Abstract
Endodontic and periodontal microsurgery has surpassed the success rates for traditional endodontic and periodontal surgical procedures. Excellent healing results are being attributed to both the techniques, when employed, for isolated endodontic or periodontal defects. Combined endodontic-periodontal lesions have been referred to as a true challenge, requiring not only endodontic microsurgical management but also concurrent bone grafting and membrane barriers techniques. The prevention of epithelial downgrowth and regeneration of periodontal cementum, fiber, and bone seals the fate of these cases. Achieving primary closure with submergence of grafts has a positive effect on GTR outcome. New techniques of periodontal microsurgery, such as minimally invasive papilla preserving flaps with passive internal mattress suturing, have managed to obtain 90% primary flap closure over grafted sites. Root surface treatment and conditioning has also shown to be beneficial for GTR. Endodontic microsurgery for the combined lesion has not integrated these advances yet. These advances, along with a recently suggested treatment strategy, are ushering in the level next in management of the combined lesions. This article offers an overview of the combined lesion, the disease, its classification, treatment strategy, regenerative tools, microsurgical recommendations, and outcome studies.
Keywords: Apicomarginal defect, combined endo-perio lesion, endodontic microsurgery, guided tissue regeneration
INTRODUCTION
Endodontic microsurgery has surpassed the success rates for traditional endodontic surgical procedures.[1,2,3] Kim and Kratchman have published an exhaustive review of endodontic microsurgery, quoting excellent healing rates for isolated endodontic lesions. They commented that the true challenge now is the combined endodontic-periodontal defects. The predictable and successful management of these cases requires not only endodontic microsurgical techniques but also concurrent bone grafting and membrane barriers techniques.[4] Despite quoted obstacles such as restricted field and depth, loss of visual reference points, accentuated physiologic tremor, extra time needed to develop experienced team, steep learning curve and expenses; periodontal microsurgery has also evolved significantly.[5] Microsurgical accurate incisions, gentle reflections, primary closures using papilla preservation flaps, precise flap approximations through micro suturing, root surface conditioning, root surface treatment, and improved root planning and scaling have been able to obtain better results than traditional attempts at periodontal GTR therapy.[5,6,7,8,9,10,11,12] Recently, a treatment algorithm for management of combined defects has been defined.[13] These advances should provide a better prognosis for the endodontic microsurgery of the combined lesion. This paper will briefly review the combined endodontic-periodontal defect from a clinical perspective, providing pertinent information on the disease, its treatment strategy, prognostic factors, regenerative tools, microsurgical recommendations, and prognosis.
THE COMBINED LESION
The endodontic-periodontal lesion may exist separately on the same tooth and then unite together (true combined lesion), or it may be primarily endodontic or periodontal with secondary involvement of the other.
In critical appraisal of the disease condition, Rotstein and Simon implicated living pathogens (bacteria, fungi, viruses, and infectious biofilms) and non-living pathogens (foreign bodies, HERS cells, cholesterol crystals, Russell bodies, Rushton hyaline bodies, Charcot Leyden crystals) as the etiologic factors. Contributing factors such as inadequate root canal treatment, coronal leakage, trauma, perforation, fractures, root resorption, and dental malformations (for example, palatogingival groove) were also identified.[14]
Classifications
The following serve as useful guides for pre-emption of case-specific treatment options, prognosis and effective management.
By Kim and Kratchman.[4]
Absence of periradicular lesion, no mobility, normal pocket depth, but unresolved symptoms after non-surgical therapies have been exhausted.
Presence of a small periradicular lesion in the apical quarter, clinical symptoms such as discomfort/sensitivity to percussion as sinus tract, normal periodontal probing depths, and no mobility.
Large periradicular lesions progressing coronally but without periodontal pockets and/or mobility.
Clinically similar to those in class C but with periodontal pockets >4 mm, and no communication of the pocket and the endodontic lesion.
Deep periradicular lesions with endodontic-periodontal communication to the apex, but no obvious fracture.
Apical lesion and complete denudement of the buccal plate but no mobility.
By Enrique Merino[15]
Large bone defects (LBD).
Through and through defects (TTD).
Apicomarginal bone defects (AMBD).
Lateromarginal bone defect (LMBD).
