Abstract
Long term clinical success of modern dental ceramics depends on a number of factors. These factors include the physical properties of the material, the laboratory fabrication process, the laboratory fabrication technique and clinical procedures that may damage these brittle materials. The surface structure and composition of a dental restorative material influences the initial bacterial adhesion, and a rough material surface will accumulate more plaque. Biomaterials for the restoration of oral function are prone to biofilm formation, affecting oral health. An up to date online database search was performed using the keywords “bacterial biofilm,” “ceramic strength,” “dental ceramics” and “surface roughness.” The searches were performed on Medline/PubMed, and Scopus and the cross references were further searched in the databases to verify further studies. The relevant papers included original articles, systemic reviews, case reports and letters to the editor. All the papers were reviewed, and the most relevant studies were selected for referencing by the author. The aim of this paper is to highlight the influence of rougher surfaces on the ceramic strength and plaque accumulation leading to bacterial biofilm formation.
Keywords: Bacterial biofilm, ceramics, strength, surface roughness
INTRODUCTION
The interest in aesthetics, biological safety, cost and the efficacy of dental care is becoming greater with time. Porcelain has excellent esthetic properties, and biocompatibility, and major emphasis in research have been directed toward the enhancement of its strength and aesthetic properties. Out of many ceramic restorations, the metal-ceramic ones are still the most commonly used restorations in fixed prosthodontics. Their use is frequent in high-stress bearing areas and in areas where restoration of multiple teeth is required.[1]
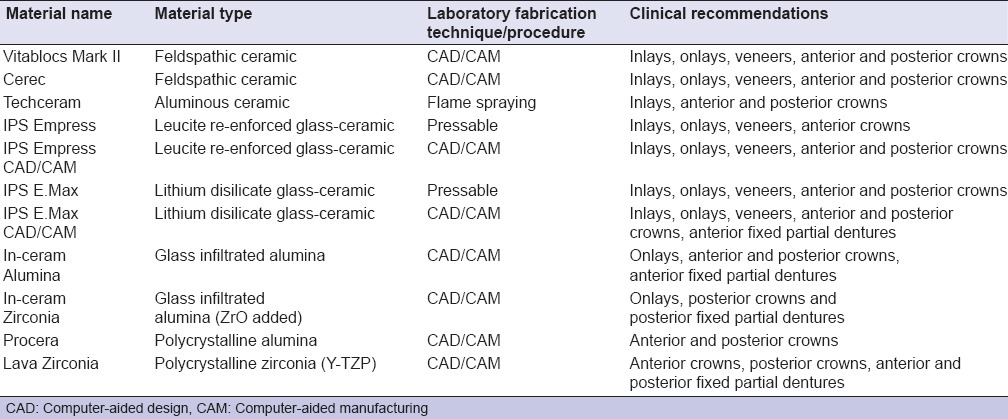
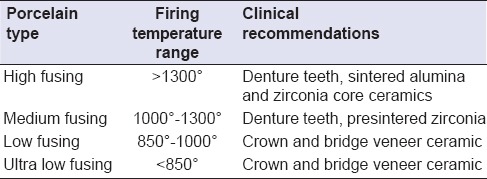
The development of all-ceramic restorative materials has seen many significant changes during the last decade. It is certainly expected that the future will bring more innovative ideas and also will bring fine tuning of the existing ceramics and existing techniques.[2] Due to the unsurpassed mechanical properties of Zirconia, its introduction to the dental market, almost a decade ago, there was considerable expansion in the range of applications of ceramics in dentistry, a field where they are classically in demand due to their chemical inertness and a wide combination of optical properties, allowing excellent esthetics. Common ceramic materials currently in dental use and their clinical recommendations are enlisted in Table 1.
Table 1.
List of all-ceramic materials, commonly used in dentistry
Zirconia (ZrO2) is a ceramic material with excellent mechanical properties with a compression resistance of about 2000 MPa. When stabilized with Y2O3, it offers the best properties for dental applications. Whenever a stress occurs on zirconia surface, a crystalline modification occurs which opposes the propagation of cracks. With fracture toughness twice or more that of alumina ceramics, transformation toughened zirconia represents an exciting potential substructure material. The invention of other all-ceramic systems like Techceram (Techceram Ltd, Shipley, UK), or any of the large number of computer-aided design/computer-aided manufacturing (CAD-CAM) systems e.g. Cerec (Siemens, Bensheim, Germany) and Procera (Nobel Biocare, Goteberg, Sweden) shows that there is an increased demand of tooth colored metal free restorations and that will certainly lead to further decrease in use of traditional cast metals used in fabrication of restorations.[3,4] Techceram all-ceramic crowns rely on a base layer that is manufactured by a ‘flame spraying’ specialist grade alumina powder onto a refractory model before sintering. The base layer is usually 0.5 mm thick for crowns and can be translucent or colored. This system is suitable for anterior and posterior single crowns and inlays and has a biaxial flexural strength of 300 Mpa. Procera, consists of high strength alumina core that is veneered using traditional porcelain. Uniform Procera copings of 0.4-0.6 mm are milled and sintered at 1600° before traditional porcelain can be added for anterior and posterior restorations. Cerec materials are available in a wide variety of shades and translucencies offering strength of 140 MPa. It has been in the market for more than 2 decades and has been routinely used to fabricate restorations including inlays, onlays, single crowns (anterior and posterior) and veneers.
Porcelain is essentially a white, translucent ceramic that is fired to a glazed state.[5] It is classified by its microstructure, processing technique and by the firing temperature. According to the firing temperature, porcelain is of ultra-low fusing, low fusing, medium fusing and high fusing type. The firing temperature ranges of dental porcelain and the clinical recommendations are enumerated in Table 2. Roughness of the porcelain can be due to certain laboratory or production reasons but may also result from chair-side modifications of the finished restoration. Finished porcelain restorations from the technical laboratory ideally should not require any changes when fitted to the patient's mouth. However, it is often necessary to adjust the occlusion for the comfort of the patient. These adjustments will then require chair side polishing to reduce the incidence of porcelain fracture, opposing tooth wear and bacterial accumulation.[6] The roughness of the intra-oral surfaces has a major impact on the initial adhesion and the retention of microorganisms, and if the roughness were sub-gingival, the retention of the microorganisms would be more.[7,8] The oral cavity is constantly contaminated by a complex diversity of microbial species that have a strong tendency to colonize surfaces. The major components involved in biofilm formation are bacterial cells, a solid surface, and a fluid medium.[9,10]
Table 2.
