Abstract
Objective:
To measure the compliance and the quality of HH practices and the knowledge of the healthcare workers’ of the university dental care center.
Materials and Methods:
All educators and students present were eligible for inclusion in the study. Each healthcare professional was observed in care situation over a period of 30 min. The knowledge, attitudes and opinions were collected through a questionnaire.
Results:
Number of healthcare professionals included was 190 (64.4%). Study group consisted of 151 students (74.4%) and 39 educators (42.4%). Out of a total number of expected disinfection of hands (993), 396 were made (39.9%). Educators had a higher compliance rates than students (63.7-35.8%, P = 10−9). Large differences were found between care situations (compliance higher before the first care to a patient and lower during installation of patient in dental X-ray area or at exit of dental X-ray area). Concerning hand rubbing (HR), 36.6% were performed correctly, and the main error was all steps of HR not observed (54.4%), and shorter duration (46.7%). The observance and the quality of HR were associated with better knowledge.
Conclusion:
This data suggests areas of improvement: (1) A comprehensive intervention including care organization/clinic ergonomics/planning/anticipation of materials needed for care; (2) the development of HH education program should include the educators, since the behavior of students is strongly influenced and formed by their mentor's attitude and behaviors.
Keywords: Compliance, dental care, hand hygiene
INTRODUCTION
Dentistry has a responsibility to adhere to scientifically accepted and evidence-based principles of infection control. This responsibility is now enforced by an increasing requirement of quality expressed by patients.[1,2] Hand hygiene (HH) in dental practice is one of the most important parts of the infection control process and is the single most important activity performed to reduce the risk of transmitting microorganisms from provider to patient.
One of the principal recommendations of HH guidelines was that waterless, alcohol-based hand rubs (HRs) (liquids or gels) are the preferred method for HH in most situations due to the superior efficacy of these agents in rapidly reducing bacterial counts on hands and their ease of use. Another widely used standard precaution is the wearing of protective gloves. Although wearing gloves offers a means of protection, it also creates a warm, moist environment in which organisms can proliferate, so HH is essential to eliminate transient microflora and decrease resident microflora, even when gloves are worn. Multiple studies have been conducted to describe the HH practices of nursing and medical students, nurses and physicians, in different countries. They concluded that compliance with HH among health care providers is as low as <40% with a baseline ranging from 5% to 89%.[3,4,5,6] Specific studies have been conducted among dental practitioners. Although HH guidelines were published >10 years ago, the extent to which dental practitioners are aware of HH protocols and use the appropriate alcohol-based hand sanitizers is relatively unknown. Some data on dentists’ knowledge, attitudes and practices regarding HH are available in Nigeria,[7] South Africa,[8] Iran,[9,10] Jordan,[11] Brazil,[12,13] Canada,[14] Soudan,[15] United Kingdom,[16,17] Germany,[18,19] United Arab Emirates,[20] Iran[21] and United States.[22] Investigators used questionnaire,[7,9,10,12,18,20,22] direct observation[13,15,16,17] and rarely questionnaire associated with direct observation.[8,11,19] The majority of the authors concluded that there is a lack of knowledge among dentists regarding the correct agents to use and the appropriate times and sequences to HH. To our knowledge, no similar data is available from France.
The main aim of this study was to observe healthcare professionals (educators, students) compliance with HH guidelines during patient care in a dental teaching hospital. Secondary aims were: (1) To measure the quality of HH procedures, (2) to identify factors influencing HH practices (3) to investigate their knowledge regarding hand washing and HR procedures and (4) to evaluate the influence of undergraduate and postgraduate HH education in HH compliance.
MATERIALS AND METHODS
The study was conducted in our dental teaching hospital, a center with providing 10 dental outpatient services, with 92 educators supervising 203 students, who operate from a total of 84 dental units. Each student undertakes a clinical training in dentistry over a period of 3 years. Preliminary teaching on infectious risk and HH techniques was given to all students before the first clinical session in the center. Since 2011 each first clinical year has received another course with practical exercises, organized by the infection control nurse and the infection control referent of the center. No continuing education program was available to educators.