Management
After reviewing 26 case reports, demonstrating successful management of the endodontic-periodontal lesions with concomitant regenerative procedures, a four-phase treatment strategy for the combined lesion has been outlined by Oh et al.[13]
Within their treatment algorithm framework and guidelines, useful suggestions of other authors are discussed herewith. In addition, if the patients presents with an emergency (endodontic/periodontal), the emergency is treated first.[16]
Presurgical assessment
The clinician should be mindful of the ability of combined endodontic-periodontal problem to get referred to other teeth.[17] Thorough case history, clinical examination, and additional tests are done to diagnose effectively.[14,18]
Most common clinical/radiographic features of endodontic-periodontal lesions were reported as periapical radiolucency, non-vital pulp status, deep pocket depths, and minimal mobility.[13]
Need to verify non-vital pulp status, extent of periodontal destruction, coronal restoration, presence of traumatic occlusion, and vertical root fracture (VRF) [Figure 1].
Figure 1.
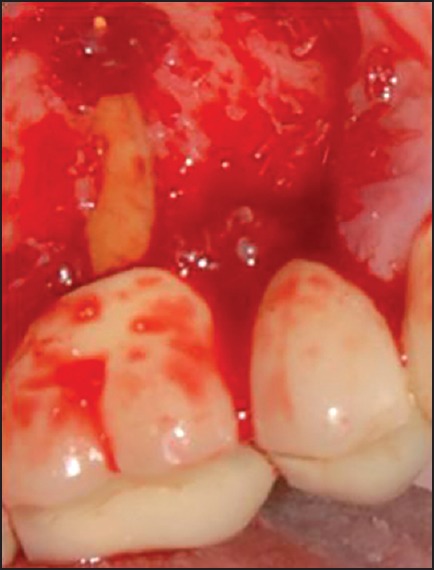
Apicomarginal defect associated with VRF
A distinction should be made between the histological and the clinical pocket depth. Tissue swelling or inflammation can lead to overestimation of pocket. A presurgical plaque control and 0.2% chlorhexidine rinse twice daily, started one week prior and continued for two weeks after the surgery helps to prevent this whilst improving healing.[19] Case-based splinting for teeth with mobility should be applied. Mobility may be caused by periodontal inflammation, loss of periodontal attachment, and functional or parafunctional forces on teeth. Occlusal therapy is undertaken to correct problems related to occlusal trauma. Temporary, provisional, or permanent, fixed or removable splints may be used to stabilize mobile teeth during surgical, especially in the regenerative phase.[20]
Bone defect morphology and VRF is better diagnosed with CBCT. Mandibular second molars and maxillary first molars and premolars are more susceptible to VRF.[21] Moule and Kahler have given a comprehensive diagnostic work-up for VRF.[22]
Prognosis of regenerative procedure should be determined.
The defect, patient, and surgery-specific factors associated with favorable periodontal regeneration are listed below.[23]
Defects
Deep, narrow, vertical, three wall defects with no/minimal furcation involvement, adequate tissue thickness (>1.1 mm) and keratinization (2 mm).
Patients
With good systemic health, stable occlusion, good oral hygiene/compliance.
Surgery
With properly designed atraumatic incision, primary closure, passive flap tension, no membrane exposure, non-disrupted wound, and sterile surgery.
The prognosis of apicomarginal defect has been reported to improve with better crown-root ratio, smaller width of dehiscence at the bone crest, and root in-housed between proximal bone margins.[15]
When periodontal lesions are chronic, with extensive loss of attachment, prognosis is poor or hopeless. Root amputation, hemisection, or bicuspidization may allow a part of tooth to be salvaged.[18] However, others claim that teeth with advanced loss may be retained through active maintenance, considering genetic, systemic, or personal risk factors and avoiding biomechanical and technical complications. It was noted that endodontically treated teeth fractured more frequently, particularly in the case of cantilever abutments. Selecting suitable post, conserving tooth structure, and providing ferrule and non-aggressive tooth cleaning protects against fracture.[24]
Sex (female), tooth position (anterior), and root end filling material (MTA and Super EBA) were found to have a positive outcome in a prospective study including endodontic-periodontal lesions.[25]
Surgeon's skill has also been considered important.[7,15]
Patient's financial commitment and esthetic demands are assessed. Possible soft tissue sequelae-like recession and scarring should be explained.[26] The better scenario is for clinician and patient to share decision-making and weighing relative benefits, risks, and costs of two or more acceptable outcomes.[15]
Endodontic phase
If prognosis for regeneration is favorable, root canal therapy follows. Combined lesion, either primary periodontal or primary endodontic in origin, has been shown to benefit from performing root canal treatment prior to regenerative periodontal treatment.[14,27] Pulpal infection may promote marginal epithelial downgrowth along a denuded dentin surface[28] or external root resorption due to possible cementum removal during periodontal treatment.[16] For primary endodontic lesion with secondary periodontal involvement, post-endodontic healing is evaluated after two to three months and only then periodontal treatment is considered. This sequence of treatment allows sufficient time for initial tissue healing, better assessment of the periodontal condition, and less potential risk of introducing bacteria and their by-products.[14]
Non-surgical retreatment has been shown to offer a more favorable long-term outcome as compared with endodontic surgery.[29] In lateral canal-based failures, if re-treatment is feasible, then a continuous ultrasonic irrigation protocol may be used for effective debridement.[30] Prognosis of root perforations would depend on the size, location, time of diagnosis and treatment, degree of periodontal damage as well as the sealing ability and biocompatibility of the repair material.[15]
It is advised to contain root fillings until level of marginal bone and extend coronal fillings until root fillings.[31]
Unsatisfactory healing after RCT is managed with root end surgery, root resection, or extraction.[18] After successful root canal therapy, mobility is reassessed to determine need for splinting.
