Abstract
Generalized anxiety disorder (GAD) and attention-deficit/hyperactivity disorder (ADHD) commonly co-occur in childhood. Inattention symptoms can be hallmarks of both conditions, however assessment tools of inattention may not effectively distinguish between the two conditions. The present study used receiver operating characteristic (ROC) analyses to examine the high-end specificity of the Attention Problems Scale of the Child Behavior Checklist (CBCL) for detecting comorbid ADHD among youth with GAD (N = 46). Results support the utility of the Attention Problems Scale for accurately distinguishing between the two groups (AUC = 0.84, SE = .06). Specifically, a cut score of 63 achieved the most favorable values across diagnostic utility indices; 74% of GAD youth with ADHD scored above this cutoff and 91% of GAD youth without ADHD scored below this cutoff. Findings provide support for the use of the CBCL Attention Problems Scale to supplement diagnostic interviews and identify inattention associated with ADHD among GAD youth.
Keywords: attention-deficit/hyperactivity disorder, Child Behavior Checklist, generalized anxiety disorder, high-end specificity, inattention
1. Introduction
Attention-deficit hyperactivity disorder (ADHD) is a highly debilitating condition that is frequently comorbid with multiple internalizing and externalizing disorders (e.g., Jensen, 2001). Roughly 7% of the U.S. child population has met diagnostic criteria for ADHD in the past year (Kessler et al., 2012), and affected youth are at risk for a host of negative sequelae, including reduced academic achievement, educational attainment, peer functioning, and overall quality of life (e.g., Hakkaart-van Roijen et al., 2007; Loe & Feldman, 2007; Murray-Close et al., 2010). Although the majority of work to date examining ADHD comorbidities has investigated dysfunction association with ADHD and other externalizing comorbidities, such as oppositional defiant disorder and conduct disorder (Kuhne, Schachar, & Tannock, 1997), recent work has specifically explored previously understudied and impairing heterotypic comorbidity patterns such as the co-occurrence of ADHD and anxiety problems (Jarrett & Ollendick, 2008; Jarrett, Wolff, Davis, Cowart, & Ollendick, 2012; Tannock, 2009).
Generalized anxiety disorder (GAD)—characterized by uncontrollable and interfering worry and related symptoms, and associated with considerable impairments in its own right (Comer et al., 2011)—is one of the most common anxiety conditions that co-occurs with ADHD in childhood and adolescence, with estimates indicating that the disorders co-occur in up to 15% of youth (Elia, Ambrosini, & Berrettini, 2008). Meta-analytic work by Willcutt and colleagues (2012) demonstrates that compared to healthy controls, children and adolescents with ADHD-Combined Subtype (ADHD-C) are 6.5 times more likely to meet criteria for comorbid GAD, while youth with the Inattentive (ADHD-I) and Hyperactive/Impulsive (ADHD-H/I) subtypes are also more likely to meet criteria for co-occurring GAD (OR = 3.5 and 4.2, respectively). Parallel comorbidity patterns have also been observed in the adult literature, with recent epidemiological studies indicating that 23% of adults with GAD suffer from comorbid ADHD (Van Ameringen, Mancini, Simpson, & Patterson, 2011). In addition, adults with GAD are more likely than adults with social phobia to have a childhood history of ADHD (Safren, Lanka, Otto, & Pollack, 2001), further supporting the specific comorbidity of these two conditions across the lifespan.
Despite evidence demonstrating the frequent co-occurrence of ADHD and GAD and unique associated impairments, much remains to be learned about the nature of this comorbidity pattern. Notably, there is some degree of overlap in the symptom criteria for both GAD and ADHD, including difficulties with inattention, problems concentrating, and restlessness (American Psychiatric Association, 2013). Such symptom overlap can increase the likelihood of misdiagnosing a child with ADHD when a diagnosis of GAD is indicated, and vice-versa. With respect to inattention symptoms, it has been suggested that intrusive worries and hypervigilance to threat cues associated with GAD often manifest as symptoms of inattention (Jarrett & Ollendick, 2008), which can complicate differential diagnosis decisions.
Recent evidence suggests that the mechanisms underlying symptoms of inattention differ between anxiety disorders and ADHD. For example, Weissman and colleagues (2012) compared the performance of anxious, inattentive-impulsive, and typically developing children on several neurocognitive tasks assessing attentional processes. The authors found that inattentive-impulsive youth performed more poorly on tests of general attentional processes, as measured by the Conners’ Continuous Performance Test (CPT-II), than anxious children and typically developing controls. In contrast, anxious youth showed greater attentional biases toward threat cues than inattentive-impulsive youth, as assessed by the Faces Dot Probe Task. Another recent study by Jarrett and colleagues (2012) compared the performance of youth with anxiety disorders only (ANX only), comorbid ADHD and anxiety disorders (ANX+ADHD), and ADHD only. Researchers found significant differences on CPT performance between groups, indicating that youth with ADHD only were significantly more impaired than groups with anxious profiles. Taken together, these findings suggest that although symptoms of inattention, broadly speaking, are hallmarks of both GAD and ADHD, some might argue that inattention in GAD may be functionally different than inattention in ADHD, given differences in neuropsychological correlates. These discrepancies provide preliminary support for distinct neurologic pathways in the etiology of attention difficulties between GAD and ADHD.