Each outpatient service has a central dispensing station of all sterile devices which services treatment boxes (small, dedicated clinical treatment area). Hand washing sinks are located between the boxes, and provide liquid soap, paper hand. Bottles of alcohol HR with pumps are widely available; single use gloves are available in central dispensing station. posters describing French Society of Hospital Hygiene seven steps hygienic hand disinfection by rubbing (http://www.sf2h.net/SF2H-outils/SF2H_hygiene-des-mains_friction-des-mains_affiche.pdf) are displayed in each box.
This study was organized by the infection control committee. The aims and objectives of the study were explained to students and educators. The 2009 French guidelines were used as references for local HH procedures. The indications of HH were detailed in the chart of care, which defined precisely the moment and the type of HH to be performed.
Hand hygiene compliance rates were measured using structured observational method. Each person was observed during a continuous period of care of 30 min minimum. Data was collected using a standardized document. The succession of gestures and HH to be recorded were already used for previous studies and had been validated. A HR was classified as technically correct if the duration was 20 s or more and if 5 of the 7 steps were made, and if the quantity of product was sufficient for a complete coverage of the hand. Investigators were infection control committee members. A preliminary course was organized for investigators. An investigators guide, with all definitions and the chart of care, was prepared and provided to investigators. The major indicators measured were: The global HH compliance (HH made/HH opportunities), the frequency of technically correct HR (correct HR/HR made), and the rate of HH made, adapted to the level of risk and technically correct (perfect HH), chosen as an indicator of cross-transmission really stopped. The absence of jewelry and short sleeves was recorded. These indicators were measured for students and educators, by outpatient services and compared between different dental care situations.
Study on the knowledge, attitudes and opinions was achieved through a questionnaire (on 8 points) given to the each person observed, at the end of the clinical observation period. Educators and students were asked whether they could recall have received training, both theoretical and practical aspects in HH. A knowledge note was calculated for each person: 1 point was given for each correct reply and the note was equal to the sum on 8. Comparison of means of knowledge notes were made between formed and not formed persons and relatively to compliance and quality of practices.
The data were entered and analyzed with Epi Info 2002 (Centers for Disease Control and Prevention (CDC) Atlanta Georgia US) and SPSS V 17 software (SPSS Inc., a IBM company, US). A Mantel Haenzel Chi-square test was used for qualitative data and ANOVA for continuous data.
RESULTS
Number of health care professionals included in the study was 190 (64.4%). Total period of observation was 77 h, which mean for each individual observation 40.5 min. Study group consisted of 151 students (74.4%) and educators 39 (42.4%). This study observed 993 occurrences where HH was expected (847 for students and 146 for educators). Density HH expected (expected number of disinfections per hour) was 12.9/h.
Professional attire perfect (no jewel, no long sleeve) was found by 25.6% of educators and by 51.7% of students. Among the incorrect situations, it is shown that the watch is most often worn: By 61.5% of educators and by 31.8% of students.
The total number of expected HH was 993. The total number of HH made was 396. This gives an overall compliance rate of HH 39.9%. Educators had a much higher compliance rates than students (63.7–35.8%, P = 10−9).
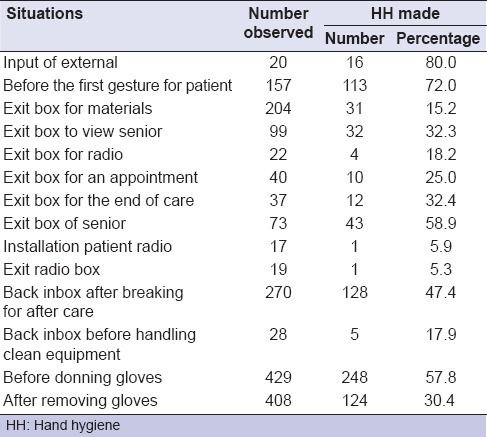
Large differences about compliance rate were found between care situations [Table 1]. Optimal compliance was seen at the beginning of clinical teaching session or when commencing clinical treatment on a patient. It was lower during installation of patient in dental X-ray area box or at exit of dental X-ray area box.
Table 1.