Periodontal surgical phase
Membrane and grafting considerations
Regeneration of periapical tissues after severe injury or periapical surgery requires recruitment/differentiation of progenitor stem cells into periapical tissue committed cells, growth/differentiation factors, and local microenvironmental cues. All these factors have to work together at the right time, space, and concentration to reconstitute the architecture and functions of the damaged periapical tissues. Ability of bone graft to induce new bone is well documented, but PDL and cementum regeneration have not been shown to benefit from bone grafting.[32] Bhatushski and Wang provided an in-depth review of the available bone replacement grafts and occlusive barrier membranes. They outlined the most common methods used to obtain regeneration, i.e., bone replacement grafts (auto grafts, allografts, alloplasts, xenografts), barrier membranes (non-absorbable, absorbable of natural or synthetic type), and host-modulating agents (PRF, PRP, PDGF, PTH, EMD, BMPs, etc). They commented that although regenerative therapies have great potential, they remain unpredictable in their ability to produce acceptable outcomes consistently in all situations.[23]
Barring autogenous, bone grafts are foreign to the host's tissue and can result in delayed healing or foreign body reaction. Biologically, a blood clot is a better space filler and ECM than all bone-grafting materials.[33]
PRP, platelet-rich fibrin membrane, and platelet-rich growth factors are emerging autologous grafts that might be used with xenograft or alloplast, without a membrane.[34,35,36,37]
Wang and Boyapati proposed the PASS principle to identify critical requirements for predictable bone regeneration: Primary wound closure, angiogenesis as a source of blood supply and undifferentiated mesenchymal cells, space maintenance, and stability of the wound.[38] Rigid membranes, tenting screw, or host bone may provide space maintenance for the regenerating tissue.
Resorbable membranes score over non-resorbables in having less exposure and may remain in place despite exposure.[39] Bioresorbable membrane and alloplastic grafts have shown to have high success rates for healing of apicomarginal defects.[39,40,41,42,43]
Some clinicians may place a barrier for LBD and TTBD categories but it actually may prevent the osteoprogenitor cells from periosteum from proliferating into the wound. In addition, if there is no periodontal involvement, the gingivomucosal cells will not proliferate into the apical defect.[32] LBD (>10 mm) and TTBD have been shown to benefit from GTR therapy.[42,43] For TTBD, two resorbable membranes alone/graft filler alone/both together has also been suggested.[28]
If the buccal dehiscence is a naturally occurring one, a fibrous connective tissue attachment is present between the root surface and the mucosa, and would not require a membrane.[24] In managing in-housed apicomarginal bone defects, the periapical area does not require any graft and can regenerate by itself; for the cervical area, the gold standard technique would be to use autologous bone chips in conjunction with non-resorbable membrane. For out-housed AMBD, inner layer of autologous bone graft and outer layer of non-resorbable bone graft covered with non-resorbable membrane are recommended.[44]
For marginal periodontal defects, for non-contained shallow defects, membrane + graft + EMD + coronally placed flap will be required, it narrows down to membrane + EMD ± coronally placed flap for non-contained moderate – deep defects, finally for deep well-contained defects, EMD alone ± coronally advanced flap has been indicated.[45]
Root surface treatment
In case of a developmental malformation such as a palatal groove, saucerization is done for shallow defects (restricted to coronal portion) whilst deeper invaginated grooves are restored. Restoration may be accomplished by GIC or composite after conditioning of the groove with acid.
