Abstract
Objective
This study examined the association of proximal femur shape with ipsilateral medial and lateral compartment knee OA.
Design
Radiographs were obtained from the NIH-funded Osteoarthritis Initiative. Cases of isolated radiographic lateral compartment knee OA were defined on baseline radiographs as Kellgren/Lawrence (K/L) Grade > = 2 and joint space narrowing (JSN) > 0 in the lateral compartment and JSN=0 in the medial compartment; isolated medial compartment knee OA had K/L ≥ 2 and JSN > 0 medially with JSN=0 in the lateral compartment. Controls had K/L < 2 and JSN = 0 in both compartments. Controls were frequency matched to cases by sex and 10-year age intervals. We characterized the shape of the proximal femurs on radiographs using Active Shape Modeling and determined the association of proximal femur shape with knee OA using logistic regression.
Results
There were 168 lateral compartment knee OA cases (mean BMI 29.72 ±5.26), 169 medial compartment knee OA cases (mean BMI 29.68±4.83) and 168 controls (mean BMI 26.87±4.2). Thirteen modes were derived for femur shape which described 95.5% of the total variance in proximal femur shape in the population. Modes 6, 8 and 12 were associated with prevalent lateral compartment knee OA. Medial compartment knee OA was associated with proximal femur modes 1, 5, 8, and 12.
Conclusions
Prevalent lateral and medial compartment knee OA are associated with different ipsilateral proximal femur shapes. Additional studies are needed to better define how the shape of the proximal femur influences compartment specific knee OA.
Keywords: hip, knee, osteoarthritis, shape, compartment
INTRODUCTION
Osteoarthritis (OA) is the most common form of arthritis, and afflicts at least 27 million US adults, almost 6 million more than in 1995 (1). Although estimates for prevalence vary in different studies, the National Health and Nutrition Examination Survey III found that 12% of US adults 60 years of age or older experience symptomatic knee OA (2),. Although many risk factors for knee OA have been identified, including demographics, obesity, and malalignment of the knee, very little attention has been given to the relationship between the adjacent joint of the hip and OA of the knee.
There is a scientific rationale and some evidence supporting the hypothesis that the shape of hip or pelvis is associated with compartment specific knee OA. Malalignment of the knee, which is a known risk factor for compartment specific knee OA incidence (3) and progression (4), may in part represent a manifestation of hip differences being expressed at a distance, possibly by altering loading patterns in the knee. Weidow et al reported that lateral OA of the knee was associated with a wider pelvis and shorter femoral neck in women (5). Weidow found that a smaller calculated lever arm at the hip was associated with lateral compartment knee OA, which they explained as reducing abductor moment at the hip, promoting hip adduction and consequent knee alignment becoming more valgus. Although this was a small study and was restricted to women, it does provide support for the idea that biomechanical differences in the hip and pelvis may be associated with compartment specific knee OA. There may also be less direct ways in which hip shape could be associated with knee OA. Our research group has recently reported that certain single-nucleotide polymorphisms of the FRZB gene are associated with hip shape and modify the relationship between hip shape and radiographic hip osteoarthritis (6), suggesting that complex relationships between genetic background, bone shape and knee osteoarthritis may exist.
Active Shape Modeling (ASM) is a statistical image analysis technique which divides differences in shape into modes of continuous variation which may be associated with prevalent or incident lateral compartment knee OA. This technique is one way to characterize a broad spectrum of variation of shape in the hip including some of the variations examined by Weidow and others but also going beyond those and allowing for previously impossible analyses of interactions between them (5, 7). Our research group used baseline hip radiographs and ASM to examine and identify the association of proximal femoral shape and incident radiographic hip OA (RHOA) in the Study of Osteoporotic Fractures (SOF) cohort (7). Similarly, reports at the 2009 American College of Rheumatology conference found that hip OA was associated with hip shape modes in ASM using DXA scans(8) and that ASM modes of the hip correlate with pain and functional impairment(9).
To date, there are no studies which have examined compartment-specific knee OA and its relation to femoral hip shape in a large dataset using modern statistical image analysis techniques. We hypothesized that specific shapes of the proximal femur would be independently associated with lateral and medial compartment knee OA. Given that there are differences by sex in the compartmental distribution, we also tested for differences by sex in any associations between proximal femur shape and knee OA.
METHODS
Study Subjects and Population
To test this question we used the NIH-Foundation funded Osteoarthritis Initiative (OAI) cohort. The OAI enrolled 4796 participants with or at high risk of knee OA at baseline in four clinical centers with a coordinating center at University of California, San Francisco (information available online at http://www.oai.ucsf.edu). Approval for the OAI project was given by the institutional review boards at each OAI center, and for this project at the IRB at University of California, Davis.