HH compliance according to dental care situations (all professionals)
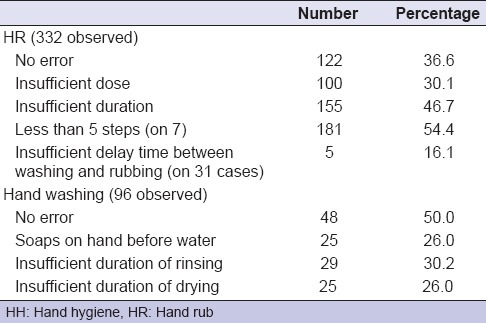
Whatever HH method expected, numerous HH were lacking [Table 2]. Furthermore, we have never observed washing, followed by rubbing when it was expected however we observed it where it was not expected. The quality of the procedure remains poor, principally in case of HR [Table 3]. Concerning HR, 36.6% were performed correctly, and among washing 50.0%. For HR, the main error sources were all steps of rubbing not observed (in 54.4% of cases), and shorter duration (in 46.7% of cases). If compliance, errors in choice of adapted procedure and quality of technic, are, take into account, only 11.1% of expected HH are made, appropriate to the situation and technically correct.
Table 2.
Adaptation of the type of HH to the dental care situation (all professionals)
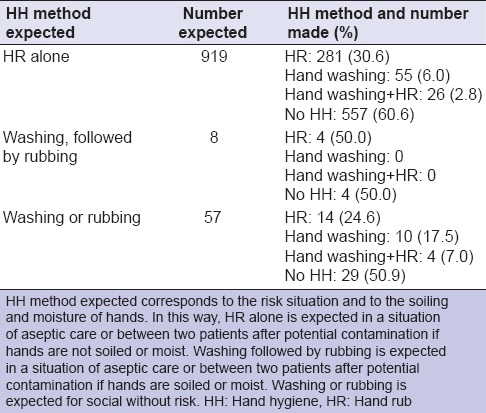
Table 3.
Quality of HH practices during dental care (all professionals)
Of the 151 students, 85 (56.3%) declared that they had been received theoretical training, and 136 (90.1%) noted that they have had a practical teaching by the infection control nurse. Of the 39 educators, two (5.1%) declared that they have received theoretical training and 13 (33.3%) that they have had a practical teaching by the infection control nurse.
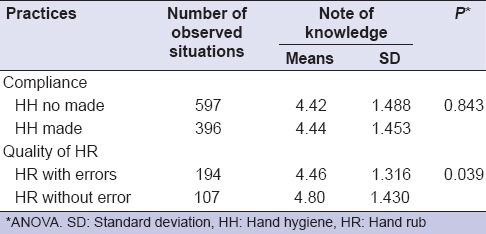
The opinions and knowledge of students and educators showed a better knowledge by the students on the specifics of HR: The rate of correct reply was significantly better by student for the items “HR is more efficient than hand washing for disinfection” and “An efficient HR is made in 7 steps,” but the knowledge notes did not differ significantly between students and educators (4.8 on 8 for students and 4.4 for teachers). Significant differences in practices were found between those who had received training, and those who had not, between persons with a teaching alone or two teaching [Tables 4 and 5], and the observance and the quality of HR have been found associated with a better knowledge [Table 6].
Table 4.
Knowledge and opinions about HH, by students and seniors
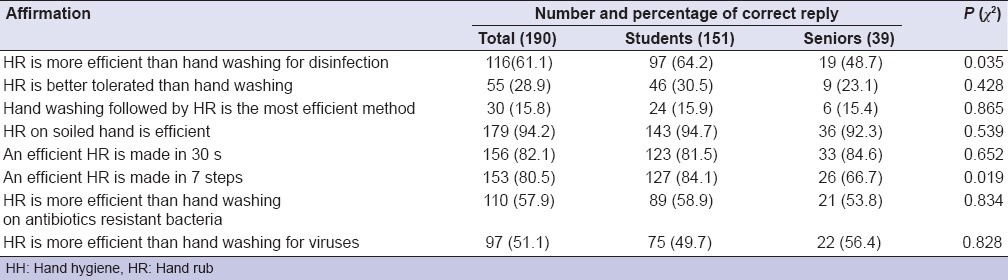
Table 5.