Firing temperature ranges of dental porcelain and their applications
Skills of the clinician and technician are important for the long-term success of a restoration. The success is also dependent on the strength of the material, its solubility in acids and the thermal its stability.[11]
FINISHING AND POLISHING OF CERAMIC RESTORATIONS
A laboratory finished ceramic restoration ideally should retain the surface glaze after it has been fitted to the abutment teeth in the oral cavity.[12,13] However, this is not always the case, and there are scenarios where adjustments are required on them. These adjustments and modifications are necessary to correct occlusal interferences and for improvements in aesthetics. A rough surface [Figure 1] will abrade the opposing dentition or restoration, and it is highly recommended that the adjusted surface is finished and polished appropriately.
Figure 1.
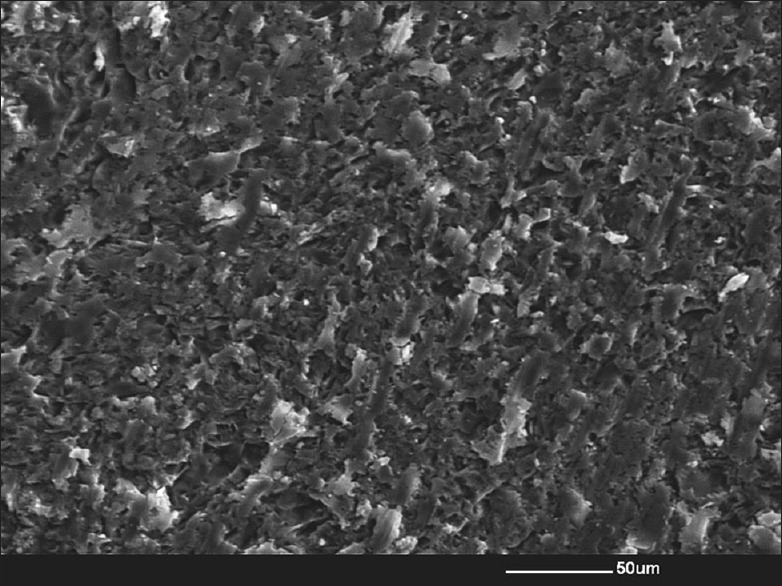
Scanning electron microscopy image of a rough ceramic surface roughened using a diamond instrument
Martínez-Gomis et al.,[14] used four different polishing techniques on a ceramic surface. Sof-lex discs white silicon, shofu polishing kit and diamond burs were used, and Sof-lex discs provided the smoothest surface finish. Odatsu et al.,[15] used carborundum points, silicone points and diamond polishing paste on zirconia and traditional feldpsathic porcelain. Feldspathic porcelain showed highest surface roughness values after finishing and polishing procedures.
The use of diamond polishing pastes for porcelain polishing in the dental office is a common practice in dentistry.[16,17] These pastes provide efficient polishing, and their use can be recommended with an appropriate vehicle. Polishing brushes, rubber cups, polishing brushes combined with abrasive pastes on tooth are the most commonly used procedures clinically.[18]
Loss of surface glaze is the usual result of the clinical intra-oral adjustment process, a situation that must be corrected by re-glazing or polishing to obtain clinical success. Surface treatments affect surface roughness and color stability, and adjusted/polished restorations could also be susceptible to staining.[19] Stainability is another important factor in the long-term clinical success of ceramic restorations. Contour adjustments on restoration surfaces cause differences in ceramic texture that may be affected differently by the staining agent. The use of appropriate polishing materials with a compatible porcelain may reduce stainability.[20,21]
THE EFFECT OF SURFACE GLAZE
Glazing of ceramic restorations is a routine laboratory procedure which involves the provision of aesthetic and hygienic glass coated surfaces to the finished restorations.[22] It is said that glazing is done to strengthen the restoration, but this is uncertain. Binns[23] stated that the process of glazing is a way of strengthening glass. However, he also has questioned the efficacy of this procedure as the surface of a dental porcelain appliance is often ground subsequent to glazing in the dental office and still provides reasonable clinical service.
The procedure of self-glazing is appropriate for the clinical use as this will provide the restoration with a smooth, hygienic surface with specimens showing better color stability.[24] Glazing as the means for strengthening brittle glass can be considered as the production of a surface layer of a thermal expansion which is lower.[25] This will serve two functions that are, it will place the surface into a compressive state, and it will also reduce the depth and width of surface flaws and will strengthen the material theoretically. However, it may be that the strength of dental porcelain is controlled by intrinsic factors rather than the surface flaws.[26]
Manipulation of porcelain requires adequate skills of laboratory technicians and fabricating porcelain crowns and bridges is highly technique sensitive. Minor laboratory faults may result in clinically unacceptable surface layers. One of the major faults as described by Rashid[27] is the formation of porosities. These porosities [Figure 2] may in turn affect the surface roughness, texture and shade. Common reasons for the formation of porosities in dental porcelain are faults during condensation, in-appropriate powder/liquid mixing ratio and due to variations in firing time and temperature.[28,29,30]
Figure 2.