Selection of Cases and Non-Cases for ASM
Three groups of hip and knee pairs were selected for this study, one group with lateral knee OA, one with medial knee OA and one non-case group with no knee OA. Eligible participants had no rheumatoid arthritis, osteonecrosis or amputation, and the knee had not been replaced. Similarly, eligible hips had no surgical replacement or fracture. Case knees were selected weighted back to the OAI population based on sex and age in ten year intervals (45-54 years /Female, 45-54 years/male, 55-64 years/female, 55-64 years/male, 65-79 years/female, 65-79 years/male). Control knees were frequency matched by sex and by age in the same 10 year intervals. Participants were eliminated if either the pelvic film or the knee film were of poor quality or if there were uninterpretable anatomy due to the proximal femur or knee projecting out of the film’s field. The final analytic sample included 506 knees with ipsilateral hip shape modes and knee OA status data available. There were 168 knees without medial or lateral knee OA, 169 knees with lateral knee OA and 169 knees with medial knee OA.
Radiography
Bilateral fixed-flexion posterior-anterior radiographs taken in plexiglass fixed-frame positioning were obtained at baseline and were read centrally by two experienced readers with musculoskeletal training with disagreements adjudicated. These radiographs provided Kellgren/Lawrence grade (K/L grade, scale from 0 to 4 (10)) and joint space narrowing (JSN; scale 0-4) by compartment for all knees within OAI. K/L grade is registered as a knee-level variable. JSN is recorded and treated separately for each compartment (medial and lateral). The cross-sectional K/L grade scores had a kappa of 0.7. Medial JSN scores had a kappa of 0.75 and lateral JSN scores had a kappa of 0.75. Antero-posterior pelvic films were acquired standing, using a special frame to keep both limbs in 10 degrees of internal rotation, and these pelvic films provided the radiographs from which proximal femoral shape was determined.
Definition of Compartment-Specific Osteoarthritis
Lateral compartment knee OA was defined as a knee having a K/L grade ≥2 along with JSN > 0 in the lateral compartment with JSN=0 in the medial compartment. Medial compartment knee OA was defined as K/L ≥2 with JSN > 0 in the medial compartment and JSN=0 in the lateral compartment. Non-cases were defined as having K/L < 2 and JSN=0 in all compartments.
Active Shape Modeling (ASM)
We utilized ASM methods similar those described in previous publications (7, 11). Two readers outlined the shape of the proximal femoral head and neck on digitized x-rays from the OAI by guiding the placement of 60 points along the hip from the lesser trochanter to the opposite side of the femoral shaft using a standardized algorithm (7, 12). Two landmark points were defined at the inferior margin of the lesser trochanter and the point on the lateral contour of the femoral shaft that is perpendicular to the femoral shaft axis. Two more landmark points were defined on the femoral neck, perpendicular to the femoral neck axis, where the femoral neck width is the narrowest. Hip shapes were 10 evenly spaced points between the lesser trochanter and inferior neck landmarks, 30 evenly spaced points between the inferior and superior neck landmark, and 20 evenly spaced points between the superior neck and lateral femoral shaft landmarks. A total of 1096 hips derived from both ipsilateral and contralateral hips (right hips mirrored to match left hips) from all analyzed participants of both case groups and control group together were used to generate a composite proximal femur shape to be used as the reference shape for measuring modes of variation from this reference. We obtained measurements of the hip shape for the cases and controls using principal components analysis, obtaining sufficient modes of variation in hip shape to account for more than 95% of the total variance in hip shape in this population. Each mode was independent of each of the other modes. We subsequently evaluated whether the modes of variation in the proximal femur shape differ in individuals with lateral compartment OA compared to controls and in individuals with medial compartment OA compared to the same controls by evaluating modes as independent predictors of prevalent OA in a logistic regression model.
Reliability
Reliability was assessed in two different ways. Inter-reader agreement on point placement within 2 millimeters (mm) was 83% and 93% on point placement within 3 mm measured on 54 hip radiographs outlined by the two readers. Inter-reader ICC for individual modes ranged from 67% to 96%. Intra-reader reliability on a repeated sample of the total sample was 89% for point placement within 2 mm and was 95% for point placement within 3 mm on 65 hips for reader 1 (KLT) and was 82% for point placement within 2 mm and 92% for point placement within 3 mm on 51 hips for reader 2 (LK). ICC for individual modes ranged from 87% to 97% for reader 1 and ranged from 73% to 96% for reader 2. These results are similar to those reported in the literature for this type of ASM assessment (7).
