Use of novel, anatomically-designed multielectrode catheters for ablation of paroxysmal atrial fibrillation(AF) has been reported1 and may potentially reduce operative times, limiting exposure to radiation. The concurrence of advances in catheter technology with the introduction of live 3-Dimensional transesophageal echocardiography (3D TEE) has potential to improve the efficiency and safety of ablation procedures. A case of AF ablation using anatomically-designed multielectrode catheters guided by live 3D TEE imaging is presented.
A 42-year-old man presented with a history of persistent AF having failed antiarrhythmic drug therapy and DC cardioversion. He subsequently underwent pulmonary vein isolation and LA ablation under general anesthesia using novel multielectrode ablation catheters with unique 3-dimensional configurations. During the procedure, live 3D TEE images were acquired with a 3-D Matrix TEE transducer (iE33 system, X7-2T transducer; Philips Medical Systems, Andover, MA, USA).
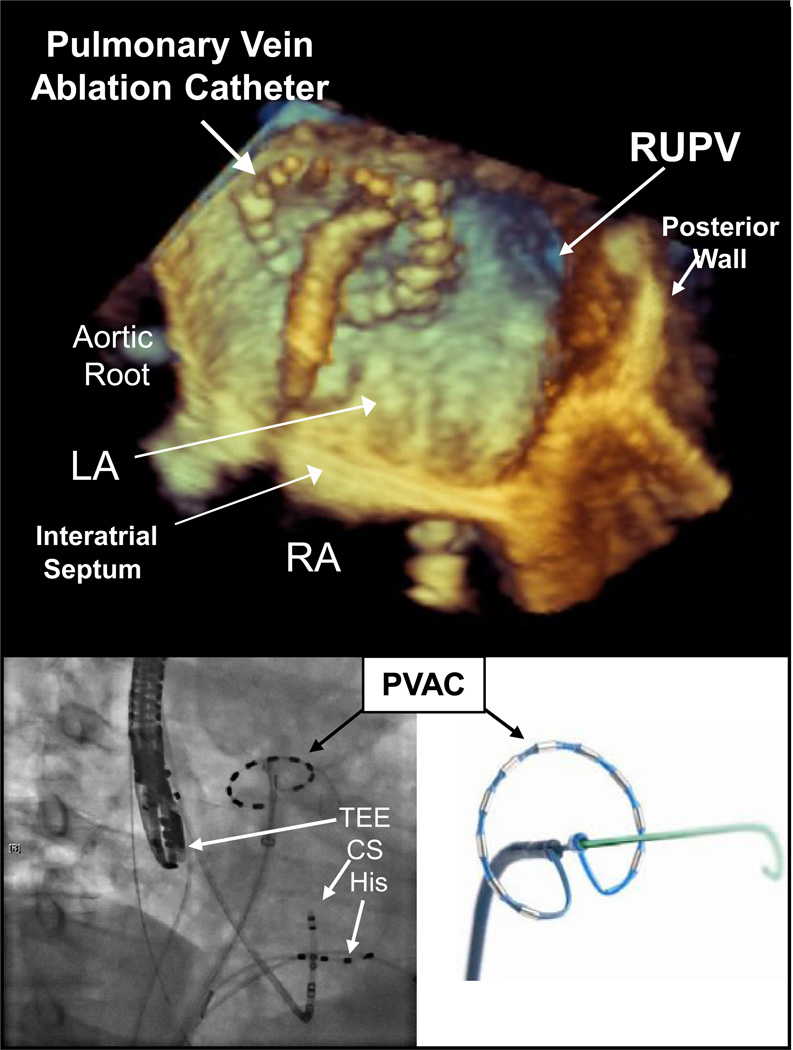
Transseptal puncture was performed with live 3D TEE imaging and fluoroscopy. Under live 3D TEE guidance, three multielectrode ablation catheters (Ablation Frontiers, Inc., Carlsbad, CA, USA) were used for ablation and mapping of the pulmonary veins, LA roof, mitral isthmus, and LA septum. Figure 1 shows a live 3-D TEE still image of the pulmonary vein ablation catheter (PVAC) in the left atrium near the right upper pulmonary vein (RUPV); the PVAC catheter is also shown ex vivo and with fluoroscopic imaging in relation to the His-bundle(HIS) and coronary sinus(CS) catheters and TEE probe. The complex configurations of the PVAC, the multi-array ablation catheter (MAAC), and the multi-array septal catheter (MASC) can be readily appreciated with live 3D TEE (see Video Attachment) and confidence during catheter placement and ablation was subjectively greatly improved.
Figure 1.
Localization of intracardiac catheters using standard 2-D echocardiography is complicated by cardiac and respiratory motion, catheter orientation, and proper identification of the catheter tip. 2-dimensional imaging is further limited in clearly defining the complex configuration and larger profile of these new multielectrode ablation catheters. In the use of multipolar ablation catheters, contact between the active electrode of the ablation catheter and the targeted cardiac tissue is an essential part of reducing risk of major complications and achieving successful ablation.1 While high resolution 3D anatomical mapping of LA anatomy can be obtained by pre-interventional MRI or CT scanning, TEE offers the only practical means of live 3D imaging of cardiac tissue during the intervention. Live 3D TEE has been used with conventional ablation catheters for real-time imaging of contact without the need for excessive manipulation during LA catheter ablation for AF;2, 3 this case demonstrates that the ability to image tissue contact with live 3D TEE is preserved with novel catheters with complex geometry.
The ability of live 3D TEE to image and guide the use of these novel catheters is evident, as is the potential for enhanced patient safety and reduced operative duration. As use of complex catheters increases, an expanding role for perioperative echocardiographers in guiding ablation procedures is anticipated.
Supplementary Material
Acknowledgements
The authors thank Scott Swenson and Ceci Canales for their assistance in the acquisition and preparation of the images presented.
Financial Support: There was no external financial support for this study. Dr. Mahajan is supported by NIH/NHLBI P01 HL078931 and NIH RO1-HL084261 grants. Dr. Shivkumar is supported by the AHA (National Affiliate (0430287N) and NIH RO1-HL084261 grants.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Boersma LV, Wijffels MC, Oral H, Wever EF, Morady F. Pulmonary vein isolation by duty-cycled bipolar and unipolar radiofrequency energy with a multielectrode ablation catheter. Heart Rhythm. 2008;5:1635–1642. doi: 10.1016/j.hrthm.2008.08.037. [DOI] [PubMed] [Google Scholar]
- 2.Mackensen GB, Hegland D, Rivera D, Adams DB, Bahnson TD. Real-time 3-dimensional transesophageal echocardiography during left atrial radiofrequency catheter ablation for atrial fibrillation. Circ Cardiovasc Imaging. 2008;1:85–86. doi: 10.1161/CIRCIMAGING.107.763128. [DOI] [PubMed] [Google Scholar]
- 3.Yang HS, Srivathsan K, Wissner E, Chandrasekaran K Images in cardiovascular medicine. Real-time 3-dimensional transesophageal echocardiography: novel utility in atrial fibrillation ablation with a prosthetic mitral valve. Circulation. 2008;117:e304–e305. doi: 10.1161/CIRCULATIONAHA.107.742148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.