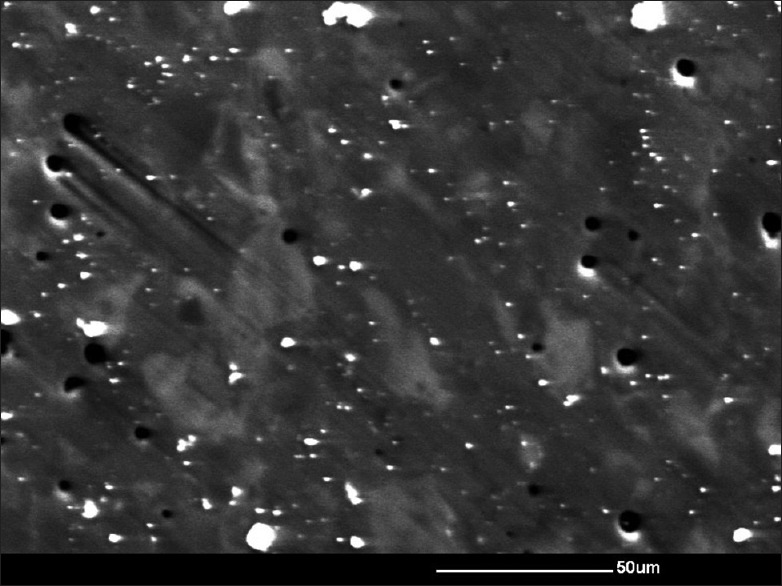
Scanning electron microscopy image of a glazed ceramic surface showing numerous porosities
STRENGTH AND SURFACE ROUGHNESS
The shape, sharpness, size, the depth of the surface flaws and internal defects determines the strength of the material.[31,32] Various techniques of polishing porcelain and glazing have been proposed to strengthen the material after the introduction of surface flaws, but it is still not clear if these measures are effective. Haralur[22] conducted a study on Vita VMK porcelain and evaluated the efficacy of Shofu polishing kit. Their results indicated that glazed surfaces showed the lowest values for surface roughness. However, Rashid[27] concluded in their study that VITA VMK glazed porcelain surfaces were rougher as compared to polished surfaces. However, both authors used different polishing techniques but used similar porcelain specimens in their investigations. Martínez-Gomis et al.[14] used different polishing techniques on a ceramic after its roughening using a diamond instrument/bur. Their investigation included the use of white polishing discs, Shofu discs and Sof-lex discs. Their results showed that Sof-lex discs produced the best finishes. Al-Shammery et al.[6] also concluded that Sof-lex discs produce best finishes on a CAD/CAM ceramic but in their study, the control group did not include glazed specimens but instead included roughened specimens. The fact that different polishing techniques may produce different results can also be explained by the fact that different systems for surface roughness evaluation have been used in different studies. The evaluating equipment included the use of scanning electron microscopy (SEM), perthometer, a tactile profilometry and confocal microscopy. These systems have different accuracies of measurements and thus may produce different results.
The strength of a porcelain material was largely determined by its surface roughness and the inner structure of the material may cause a larger stress concentration than that caused by the surface roughness in combination with the surface flaws present on the material.[33] If the material is given an adequate surface treatment, it will not require properties that stop cracking and the surface of the material would remain smooth, which in turn results in a restoration that will be long lasting.
Clinically, common problems with ceramic materials in the literature are chipping, marginal fracture and fracture of the restoration bulk.[34,35] Bulk fractures are still one of the main reason for failures, but reports have also suggested long term survival of different ceramic systems.[36,37,38] These fractures are observed throughout their clinical life. Prospective studies on zirconia ceramics have shown to give promising long time results, but authors also reported 15% chipping of the veneering ceramics.[39,40,41,42] High demands of aesthetic and biocompatible materials extend the significance of ceramics in dentistry and main emphasis of the developers around the world has been towards the improvement of the mechanical properties.
In general, ceramic strength is limited by the size and distribution of an inherent flaw population. Fracture may occur without measurable plastic deformation and failure can also start from small flaws prior to plastic deformation. This fact is expressed by a low resistance against crack extension, which is characterized by the parameter fracture toughness Kc.[43] Combination of bending and torsion forces produce surface flaws in ceramics and once critical dimensions are reached, the fracture occurs. Numerous studies have shown that catastrophic failure may occur far below the short-time fracture strength due to a slow growth of a subcritical crack up to the critical crack length.[44,45] This indicates that the strength degradation is measured during a period of a lifetime.[46] Slow crack growth is strongly influenced by the amount and composition of a glass phase in the ceramic microstructure[47] and the deleterious effect of slow crack propagation may be attributed to the stress-enhanced chemical reaction occurring in the presence of water vapor at a crack tip. This occurs preferentially in silicate base glasses resulting in bond rupture.[48] Studies indicate that even moisture levels of 0.017% may cause stress corrosion.[49] Charles[50] explained that cracks present in ceramics tend to grow at a slow rate first under the influence of stress. This slow growth of cracks continues until the intensity of stress reaches a critical value for a particular ceramic restorative material.
Several factors including powder compaction, process of forming, firing and also shaping can also cause flaws in ceramics. During these laboratory processes, the flaws may become inherited in the micro structure of the ceramic. Damage caused during grinding; pull-out caused during polishing, micro-porosity present on the subsurface and the introduction of large pores by technicians during restoration manufacture are common technical laboratory flaws.[20,51] Other flaws may be inherent which include cracking around grains with thermal expansion and porosities, which are developed during the process of ceramic firing.[52]
The failure of many materials, including ceramics, is attributed to the propagation of densely distributed cracks, rather than to a single precisely defined the fracture.[53] The number of cracks and micro cracks is extremely large, and their location and orientation are random. Irwin[54] demonstrated that stress intensity is related to a crack shape in a particular location with respect to the loading geometry. The finishing procedures influence the existence of micro cracks and residual stress. For example, glazing could round the crack tip of possible micro crack and these changes in length and tip would in turn change the strength of the material. Surface roughness will lead to a non-uniform stress distribution and concentrate locally an applied stress due to the shape differences in the surface layer.[33] Due to the presence of surface roughness, the developed cracks may not propagate randomly, but occur or propagate at points with higher stress. The theory that initiation of cracks starts at stress concentration points caused by surface roughness was given by Mecholsky et al.[55] who loaded samples with grinding grooves and gouges both perpendicular and parallel to the loading direction.