Adjustment Variables
Age, race, clinic site and body mass index (BMI) were evaluated at the baseline visit in OAI, the first three by questionnaire, and BMI by measurement of height and weight.
Statistical Methods
We compared the characteristics of subjects among the isolated lateral and medial knee OA cases and non-cases using analysis of variance (ANOVA) for normally distributed continuous variables, non-parametric Wilcoxon tests for skewed continuous variables; and chi-square tests for categorical variables. To test the association of knee OA with ipsilateral hip shape, we performed a multivariable unconditional logistic regression with “no knee OA” as the reference group. All 13 hip shape modes were entered into a single model and odds ratio for each hip shape mode was reported. Base models were adjusted for age, race, clinic site, and BMI. We chose not to adjust for alignment of the limb because it can be an outcome of knee OA and might have introduced collider bias into the analysis. Models were run using unconditional logistic regression since frequency matching for controls was done by sex and age intervals. To confirm the validity of the model, we checked to see if the model met convergence criteria. To test the overall goodness of fit of the model we used the Akaike Information Criterion (AIC). This criterion tests models with intercept only and the full model with all covariates and the hip shape modes. The model with all covariates and the hip shape modes had best overall fit. Interaction for sex with significant hip shape modes in base models was tested. Statistical analyses were completed using SAS v9.2 (SAS, Inc, Cary, North Carolina).
RESULTS
There were 168 cases of lateral compartment knee OA (mean BMI 29.72 ±5.26), 169 cases of medial compartment knee OA (mean BMI 29.68±4.83) and 168 controls (mean BMI 26.87±4.2); no participants contributed both knees to the analysis. Individuals with either medial or lateral compartment knee OA were more likely to be African American (14.3% of controls versus 27.2% of lateral cases and 26.7% of medial cases) and to have a statistically significantly higher BMI than the control group (lateral cases mean BMI 29.72 ±5.26 vs. medial cases mean BMI 29.68±4.83 vs. controls mean BMI 26.87±4.2) (Table 1).
Table 1.
Subject characteristics
| Characteristics | CATEGORY | Control Knees | Lateral Knee OA | Medial Knee OA | OVERALL | P-value |
|---|---|---|---|---|---|---|
| (N= 168) | (N= 169) | (N= 169) | (N= 506) | |||
| AGE AT ENROLLMENT | 62.93 +/− 8.54 | 63.28 +/− 8.74 | 63.31 +/− 8.95 | 63.18 +/− 8.73 | 0.9068 | |
| WHITE VS NON WHITE | 144(85.71) | 123(72.78) | 124(73.37) | 391 (77.27) | 0.006 | |
| BMI | 26.87 +/− 4.2 | 29.72 +/− 5.26 | 29.68 +/− 4.83 | 28.76 +/− 4.96 | <.0001 | |
| Sex (No.(%)) | Males | 52 (30.95) | 54 (31.95) | 50 (29.59) | 156(30.83) | 0.8942 |
| Females | 116(69.05) | 115(68.05) | 119(70.41) | 350(69.17) |
Active Shape Modeling
Active shape modeling was performed on the proximal femurs and in this population that included both cases of lateral and medial compartment knee OA and non-cases, 13 modes were derived for proximal femur shape that described 95.5% of the total variance.(Table 2). Modes 6, 8 and 12 were significantly associated with lateral compartment knee OA. Modes 1, 5, 8, and 12 were significantly associated with medial compartment knee OA.
Table 2.
Odds ratio for disease ordered by percentage of variance. Adjusted for age, race, sex, site, BMI, and all other hip shape modes.
