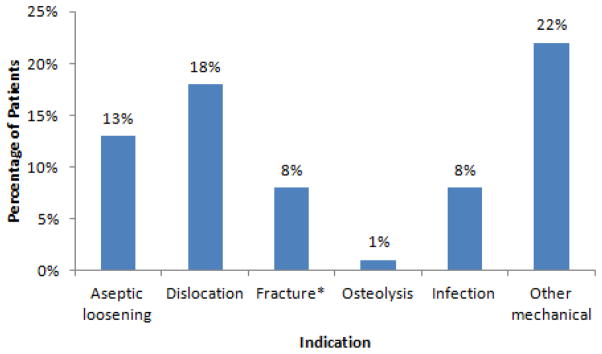
*prosthetic or peri-prosthetic
Total does not equal 100% since only select indications included
DISCUSSION
We assessed recent estimates of utilization of primary and revision shoulder arthroplasty in the United States. We also determined the contribution of reverse shoulder arthroplasty to overall utilization of primary shoulder arthroplasty and present age and sex stratified national rates of shoulder arthroplasty. We found that the utilization of primary shoulder arthroplasty has significantly increased in just a three year span from 2009 to 2011, with a major contribution from reverse shoulder arthroplasty in 2011. There was also a substantial yearly revision arthroplasty rate of 8.2%–8.8% from 2009 to 2011. Although complication and mortality rates of shoulder arthroplasty were low, reverse shoulder arthroplasty had higher rates as compared with anatomic total shoulder arthroplasty.
Kim et al used the Nationwide Inpatient Samples from 1993 to 2008 and reported an increase from an estimated 13,837 primary shoulder arthroplasty procedures in 1993 to 46,951 procedures in 2008 (an increase of 339% from 1993 and 246% from 1999)19. In contrast, the utilization of total knee arthroplasty increased from an estimated 262,601 procedures in 1999 to 615,050 procedures in 2008 (an increase of 135% from 1999)20. Kim et al postulated that some of the growth in shoulder arthroplasty was secondary to the approval of reverse shoulder arthroplasty by the FDA in 200319. However, reverse shoulder arthroplasty did not have a dedicated ICD-9-CM procedure code and therefore the contribution of reverse shoulder arthroplasty to the overall growth in shoulder arthroplasty could not be determined from this study. For the first time, the 2011 Nationwide Inpatient Sample permits calculations of reverse shoulder arthroplasty estimates because the Center for Medicare & Medicaid Services (CMS) assigned reverse shoulder arthroplasty a dedicated ICD-9-CM procedure code that was effective on October 1, 20109. Our study shows that in a short span of three years, there has been significant growth in the utilization of primary shoulder arthroplasty and reverse shoulder arthroplasty comprised 42% of all primary shoulder arthroplasty procedures in 2011. Although the growth in primary shoulder arthroplasty was greater than for total knee arthroplasty between 1999 and 2008, the absolute utilization of shoulder arthroplasty is only a fraction of total knee arthroplasty. Moreover, the advent of the reverse shoulder prosthesis represents a substantial improvement in prosthetic strategy for shoulder arthroplasty; such a parallel does not exist for total knee arthroplasty.