Since fabrication of conventional dental porcelains consists of a frit condensation, followed by a sintering process, thermally induced residual stresses in the material may also be introduced[56] which may cause modification of the measured biaxial flexure strength.[57,58,59] The moisture content of the veneering material during sintering might induce changes in the zirconia/veneering interface and provoke transformation from the tetragonal phase to the monoclinic phase.[60] Swain et al.[61] recognized that residual stresses and contact-induced cracking will develop chip-fracture. Beuer et al.[62] reported higher strength of CAD/CAM veneering ceramic compared to the layered veneering technique. Using of the pressed ceramic may reduce the chipping incidence,[63] since the heat pressing fabrication method would reduce the formation of large surface and flaws present in the bulk of the material. This would minimize the thermally induced residual[56,59] stresses. Greater porosities are results of human error that may occur during the fabrication stages in the dental laboratory.[64,65] The shrinkage level of the porcelain may be related to the ratio of the mixed powder/liquid veneering ceramic and minimal three firing cycles are required. Catastrophic failures may also be induced by the incorporation of small impurities like pores, since cracks cannot be healed, but slow growth may occur under oral conditions.[65,66,67]
BACTERIAL ADHESION AND BIOFILM FORMATION
The oral cavity is an open growth system.[7] Various organisms are present in the oral cavity, and they are considered to be responsible for tooth decay and infections of the oral cavity.[68] Usually, the survival of the organisms is easy when they adhere to rough surfaces in the mouth.[7,8] The roughness of intra oral surfaces has a major impact on the initial adherence and the retention of micro-organisms, and if the roughness were sub-gingival, the retention of the micro-organisms would be more.[7] SEM clearly revealed that the initial adherence and colonization on the tooth enamel started where surface irregularities were present. These surface irregularities, include cracks, grooves and abrasion defects. The colonization of bacteria then spreads out from these irregularities to other areas of teeth. Surfaces in the oral cavity such as the dorsum of the tongue roughened by presence of papilla and the desquamating epithelium of the mucosa harbors other surfaces for the adhesion of bacteria. Along with these surfaces, the enamel surface of gingival crevices and the tonsils are also believed to be the sites where bacterial adhesion occurs. Microorganisms as stated by the authors are specifically present at these sites, but they are believed to exist on all the hard and soft tissues of the oral cavity. The rough surfaces may also cause aesthetic problems at the facial surfaces. Furthermore, a rough occlusal surface is also not acceptable clinically.[6] The increase in surface roughness on fabricated ceramic restorations may result from chair-side modifications of the restoration by the clinician. These modifications are sometimes necessary for proper contouring of the restoration which includes the reduction of the proximal contour, to provide inter-proximal contact areas, adjusting the occlusal contacts and the refining of the cervical margins.
Biofilms are believed to be formed on nearly all surfaces exposed to the natural environment.[69] There is no doubt that the biofilm formation in the mouth is a well-known example and controlling its formation is an everlasting daily struggle for the researchers and for all of us. Biofilms forms on all dental hard and soft tissues and is the major cause of caries and periodontal problems.[70] It also affects the biomaterial surfaces used for the restoration of function in the oral cavity. Although, initially, the biofilm formation on biomaterial surfaces in the mouth could appear fairly harmless, dependent on its site, its consequences may be much more harmful and severe. Similar to the development of periodontitis after accumulation around the gingiva, biofilms around dental implants may lead to their infection that is, peri-implantitis.[71] A Class II filling which is overhanging and is located in the gingival margin is prone to bacterial colonization, with an impact on gingival health.[72,73,74] The surfaces of composite resins get roughened due to biofilm formation leading to their degradation.[75] The colonizing bacteria over composites, usually, invade the interface between the restoration and the tooth,[76] leading to secondary caries[77] and pulpal pathology.[78] Around the brackets during orthodontic treatment, biofilms may cause demineralization of the surrounding enamel leading to a negative side-effect of the treatment.[79,80] Consequently, the interest in new dental materials attracting less biofilm or releasing antimicrobial compounds is increasing.
Four well-defined stages of biofilm formation in the oral cavity have been described in the literature.[81,82,83,84,85,86] These are:
Stage 1: Surface transport
Brownian motion causes the initial transport of a bacterium to the surface, through sedimentation of the bacterium in the solution, through liquid flow or through active bacterial movement. Microbial aggregates may also lead to microbial transportation.
Stage 2: Initial adherence phase
This is the stage where reversible adhesion of the bacterium occurs through long-and short-range forces. The organisms will be attracted or repelled by the surface, depending on the result of non-specific interaction forces.
Stage 3: Attachment phase
Once the contact is established between bacterium and surface, a firm anchorage between bacteria and surface is established by specific interactions that are, covalent, ionic or hydrogen bonding.
Stage 4: Plaque maturation phase
When the firmly attached microorganisms start growing and newly formed cells remain attached, biofilms can develop. The growth rate of sessile microorganisms has been found to be partially depending on the biomaterial involved.
Teughels et al.[87] conducted a Medline search and summarized the data of 24 papers as follows:
Rougher surfaces of crowns, bridges, implant abutments, and denture bases accumulate and retain more plaque
After several days of undisturbed plaque formation, rough surfaces harbor a more mature plaque characterized by an increased proportion of rods, motile organisms, and spirochetes
Tooth surfaces with rough surfaces are more frequently surrounded by an inflamed periodontium, characterized by a higher bleeding index, an increased crevicular fluid production, and/or an increased inflammatory infiltrate.
It may be well-known that less plaque accumulates on ceramic or porcelain restorations; a rough surface accelerates plaque accumulation.[88] Increased amount of plaque on the rough surfaces of ceramics will exert not only caries-causing virulence, but also a harmful influence on periodontal tissue. For a full-coverage crown or a bridge, caries incidence risk would be slight, but instead much attention has to be given to the gingival tissues. Kawai et al.,[88] concluded that more plaque was adhered over glazed surfaces of ceramics as compared with their polished surfaces. This means that a glazed surface would not be clinically acceptable from a biologic point of view. Glazing can produce an undulating and rough surface that, usually, has irregularities, inducing more adhesion of bacteria and other substances. Rashid[27] also concluded that glazed surfaces are rougher as compared to the polished surfaces. Although polished surfaces have been reported to have voids and micro cracks on the subsurface of porcelain,[89] these superficial defects did not contribute to the Average Roughness (Ra) values or the amount of plaque adhesion. Contrary to other reports, polishing with diamond paste is helpful for obtaining a smoother surface that will prevent plaque from accumulating.