Accurate assessment is the critical first step in the design of indicated treatment planning. Given overlapping symptom presentations from a topographical perspective across GAD and ADHD, assessment tools that inform differential diagnosis, which in turn informs treatment planning among anxious youth, must be sensitive enough to distinguish inattention symptoms associated with ADHD from GAD-related inattention. Although structured and semi-structured diagnostic interviews, neuropsychological assessments, and behavioral observations can offer more comprehensive assessments of a child’s differential clinical portrait, such assessment methods are time- and cost-intensive, and as such are used less frequently in clinical practice than self-administered symptom questionnaires (Pelham, Fabiano, & Massetti, 2005). Therefore it is crucial that screening measures widely used in clinical practice be empirically scrutinized with regard to their ability to distinguish between GAD- and ADHD-related attention problems.
The Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) is one of the most widely used and well-supported parent-report measures of child psychopathology in clinical practice. The Attention Problems Scale—one of nine CBCL clinical syndrome scales—purportedly assesses the presence of inattention symptoms frequently associated with ADHD. Research indicates that inattention as measured by the CBCL Attention Problems Scale is a continuously distributed phenomenon (Hudziak, Wadsworth, Heath, & Achenbach, 1999), and the Attention Problems scale has shown strong discriminating power for detecting ADHD in general samples (Chen, Faraone, Biederman, & Tsaung, 1994; Lampert, Polanczyk, Tramontina, Mardini, & Rohde, 2004).
Despite support for the CBCL Attention Problems Scale for detecting broad symptoms of inattention in non-anxious samples, research has yet to evaluate the performance of the Attention Problems Scale for detecting inattention among youth with GAD. Given the frequency with which the CBCL Attention Problems Scale is administered in the assessment of childhood psychopathology, in concert with concerns about the impact of diagnostic misattribution of inattention symptoms on treatment planning, research is needed to evaluate the “high-end specificity” (Kendall, Hollon, Beck, Hammen, & Ingram, 1987) of the Attention Problems Scale for detecting inattention associated with ADHD. High-end specificity refers to the evaluation of a measure’s ability to differentiate between overlapping or neighboring symptom presentations in order to assess the extent to which high scores on the measure are associated exclusively with the diagnosis in question (see Kendall et al., 1987).
The present study examined the high-end specificity of the CBCL Attention Problems Scale for detecting inattention associated with comorbid ADHD among youth with GAD. We hypothesized that if the CBCL is able to accurately capture symptoms of inattention associated with ADHD, children with comorbid GAD and ADHD should score higher on the CBCL Attention Problems Scale relative to those children presenting with GAD only even though these latter youth also present with inattention. Further, in accordance with Matthey and Petrovski’s (2002) guidelines for identifying a favorable cut score with diagnostic utility, we attempted to identify a t-score cutoff on the CBCL Attention Problems Scale that would sensitively classify at least 70% of “true” ADHD cases (as determined by structured diagnostic interviewing methods) as having inattention associated with ADHD, and would accurately classify at least 80% of GAD-only cases as not having inattention associated with ADHD.
2. Method
2.1 Participants
Participants were 46 English-speaking youth diagnosed with GAD between the ages of 7 and 18 (54% female; MAge = 12.03 years, SD = 3.3) and their English-speaking mothers who presented for clinical services for child anxiety at an urban, university-based anxiety specialty clinic in New England. The clinic from which data were drawn excludes youth with thought disorders, pervasive developmental disorders, organic brain syndromes, intellectual disabilities, or current suicidal ideation from research. Participants were predominantly Caucasian/Non-Hispanic (80.4%). Families ranged in resources: 30.3% were at or below 300% of the national poverty line for their year (e.g., in 2007, $63,609 for a family of 4; $75,240 for a family of 5) whereas 21.2% of households earned at least 600% of the national poverty line at their year of assessment (e.g., in 2007, $127,218 for a family of 4; $150,480 for a family of 5). Parents of the majority of children were married or cohabitating (83.7%); 2.3% of children’s parents were previously but no longer married, and 6.5% of parents reported being separated, widowed, or never married. The majority of participants (63.0%) were not taking psychotropic medications at the time of the assessment. Among those taking psychotropic medications, antidepressants were most common (N = 6), followed by stimulant medications (N = 5); 6 participants were taking multiple medications, as is common in outpatient samples (Comer, Olfson, & Mojtabai, 2010).
Participant diagnostic profiles were generated following formal semi-structured diagnostic interviews conducted with children and parents. GAD was the principal diagnosis or co-principal diagnosis for 25 participants (54.3%); for the remainder of the sample all GAD criteria were met with associated impairment, but another disorder presented with even greater severity. Comorbid diagnoses were common. Youth with GAD also met diagnostic criteria for the following disorders at clinical levels: ADHD (N = 23; 50.0%), social anxiety disorder (N = 14, 30.4%), specific phobia (N = 13, 28.3%), obsessive-compulsive disorder (N = 9, 19.6%), separation anxiety disorder (N = 7, 15.2%), major depressive disorder (N = 3, 6.5%), panic disorder with agoraphobia (N = 6, 13.0%), dysthymia (N = 4, 8.7%), oppositional defiant disorder (N = 3, 6.5%), depressive disorder not otherwise specified (N = 3, 6.5%), enuresis (N = 2, 4.3%), anxiety disorder not otherwise specified (N = 1, 2.2%), disruptive behavior disorder not otherwise specified (N = 1, 2.2%), post-traumatic stress disorder (N = 1, 2.2%), and trichotillomania (N = 1, 2.2.%). Of those participants with ADHD, the majority of the sample met full inattention criteria (i.e., 91.3%); specifically, thirteen participants (56.5%) were diagnosed with ADHD-C and seven participants (34.8%) with ADHD-I alone. Only two participants (8.7%) met criteria for ADHD-H/I” without meeting criteria for the inattention criteria as well.