Trials evaluating minimally invasive surgery, using microsurgical access flap with EMD application reported predictable regeneration for intrabony periodontal defects.[7,8,9,10,11] Conversely, it was found that minimally invasive surgical technique for treatment of intrabony defects was as effective alone as with EMD.[12]
Root surface conditioning prior to EMD placement/regenerative grafting is done with neutral 24% EDTA gel for two minutes or 250 mg tetracycline HCL capsule diluted with saline, for 3 minutes.[46]
Microsurgical recommendations
Anesthesia
For adequate vasoconstriction and hemostasis, a 15-minute wait post injection is necessary.[15] In addition, profoundity of anesthesia should be ensured before operating, since tachyphylaxis may prevent effective anesthesia after patient is already experiencing pain.[47]
Magnification
Low magnification (×3-×8) is suggested for orientation to surgical field, osteotomy, alignment of tips, retropreparation, and suturing. Midrange magnification (×8-×16) is used for most procedures including hemostasis, removal of granulation tissue, detection of root tips, apicoetomy, rinsing, drying, retropreparation, and obturation. High magnification (×16-×30) is used to inspect resected root surface for details such as isthmus, cracks, and inspection prior to suturing.[15]
Micro instruments
Microsurgical instruments of 15 cm length and circular cross section are used to aid grasp, smooth rotation, and precision. Periodontal microsurgery uses needles of a fine-gauge material that are small to very small. The needle holder must be appropriately sized for the needle and suture selected.[5,6] For atraumatic retraction, retractors should be adequately wide (15 mm), thin (0.5 mm), serrated, and preferably contoured to cortex bone shapes.[15]
For obtaining intraoral graft, a bone mill, scraper, and trephine are essential. Intraoral harvesting sites are extraction sockets, edentulous ridges, ramus, symphysis, tuberosity, and buccal plate. Larger grafts are harvested from iliac crest or tibia.[23] Titanium tags serve well to fix the membranes.
Operator positioning
The surgeon's hand should directly or indirectly rest on an immovable surface to prevent physiologic tremor. Only the fingertips move.[5]
Patient positioning
Hands-free fine focus may be achieved with the operator knee adjustment under patient's headrest. When working in the anterior region, the patient's head should be tilted up or down to allow for straight-line access through the microscope. For mandibular molars, the patient closing in a slightly class III occlusion, brings the buccal surface out for better vision.[48] For maxillary posterior teeth, the patient can be tilting or lying on the opposite side with the mandible excursive on the same side; for mandibular right posterior teeth, the patient is facing slightly to the right, and for left mandibular posterior teeth, the patient lies on the right side with the head turned up.[15]
Raising the flap
With the pencil hold on scalpel, sharp complete incision should be made at 90 degrees to the tissue and bone.[9] In cases where the submucosa of the flap is joined to granulation tissue of the bone lesion without a periosteum, a blade is used to resect and obtain reflection. For harvesting autologous graft and passive graft submerging, the flap should be longer than usual.
A microsurgical, papilla-preserving flap (PPF) is highly recommended for the defect-associated papilla. In this technique, the horizontal incision of the flap is at the base of the papilla on the lingual aspect of the interproximal space and thus mobilizes the lingual and buccal papilla to the buccal. This allows the membrane and graft to be completely submerged and achieve primary closure. The simplified PPF or modified PPF are used for interdental spaces having width of less than two mm or more, respectively. Use of internal mattress sutures provides primary passive suturing of the reflected papilla.[7]
Remainder flap may be a papilla base flap with case specific vertical releasing incisions[19,49] Most periodontal microsurgical suturing is done with sutures ranging in size from 6-0 to 9-0. Until 6-0, monofilament non-resorbable sutures may be too sharp-ended and may tear flap. This is avoided from 7-0 size onwards.
Atraumatic tissue reflection and keeping reflected tissue moist aids recession-free healing. The elevation procedure should always begin from the release incision, as the surgeon first mobilizes the alveolar area. Scaling of root attached tissue and tissue tags on the cortical bone should be avoided to allow rapid reattachment and protection against bone resorption.[19] The reflected flap can be atraumatically retracted by either suturing it, placing gauze between it and the retractor, or cutting groove into the bone to rest the retractor.[26]
Osteotomy
If needed, a 5-mm osteotomy over the root apex is sufficient. If the canal cleanliness is suspect, retrocavity should be prepared up to all the negotiable canal length with ultrasonic files. This will require larger osteotomy than 5 mm. Using a trephine will help provide autologous bone for grafting.[15]
Hemostasis is obtained by curettage first and then in small defects with epinephrine pellets or ferric sulphate. Large defects benefit from calcium sulphate.[15] Root surface is scaled and planed under magnification for superior debridement,[6] prior to root resection.