Hahn et al.[90] mentioned that the inlays of two ceramic types collected less plaque with reduced viability over a three-day period of no oral hygiene than did the natural tooth surface. Auschill[91] showed that biofilms on ceramic biomaterials formed in vivo during 5 days were relatively thin, but highly viable. They suggested that thick biofilms are less viable than thin ones, due to a hampered supply of nutrients to a thick biofilm. The effect of surface glazing and polishing of ceramics on early dental biofilm formation was evaluated and found that glazed surfaces tended to accumulate more biofilm compared to polished surfaces.[92] However, Bremer et al.[93] mentioned that Biofilm formation on various types of dental ceramics differed significantly; and found zirconia to exhibit low plaque accumulation.
CONCLUSION
Ceramic failure is largely influenced by the presence of densely distributed cracks present on rougher surfaces. Modification of surface finishing of ceramics influences their strength and may cause weakening of the structure. If occlusal grinding of a ceramic restoration is done after its cementation, there is always a need for careful intra-oral polishing. If adequate polishing is not done, there is also a tendency that micro-cracks are left which may cause catastrophic fractures in the future. The surface quality of dental ceramics also influences the formation of bacterial biofilm. In the oral environment, the dental plaque forms a constant threat for periodontitis and other conditions such as peri-implantitis, in susceptible individuals. The adherence of microbial species to dental ceramics and the subsequent formation of biofilms on their rough surfaces may also be contributory factors to plaque-related systemic diseases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Moffa JP. Porcelain materials. Adv Dent Res. 1988;2:3–6, 8. doi: 10.1177/08959374880020011601. [DOI] [PubMed] [Google Scholar]
- 2.Kelly JR, Benetti P. Ceramic materials in dentistry: Historical evolution and current practice. Aust Dent J. 2011;56(Suppl 1):84–96. doi: 10.1111/j.1834-7819.2010.01299.x. [DOI] [PubMed] [Google Scholar]
- 3.Shenoy A, Shenoy N. Dental ceramics: An update. J Conserv Dent. 2010;13:195–203. doi: 10.4103/0972-0707.73379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qualtrough AJ, Piddock V. Dental ceramics: what's new? Dent Update. 2002;29:25–33. doi: 10.12968/denu.2002.29.1.25. [DOI] [PubMed] [Google Scholar]
- 5.Brien O. 3rd ed. Ch 15. Chicago: Quintessence; 2002. Dental Materials and Their Selection; pp. 210–6. [Google Scholar]
- 6.Al-Shammery HA, Bubb NL, Youngson CC, Fasbinder DJ, Wood DJ. The use of confocal microscopy to assess surface roughness of two milled CAD-CAM ceramics following two polishing techniques. Dent Mater. 2007;23:736–41. doi: 10.1016/j.dental.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 7.Quirynen M, Bollen CM. The influence of surface roughness and surface-free energy on supra-and subgingival plaque formation in man. A review of the literature. J Clin Periodontol. 1995;22:1–14. doi: 10.1111/j.1600-051x.1995.tb01765.x. [DOI] [PubMed] [Google Scholar]
- 8.Quirynen M, Marechal M, Busscher HJ, Weerkamp AH, Darius PL, van Steenberghe D. The influence of surface free energy and surface roughness on early plaque formation. An in vivo study in man. J Clin Periodontol. 1990;17:138–44. doi: 10.1111/j.1600-051x.1990.tb01077.x. [DOI] [PubMed] [Google Scholar]
- 9.Gharechahi M, Moosavi H, Forghani M. Effect of surface roughness and materials composition on biofilm formation. J Biomater Nanobiotechnol. 2012;3:541–6. [Google Scholar]
- 10.Busscher HJ, Rinastiti M, Siswomihardjo W, van der Mei HC. Biofilm formation on dental restorative and implant materials. J Dent Res. 2010;89:657–65. doi: 10.1177/0022034510368644. [DOI] [PubMed] [Google Scholar]
- 11.Isgrò G, Kleverlaan CJ, Wang H, Feilzer AJ. The influence of multiple firing on thermal contraction of ceramic materials used for the fabrication of layered all-ceramic dental restorations. Dent Mater. 2005;21:557–64. doi: 10.1016/j.dental.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Boaventura JM, Nishida R, Elossais AA, Lima DM, Reis JM, Campos EA, et al. Effect finishing and polishing procedures on the surface roughness of IPS Empress 2 ceramic. Acta Odontol Scand. 2013;71:438–43. doi: 10.3109/00016357.2012.690570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flury S, Lussi A, Zimmerli B. Performance of different polishing techniques for direct CAD/CAM ceramic restorations. Oper Dent. 2010;35:470–81. doi: 10.2341/09-373-L. [DOI] [PubMed] [Google Scholar]
- 14.Martínez-Gomis J, Bizar J, Anglada JM, Samsó J, Peraire M. Comparative evaluation of four finishing systems on one ceramic surface. Int J Prosthodont. 2003;16:74–7. [PubMed] [Google Scholar]
- 15.Odatsu T, Jimbo R, Wennerberg A, Watanabe I, Sawase T. Effect of polishing and finishing procedures on the surface integrity of restorative ceramics. Am J Dent. 2013;26:51–5. [PubMed] [Google Scholar]