Comparison of knowledge note (on 8) relatively to teaching received (all professionals)
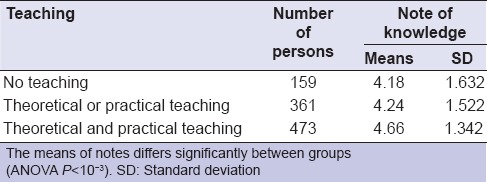
Table 6.
Relation between knowledge note (on 8) and compliance and quality of practices (all professionals)
DISCUSSION
The present study aimed to assess the undergraduate and postgraduate dental students’ and educators’ awareness and compliance for HH in a dental teaching hospital. It showed a very different compliance rate between dental clinical situations and limited quality of the HR technique. It showed also a better quality for the professionals who have benefited of a training program.
To author's knowledge, this is the first study that provides a comprehensive assessment of the HH practices and beliefs of dental health workers in France. The study on a weighty population offers robust results. Indeed, detection of HH compliance by a validated observer (direct observation) is currently considered the gold standard in HH compliance monitoring. It is the only method available to detect all occurring HH opportunities and actions and to assess the number of times and appropriate timing when HH action would be required in the sequence of care (WHO, 2009). The observation and the validation of observers were conducted according to the WHO Guidelines on HH in Health Care (part III) (2009).
In this study, the overall compliance rate with HH was only 39.9%. These results are alarming low, but on review of the literature, this is comparable from other studies. Indeed, a recent review (WHO, 2009) reported an average compliance of 38.7% with a baseline ranging from 5% to 89%. These results are inferior than many studies conducted for dental healthcare workers in countries such as Africa (25% before glowing and 47% after),[7,8] Italy (55.5%),[13] Canada (76%),[14] USA (75%)[22], Khartoum state (44%),[15] United Kingdom (26–63%).[23] Moreover, it is important to distinguish between studies undertaken in teaching and nonteaching centers, when comparing results. In studies including dental educators and students, a better HH compliance was observed in educators in any studies, and a lower rate in another.[13,23] Furthermore the methods of collecting data vary widely between studies and could explain the large differences. Studies from Canada, USA, Jordan, Africa or Germany[18] were only based on the analysis of a questionnaire about knowledge regarding HH and not for direct observations. As observed in this study, there is a limited link between knowledge and compliance.
Different causes could explain health care professional attitudes toward HH.
First, paradoxically, use of gloves may give a security perception to health care professionals. Indeed, use of gloves has been found to be a barrier to effective HH. The results confirm this data since only 57.8%, and 30.4% of observed dental workers realized correctly HH before and after use of gloves respectively [Table 1]. The results are similar as those of Edwards et al. who recorded that 40% of the dental students failed to decontaminate their hands after patient treatment[23] and as those of Omogbai et al. who concluded that only 46.7% of dental professionals washed their hands after removing torn gloves or before re-gloving.[7]
Second, interruption in care is an important cause of low compliance[24] and this frequent situation occurs during student treatment sessions. Environmental and personal barriers could explain these iterative breaks. In particular, organization with central dispensing station of all sterile devices enhances the number of student moving around the clinic and increases the risk of not following the correct HH protocol. Furthermore, the lack of rationalization of required material throughout the time of the care leads students to stop often their medical act. Finally, the low HH compliance rate observed during seating a patient for a dental X-ray and the patient leaving after the X-ray has been taken underlines the problem of displacement. The choice to follow HH protocols is often determined by whether the student considers it to be a medical/dental procedure or not.
Barriers to HH compliance are regrettable since the successful implementation of HH quality program requires that there is basic compliance with HH protocols. When there was compliance with HH, the results showed a correlation between knowledge note and quality of HR [Table 6] and tend to support the findings that HH quality improved with increasing knowledge of practice. This importance of increasing knowledge about infection control scientific data and about protocols for better compliance was demonstrated by surveys of Cheng et al. in Taiwan,[25] Cleveland et al. in US[26] and Hübner et al. in Germany.[19] They concluded that compliance depends in transmitting correct information about infection control through multiple modes of instruction such as the Internet, seminars, conferences, continuing education programs and infection control guidelines.