| Lateral OA cases (N=169) vs non-cases | Medial OA cases (N=169) vs non-cases | Medial OA compared with Lateral OA | ||||
|---|---|---|---|---|---|---|
| Mode | OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value |
| 1 | 0.86(0.66–1.1) | 0.23 | 0.73(0.57–0.94) | 0.01 | 0.95(0.74–1.21) | 0.66 |
| 2 | 1.06(0.79–1.43) | 0.71 | 0.9(0.64–1.27) | 0.55 | 0.95(0.71–1.28) | 0.75 |
| 3 | 0.98(0.76–1.27) | 0.90 | 1.02(0.76–1.38) | 0.88 | 1.07(0.84–1.38) | 0.57 |
| 4 | 0.94(0.72–1.23) | 0.65 | 0.77(0.58–1.04) | 0.08 | 0.81 (0.62–1.05) | 0.10 |
| 5 | 0.86(0.66–1.12) | 0.26 | 0.7(0.53–0.91) | 0.01 | 0.77(0.6–0.97) | 0.03 |
| 6 | 1.49(1.14–1.95) | 0.004 | 1.1 (0.85–1.42) | 0.48 | 0.78(0.62–0.98) | 0.03 |
| 7 | 0.98(0.76–1.26) | 0.88 | 1.06(0.81–1.4) | 0.66 | 0.95(0.74–1.23) | 0.72 |
| 8 | 0.72(0.56–0.94) | 0.01 | 0.56 (0.42–0.73) | <.0001 | 0.7(0.55–0.89) | 0.004 |
| 9 | 1.19(0.94–1.51) | 0.15 | 1.05(0.83–1.34) | 0.68 | 0.88(0.7–1.1) | 0.26 |
| 10 | 1.03(0.81–1.31) | 0.84 | 1.26(0.98–1.63) | 0.08 | 1.22(0.97–1.53) | 0.09 |
| 11 | 1.01 (0.77–1.32) | 0.95 | 1.18(0.89–1.56) | 0.24 | 1.09(0.86–1.4) | 0.48 |
| 12 | 0.73(0.57–0.95) | 0.02 | 0.69(0.54–0.89) | 0.005 | 0.89(0.71–1.11) | 0.29 |
| 13 | 1.15(0.88–1.49) | 0.30 | 0.95(0.73–1.25) | 0.72 | 0.83(0.65–1.07) | 0.15 |
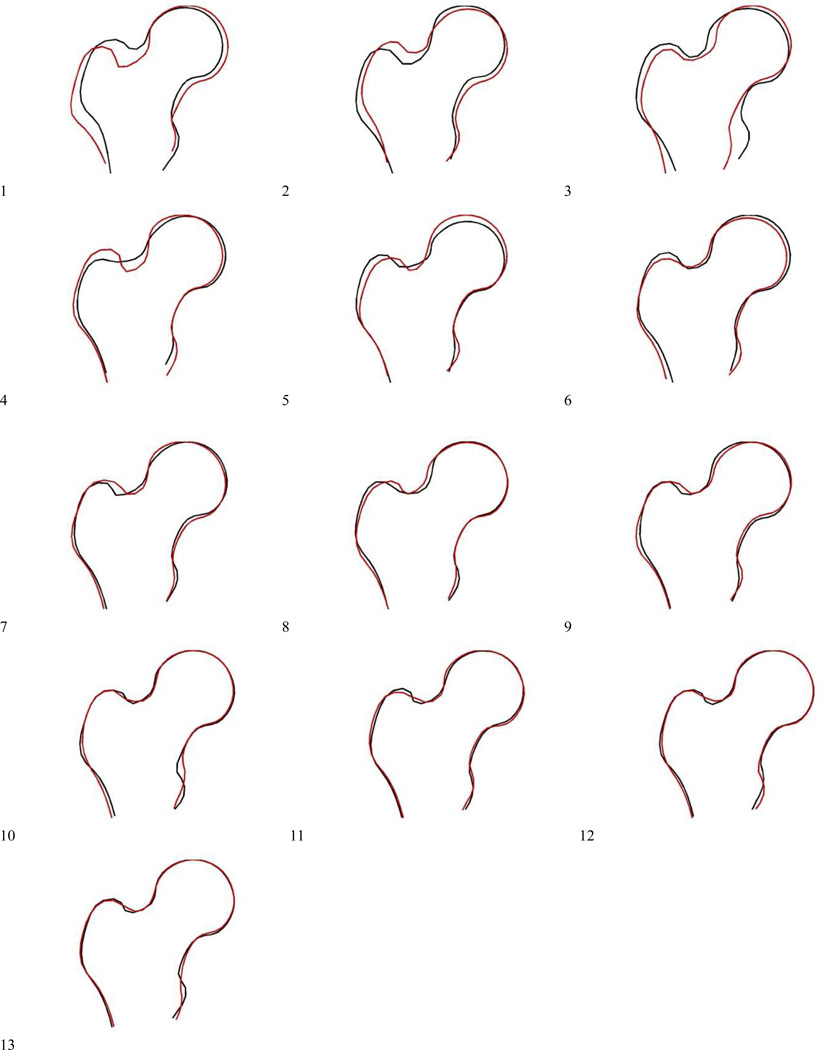
Mode 1
Mode 1 is characterized by changes in the lateral and superior extension of the greater trochanter, the girth of the femoral neck, size of the femoral head, and axis of the femoral shaft, as can be observed in Figure 1. An increased SD of Mode 1 was associated with decreased odds of medial compartment knee OA compared with controls (OR=0.73 per +1 SD increase in Mode 1, 95% CI 0.57-0.94). Positive values of Mode 1 appear to be characterized by femoral necks shifted inferiorly with respect to the greater trochanter and femoral head, a narrower superior aspect of the greater trochanter resulting in a more acute junction with the femoral neck, a lateral aspect of the greater trochanter which protrudes more, increased size of the femoral head, and increased femoral shaft angle medially.