- 16.Haywood VB, Heymann HO, Kusy RP, Whitley JQ, Andreaus SB. Polishing porcelain veneers: An SEM and specular reflectance analysis. Dent Mater. 1988;4:116–21. doi: 10.1016/s0109-5641(88)80003-4. [DOI] [PubMed] [Google Scholar]
- 17.Camacho GB, Vinha D, Panzeri H, Nonaka T, Gonçalves M. Surface roughness of a dental ceramic after polishing with different vehicles and diamond pastes. Braz Dent J. 2006;17:191–4. doi: 10.1590/s0103-64402006000300003. [DOI] [PubMed] [Google Scholar]
- 18.Sarikaya I, Güler AU. Effects of different polishing techniques on the surface roughness of dental porcelains. J Appl Oral Sci. 2010;18:10–6. doi: 10.1590/S1678-77572010000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Motro PF, Kursoglu P, Kazazoglu E. Effects of different surface treatments on stainability of ceramics. J Prosthet Dent. 2012;108:231–7. doi: 10.1016/S0022-3913(12)60168-1. [DOI] [PubMed] [Google Scholar]
- 20.Kursoglu P, Karagoz Motro PF, Kazazoglu E. Correlation of surface texture with the stainability of ceramics. J Prosthet Dent. 2014;112:306–13. doi: 10.1016/j.prosdent.2013.09.028. [DOI] [PubMed] [Google Scholar]
- 21.Sethi S, Kakade D, Jambhekar S, Jain V. An in vitro investigation to compare the surface roughness of auto glazed, reglazed and chair side polished surfaces of Ivoclar and Vita feldspathic porcelain. J Indian Prosthodont Soc. 2013;13:478–85. doi: 10.1007/s13191-012-0223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haralur SB. Evaluation of efficiency of manual polishing over autoglazed and overglazed porcelain and its effect on plaque accumulation. J Adv Prosthodont. 2012;4:179–86. doi: 10.4047/jap.2012.4.4.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Binns D. The physical and chemical properties of dental porcelain (41-48) In: McLean JW, editor. Dental Ceramics. Proceeding of the First International Symposium on Ceramics. Chicago, USA: Quintessence Publishing; 1983. [Google Scholar]
- 24.Yilmaz C, Korkmaz T, Demirköprülü H, Ergün G, Ozkan Y. Color stability of glazed and polished dental porcelains. J Prosthodont. 2008;17:20–4. doi: 10.1111/j.1532-849X.2007.00237.x. [DOI] [PubMed] [Google Scholar]
- 25.Fairhurst CW, Lockwood PE, Ringle RD, Thompson WO. The effect of glaze on porcelain strength. Dent Mater. 1992;8:203–7. doi: 10.1016/0109-5641(92)90084-p. [DOI] [PubMed] [Google Scholar]
- 26.Corbitt G, Morena R, Fairhurst C. Fracture stress of a commercial dental porcelain and its components. J Dent Res. 1985;64:296. [Google Scholar]
- 27.Rashid H. Comparing glazed and polished ceramic surfaces using confocal laser scanning microscopy. J Adv Microscop Res. 2012;7:208–13. [Google Scholar]
- 28.Evans DB, Barghi N, Malloy CM, Windeler AS. The influence of condensation method on porosity and shade of body porcelain. J Prosthet Dent. 1990;63:380–9. doi: 10.1016/0022-3913(90)90224-z. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Y, Griggs JA, Benham AW. Influence of powder/liquid mixing ratio on porosity and translucency of dental porcelains. J Prosthet Dent. 2004;91:128–35. doi: 10.1016/j.prosdent.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 30.Cheung KC, Darvell BW. Sintering of dental porcelain: effect of time and temperature on appearance and porosity. Dent Mater. 2002;18:163–73. doi: 10.1016/s0109-5641(01)00038-0. [DOI] [PubMed] [Google Scholar]
- 31.Mencik J. Glass Science and Technology. Vol. 12. Amsterdam: Elsevier; 1992. Strength and Fracture of Glass Ceramics. [Google Scholar]
- 32.Fischer H, Schäfer M, Marx R. Effect of surface roughness on flexural strength of veneer ceramics. J Dent Res. 2003;82:972–5. doi: 10.1177/154405910308201207. [DOI] [PubMed] [Google Scholar]
- 33.de Jager N, Feilzer AJ, Davidson CL. The influence of surface roughness on porcelain strength. Dent Mater. 2000;16:381–8. doi: 10.1016/s0109-5641(00)00030-0. [DOI] [PubMed] [Google Scholar]
- 34.Molin MK, Karlsson SL. A randomized 5-year clinical evaluation of 3 ceramic inlay systems. Int J Prosthodont. 2000;13:194–200. [PubMed] [Google Scholar]
- 35.Krämer N, Frankenberger R. Clinical performance of bonded leucite-reinforced glass ceramic inlays and onlays after eight years. Dent Mater. 2005;21:262–71. doi: 10.1016/j.dental.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 36.Pallesen U, van Dijken JW. An 8-year evaluation of sintered ceramic and glass ceramic inlays processed by the Cerec CAD/CAM system. Eur J Oral Sci. 2000;108:239–46. doi: 10.1034/j.1600-0722.2000.108003239.x. [DOI] [PubMed] [Google Scholar]
- 37.Hayashi M, Wilson NH, Yeung CA, Worthington HV. Systematic review of ceramic inlays. Clin Oral Investig. 2003;7:8–19. doi: 10.1007/s00784-002-0186-z. [DOI] [PubMed] [Google Scholar]
- 38.Reiss B, Walther W. Clinical long-term results and 10-year Kaplan-Meier analysis of Cerec restorations. Int J Comput Dent. 2000;3:9–23. [PubMed] [Google Scholar]
- 39.Raigrodski AJ, Chiche GJ, Potiket N, Hochstedler JL, Mohamed SE, Billiot S, et al. The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed partial dental prostheses: A prospective clinical pilot study. J Prosthet Dent. 2006;96:237–44. doi: 10.1016/j.prosdent.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 40.Sailer I, Fehér A, Filser F, Gauckler LJ, Lüthy H, Hämmerle CH. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont. 2007;20:383–8. [PubMed] [Google Scholar]