Boguski et al used 2012 data on 3,119 shoulder arthroplasty cases from 100 hospitals in 18 states to characterize variation in utilization of reverse shoulder arthroplasty across hospitals and the effect of hospital volume on this variation1. They reported wide variation between 0% and 100% (mean of 42.3%) in the use of reverse shoulder arthroplasty across hospitals. They also found that high total shoulder arthroplasty replacement volume hospitals had a lower variation in reverse shoulder arthroplasty use as compared with low volume hospitals. In our study, reverse shoulder arthroplasty accounted for 42% of all primary shoulder arthroplasty cases. This is similar to that reported by Boguski et al except that our study also includes hemiarthroplasty in this calculation. Thus, the utilization of reverse shoulder arthroplasty was substantial and may possibly comprise a majority of shoulder arthroplasty procedures in the future. Despite the high reverse shoulder arthroplasty utilization, there are only few studies documenting improved pain and functional outcomes after reverse shoulder arthroplasty3, 4, 26, 32, 40 and there is lack of data on long-term outcomes from robustly designed longitudinal studies. Reverse shoulder arthroplasty is a complex surgical procedure22. Prior studies have also reported high rates of complications such as scapular notching, glenoid dissociation (due to baseplate failure or loosening), acromial/scapular spine fracture, and dislocation13, 30, 32, 33, 35, 42. Reoperation rates of 12% and 33% were reported in two prior studies13, 42. These rates are higher than the 8.2–8.8% overall revision arthroplasty rates reported in our study. Reverse shoulder arthroplasty also had a substantially higher in-hospital mortality and post-operative infection/wound complication rate as compared with anatomic total shoulder arthroplasty in our study. Our data additionally showed a higher mean length of stay after reverse shoulder arthroplasty as compared with anatomic total shoulder arthroplasty. Thus, the increased utilization of reverse shoulder arthroplasty needs further assessment.
Reverse shoulder arthroplasty was initially described by Grammont15, and is principally indicated in cases of glenohumeral arthritis associated with instability as a result of a functionally or anatomically deficient rotator cuff in the elderly2, 13, 16, 22; however, our data shows that the concomitant diagnosis of osteoarthritis and rotator cuff disorder was coded in only 29.8% of cases undergoing reverse shoulder arthroplasty. This is likely because the indications for reverse shoulder arthroplasty have expanded to include isolated large rotator cuff tears, proximal humeral fractures, cases of revision arthroplasty, and younger patients5, 25, 26. Reverse shoulder arthroplasty has also been recently described to produce good results in patients with primary glenohumeral osteoarthritis and biconcave glenoid without rotator cuff impairment23.
Day et al used the Nationwide Inpatient Samples to project future growth in shoulder arthroplasty procedures11. They presented an estimated growth rate of 205% for hemiarthroplasty and 353% for revision arthroplasty between 2007 and 2015. As per our estimates the cumulative rate of shoulder arthroplasty increased by 60% between 2007 and 2011. Although this is slower than estimated by Day et al and may not reach 205% by 2015, the growth is substantial. Possible contributors to this growth include the addition of reverse shoulder arthroplasty to shoulder arthroplasty procedures, expansion of indications for shoulder arthroplasty, and an increasing elderly population. Other reasons may include serving an unmet need in patients who did not previously have awareness or access to primary shoulder arthroplasty that has been reliably shown to provide pain relief and improve functional outcomes in patients with shoulder arthropathies and fractures10, 14, 21, 29, 38. Orthopedic surgeons may also have increased awareness and expertise in performing shoulder arthroplasty over the last decade; thus improving patient access.
As reported by Kim et al, there was also a growth in orthopedic surgeon density between 2008 and 2010 from 5.8 to 7.2 surgeons per 100,000 persons.19 The American Academy of Orthopaedic Surgeons recently estimated that the orthopaedic surgeon density further increased to 8.7 per 100,000 persons in 201237. There has also been a rapid increase in dedicated shoulder surgery fellowships since the mid-1990s. Although the relationship between orthopedist density and rates of surgery is debated,39, 41 it is possible that the increase in density of surgeons with expertise in performing shoulder surgery is one of the factors that has contributed to the increase in rates of shoulder arthroplasty.