Figure 1.
Figures showing proximal femur shape variations by mode, with +2 SD and −2 SD displayed for each mode. (see text for details.)
Mode 5
Mode 5 is characterized by relative size and superior extension of the femoral head with respect to the femoral neck, along with changes in the lateral aspect of the greater trochanter. Increased values for Mode 5 appear as increased overall size and superior extension of the femoral head and decreased lateral protrusion of the greater trochanter relative to the neck and shaft as well as a more acute angle between the greater trochanter and the femoral neck, and were associated with decreased odds of medial compartment knee OA (OR=0.7 per +1 SD increase in Mode 5, 95% CI 0.53-0.91).
Mode 6
Positive values of mode 6 are characterized by a decrease in the superior extension of the greater trochanter relative to the femoral neck, decreased total circumference of the femoral head, broadening and shortening of the femoral neck and wider proximal femoral shafts along with increased medial protrusion of the lesser trochanter. The positive values of Mode 6 were associated with increased odds of lateral compartment knee OA (OR=1.49 per +1 SD increase in Mode 6, 95% CI 1.14-1.95).
Mode 8
Positive values in mode 8 are characterized primarily by a more medial orientation of the greater trochanter and a decrease in the protrusion of the lesser trochanters, and by an increase in the acuity of the angle where the greater trochanter meets the femoral neck as well as by a broadening and shortening of the femoral neck. Positive weightings of Mode 8 were associated with decreased odds of medial compartment knee OA (OR=0.56 per +1 SD increase in Mode 8, 95% CI 0.42-0.73) and with decreased odds of lateral compartment knee OA (OR=0.72 per +1 SD increase in Mode 8, 95% CI 0.56-0.94).
Mode 12
Positive values of mode 12 displayed a more prominent lesser trochanter and less acute angulation at the juncture of the greater trochanter and the femoral neck. Positive values of this mode were associated with decreased odds of medial compartment knee OA (OR=0.69, 95% CI 0.54-0.89) and with decreased odds of lateral compartment knee OA (OR=0.73, 95% CI 0.57-0.95).
Comparing Medial Compartment Knee OA to Lateral Compartment Knee OA
Three modes showed significant differences in their associations with medial compartment knee OA versus lateral compartment knee OA after adjustment for age, race, clinic site, and BMI. These were modes 5 (OR=0.77, 95% CI 0.6-0.97), mode 6 (OR=0.78, 95% CI 0.62-0.98), and mode 8 (OR=0.7, 95% CI 0.55-0.89). (See Table 2)
Sex Interaction
We tested for sex interaction, and none of the modes were significant, either unadjusted or adjusted for potential confounding variables.
DISCUSSION
Active shape modeling has recently been adapted to assess the two dimensional shape of both proximal and distal femurs (7, 13, 14). We determined that there were proximal femur shapes or modes that were independently related to lateral and medial compartment knee OA.
There are some shared components of shape between some modes, suggesting that the association groupings we are reporting may derive from shared component shape aspects. We observed that an increase in the angle formed by the greater trochanter with the femoral neck is associated with decreased odds of medial compartment knee OA in Modes 1 and 5 and 8, but with increased odds of medial compartment knee OA in Mode 12 (although it should be noted that this mode only accounts for 0.8% of the total variance, whereas modes 1, 5, and 7 account for 31.1%, 6.2%, and 1.8% respectively). Changes in the shape or relative size of the femoral head in Modes 1 and 5 were associated with medial compartment OA. Increases in medial protrusion of the lesser trochanter in modes 6 and 8 were associated with increased odds of lateral compartment knee OA, and in Mode 12 the variation in the shape of the lesser trochanter was more complex and difficult to characterize. It is interesting to consider whether or how these specific components of the shape differences might influence risk of compartment-specific OA. However, it is important to recognize that the modes represent complex shape variations, and risk differences may be dependent on the totality of each shape change rather on individual components of shape within each mode.