Based on diagnostic profiles, participants were classified into two groups: (1) Youth with GAD in the diagnostic profile, but not ADHD (i.e., GAD youth; N = 23); and (2) youth with GAD in the diagnostic profile as well as comorbid ADHD (i.e., GAD+ADHD youth; N = 23).
2.2. Measures
2.2.1. Child Diagnostic Profile
The Anxiety Disorders Interview Schedule for DSM-IV-TR: Child and Parent Versions (ADIS-C/P; Silverman & Albano, 1997) was used to collect parent and child reports of DSM-IV-TR symptoms to inform clinician-generated diagnoses. The ADIS-C/P is a semi-structured diagnostic interview that thoroughly assesses child mood, anxiety, and disruptive behavior disorders in strict accordance with DSM–IV-TR criteria. The ADIS-C (child version) and the ADIS-P (parent version) collect data on child and parent reports of child symptoms, respectively. The ADIS-C/P is the most widely used diagnostic interview in clinical research with child anxiety populations, due to its strong reliability, validity, and sensitivity to change (Silverman & Ollendick, 2005; Wood, Piacentini, Berman, McCracken, & Barrios, 2002). In age ranges comparable to the present sample, the ADIS-C/P has demonstrated good reliability for parent (k range from 0.65–0.88) and child diagnostic profiles (k range from 0.63–0.88) (Silverman & Ollendick, 2005; Silverman, Saavedra, & Pina, 2001). Moreover, the ADHD module of the ADIS-C/P has shown strong concurrent validity with established parent-report and performance-based measures of ADHD (Jarrett, Wolff, & Ollendick, 2007).
2.2.2. Inattention Symptoms
Inattention symptoms were assessed using the mother-reported Attention Problems Scale of the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001). The CBCL is a 113-item parent-report instrument for youth aged 6–18 years used to assess a broad range of children’s behavioral and emotional functioning, and has shown strong psychometric properties in the assessment of children and adolescents. Parents are asked to indicate the extent to which each item describes their child now or within the past 6 months on a three-point scale, where 0 = “not true,” 1 = “somewhat or sometimes true,” and 2 = “very true or often true.” The CBCL Attention Problems Scale is one of eight CBCL Syndrome Scales. Individual items on the scale are summed, and raw scores are converted to t-scores accounting for child age and gender with a mean of 50 and a standard deviation of 10. Syndrome scales with t-scores between 65 and 69 are considered to be in the “borderline clinical” range, while t-scores above 70 are described as falling in the “clinical” range. The 10 items on the Attention Problems scale include symptoms of inattention (e.g., can’t pay attention for long”), as well as some items of hyperactivity/impulsivity (e.g., “can’t sit still, restless, or hyperactive”) and sluggish cognitive tempo (e.g., “stares blankly”). Although some of the items of the Attention Problems Scale are associated with hyperactivity/impulsivity (i.e. “can’t sit still”) and others are associated with sluggish cognitive tempo (i.e. “confused”), the scale has been supported extensively by factor analytic work (Achenbach & Rescorla, 2001; Bérubé & Achenbach, 2009), and research repeatedly supports the convergence between the Attention Problems Scale and clinician-determined ADHD diagnosis (Biederman et al., 1993; Chen et al., 1994). Moreover, evidence suggests that the Attention Problems Scale effectively distinguishes between groups of anxiety-disorders youth with and without ADHD (Jarrett et al., 2012)
2.3. Procedures
Participating families were referred to the study clinic by parents, school personnel, and mental health professionals for specialty child anxiety services. Participating children and their mothers completed all study assessments as part of a standard baseline evaluation for families seeking services. During this baseline evaluation, the ADIS-C and ADIS-P were administered separately by postdoctoral fellows and doctoral candidates in clinical psychology specializing in the assessment and treatment of pediatric disorders. All diagnoses were reviewed at a weekly diagnostic consensus meeting. Child and parent diagnostic profiles were integrated into a composite profile using the “Or” rule (see Comer & Kendall, 2004), in which symptoms were considered present if the parent or child endorsed that symptom. In addition, no children in the sample were assigned a diagnosis of ADHD based solely on the child interview.
All diagnosticians met internal certification and reliability procedures in structured diagnostic interviewing, developed in collaboration with one of the ADIS-C/P authors. Specifically, after completing extensive didactic training in child diagnoses and structured interviewing, trainee diagnosticians observed three complete interviews conducted by trained diagnosticians, collaboratively administered three interviews with a trained diagnostician, and then conducted supervised ADIS interviews until achieving the reliability criterion (i.e., full diagnostic profile agreement on 3 of 5 consecutive supervised assessments). Demographic information was obtained from parent report gathered during the intake. Consistent with previous research (Merikangas et al., 2007), household income was used to calculate a poverty ratio index (i.e. household income divided by US poverty threshold during the year of the interview), resulting in four ratio index categories: <1.5, 1.5 to <3.0, 3.0 to <6.0, and ≥6.0. Mothers also completed the CBCL at the time of the initial evaluation.