Inspection
One percent methylene blue is applied on the exposed root surface and resected root end with microbrush for 10-15 seconds and then rinsed away with saline. Inspection is done at ×26 for fractures, root resection (complete outline), and anatomical details (isthmus, extra canals). Thin ultrasonic tips should be used, with light touch and copious irrigation.[50]
For retrofilling, MTA is material of choice, followed by super EBA (easier and faster). In large defects or strips, IRM is used (longer setting time). MTA may be placed in a liquid form inside the retrocavity with the tip of fine instrument, with the instrument moving up and down throughout the filling. A dry paper point then removes excess moisture, and a wet paper point removes MTA from the root end. If roots are excessively thin, retropreparation is not done and composite cap is recommended.[15]
Sutured flap is tested by movement of lips and cheeks if gaps are evident; they are closed with interrupted suture. If there is tension in reapproximating flap, releasing incision should be carried further apically.
Post-surgically, antibiotics are prescribed;[43] 0.12% chlorhexidine mouth rinsing thrice a day and weekly prophylaxis is prescribed. Patients are requested to avoid brushing, flossing, and chewing in the treated area for periods of three to four weeks. Thereafter, patients will resume full oral hygiene. After this, a three-month recall is scheduled.[7]
A post-GTR reevaluation phase
In cases with persistent pockets after GTR therapy, a second GTR procedure may be considered.[13]
Outcome studies
Many case reports using GTR for combined lesions have reported a favorable outcome.[13,51,52,53,54,55,56] Systematic reviews on outcome of endodontic microsurgeries usually exclude endodontic-periodontal combined lesion cases.[1,2] In evaluating combined lesions, evidence suggests that most case failures happen in the first year, and there is little change in status after that.[57,58] PubMed and EBSCO databases were searched using the following strategy: (“endodontic microsurgery” OR “endodontic surgery” OR “apical surgery” OR microsurgery OR “periapical surgery” OR “periradicular surgery” OR “root end surgery” OR apicoe*) AND (“GTR” OR regeneration* OR endo perio OR endo perio lesion OR “combined endo perio lesion” OR apicomarginal OR perio endo OR “perio endo lesion”) AND (study OR outcome OR success OR healing). Search limitations of English, humans, and dental journals were applied. Articles were further scanned for references of relevant studies. Only three clinical studies with minimum follow up of one year were found, which had used microsurgery with regenerative techniques. In these three studies, factors affecting prognosis such as the dimensions of buccal defect, root housed within or outside bone, crown root ratio, and mobility[15] were not defined; and papilla preservation flap, root surface conditioning, or treatment were not used. They reported a success rate of 77.5-89%, and are described below. This is far removed from the traditional hopeless category allotted to the combined lesions.
Kim et al. noted a 77.5% successful outcome for combined endodontic-periodontal lesions at five-year observation period. They excluded teeth with class II or greater mobility, horizontal, and vertical fractures, and perforations. Class F lesions received calcium sulphate graft for periradicular bone defects and denuded buccal root surface was covered with a resorbable membrane.[57]
The successful cases of the above study were further followed up for duration of six to ten years. The loss of follow up, specifically for endo-perio cases, was not reported. Among the 23 cases of combined lesion that reported for follow up, only one case had failed. The authors recommended further long-term studies with larger sample size to assess the prognosis for combined lesion.[58]
Goyal et al. studied 30 teeth with apicomarginal defects for one year and found healing between groups to be 80-88.89%. They concluded that application of PRP to these defects is a viable alternative to using a GTR membrane.[34]
A double-blind randomized clinical trial recorded similar healing results for periosteal sliding graft or a bioresorbable membrane, applied for apicomarginal defects with suppurative chronic apical periodontitis. Chronic generalized periodontitis, vertical root fractures, and advanced root resorption cases were excluded. After one year, 26 out of the 30 patients treated had completely or incompletely healed, two had uncertain healing, and two failed.[59]
CONCLUSION
The very few studies, which have applied microsurgery and GTR to carefully selected combined lesion cases, have reported a success rate of 77.5-89%. This is far-removed from the traditional hopeless category allotted to the combined lesions.