Females had higher utilization rates of primary shoulder arthroplasty procedures, including those for reverse shoulder arthroplasty. This is in agreement with previous reports19. The highest utilization of reverse shoulder arthroplasty was in the 75–84 age-groups. Since there is an increasing rate of rotator cuff impairment (symptomatic and asymptomatic) with increasing age24, 34, 36, 44, it is possible that reverse shoulder arthroplasty was the preferred option in older patients needing shoulder arthroplasty. Overall primary shoulder arthroplasty rates were also the highest in 75–84 year old females, followed by 65–74 year old females, and then by 75–84 year old males likely due to a higher incidence of osteoarthritis with increasing age. The rates of primary shoulder arthroplasty were substantially lower in patients 85 years and older likely because of concerns of surgical morbidity and mortality and the ability of patients to participate in post-operative rehabilitation. The in-hospital mortality and length of stay were higher for hemiarthroplasty and reverse shoulder arthroplasty (as opposed to primary anatomic shoulder arthroplasty) likely because these patients were older and a larger proportion of patients undergoing hemiarthroplasty had a proximal humeral fracture that is cause for additional morbidity and mortality.
Although our data permits calculation of nationally representative shoulder arthroplasty rates, our study has a few limitations. These include the use of ICD-9-CM codes that are not entirely specific to the procedure of interest. Hence, procedures such as resurfacing of the humeral head or glenoid may be included in total shoulder arthroplasty or hemiarthroplasty estimates. However, these only form a small fraction of shoulder arthroplasty procedures and may also be coded using a non-specific shoulder arthroplasty/repair code of 81.83. We were also unable to ascertain yearly estimates for reverse shoulder arthroplasty in 2009 and 2010 due to lack of an ICD-9-CM code specific to reverse shoulder arthroplasty. Hence, reverse shoulder arthroplasty procedures in 2009 and for most part of 2010 were likely coded as total shoulder arthroplasty or hemiarthroplasty. We used the revision arthroplasty code of 81.97 as has been previously described11. However, the ICD-9-CM code of 81.83 may also be assigned to cases of revision shoulder arthroplasty. The 81.83 code is described as “Other repairs of shoulder” and may also include shoulder procedures with use of internal fixation device, or external traction or fixation. Hence, we did not use 81.83 to calculate cases of revision arthroplasty in our study and likely underestimated utilization of revision arthroplasty. Our data source also does not specifically allow for recognition of revision reverse shoulder arthroplasty cases since a specific corresponding ICD-9-CM procedure code does not exist. More specific details on complications of hemiarthroplasty such as due to tuberosity healing, of total shoulder arthroplasty such as glenoid loosening, and of reverse shoulder arthroplasty such as instability cannot be ascertained from our data.
CONCLUSION
The utilization of primary shoulder arthroplasty has substantially increased in just a three year time span from 2009 to 2011 with a major contribution from reverse shoulder arthroplasty in 2011. Efforts to understand long-term outcomes of reverse shoulder arthroplasty are needed. The practice of reverse shoulder arthroplasty utilization in patients without rotator cuff impairments also needs further assessment given the large proportion of patients without concomitant osteoarthritis and rotator cuff impairment undergoing reverse shoulder arthroplasty. There was a low in-hospital complication and mortality rate after primary and revision shoulder arthroplasty, and mechanical complications and dislocation were the main causes of revision arthroplasties. The burden from revision arthroplasties in the United States is also substantial and assessment of strategies to optimize longevity and outcomes of primary shoulder arthroplasty are needed.
Supplementary Material
Acknowledgments
Source of Funding
Dr. Jain is supported by funding from National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) project number 1K23AR059199, Foundation for PM&R, and Biomedical Research Institute at Brigham and Women’s Hospital. Dr. Yamaguchi is supported by funding from National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) project number 5R01AR051026.