- 41.Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H. Clinical behavior of zirconia-based fixed partial dentures made of DC-Zirkon: 3-year results. Int J Prosthodont. 2008;21:217–22. [PubMed] [Google Scholar]
- 42.Beuer F, Edelhoff D, Gernet W, Sorensen JA. Three-year clinical prospective evaluation of zirconia-based posterior fixed dental prostheses (FDPs) Clin Oral Investig. 2009;13:445–51. doi: 10.1007/s00784-009-0249-5. [DOI] [PubMed] [Google Scholar]
- 43.Munz D, Fett T. Berlin: Springer; 1999. Ceramics. [Google Scholar]
- 44.Fairhurst CW, Lockwood PE, Ringle RD, Twiggs SW. Dynamic fatigue of feldspathic porcelain. Dent Mater. 1993;9:269–73. doi: 10.1016/0109-5641(93)90073-y. [DOI] [PubMed] [Google Scholar]
- 45.Ritchie R, Dauskardt R. Cyclic fatigue of ceramics: A mechanics approach to subcritical crack growth and life prediction. J Ceram Soc Japan. 1991;99:1047–62. [Google Scholar]
- 46.Mecholsky JJ., Jr Fracture mechanics principles. Dent Mater. 1995;11:111–2. doi: 10.1016/0109-5641(95)80044-1. [DOI] [PubMed] [Google Scholar]
- 47.Bloyer DR, McNaney JM, Cannon RM, Saiz E, Tomsia AP, Ritchie RO. Stress-corrosion crack growth of Si-Na-K-Mg-Ca-P-O bioactive glasses in simulated human physiological environment. Biomaterials. 2007;28:4901–11. doi: 10.1016/j.biomaterials.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Charles R. Dynamic fatigue of glass. J Appl Phys. 1958;29:1657–62. [Google Scholar]
- 49.Wiederhorn S. Influence of water vapor on crack propagation in soda-lime-glass. J Am Ceram Soc. 1967;50:407–14. [Google Scholar]
- 50.Charles R. Static fat igue of glass. J Appl Phys. 1958;29:1549–53. [Google Scholar]
- 51.Dalkiz M, Sipahi C, Beydemir B. Effects of six surface treatment methods on the surface roughness of a low-fusing and an ultra low-fusing feldspathic ceramic material. J Prosthodont. 2009;18:217–22. doi: 10.1111/j.1532-849X.2008.00410.x. [DOI] [PubMed] [Google Scholar]
- 52.Kelly JR, Tesk JA, Sorensen JA. Failure of all-ceramic fixed partial dentures in vitro and in vivo: Analysis and modeling. J Dent Res. 1995;74:1253–8. doi: 10.1177/00220345950740060301. [DOI] [PubMed] [Google Scholar]
- 53.Bazant Z. Mechanics of distributed cracking. Appl Mech Rev. 1986;39:675–705. [Google Scholar]
- 54.Irwin G. Analysis of stresses and strains near the end of a crack transversing a plate. J Appl Mech. 1957;24:361–4. [Google Scholar]
- 55.Mecholsky J, Freiman S, Rice R. Effect of grinding on flaw geometry and fracture of glass. J Am Ceram Soc. 1977;60:114–7. [Google Scholar]
- 56.Coffey JP, Anusavice KJ, DeHoff PH, Lee RB, Hojjatie B. Influence of contraction mismatch and cooling rate on flexural failure of PFM systems. J Dent Res. 1988;67:61–5. doi: 10.1177/00220345880670011201. [DOI] [PubMed] [Google Scholar]
- 57.Isgró G, Addison O, Fleming GJ. Transient and residual stresses induced during the sintering of two dentin ceramics. Dent Mater. 2011;27:379–85. doi: 10.1016/j.dental.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 58.McLean JW, Hughes TH. The reinforcement of dental porcelain with ceramic oxides. Br Dent J. 1965;21(119):251–67. [PubMed] [Google Scholar]
- 59.Isgró G, Addison O, Fleming GJ. Transient and residual stresses in a pressable glass-ceramic before and after resin-cement coating determined using profilometry. J Dent. 2011;39:368–75. doi: 10.1016/j.jdent.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 60.Tholey MJ, Swain MV, Thiel N. SEM observations of porcelain Y-TZP interface. Dent Mater. 2009;25:857–62. doi: 10.1016/j.dental.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 61.Swain MV. Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures. Acta Biomater. 2009;5:1668–77. doi: 10.1016/j.actbio.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 62.Beuer F, Schweiger J, Eichberger M, Kappert HF, Gernet W, Edelhoff D. High-strength CAD/CAM-fabricated veneering material sintered to zirconia copings – A new fabrication mode for all-ceramic restorations. Dent Mater. 2009;25:121–8. doi: 10.1016/j.dental.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 63.Schley JS, Heussen N, Reich S, Fischer J, Haselhuhn K, Wolfart S. Survival probability of zirconia-based fixed dental prostheses up to 5 yr: A systematic review of the literature. Eur J Oral Sci. 2010;118:443–50. doi: 10.1111/j.1600-0722.2010.00767.x. [DOI] [PubMed] [Google Scholar]
- 64.Albashaireh ZS, Ghazal M, Kern M. Two-body wear of different ceramic materials opposed to zirconia ceramic. J Prosthet Dent. 2010;104:105–13. doi: 10.1016/S0022-3913(10)60102-3. [DOI] [PubMed] [Google Scholar]
- 65.Stawarczyk B, Ozcan M, Roos M, Trottmann A, Sailer I, Hämmerle CH. Load-bearing capacity and failure types of anterior zirconia crowns veneered with overpressing and layering techniques. Dent Mater. 2011;27:1045–53. doi: 10.1016/j.dental.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 66.Drummond JL. Dental Materials in vivo: Aging and Related Phenomena. IL: Quinte Chicago; 2003. Ceramic behavior under different environmental and loading conditions; pp. 35–45. [Google Scholar]