Integration with periodontal microsurgical techniques such as primary flap closures over grafted sites using papilla preservation flaps, precise flap approximations through micro suturing, root surface conditioning, and root surface treatment should help enhance these outcomes. There is a need for more such studies in this area and a need for sub-classifying the combined lesion in terms of factors such as crown root ratio, width of defect crestally, root housing in bone, and mobility to enable comparability of results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S. Outcome of endodontic surgery: A Meta — analysis of literature- part 1: Comparison of traditional root end surgery and endodontic microsurgery. J Endod. 2010;36:1757–65. doi: 10.1016/j.joen.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Tsesis I, Faivishevsky V, Kfir A, Rosen E. Outcome of surgical endodontic treatment performed by a modern technique: A meta-analysis of literature. J Endod. 2009;35:1505–11. doi: 10.1016/j.joen.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 3.Saunders WP. A prospective clinical study of periradicular surgery using mineral trioxide aggregate as a root-end filling. J Endod. 2008;34:660–5. doi: 10.1016/j.joen.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Kim S, Kratchman S. Modern endodontic surgery concepts and practice: A review. J Endod. 2006;32:601–23. doi: 10.1016/j.joen.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 5.Tibbetts LS, Shanelec D. Principles and practice of periodontal microsurgery. Int J Microdent. 2009;1:13–24. [Google Scholar]
- 6.Belcher JM. A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent. 2001;21:191–6. [PubMed] [Google Scholar]
- 7.Cortellini P, Tonetti MS. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: A novel approach to limit morbidity. J Clin Periodontol. 2007;34:87–93. doi: 10.1111/j.1600-051X.2006.01020.x. [DOI] [PubMed] [Google Scholar]
- 8.Jepsen S, Topoll H, Rengers H, Heinz B, Teich M, Hoffmann T, et al. Clinical outcomes after treatment of intra-bony defects with an EMD/synthetic bone graft orEMD alone: A multicentre randomized controlled clinical trial. J Clin Periodontol. 2008;35:420–8. doi: 10.1111/j.1600-051X.2008.01217.x. [DOI] [PubMed] [Google Scholar]
- 9.Meyle J. Papilla preservation technique with enamel matrix derivative (EMD) in the treatment of periodontis – A case report. Periodontol. 2004;1:123–9. [Google Scholar]
- 10.Fickl S, Thalmair T, Kebschull M, Böhm S, Wachtel H. Microsurgical access flap in conjunction with enamel matrix derivative for the treatment of intra-bony defects: A controlled clinical trial. J Clin Periodontol. 2009;36:784–90. doi: 10.1111/j.1600-051X.2009.01451.x. [DOI] [PubMed] [Google Scholar]
- 11.Harrel SK, Wilson TG, Jr, Nunn ME. Prospective assessment of the use of enamel matrix derivative with minimally invasive surgery: 6-year results. J Periodontol. 2010;81:435–41. doi: 10.1902/jop.2009.090393. [DOI] [PubMed] [Google Scholar]
- 12.Ribeiro FV, Casarin RC, Júnior FH, Sallum EA, Casati MZ. The role of enamel matrix derivative protein in minimally invasive surgery in intrabony defects in single rooted teeth: A randomized clinical trial. J Periodontol. 2011;82:522–32. doi: 10.1902/jop.2010.100454. [DOI] [PubMed] [Google Scholar]
- 13.Oh SL, Fouad AF, Park SH. Treatment strategy for guided tissue regeneration in combined endodontic –periodontal lesions: Case report and review. J Endod. 2009;35:1331–6. doi: 10.1016/j.joen.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Rotstein I, Simon JH. The endo- perio lesion: A critical appraisal of the disease condition. Endod Top. 2006;13:34–56. [Google Scholar]
- 15.Merino EM. 1st ed. Paris: Quintessence Publishing Co Lt; 2008. Endodontic Microsurgery; p. 9. 29, 30, 47, 66, 78. [Google Scholar]
- 16.Abbott PV, Salgado JC. Strategies for the endodontic management of concurrent endodontic and periodontal diseases. Aust Dent J. 2009;54(Suppl 1):S70–85. doi: 10.1111/j.1834-7819.2009.01145.x. [DOI] [PubMed] [Google Scholar]
- 17.Koyess E, Fares M. Referred pain: A confusing case of differential diagnosis between two teeth presenting with endo-perio problems. Int Endod J. 2006;39:724–9. doi: 10.1111/j.1365-2591.2006.01139.x. [DOI] [PubMed] [Google Scholar]