2.4. Data Analysis
Receiver operating characteristic (ROC) analyses were conducted to investigate the extent to which inattention symptoms (as measured by the CBCL Attention Problems Scale) can correctly detect ADHD among GAD youth. ROC analyses characterize the diagnostic utility of a variable (in this case inattention symptoms) by revealing the limits of the variable’s ability to discriminate over the complete spectrum of possible scores (for a review of ROC analysis, see Zweig and Campbell, 1993; see also Comer & Kendall, 2005 and Puliafico, Comer, & Kendall, 2007). Sensitivity at each potential Attention Problem Subscale t-score cutoff was defined as the percentage of GAD+ADHD youth (as classified by the ADIS-C/P) who scored above that inattention cutoff. Specificity at each potential Attention Problem Subscale t-score cutoff was defined as the percentage of GAD-only youth who scored below that inattention cutoff. Plotting the sensitivities and corresponding specificities linked to each of Attention Problem Subscale cutoff provides a curve, the area under which ranges from 1.0 (i.e., perfect separation of diagnostic groups by the Attention Problems Scale) and 0.5 (no apparent distributional difference between the two diagnostic groups’ Attention Problems Scale scores). This area under the curve (AUC) yields a quantitative estimate of diagnostic utility of the CBCL Attention Problems Scale (across all potential cutoffs) in distinguishing children diagnosed with ADHD and GAD from children with only GAD.
Positive Predictive Power (PPP) at each potential Attention Problems Scale cutoff was defined as the percentage of youth scoring above that inattention cutoff who actually have ADHD (i.e., member of the GAD+ADHD group), and Negative Predictive Power (NPP) was defined as the percentage of youth scoring below that inattention cutoff who do not have ADHD (i.e., member of the GAD only group). Base rate at each potential CBCL Attention Problems Scale cutoff was defined as percentage of youth across the full sample who scored above that inattention cutoff. Finally, for each potential CBCL Attention Problems Scale cutoff, the Overall Correct Classification (OCC) rate was defined as the percentage of cases across the full sample who either (a) scored above that inattention cutoff and had ADHD (i.e., member of the GAD+ADHD group), or (b) scored below that inattention cutoff and did not have ADHD (i.e., member of the GAD only group).
3. Results
Table 1 presents the means and standard deviations of demographic variables across GAD and GAD+ADHD youth and their mothers at the time of assessment, as well as CBCL Attention Problems Scale scores. The proportion of females in the GAD+ADHD group (65.2%) was not significantly different than the proportion of females in the GAD group (43.5%), χ2(1) = 2.19, p = .24. Child age was comparable across the two groups, t(44) = −.44, p = .66, as was ethnicity, χ2(1) = 1.24, p = .46. After controlling for number of comorbid diagnoses, CBCL Attention Problems Scale scores were significantly higher among GAD+ADHD youth with all ADHD subtypes than GAD only youth, F(1, 46) = 12.45, p = .001. Further, CBCL Attention Problem Scale scores were significantly higher among GAD+ADHD youth with inattentive profiles (i.e. participants who met for ADHD-I or ADHD-C) than for GAD Only youth, after controlling for number of comorbid diagnoses, F(1, 41) = 11.07, p < .01.
Table 1.
Demographic characteristics associated with GAD versus GAD and comorbid ADHD in a treatment-seeking sample (N = 46)
| GAD Only (n = 23)
|
GAD + ADHD (n =23)
|
|||
|---|---|---|---|---|
| N | % | N | % | |
| Gender | ||||
| Male | 13 | 56.3 | 8 | 34.8 |
| Female | 10 | 43.5 | 15 | 65.2 |
| Race/Ethnicity | ||||
| Minority | 6 | 26.1 | 3 | 13.0 |
| White | 17 | 73.9 | 20 | 87.0 |
| Poverty/Income Ratio | ||||
| <1.5 | 0 | 0.0 | 3 | 16.7 |
| 1.5 to <3.0 | 5 | 33.3 | 3 | 16.7 |
| 3.0 to <6.0 | 6 | 40.0 | 9 | 50.0 |
| ≥6.0 | 4 | 26.7 | 3 | 16.7 |
| Parent marital status | ||||
| Married | 22 | 100.0 | 14 | 66.7 |
| Divorced | 0 | 0.0 | 4 | 19.0 |
| Other | 0 | 0.0 | 3 | 14.3 |
| Mean | SD | Mean | SD | |
| Child age, years | 11.8 | 3.3 | 12.25 | 3.4 |
| CBCL Attention Problems Scale, t-score | 56.3 | 5.6 | 65.2 | 7.3 |
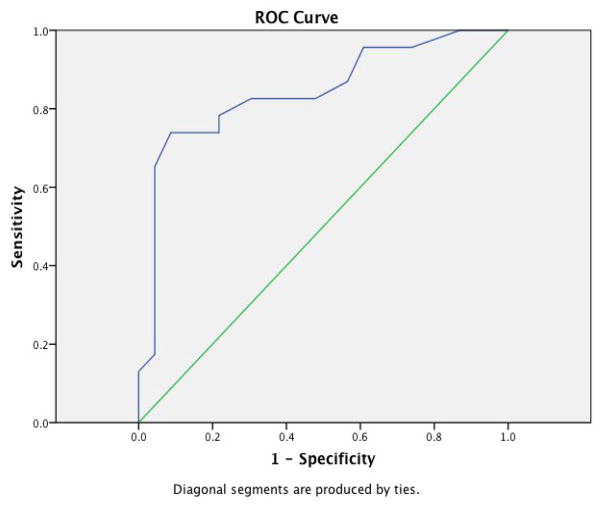
ROC analysis was conducted to investigate the overall utility of inattention symptoms (as measured by the CBCL Attention Problems Scale) for distinguishing between GAD youth and GAD+ADHD youth across all possible t-score cutoffs. Figure 1 shows the ROC curve generated by plotting all sensitivities and corresponding 1 – specificities for each potential cut score of the CBCL Attention Problems Scale. Across the entire range of potential cutoffs, inattention symptoms demonstrated a strong overall ability to successfully distinguish GAD from GAD+ADHD youth (AUC = .84, SE = .06). This value was significantly different from the null value of 0.5, which would reflect that there were no differences in the distribution of scores between the GAD versus GAD+ADHD youth (p < .001). When considering only GAD+ADHD youth who meet the inattention criteria (i.e. ADHD-I and ADHD-C), CBCL inattention symptoms again demonstrated a strong ability to differentiate between youth with GAD only versus GAD+ADHD (AUC = .84, SE = .06).