The presence in the center of infection control committee, and teachers well knows as infection control qualified have had a complementary effect as is was demonstrate in Cardiff.[27]
Taking together this data suggest some improvement:
An intervention focused on care organization/outpatient clinic ergonomics could have an important effect on compliance. Notably, presence of gloves and alcohol HR in each box would decrease the number of displacement and promote HH behavior
Anticipation of materials needed for care would decrease the number of interruption in care
Emphasis on HH education program would improve the quality of behavior. In particular, this HH education program have to be enlarged to teachers since the behavior of students is strongly influenced and molded by their mentor's attitude at the unit chair side.
ACKNOWLEDGMENT
We thank Pr. Guillaume MALQUARTI, who is the head of the dental teaching hospital, Mathilde PONCET, Béatrice CRACCO, Dominique DECORET, Florence CARROUEL, Sylvie IVANES, Réjane FERULLO, Katalyne DAMBAS, Sandrine FRANCOIS, Hélène GAUTHIER, Laurence BAUME, Ouiba LAMAMRA and Julian FISHER for their technical help.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Baseer MA, Rahman G, Yassin MA. Infection control practices in dental school: A patient perspective from Saudi Arabia. Dent Res J (Isfahan) 2013;10:25–30. doi: 10.4103/1735-3327.111763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Close RM, Gray S, Bennett S, Appleby S, Khan F, Payne C, et al. What are the costs and benefits of patient notification exercises following poor infection control practices in dentistry? Public Health. 2013;127:1021–7. doi: 10.1016/j.puhe.2013.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings. Recommendations of the healthcare infection control practices advisory committee and the HICPAC/SHEA/APIC/IDSA hand hygiene task force. society for healthcare epidemiology of America/Association for professionals in infection Control/Infectious diseases society of America. MMWR Recomm Rep. 2002;51:1–45. [PubMed] [Google Scholar]
- 4.Creedon SA. Healthcare workers’ hand decontamination practices: Compliance with recommended guidelines. J Adv Nurs. 2005;51:208–16. doi: 10.1111/j.1365-2648.2005.03490.x. [DOI] [PubMed] [Google Scholar]
- 5.van de Mortel TF, Apostolopoulou E, Petrikkos G. A comparison of the hand hygiene knowledge, beliefs, and practices of Greek nursing and medical students. Am J Infect Control. 2010;38:75–7. doi: 10.1016/j.ajic.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Al Kadi A, Salati SA. Hand Hygiene Practices among Medical Students. Interdiscip Perspect Infect Dis 2012. 2012:679129. doi: 10.1155/2012/679129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omogbai JJ, Azodo CC, Ehizele AO, Umoh A. Hand hygiene amongst dental professionals in a tertiary dental clinic. Afr J Clin Exp Microbiol. 2011;12:9–14. [Google Scholar]
- 8.Mehtar S, Shisana O, Mosala T, Dunbar R. Infection control practices in public dental care services: Findings from one South African Province. J Hosp Infect. 2007;66:65–70. doi: 10.1016/j.jhin.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Askarian M, Mirzaei K, McLaws ML. Attitudes, beliefs, and infection control practices of Iranian dentists associated with HIV-positive patients. Am J Infect Control. 2006;34:530–3. doi: 10.1016/j.ajic.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Askarian M, Mirzaei K, Mundy LM, McLaws ML. Assessment of knowledge, attitudes, and practices regarding isolation precautions among Iranian healthcare workers. Infect Control Hosp Epidemiol. 2005;26:105–8. doi: 10.1086/502495. [DOI] [PubMed] [Google Scholar]
- 11.AlNegrish A, Al Momani AS, Al Sharafat F. Compliance of Jordanian dentists with infection control strategies. Int Dent J. 2008;58:231–6. doi: 10.1111/j.1875-595x.2008.tb00193.x. [DOI] [PubMed] [Google Scholar]
- 12.de Melo GB, Gontijo Filho PP. Survey of the knowledge and practice of infection control among dental practitioners. Braz J Infect Dis. 2000;4:291–5. [PubMed] [Google Scholar]