- 18.Sunitha VR, Emmadi P, Namasivayam A, Thyegarajan R, Rajaraman V. The periodontal – endodontic continuum: A review. J Conserv Dent. 2008;11:54–62. doi: 10.4103/0972-0707.44046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Velvart P, Peters CI, Peters OA. Soft tissue management: Flap design, incision, tissue elevation, and tissue retraction. Endod Top. 2005;11:78–97. [Google Scholar]
- 20.Serio FG. Clinical rationale for tooth stabilization and splinting. Dent Clin North Am. 1999;43:1–6. [PubMed] [Google Scholar]
- 21.Johnson BR, Fayad MI, Witherspoon DE. 10th ed. India: Elsevier; 2011. Cohen's Pathways of the Pulp; p. 27. [Google Scholar]
- 22.Moule AJ, Kahler B. Diagnosis and management of teeth with vertical root fractures. Aust Dent J. 1999;44:75–87. doi: 10.1111/j.1834-7819.1999.tb00205.x. [DOI] [PubMed] [Google Scholar]
- 23.Bashutski JD, Wang HL. Periodontal and endodontic regeneration. J Endod. 2009;35:321–8. doi: 10.1016/j.joen.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 24.Rühling A. Treatment strategies in the case of advanced attachment loss -part 2: Extraction of critical teeth and dental restorations on movable abutments. Periodontol. 2004;1:213–25. [Google Scholar]
- 25.Song M, Jung IY, Lee SJ, Lee CY, Kim E. Prognostic factors for clinical outcomes in endodontic microsurgery: A retrospective study. J Endod. 2011;37:927–33. doi: 10.1016/j.joen.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 26.von Arx T, Salvi GE. Incision techniques and flap designs for apical surgery in the anterior maxilla. Eur J Esthet Dent. 2008;3:110–26. [PubMed] [Google Scholar]
- 27.Kwon EY, Cho Y, Lee JY, Kim SJ, Choi J. Endodontic treatment enhances the regenerative potential of teeth with advanced periodontal disease with secondary endodontic involvement. J Periodontal Implant Sci. 2013;43:136–40. doi: 10.5051/jpis.2013.43.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blomlöf L, Lengheden A, Lindskog S. Endodontic infection and calcium hydroxide treatment. Effects on periodontal healing in mature and immature replanted monkey teeth. J Clin Periodontol. 1992;19:652–8. doi: 10.1111/j.1600-051x.1992.tb01714.x. [DOI] [PubMed] [Google Scholar]
- 29.Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: A systematic review. J Endod. 2009;35:930–7. doi: 10.1016/j.joen.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 30.Castelo-Baz P, Martin-Biedma B, Cantatore G, Ruiz-Pinon M, Bahillo J, Rivas-Mundina B, et al. In vitro comparison of passive and continuous ultrasonic irrigation in simulated lateral canals of extracted teeth. J Endod. 2012;38:688–91. doi: 10.1016/j.joen.2011.12.032. [DOI] [PubMed] [Google Scholar]
- 31.Stassen IG, Hommez GM, De Bruyn H, De Moor RJ. The relation between apical periodontitis and root-filled teeth in patients with periodontal treatment need. Int Endod J. 2006;39:299–308. doi: 10.1111/j.1365-2591.2006.01098.x. [DOI] [PubMed] [Google Scholar]
- 32.Lin L, Chen MY, Ricucci D, Rosenberg PA. Guided tissue regeneration in periapical surgery. J Endod. 2010;36:618–25. doi: 10.1016/j.joen.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 33.Cotran RS, Kumar V, Collins T. 6th ed. Philadelphia: WB Saunders; 1999. Robbin's pathologic basis of disease. [Google Scholar]
- 34.Goyal B, Tewari S, Duhan J, Sehgal PK. Comparative evaluation of platelet-rich plasma and guided tissue regeneration membrane in the healing of apicomarginal defects: A clinical study. J Endod. 2011;37:773–80. doi: 10.1016/j.joen.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 35.Lucarelli E, Beretta R, Dozza B, Tazzari PL, O’Connel SM, Ricci F, et al. A recently developed bifacial platelet-rich fibrin matrix. Eur Cell Mater. 2010;20:13–23. doi: 10.22203/ecm.v020a02. [DOI] [PubMed] [Google Scholar]
- 36.Tanya J, Thomas BS. Platelet rich fibrin membrane for recession coverage. J Dent. 2012;2:223–7. [Google Scholar]
- 37.Li Q, Pan S, Dangaria SJ, Gopinathan G, Kolokythas A, Chu S, et al. Platelet-rich fibrin promotes periodontal regeneration and enhances alveolar bone augmentation. Biomed Res Int 2013. 2013:638043. doi: 10.1155/2013/638043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang HL, Boyapati L. “PASS” principles for predictable bone regeneration. Implant Dent. 2006;15:8–17. doi: 10.1097/01.id.0000204762.39826.0f. [DOI] [PubMed] [Google Scholar]