Figure 1.
ROC plot of sensitivities and 1-specificities for each CBCL Attention Problems potential cut score.
Examining the area under the ROC curve informs the overall utility of CBCL Attention Problem scores for distinguishing GAD+ADHD youth from GAD-only youth across all potential scores, but does not inform the specific diagnostic utility of inattention symptoms at each potential cutoff. Such information is critical for informing clinical assessment in routine practice settings where structured diagnostic interviews are not always feasible. Table 2 presents the sensitivity, specificity, PPP, NPP, base rate, and overall correct classification rate associated with each potential CBCL Attention Problems Scale cutoff for which sensitivity and specificity were both above 50%. As cut scores increase, the percentage of GAD+ADHD youth whose Attention Problems Scale score exceeds that cutoff (i.e. sensitivity) decreases, with indices ranging from 52.2 to 82.6 (when employing cut scores of 66 and 57, respectively).Alternatively, as the cut scores increase, the percentage of GAD youth not meeting criteria for ADHD whose Attention Problems Scale score falls below that cutoff (i.e., specificity) increases, with indices ranging from 52.2 to 95.7 (when employing cut scores of 57 and 66, respectively). Matthey and Petrovski (2002) argue that a favorable cut score with diagnostic utility is characterized by a sensitivity of at least .70 and a specificity of at least .80. In the present analysis, an Attention Problems Scale cut score of 63 exhibited the most favorable properties in correctly distinguishing between GAD and GAD+ADHD youth. At a cut score of 63, 74% of GAD youth with ADHD scored above the cutoff and 91% of youth without ADHD but with GAD scored below the cutoff. Moreover, 90% of GAD youth with an Attention Problems Scale score above 63 actually had a formal diagnosis of ADHD (PPP=89.5) and almost 80% of GAD youth who scored lower than 63 did not have a diagnosis of ADHD (NPP=77.8).
Table 2.
Diagnostic Utility Properties of the CBCL Attention Problems Scale for Distinguishing GAD (N=23) from GAD with comorbid ADHD (N=23)
| CBCL Cut-Score | Sensitivity | Specificity | PPP | NPP | Base Rate | OCC |
|---|---|---|---|---|---|---|
| 57 | 82.6 | 52.2 | 63.3 | 75.0 | 65.2 | .913 |
| 58 | 82.6 | 69.6 | 73.1 | 80.0 | 56.5 | .913 |
| 59 | 82.6 | 69.6 | 73.1 | 80.0 | 56.5 | .913 |
| 60 | 78.3 | 78.3 | 78.3 | 78.3 | 50.0 | .782 |
| 61 | 78.3 | 78.3 | 78.3 | 78.3 | 50.0 | .782 |
| 62 | 73.9 | 78.3 | 77.3 | 75.0 | 47.8 | .760 |
| 63 | 73.9 | 91.3 | 89.5 | 77.8 | 41.3 | .826 |
| 64 | 65.2 | 95.7 | 93.8 | 73.3 | 34.8 | .804 |
| 65 | 56.5 | 95.7 | 92.9 | 68.8 | 30.4 | .761 |
| 66 | 52.2 | 95.7 | 92.3 | 66.7 | 28.3 | .739 |
Note: CBCL = Child Behavior Checklist; PPP = positive predictive power; NPP = negative predictive power; OCC = overall correct classification.
4. Discussion
The present findings support the utility of the CBCL Attention Problems Scale as a continuous measure that can favorably distinguish between inattention simply due to GAD versus ADHD-related inattention among anxious youth. Specifically, ROC analysis demonstrated that across potential cut scores, the Attention Problems Scale accurately classified youth with ADHD within a sample of GAD youth seeking treatment. These findings support the high-end specificity (see Comer & Kendall, 2005) of the Attention Problems Scale, or the extent to which high scores on the CBCL Attention Problems Scale are associated solely with inattention due to ADHD and not neighboring symptom presentations. The present findings are highly encouraging given the extent to which the CBCL is used in clinical practice—often in the absence of structured diagnostic interviewing procedures.
Analyses found that an Attention Problems cut score of 63 achieved the most favorable balance of correctly classifying ADHD among GAD youth, closely approximating the recommended criteria for diagnostic utility indices, with sensitivity of .70 and specificity of .80 (Matthey & Petrovski, 2002). This cut score allowed for nearly 74% of GAD+ADHD cases to be accurately classified, while also ensuring that over 91% of cases with GAD-only were correctly identified. In total, 83% of GAD youth either (a) scored above 63 and had ADHD, or (b) scored below 63 and did not have ADHD. Interestingly, this value is slightly lower than the conventional t-score of 65 recommended by the developers of the CBCL to identify “borderline clinical” impairment associated with ADHD, and is 7 points lower than the t-score of 70 which denotes impairment at a clinical level (Achenbach & Rescorla, 2001). However, the cut score of 65 did not meet the established sensitivity/specificity criteria of .70/.80, and at this cut score only 76% of participants were correctly classified.