We found three modes that were associated with lateral compartment knee OA, Modes 6, 8, and 12, and all were characterized by changes in the lesser trochanter and changes in the acuity of the angle where the greater trochanter joins the femoral neck. In both modes 6 and 8, a more prominent lesser trochanter visible on the radiograph is associated with increased odds of lateral compartment knee OA; mode 12 has a complex change at the lesser trochanter that is difficult to characterize. In modes 6 and 8, the effect direction for the greater trochanter is the same, where an increase in the acuity of the angle where the greater trochanter meets the femoral neck is associated with decreased odds of lateral compartment knee OA, suggesting that this type of shape variation in the hip may have a protective effect for this type of knee OA. (Mode 12 has an opposite association, but only accounts for 0.8% of variation in shape and any effect of the greater trochanter change could be outweighed by changes at the lesser trochanter.) We also note that there is a shortening and broadening of the femoral neck in associated modes 6 and 8. Interestingly, a widening and shortening of the neck of the femur as determined by ASM was reported to be associated with incident radiographic hip OA (7).
Wise et al. determined the prevalence of isolated lateral compartment knee OA in the Multicenter Osteoarthritis Study (MOST) at the baseline visit to be 8.2% of knees had isolated lateral compartment OA, 2.2% had mixed lateral and medial, and 29.5% had isolated medial disease (15). This distribution suggests that lateral disease is a separate category from medial disease, rather than simply a late-stage sequela of medial disease. Our findings in the present study that there are different hip shape modes associated with medial and lateral compartment disease supports the concept that they are actually quite different disease entities with different associations and risk factors.
Weidow et al reported that lateral compartment tibio-femoral OA of the knee was associated with a wider pelvis and shorter femoral neck compared with medial compartment OA but longer femoral neck than normal controls (5). Although this study was small and restricted to women, it supports the concept that biomechanical differences in the hip and pelvis may be associated with lateral compartment OA. In the present study, lateral compartment knee OA was associated with a broadening and a coincident shortening of the femoral neck in significantly associated modes; however, the femoral neck length measurement used by Weidow represents the distance between the center of the femoral head and the point where the femoral shaft and femoral neck lines cross, which is not the same as the relative evaluation of femoral neck used in this study. Our results appear to confirm and extend the Weidow finding that geometry at the femoral neck/head juncture may influence lateral compartment knee OA risk. Furthermore, the present study examined both men and women and in a much larger group, expanding the nature of this confirmation. It is also worth noting that the broadening of the femoral neck in Modes 6 and 8 is something that Weidow did not examine and may have separate associations from the neck length, or may simply give a more complete understanding of the anatomy that Weidow observed. In considering the similarities and differences between Weidow’s findings and the present study, it is important to keep in mind that Weidow’s cohort was only women with advanced knee OA that were scheduled for knee replacement who were undergoing knee replacement surgery and with a high percentage of hip OA (52% of subjects with lateral knee OA and 6% of subjects with medial knee OA), all of which is quite different from the participants used in the present study.
Aspects of alignment distant from the knee itself have been demonstrated to be associated with medial compartment OA. Recently Chang et al. identified that lateral bowing of the femur was associated with (primarily medial) knee OA and this differed between sexes in a Korean population (16). There have also been other studies that have suggested that an association between hip OA and knee OA. Recently Sayre et al studied the Johnston County cohort (n=3068) and reported a moderate cross-sectional association between hip OA and knee OA (odds ratios varying from 1.4 to 1.8 depending on model) (17) . Given that we previously found an association between hip shape and hip OA (7), the Sayre report supports the notion that changes in hip shape may predispose to both hip and indirectly to knee OA through as-yet unidentified mechanisms. Kim et al reported that in Koreans the “femoral intermedullary guide angle” is associated with coronal femoral bowing (18). The shapes that we report encompass other elements of shape in addition to this angle. There are large variations in shape of the entire femur all of which may be associated with a variety of outcomes, but in the present paper we have focused on local shape of the proximal femur. Limb length discrepancy could be potentially associated both with proximal femur shape and with knee OA. We were unable to adjust for limb length in this analysis, but this may be a consideration for future work.
The observation that the effect sizes and significance of the results in the present study did not vary by sex is interesting. Lateral compartment knee OA is much more prevalent in women than in men (15). Although the effect sizes vary slightly by sex (data not shown) there does not appear to be significant interaction by sex in those modes. This would argue that shape difference at the proximal femoral head is not an explanatory reason for prevalence differences by sex in lateral compartment knee OA.