- 13.de Amorim-Finzi MB, Cury MV, Costa CR, Dos Santos AC, de Melo GB. Rate of Compliance with Hand Hygiene by Dental Healthcare Personnel (DHCP) within a Dentistry Healthcare First Aid Facility. Eur J Dent. 2010;4:233–7. [PMC free article] [PubMed] [Google Scholar]
- 14.McCarthy GM, Koval JJ, MacDonald JK, John MA. The role of age- and population-based differences in the attitudes, knowledge and infection control practices of Canadian dentists. Community Dent Oral Epidemiol. 1999;27:298–304. doi: 10.1111/j.1600-0528.1998.tb02024.x. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed EE. Thesis. Dublin: Royal College of Surgeons in Ireland; 2011. Improving hand hygiene compliance among dental health workers in 3 dental clinics in Khartoum. [Google Scholar]
- 16.Scully C, Porter SR, Epstein J. Compliance with infection control procedures in a dental hospital clinic. Br Dent J. 1992;173:20–3. doi: 10.1038/sj.bdj.4807931. [DOI] [PubMed] [Google Scholar]
- 17.Porter SR, El-Maaytah M, Alfonso W, Scully C, Leung T. Cross-infection compliance of UK dental staff and students. Oral Dis. 1995;1:198–200. doi: 10.1111/j.1601-0825.1995.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 18.Vega OG, Janus C, Laskin DM. Hand-washing knowledge and practices among dentists and dental specialists. Quintessence Int. 2012;43:429–34. [PubMed] [Google Scholar]
- 19.Hübner NO, Handrup S, Meyer G, Kramer A. Impact of the “Guidelines for infection prevention in dentistry” (2006) by the Commission of Hospital Hygiene and Infection Prevention at the Robert Koch-Institute (KRINKO) on hygiene management in dental practices – Analysis of a survey from 2009. GMS Krankenhhyg Interdiszip. 2012;7:Doc14. doi: 10.3205/dgkh000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rahman B, Abraham SB, Alsalami AM, Alkhaja FE, Najem SI. Attitudes and practices of infection control among senior dental students at college of dentistry, university of Sharjah in the United Arab Emirates. Eur J Dent. 2013;7:S15–9. doi: 10.4103/1305-7456.119058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moradi Khanghahi B, Jamali Z, Pournaghi Azar F, Naghavi Behzad M, Azami-Aghdash S. Knowledge, Attitude, Practice, and Status of Infection Control among Iranian Dentists and Dental Students: A Systematic Review. J Dent Res Dent Clin Dent Prospects. 2013;7:55–60. doi: 10.5681/joddd.2013.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers R, Larson E, Cheng B, Schwartz A, Da Silva K, Kunzel C. Hand hygiene among general practice dentists: a survey of knowledge, attitudes and practices. J Am Dent Assoc. 2008;139:948–57. doi: 10.14219/jada.archive.2008.0282. [DOI] [PubMed] [Google Scholar]
- 23.Edwards G, Johnstone L, Paterson G, McIntyre J, McHugh S, Smith AJ. Hand hygiene undertaken by students and staff in a dental teaching hospital. J Hosp Infect. 2009;71:188–9. doi: 10.1016/j.jhin.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 24.Sinkowitz-Cochran RL, Burkitt KH, Cuerdon T, Harrison C, Gao S, Obrosky DS, et al. The associations between organizational culture and knowledge, attitudes and practices in multicenter Veterans Affairs quality improvement initiative to prevent methicillin-resistant Staphylococcus aureus. Am J Infect Control. 2012;40:138–143. doi: 10.1016/j.ajic.2011.04.332. [DOI] [PubMed] [Google Scholar]
- 25.Cheng HC, Su CY, Huang CF, Chuang CY. Changes in compliance with recommended infection control practices and affecting factors among dentists in Taiwan. J Dent Educ. 2012;76:1684–90. [PubMed] [Google Scholar]
- 26.Cleveland JL, Bonito AJ, Corley TJ, Foster M, Barker L, Gordon Brown G, et al. Advancing infection control in dental care settings: Factors associated with dentists’ implementation of guidelines from the Centers for Disease Control and Prevention. J Am Dent Assoc. 2012;143:1127–38. doi: 10.14219/jada.archive.2012.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lynch CD, Ash PJ, Chadwick BL. Evaluation of a community-based clinical teaching programme by current and former student dental therapists and dental hygienists: A pilot investigation. Br Dent J. 2011;210:481–5. doi: 10.1038/sj.bdj.2011.384. [DOI] [PubMed] [Google Scholar]