- 39.Douthitt JC, Gutmann JL, Witherspoon DE. Histologic assessment of healing after the use of a bioresorbable membrane in the management of buccal bone loss concomitant with periradicular surgery. J Endod. 2001;27:404–10. doi: 10.1097/00004770-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Britain SK, Arx T, Schenk RK, Buser D, Nummikoski P, Cochran DL. The use of guided tissue regeneration principles in endodontic surgery for induced chronic periodontic-endodontic lesions: A clinical, radiographic, and histologic evaluation. J Periodontol. 2005;76:450–60. doi: 10.1902/jop.2005.76.3.450. [DOI] [PubMed] [Google Scholar]
- 41.Dietrich T, Zunker P, Dietrich D, Bernimoulin JP. Periapical and periodontal healing after osseous grafting and guided tissue regeneration treatment of apicomarginal defects in periradicular surgery: Results after 12 months. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:474–82. doi: 10.1067/moe.2003.39. [DOI] [PubMed] [Google Scholar]
- 42.Tsesis I, Rosen E, Tamse A, Taschieri S, Del Fabbro M. Effect of guided tissue regeneration on the outcome of surgical endodontic treatment: A systematic review and meta-analysis. J Endod. 2011;37:1039–45. doi: 10.1016/j.joen.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 43.von Arx T, Alsaeed M. The use of regenerative techniques in endodontic surgery: A literature review. Saudi Dent J. 2011;23:113–27. doi: 10.1016/j.sdentj.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Merino EM. Treatment of bone defects in apical endodontic microsurgery. ENDO (Long Engl) 2011;5:163–73. [Google Scholar]
- 45.Newman MG, Takaei H, Klokkevold PR, Carranza FA. 10th ed. Missouri: Elsevier; 2006. Carranza's clinical periodontology; pp. 982–3. [Google Scholar]
- 46.Sterrett JD, Simmons J, Whitford G, Russell CM. Tetracycline demineralization of dentin: The effects of concentraton and application time. J Clin Periodontol. 1997;24:457–63. doi: 10.1111/j.1600-051x.1997.tb00212.x. [DOI] [PubMed] [Google Scholar]
- 47.Malamed SF. 4th ed. Missouri: Mosby-Year book inc; 1997. Handbook of local anaesthesia; p. 22. [Google Scholar]
- 48.Kratchman SI. Endodontic microsurgery. Compend Contin Educ Dent. 2007;28:399–405. [PubMed] [Google Scholar]
- 49.Velvart P, Ebner-Zimmermann U, Ebner JP. Comparison of papilla healing following sulcular full-thickness flap and papilla base flap in endodontic surgery. Int Endod J. 2003;36:653–9. doi: 10.1046/j.1365-2591.2003.00693.x. [DOI] [PubMed] [Google Scholar]
- 50.Stopko J, Doyon GE, Gutmann JL. Root -end management: Resection, cavity preparation, and material placement. Endod Top. 2005;11:131–51. [Google Scholar]
- 51.Ballal NV, Jothi V, Bhat KS, Bhat KM. Salvaging a tooth with a deep palatogingival groove: An endo-perio treatment — a case report. Int Endod J. 2007;40:808–17. doi: 10.1111/j.1365-2591.2007.01289.x. [DOI] [PubMed] [Google Scholar]
- 52.Verma PK, Srivastva R, Gupta K, Srivastva A. Combined endodontic-periodontal lesion- a clinical dilemma. J Interdiscip Dent. 2011;1:119–24. [Google Scholar]
- 53.Oh SL. Mesiobuccal root resection in endodontic–periodontal combined lesions. Int Endod J. 2012;45:660–9. doi: 10.1111/j.1365-2591.2012.02020.x. [DOI] [PubMed] [Google Scholar]
- 54.Mali R, Lele P, Vishakha Guided tissue regeneration in communicating endodontal periodontic lesions- A hope for the hopeless! J Indian Soc Periodontol. 2011;15:410–3. doi: 10.4103/0972-124X.92582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Walter C, Krastl G, Weiger R. Step-wisetreatmentoftwoperiodontal-endodontic lesions in a heavy smoker. Int Endod J. 2008;41:1015–23. doi: 10.1111/j.1365-2591.2008.01458.x. [DOI] [PubMed] [Google Scholar]
- 56.Karabucak B, Setzer FC. Conventional and surgical retreatment of complex periradicular lesions with periodontal involvement. J Endod. 2009;35:1310–5. doi: 10.1016/j.joen.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 57.Kim E, Song JS, Jung IY, Lee SJ, Kim S. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod. 2008;34:546–51. doi: 10.1016/j.joen.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 58.Song M, Chung W, Lee SJ, Kim E. Long-term outcome of the cases classified as successes based on short-term follow-up in endodontic microsurgery. J Endod. 2012;38:1192–6. doi: 10.1016/j.joen.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 59.Marín-Botero ML, Domínguez-Mejía JS, Arismendi-Echavarría JA, Mesa-Jaramillo AL, Flórez-Moreno GA, Tobón-Arroyave SI. Healing response of apicomarginal defects to two guided tissue regeneration techniques in periradicular surgery: A double-blind, randomized-clinical trial. Int Endod J. 2006;39:368–77. doi: 10.1111/j.1365-2591.2006.01081.x. [DOI] [PubMed] [Google Scholar]