Footnotes
Disclosures: Dr. Yamaguchi receives royalties from Zimmer and Tornier related to development of joint arthroplasty systems.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boguski RM, Miller BS, Carpenter JE, Mendenhall S, Hughes RE. Variation in use of reverse total shoulder arthroplasty across hospitals. J Shoulder Elbow Surg. 2013;22(12):1633–8. doi: 10.1016/j.jse.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Bohsali KI, Wirth MA, Rockwood CA., Jr Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(10):2279–92. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg. 2009;18(4):600–6. doi: 10.1016/j.jse.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15(5):527–40. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br. 2007;89(4):516–20. doi: 10.1302/0301-620X.89B4.18435. [DOI] [PubMed] [Google Scholar]
- 6.Census. United States Census Bureau. Annual Estimates of the Resident Population for the United States, Regions, States, and Puerto Rico: April 1, 2000 to July 1, 2009. 2010 http://www.census.gov/popest/data/historical/2000s/vintage_2009/ [cited 2012 June 7]; Available from: http://www.census.gov/popest/data/historical/2000s/vintage_2009/
- 7.Census. United States Census Bureau. Age and Sex Composition in the United States: 2010. 2012 http://www.census.gov/population/age/data/2010comp.html. [cited 2013 December 11]
- 8.Census. United States Census Bureau. Age and Sex Composition in the United States: 2011. 2012 www.census.gov/population/age/data/2011comp.html. [cited 2013 December 11]
- 9.CMS. Centers for Medicare & Medicaid Services (CMS) 2010 Pub 100-04 Medicare Claims Processing. http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R2017CP.pdf. [cited 2013 December 11]
- 10.Cofield RH. Total shoulder arthroplasty with the Neer prosthesis. J Bone Joint Surg Am. 1984;66(6):899–906. doi: 10.2106/00004623-198466060-00010. [DOI] [PubMed] [Google Scholar]
- 11.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19(8):1115–20. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 12.FDA. Food and Drug Administration. 510(k) Summary: Delta Shoulder. Rockville, MD: 2003. http://www.accessdata.fda.gov/cdrh_docs/pdf2/K021478.pdf. [cited 2013 December 11]; Available from: http://www.accessdata.fda.gov/cdrh_docs/pdf2/K021478.pdf. [Google Scholar]
- 13.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87(8):1697–705. doi: 10.2106/JBJS.D.02813. [DOI] [PubMed] [Google Scholar]
- 14.Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am. 2000;82(1):26–34. doi: 10.2106/00004623-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16(1):65–8. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 16.Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742–7. doi: 10.2106/JBJS.E.00851. [DOI] [PubMed] [Google Scholar]
- 17.HCUP. Healthcare Cost and Utilization Project (HCUP) NIS Database Documentation. Rockville, MD: Agency for Healthcare Research and Quality; 2013. [cited 2013 April 21]; Available from: http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. [Google Scholar]
- 18.Jain NB, Higgins LD, Guller U, Pietrobon R, Katz JN. Trends in the epidemiology of total shoulder arthroplasty in the United States from 1990–2000. Arthritis Rheum. 2006;55(4):591–7. doi: 10.1002/art.22102. [DOI] [PubMed] [Google Scholar]
- 19.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93(24):2249–54. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 20.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(3):201–7. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsen FA., 3rd Early effectiveness of shoulder arthroplasty for patients who have primary glenohumeral degenerative joint disease. J Bone Joint Surg Am. 1996;78(2):260–4. doi: 10.2106/00004623-199602000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Matsen FA, 3rd, Boileau P, Walch G, Gerber C, Bicknell RT. The reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007;89(3):660–7. doi: 10.2106/00004623-200703000-00027. [DOI] [PubMed] [Google Scholar]