These results support the use of the CBCL to supplement diagnostic interviewing and inform differential diagnosis and identify symptoms of inattention due ADHD among GAD youth. To our knowledge, this is the first examination of a parent-report measure’s ability to detect ADHD symptoms specifically among anxious youth with presentations characterized by inattention. In the absence of evidence that other available self- and parent-reports of ADHD symptoms accurately classify inattention symptoms due to ADHD among anxious youth, the present findings suggest that among parent-report options, the CBCL Attention Problems Scale is the most promising in the context of anxious youth. Of course, when resources, time, and training allow for the concurrent administration of diagnostic interviews, neuropsychological testing, and teacher reports, such methods should be pursued in conjunction with administration of the CBCL parent report. However, given the limited resources that frequently characterize many practice settings, the present findings suggest that in the absence of multimodal assessments the CBCL Attention Problems Scale can be used with reasonable confidence to classify attention problems associated with ADHD among anxious youth.
This study used a well-defined sample drawn from a large population of treatment-seeking anxious youth, and incorporated data derived from child-report, parent-report, and clinician-administered diagnostic interviews. However, several limitations merit comment. First, the sociodemographic make-up and treatment-seeking nature of the sample may differ from broader clinical populations in the community, thereby limiting the generalizability of the present findings. Second, it is possible that a larger sample size might have yielded somewhat different results. Third, neither neuropsychological testing nor teacher report were presently included to confirm ADHD diagnoses generated by structured diagnostic interviews. Though a multimodal, multi-informant method of diagnostic assessment for the presence of ADHD is recommended (e.g., Barkley, 2006; Lahey et al., 1994; Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management, 2011), given evidence of low concordance rates between parent and teacher report of ADHD symptoms in children (e.g. Jensen et al., 1999; Mitsis et al., 2000; Sollie, Larsson, & Mørch, 2012), in the absence of available resources, parent report is among the optimal measures of assessing ADHD symptomatology in children (Pelham et al., 2005). Thus, the assessment methods herein are representative of those used in a large proportion of clinics in which formal neuropsychological testing and teacher reports are not incorporated into assessment procedures. Finally, given only two GAD+ADHD participants presented with ADHD-H/I, it was not possible to evaluate group differences based on ADHD subtype. Future work incorporating larger samples would do well to examine how the Attention Problems Scale can classify comorbid ADHD within samples of non-GAD anxious youth, and to test differences in the utility of the CBCL Attention Problems Scale to correctly classify youth with varying subtypes of ADHD.
Although there is a long history supporting the convergence between the Attention Problems Scale of the CBCL and ADHD diagnosis (Biederman et al., 1993; Chen et al., 1994), the CBCL Attention Problems Scale is briefer and more broad based than other parent-report measures checklists of ADHD symptomatology, such as the Vanderbilt ADHD Diagnostic Parent Rating Scale (Wolraich et al., 2003). Importantly, the present analyses did not allow for comparison of the relative utility of the CBCL versus other commonly used parent-report measures for detecting ADHD symptoms in anxious youth. Future research would do well to extend the current work by evaluating the high-end specificity of other measures of ADHD.
Accurate assessment is the critical first step in effective treatment planning, and the importance of using well-validated instruments with strong classification properties and high-end specificity cannot be overstated. Given the expanded use of psychotropic stimulant medications as a first-line approach to address ADHD symptoms in children (e.g., Comer et al., 2010; Olfson, Gameroff, Marcus, & Jensen, 2003), a proportion of misdiagnosed GAD youth may receive stimulant medication to manage symptoms of anxiety-related inattention mistaken for ADHD, even though stimulant medications do not address attentional biases found in GAD. Further, increases in anxiety can be a common side effect of stimulant medications (e.g., Vance, Luk, Costin, Tonge, & Pantelis, 1999), suggesting that for some GAD youth, stimulant treatment may contribute to worsening inattention symptoms and greater impairment. In addition, behavioral methods targeting ADHD that focus on behavioral parent training and/or parent-school coordinated contingency management of a child’s behavior do not address maladaptive anxious cognitions or avoidance patterns that are at the center of child anxiety problems. Moreover, antidepressants and exposure therapy are not effective in managing the broad inattention and executive functioning deficits at the center of ADHD. Poor assessment practices can result in contraindicated or ineffective psychopharmacology and psychological treatment regimens.
In light of these concerns, an argument could be made for prioritizing specificity over sensitivity in the diagnosis of ADHD, so as to avoid medicating youth for whom such treatments are possibly contraindicated. Despite the efficacy of these treatments, stimulant medications may be associated with unfavorable side effects, misuse/abuse, overdose, and injury (e.g. Graham & Coghill, 2008; Hartung et al., 2013; Marcus, Wan, Zhang, & Olfson, 2007; Spiller, Hayes, & Aleguas, 2013), and can even contribute to worsening symptoms for those youth with anxiety disorders (Vance et al., 1999). At the same time, others might argue that in the absence of widespread access to quality behavior therapy (e.g. National Organization of State Offices of Rural Health, 2011), sensitivity should be prioritized over specificity in the diagnosis of ADHD to ensure that youth with ADHD are more likely to be identified by their pediatrician and receive medication treatment. Both sides of this debate contain merit, and highlight the need for a favorable balance between sensitivity and specificity. However, prudence may suggest cautioning on the side of specificity given the risks of placing children on non-indicated stimulant medications with risk profiles, and access to behavioral treatments and parent training approaches when available. Careful monitoring of inattention symptoms should subsequently assess whether improvements in inattention symptoms follow the initiation of psychotherapeutic approaches, with the initiation of medication treatment occurring only in the absence of symptoms improvement.
Accurate assessment is the critical first step in effective treatment planning, and the importance of using well-validated instruments with strong classification properties and high-end specificity cannot be overstated. The present findings document that in the treatment of anxious youth, the CBCL Attention Problems Scale can be a highly useful tool for detecting inattention symptoms associated with ADHD from GAD-related inattention.
Highlights.