The present study has a number of strengths including the use of the Osteoarthritis Initiative that has detailed covariate information and bilateral annual radiographs that were obtained with a very detailed protocol to insure high quality data. In addition, we used 60 landmark points to determine the proximal femur shape, vs. the 29 points used by Gregory et al. The OAI includes a large population of both men and women and both whites and African Americans, suggesting that our results are generalizable to a broad population of persons with knee OA or at high risk of the disease.
However, this study also has a number of limitations. First, two-dimensional femoral shape is a proxy for full three-dimensional shape and may or may not have important missing information. Second, although the reading of knee x-rays in OAI was standardized, elements of JSN and others may not be visible or evaluable in these films, leading to a misclassification bias. Third, there is an element of human error in the ASM reading, with unknown effects on the shapes derived. Fourth, acetabulum shape was not considered, but may contribute to the relationship between hip and knee OA. Finally, although the methods for positioning the leg for x-ray in OAI were standardized, there may still be variation in rotation of the limb that could have affected ASM shape results.
In summary, lateral compartment and medial compartment knee OA are associated with different modes of hip shape variation. The identification of modes that define the shape of the proximal femur that are associated with ipsilateral lateral or medial compartment knee OA could lead to clinical intervention to improve the prognosis for each type of disease.
ACKNOWLEDGEMENTS
The authors thank the participants in the Osteoarthritis Initiative.
This work was supported by the following funding sources: the Center for Musculoskeletal Health at University of California, Davis School of Medicine; NIH K24 AR048841 (NEL); NIH P50 AR060752 (BLW, NEL); NIH P50 AR063043 (BLW, NEL); the University of California, Davis Building Interdisciplinary Research Careers in Women’s Health Program (NIH K12HD051958) (BLW); and the Endowed Chair for Aging at University of California, Davis School of Medicine (NEL). The Osteoarthritis Initiative (OAI) is a public–private partnership comprised of 5 contracts (N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, and N01-AR-2-2262) funded by the NIH, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Pfizer, Novartis Pharmaceuticals, Merck Research Laboratories, and Glaxo-SmithKline. Private sector funding for the OAI is managed by the Foundation for the NIH.
ROLE OF THE FUNDING SOURCE
The study sponsors (National Institutes of Health) had no involvement in the analysis or interpretation of data, in the writing of the manuscript or in the decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
AUTHOR CONTRIBUTIONS
Conception and Design: BLW, JL, MCN, NEL
Analysis and Interpretation of Data: BLW, JL, FL, NP, NEL
Drafting of the Article: BLW, LK, NEL
Critical Revision of the Article for Important Intellectual Content: BLW, JL, FL, NP, MCN, NEL
Final Approval of the Article: BLW, LK, JL, FL, NP, KLT, MCN, NEL
Collection and Assembly of Data: BLW, LK, JL, FL, NP, KLT
Obtaining Funding: BLW, NEL
CONFLICT OF INTEREST
BLW has had a contract with Pfizer, Inc., for unrelated work in the last 5 years. Other authors had no competing interests.
REFERENCES
- 1.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. PubMed PMID: 18163497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes. 2001;(20):1–10. PubMed PMID: 11676466. [PubMed] [Google Scholar]
- 3.Felson DT, Niu J, Gross KD, Englund M, Sharma L, Cooke TD, Guermazi A, Roemer FW, Segal N, Goggins JM, Lewis CE, Eaton C, Nevitt MC. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis and rheumatism. 2013;65(2):355–62. doi: 10.1002/art.37726. PubMed PMID: 23203672; PubMed Central PMCID: PMC3558618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. Jama. 2001;286(2):188–95. doi: 10.1001/jama.286.2.188. PubMed PMID: 11448282. [DOI] [PubMed] [Google Scholar]
- 5.Weidow J, Mars I, Karrholm J. Medial and lateral osteoarthritis of the knee is related to variations of hip and pelvic anatomy. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2005;13(6):471–477. doi: 10.1016/j.joca.2005.01.009. PubMed PMID: 15922181. [DOI] [PubMed] [Google Scholar]