- 23.Mizuno N, Denard PJ, Raiss P, Walch G. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am. 2013;95(14):1297–304. doi: 10.2106/JBJS.L.00820. [DOI] [PubMed] [Google Scholar]
- 24.Moosmayer S, Smith HJ, Tariq R, Larmo A. Prevalence and characteristics of asymptomatic tears of the rotator cuff: an ultrasonographic and clinical study. J Bone Joint Surg Br. 2009;91(2):196–200. doi: 10.1302/0301-620X.91B2.21069. [DOI] [PubMed] [Google Scholar]
- 25.Muh SJ, Streit JJ, Wanner JP, Lenarz CJ, Shishani Y, Rowland DY, et al. Early follow-up of reverse total shoulder arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2013;95(20):1877–83. doi: 10.2106/JBJS.L.10005. [DOI] [PubMed] [Google Scholar]
- 26.Mulieri P, Dunning P, Klein S, Pupello D, Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am. 2010;92(15):2544–56. doi: 10.2106/JBJS.I.00912. [DOI] [PubMed] [Google Scholar]
- 27.NCI. National Cancer Institute. Average Annual Percent Change (AAPC) 2013 http://surveillance.cancer.gov/joinpoint/aapc.html. [cited 2013 December 12]
- 28.NCI. National Cancer Institute. Joinpoint regression program. 2013 http://surveillance.cancer.gov/joinpoint/ [cited 2013 December 11]
- 29.Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg. 2002;11(2):130–5. doi: 10.1067/mse.2002.121146. [DOI] [PubMed] [Google Scholar]
- 30.Nwakama AC, Cofield RH, Kavanagh BF, Loehr JF. Semiconstrained total shoulder arthroplasty for glenohumeral arthritis and massive rotator cuff tearing. J Shoulder Elbow Surg. 2000;9(4):302–7. doi: 10.1067/mse.2000.106467. [DOI] [PubMed] [Google Scholar]
- 31.Rejeski WJ, Focht BC, Messier SP, Morgan T, Pahor M, Penninx B. Obese, older adults with knee osteoarthritis: weight loss, exercise, and quality of life. Health Psychol. 2002;21(5):419–26. doi: 10.1037/0278-6133.21.5.419. [DOI] [PubMed] [Google Scholar]
- 32.Rittmeister M, Kerschbaumer F. Grammont reverse total shoulder arthroplasty in patients with rheumatoid arthritis and nonreconstructible rotator cuff lesions. J Shoulder Elbow Surg. 2001;10(1):17–22. doi: 10.1067/mse.2001.110515. [DOI] [PubMed] [Google Scholar]
- 33.Seebauer L, Walter W, Keyl W. Reverse total shoulder arthroplasty for the treatment of defect arthropathy. Oper Orthop Traumatol. 2005;17(1):1–24. doi: 10.1007/s00064-005-1119-1. [DOI] [PubMed] [Google Scholar]
- 34.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77(1):10–5. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388–95. doi: 10.1302/0301-620X.86B3.14024. [DOI] [PubMed] [Google Scholar]
- 36.Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8(4):296–9. doi: 10.1016/s1058-2746(99)90148-9. [DOI] [PubMed] [Google Scholar]
- 37.Tierney S, Mamas M, Woods S, Rutter MK, Gibson M, Neyses L, et al. What strategies are effective for exercise adherence in heart failure? A systematic review of controlled studies. Heart Fail Rev. 2012;17(1):107–15. doi: 10.1007/s10741-011-9252-4. [DOI] [PubMed] [Google Scholar]
- 38.Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495–505. doi: 10.1016/s1058-2746(97)90081-1. [DOI] [PubMed] [Google Scholar]
- 39.Vitale MG, Krant JJ, Gelijns AC, Heitjan DF, Arons RR, Bigliani LU, et al. Geographic variations in the rates of operative procedures involving the shoulder, including total shoulder replacement, humeral head replacement, and rotator cuff repair. J Bone Joint Surg Am. 1999;81(6):763–72. doi: 10.2106/00004623-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Wall B, Nove-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476–85. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 41.Weinstein JN, Birkmeyer JD. Dartmouth Medical School. Chicago, IL: AHA; 2000. The Center of the Evaluative Clinical Sciences. [Google Scholar]
- 42.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87(7):1476–86. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
- 43.Whalen D, Houchens R, Elixhauser A. Final 2000 NIS Comparison Report. HCUP Methods Series Report#2003–1. 2003 Available at: http://www.hcup-us.ahrq.gov/reports/2000NISComparisonReportFinal.pdf.
- 44.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699–704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