The high-end specificity of the Attention Problems Scale of the CBCL was examined.
The Attention Problems Scale accurately detects ADHD among youth with comorbid GAD.
A cut score of 63 achieved the most favorable balance of correct classification.
The CBCL is useful in distinguishing between GAD- and ADHD-related inattention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington VT: University of Vermont Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Barkley R. Attention-deficit/hyperactivity disorder: A handbook for diagnosis and treatment. 3. New York, NY: Guilford Press; 2006. [Google Scholar]
- Bérubé RL, Achenbach TM. Bibliography of published studies using the ASEBA. Burlington VT: University of Vermont Research Center for Children, Youth, and Families; 2009. [Google Scholar]
- Biederman J, Faraone SV, Doyle A, Lehman BK, Kraus I, Perrin J, Tsuang MT. Convergence of the Child Behavior Checklist with structured interview-based diagnoses of ADHD children with and without comorbidity. Child Psychology and Psychiatry and Allied Disciplines. 1993;34(7):1241–1251. doi: 10.1111/j.1469-7610.1993.tb01785.x. [DOI] [PubMed] [Google Scholar]
- Chen WJ, Faraone SV, Biederman J, Tsuang MT. Diagnostic accuracy of the child behavior checklist scales for attention-deficit hyperactivity disorder: A receiver-operating characteristic analysis. Journal of Consulting and Clinical Psychology. 1994;62:1017–1025. doi: 10.1037/0022-006X.62.5.1017. [DOI] [PubMed] [Google Scholar]
- Comer JS, Blanco C, Hasin DS, Liu S, Grant BF, Turner JB, Olfson M. Health-related quality of life across the anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2011;72(1):43–50. doi: 10.4088/JCP.09m05094blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Kendall PC. A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:878–886. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- Comer JS, Kendall PC. High-end specificity of the Children’s Depression Inventory (CDI) in a sample of anxiety-disordered youth. Depression and Anxiety. 2005;22:11–19. doi: 10.1002/da.20059. [DOI] [PubMed] [Google Scholar]
- Comer JS, Olfson M, Mojtabai R. National trends in child and adolescent psychotropic polypharmacy in office-based practice, 1996–2007. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1001–1010. doi: 10.1016/j.jaac.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elia J, Ambrosini P, Berrettini W. ADHD characteristics: Concurrent co-morbidity patterns in children and adolescents. Child and Adolescent Psychiatry and Mental Health. 2008;2(15) doi: 10.1186/1753-2000-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham J, Coghill D. Adverse effects of pharmacotherapies for attention- deficit/hyperactivity disorder: Epidemiology, prevention and management. CNS Drugs. 2008;22(3):213–237. doi: 10.2165/00023210-200822030-00003. [DOI] [PubMed] [Google Scholar]
- Hakkaart-van Roijen L, Zwirs BWC, Bouwmans C, Tan SS, Schulpen TWJ, Vlasveld L, Buitelaar JK. Societal costs and quality of life of children suffering from attention deficit hyperactivity disorder (ADHD) European Child and Adolescent Psychiatry. 2007;16(5):316–326. doi: 10.1007/s00787-007-0603-6. [DOI] [PubMed] [Google Scholar]
- Hartung CM, Canu WH, Cleveland CS, Lefler EK, Mignogna MJ, Fedele DA, Clapp JD. Stimulant medication use in college students: Comparison of appropriate users, misusers, and non-users. Psychology of Addictive Behaviors. 2013;27(3):832–840. doi: 10.1037/a0033822. [DOI] [PubMed] [Google Scholar]
- Hudziak JJ, Wadsworth ME, Heath AC, Achenbach TM. Latent class analysis of Child Behavior Checklist attention problems. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:985–991. doi: 10.1097/00004583-199908000-00014. [DOI] [PubMed] [Google Scholar]
- Jarrett MA, Ollendick TH. A conceptual review of the comorbidity of attention-deficit/hyperactivity disorder and anxiety: Implications for future research and practice. Clinical Psychology Review. 2008;28:1266–1280. doi: 10.1016/j.cpr.2008.05.004. [DOI] [PubMed] [Google Scholar]
- Jarrett MA, Wolff JC, Ollendick TH. Concurrent validity and informant agreement of the ADHD module of the Anxiety Disorders Interview Schedule for DSM-IV. Journal of Psychopathology and Behavioral Assessment. 2007;29:159–168. doi: 10.1007/s10862-006-9041-x. [DOI] [Google Scholar]
- Jarrett MA, Wolff JC, Davis TE, III, Cowart MJ, Ollendick TH. Characteristics of children with ADHD and comorbid anxiety. Journal of Attention Disorders. 2012 doi: 10.1177/1087054712452914. Online first publication. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, Lahey BB. Parents and child contributions to diagnosis of mental disorder: Are both informants always necessary? Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(12):1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn J, Abikoff HB, Vitiello B. ADHD comorbidity findings from the MTA study: Comparing comorbid subgroups. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(2):147–158. doi: 10.1097/00004583-200102000-00009. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hollon SD, Beck A, Hammen CL, Ingram RE. Issues and recommendations regarding the use of the Beck Depression Inventory. Cognitive Therapy and Research. 1987;11(3):289–299. doi: 10.1007/BF01186280. [DOI] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, Merikangas KR. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2012;69(4):372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khune M, Schachar R, Tannock R. Impact of comorbid oppositional or conduct problems on attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(12):1715–1725. doi: 10.1097/00004583-199712000-00020. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J, Greenhill L, Hynd GW, Shaffer D. DSM-IV field trials for attention-deficit-hyperactivity disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- Lampert TL, Polanczyk G, Tramontina S, Mardini V, Rohde LA. Diagnostic performance of the CBCL Attention Problem Scale as a screening measure in a sample of Brazilian children with ADHD. Journal of Attention Disorders. 2004;8:63–71. doi: 10.1177/108705470400800204. [DOI] [PubMed] [Google Scholar]
- Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Journal of Pediatric Psychology. 2007;32(6):643–654. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]
- Marcus SC, Wan GJ, Zhang HF, Olfson M. Injury among stimulant-treated youth with ADHD. Journal of Attention Disorders. 2008;12(1):64–69. doi: 10.1177/1087054707305168. [DOI] [PubMed] [Google Scholar]
- Matthey S, Patrovski P. The Children’s Depression Inventory: Errors in cutoff scores for screening purposes. Psychological Assessment. 2002;14:146–149. doi: 10.1037/1040-3590.14.2.146. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Ames M, Cui L, Stang PE, Ustun TB, Von Korff M, Kessler RC. The impact of comorbidity of mental and physical conditions on role disability in the US adult household population. Archives of General Psychiatry. 2007;64(10):1180–1188. doi: 10.1001/archpsyc.64.10.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistis EM, McKay KE, Schulz KP, Newcorn JH, Halperin JM. Parent-teacher concordance for DSM-IV attention-deficit/hyperactivity disorder in a clinic-referred sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(3):308–313. doi: 10.1097/00004583-200003000-00012. [DOI] [PubMed] [Google Scholar]
- Murray-Close D, Hoza B, Hinshaw SP, Arnold EL, Swanson J, Jensen PS, Wells K. Developmental processes in peer problems of children with attention-deficit/hyperactivity disorder in the Multimodal Treatment Study of Children with ADHD: Developmental cascades and vicious cycles. Development and Psychopathology. 2010;22(4):785–802. doi: 10.1017/S0954579410000465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Organization of State Offices of Rural Health. Statement on reducing behavioral health disparities in rural communities. Sterling Heights, MI: 2011. [Google Scholar]
- Olfson M, Gameroff MJ, Marcus SC, Jensen PS. National trends in the treatment of attention deficit hyperactivity disorder. American Journal of Psychiatry. 2003;160:1071–1077. doi: 10.1176/appi.ajp.160.6.1071. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA, Massetti GA. Evidence-based assessment of attention-deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Puliafico AC, Comer JS, Kendall PC. Social phobia in youth: The diagnostic utility of feared social situations. Psychological Assessment. 2007;19:152–158. doi: 10.1037/1040-3590.19.1.152. [DOI] [PubMed] [Google Scholar]
- Safren SA, Lanka GB, Otto MW, Pollack MH. Prevalence of childhood ADHD among patients with generalized anxiety disorder and a comparison condition, social phobia. Depression and Anxiety. 2001;13:190–191. doi: 10.1002/da.1036.abs. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV, Child & Parent Versions. San Antonio, TX: Psychological Corporations; 1997. [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Sollie H, Larsson B, Mørch W-T. Comparison of mother, father and teacher reports of ADHD core symptoms in a sample of psychiatric outpatients. Journal of Attention Disorders. 2012;17(8):699–710. doi: 10.1177/1087054711436010. [DOI] [PubMed] [Google Scholar]
- Spiller HA, Hays HL, Aleguas A. Overdoes of drugs for attention-deficit/hyperactivity disorder: Clinical presentation, mechanism of toxicity, and management. CNS Drugs. 2013;27(7):531–543. doi: 10.1007/s40263-013-0084-8. [DOI] [PubMed] [Google Scholar]
- Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management. ADHD: Clinical practice guidelines for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tannock R. ADHD with anxiety disorders. In: Brown TE, editor. ADHD comorbidities: Handbook for ADHD complications in children and adults. Arlington, VA: American Psychiatric Publishing; 2009. pp. 131–155. [Google Scholar]
- Van Ameringen M, Mancini C, Simpson W, Patterson B. Adult attention deficit hyperactivity disorder in an anxiety disorders population. CNS Neuroscience and Therapeutics. 2011;17:221–226. doi: 10.1111/j.1755-5949.2010.00148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vance AL, Luk ES, Costin J, Tonge BJ, Pantelis C. Attention-deficit hyperactivity disorder: Anxiety phenomena in children treated with psychostimulant medication for 6 months or more. Australian and New Zealand Journal of Psychiatry. 1999;33(3):399–406. doi: 10.1046/j.1440-1614.1999.00575.x. [DOI] [PubMed] [Google Scholar]
- Weissman AS, Chu BC, Reddy LA, Mohlman J. Attention mechanisms in children with anxiety disorders and in children with attention deficit hyperactivity disorder: Implications for research and practice. Journal of Clinical Child and Adolescent Psychology. 2012;41(2):117–126. doi: 10.1080/15374416.2012.651993. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, Lahey BB. Validity of DSM-IV attention-deficit/hyperactivity disorder symptom dimensions and subtypes. Journal of Abnormal Psychology. 2012;121(4):991–1010. doi: 10.1037/a0027347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolraich ML, Lambert W, Doffing MA, Bickman L, Simmons T, Worley K. Psychometric properties of the Vanderbilt ADHD Diagnostic Parent Rating Scale in a referred population. Journal of Pediatric Psychology. 2003;28(8):559–568. doi: 10.1093/jpepsy/jsg046. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Berman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of Clinical Child and Adolescent Psychology. 2002;31(3):335–342. doi: 10.1207/153744202760082595. [DOI] [PubMed] [Google Scholar]
- Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clinical Chemistry. 1993;39:561–577. [PubMed] [Google Scholar]