- 6.Baker-Lepain JC, Lynch JA, Parimi N, McCulloch CE, Nevitt MC, Corr M, Lane NE. Variant alleles of the Wnt antagonist FRZB are determinants of hip shape and modify the relationship between hip shape and osteoarthritis. Arthritis and rheumatism. 2012;64(5):1457–1465. doi: 10.1002/art.34526. Epub 2012/05/01. PubMed PMID: 22544526; PubMed Central PMCID: PMC3340442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch JA, Parimi N, Chaganti RK, Nevitt MC, Lane NE. The association of proximal femoral shape and incident radiographic hip OA in elderly women. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2009;17(10):1313–1318. doi: 10.1016/j.joca.2009.04.011. PubMed PMID: 19427402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoshida KGJ, Barr RJ, Alesci S, Aspden RM, Reid DM. TEMPORAL STRUCTURAL CHANGES IN HIP OA DETECTED BY SHAPE AND APPEARANCE MODELLING OF DXA IMAGES: A ONE-YEAR PROSPECTIVE LONGITUDINAL STUDY. Osteoarthritis and Cartilage. 2009;17(Supplement 1):S24. [Google Scholar]
- 9.Barr RJGJ, Reid DM, Aspden R, Yoshida K, Alesci S, Hosie G, Silman A, Macfarlane GJ. PREDICTING OSTEOARTHRITIS PROGRESSION TO TOTAL HIP REPLACEMENT: CAN WE DO BETTER THAN RISK FACTORS ALONE USING ACTIVE SHAPE MODELLING? Rheumatology. 2009;48(Supplement 1):i100. doi: 10.1093/rheumatology/ker382. (Abstract) [DOI] [PubMed] [Google Scholar]
- 10.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Annals of the rheumatic diseases. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. PubMed PMID: 13498604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cootes TF, Taylor CJ, Cooper DH, Graham J. Active Shape Models - Their Training and Application. Comput Vis Image Und. 1995;61(1):38–59. PubMed PMID: ISI:A1995QL13400004. [Google Scholar]
- 12.Gregory JS, Waarsing JH, Day J, Pols HA, Reijman M, Weinans H, Aspden RM. Early identification of radiographic osteoarthritis of the hip using an active shape model to quantify changes in bone morphometric features: can hip shape tell us anything about the progression of osteoarthritis? Arthritis and rheumatism. 2007;56(11):3634–3643. doi: 10.1002/art.22982. Epub 2007/10/31. PubMed PMID: 17968890. [DOI] [PubMed] [Google Scholar]
- 13.Barr RJGJ, Yoshida K, Alesci S, Reid DM, Aspden R. Knee joint shape assessed by a active shape modelling of plain radiographs is related to osteoarthritis severity. Osteoarthritis and Cartilage. 2009;17(Supplement):S200–S201. [Google Scholar]
- 14.Bredbenner TL, Eliason TD, Potter RS, Mason RL, Havill LM, Nicolella DP. Statistical shape modeling describes variation in tibia and femur surface geometry between Control and Incidence groups from the osteoarthritis initiative database. Journal of biomechanics. 2010;43(9):1780–1786. doi: 10.1016/j.jbiomech.2010.02.015. PubMed PMID: 20227696; PubMed Central PMCID: PMC2997679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wise BL, Niu J, Yang M, Lane NE, Harvey W, Felson DT, Hietpas J, Nevitt M, Sharma L, Torner J, Lewis CE, Zhang Y Multicenter Osteoarthritis (MOST) Group. Patterns of compartment involvement in tibiofemoral osteoarthritis in men and women and in whites and African Americans. Arthritis Care Res (Hoboken) 2012;64(6):847–852. doi: 10.1002/acr.21606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang CB, Choi JY, Koh IJ, Seo ES, Seong SC, Kim TK. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 18(4):530–538. doi: 10.1016/j.joca.2009.12.004. PubMed PMID: 20060951. [DOI] [PubMed] [Google Scholar]
- 17.Sayre EC, Jordan JM, Cibere J, Murphy L, Schwartz TA, Helmick CG, Renner JB, Rahman MM, Aghajanian J, Kang W, Badley EM, Kopec JA. Quantifying the association of radiographic osteoarthritis in knee or hip joints with other knees or hips: the Johnston County Osteoarthritis Project. The Journal of rheumatology. 2010;37(6):1260–1265. doi: 10.3899/jrheum.091154. PubMed PMID: 20395646. [DOI] [PubMed] [Google Scholar]
- 18.Kim JM, Hong SH, Kim JM, Lee BS, Kim DE, Kim KA, Bin SI. Femoral shaft bowing in the coronal plane has more significant effect on the coronal alignment of TKA than proximal or distal variations of femoral shape. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2014 doi: 10.1007/s00167-014-3006-5. PubMed PMID: 24760162. [DOI] [PubMed] [Google Scholar]