- 67.Holden JE, Goldstein GR, Hittelman EL, Clark EA. Comparison of the marginal fit of pressable ceramic to metal ceramic restorations. J Prosthodont. 2009;18:645–8. doi: 10.1111/j.1532-849X.2009.00497.x. [DOI] [PubMed] [Google Scholar]
- 68.Loesche WJ, Syed SA, Schmidt E, Morrison EC. Bacterial profiles of subgingival plaques in periodontitis. J Periodontol. 1985;56:447–56. doi: 10.1902/jop.1985.56.8.447. [DOI] [PubMed] [Google Scholar]
- 69.Moons P, Michiels CW, Aertsen A. Bacterial interactions in biofilms. Crit Rev Microbiol. 2009;35:157–68. doi: 10.1080/10408410902809431. [DOI] [PubMed] [Google Scholar]
- 70.Sbordone L, Bortolaia C. Oral microbial biofilms and plaque-related diseases: microbial communities and their role in the shift from oral health to disease. Clin Oral Invest. 2003;7:181–8. doi: 10.1007/s00784-003-0236-1. [DOI] [PubMed] [Google Scholar]
- 71.Grössner-Schreiber B, Teichmann J, Hannig M, Dörfer C, Wenderoth DF, Ott SJ. Modified implant surfaces show different biofilm compositions under in vivo conditions. Clin Oral Implants Res. 2009;20:817–26. doi: 10.1111/j.1600-0501.2009.01729.x. [DOI] [PubMed] [Google Scholar]
- 72.Jansson L, Ehnevid H, Lindskog S, Blomlöf L. Proximal restorations and periodontal status. J Clin Periodontol. 1994;21:577–82. doi: 10.1111/j.1600-051x.1994.tb00746.x. [DOI] [PubMed] [Google Scholar]
- 73.Jansson L, Blomster S, Forsgårdh A, Bergman E, Berglund E, Foss L, et al. Interactory effect between marginal plaque and subgingival proximal restorations on periodontal pocket depth. Swed Dent J. 1997;21:77–83. [PubMed] [Google Scholar]
- 74.Cenci MS, Lund RG, Pereira CL, de Carvalho RM, Demarco FF. In vivo and in vitro evaluation of Class II composite resin restorations with different matrix systems. J Adhes Dent. 2006;8:127–32. [PubMed] [Google Scholar]
- 75.Beyth N, Bahir R, Matalon S, Domb AJ, Weiss EI. Streptococcus mutans biofilm changes surface-topography of resin composites. Dent Mater. 2008;24:732–6. doi: 10.1016/j.dental.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 76.Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996;21:17–24. [PubMed] [Google Scholar]
- 77.Collins CJ, Bryant RW, Hodge KL. A clinical evaluation of posterior composite resin restorations: 8-year findings. J Dent. 1998;26:311–7. doi: 10.1016/s0300-5712(97)00019-5. [DOI] [PubMed] [Google Scholar]
- 78.Pashley DH. Clinical considerations of microleakage. J Endod. 1990;16:70–7. doi: 10.1016/S0099-2399(06)81567-0. [DOI] [PubMed] [Google Scholar]
- 79.Mitchell L. Decalcification during orthodontic treatment with fixed appliances – An overview. Br J Orthod. 1992;19:199–205. doi: 10.1179/bjo.19.3.199. [DOI] [PubMed] [Google Scholar]
- 80.Papaioannou W, Gizani S, Nassika M, Kontou E, Nakou M. Adhesion of Streptococcus mutans to different types of brackets. Angle Orthod. 2007;77:1090–5. doi: 10.2319/091706-375.1. [DOI] [PubMed] [Google Scholar]
- 81.Busscher H, Weerkamp A. Specific and nonspecific interactions in bacterial adhesion to solid substrata. FEMS Microbiol Rev. 1987;46:165–73. [Google Scholar]
- 82.Busscher H, Sjollema J, van der Mei H. Relative importance of surface free energy as a measure of hydrophobicity in bacterial adhesion to solid surfaces. In: Doyle RJ, Rosenberg M, editors. Microbial Cell Surface Hydrophobicity. Washington, DC: American Society for Microbiology; 1990. pp. 335–9. [Google Scholar]
- 83.Van Loosdrecht M, Zehnder A. Energetics of bacterial adhesion. Experientia. 1990;46:817–22. [Google Scholar]
- 84.van Loosdrecht MC, Lyklema J, Norde W, Zehnder AJ. Influence of interfaces on microbial activity. Microbiol Rev. 1990;54:75–87. doi: 10.1128/mr.54.1.75-87.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Scheie A. Mechanisms of dental plaque formation. Adv Dent Res. 1994;8:246–53. doi: 10.1177/08959374940080021801. [DOI] [PubMed] [Google Scholar]
- 86.Bos R, van der Mei HC, Busscher HJ. Physico-chemistry of initial microbial adhesive interactions – Its mechanisms and methods for study. FEMS Microbiol Rev. 1999;23:179–230. doi: 10.1111/j.1574-6976.1999.tb00396.x. [DOI] [PubMed] [Google Scholar]
- 87.Teughels W, Van Assche N, Sliepen I, Quirynen M. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006;17(Suppl 2):68–81. doi: 10.1111/j.1600-0501.2006.01353.x. [DOI] [PubMed] [Google Scholar]
- 88.Kawai K, Urano M, Ebisu S. Effect of surface roughness of porcelain on adhesion of bacteria and their synthesizing glucans. J Prosthet Dent. 2000;83:664–7. [PubMed] [Google Scholar]
- 89.Patterson CJ, McLundie AC, Stirrups DR, Taylor WG. Efficacy of a porcelain refinishing system in restoring surface finish after grinding with fine and extra-fine diamond burs. J Prosthet Dent. 1992;68:402–6. doi: 10.1016/0022-3913(92)90400-5. [DOI] [PubMed] [Google Scholar]
- 90.Hahn R, Weiger R, Netuschil L, Brüch M. Microbial accumulation and vitality on different restorative materials. Dent Mater. 1993;9:312–6. doi: 10.1016/0109-5641(93)90049-v. [DOI] [PubMed] [Google Scholar]
- 91.Auschill TM, Arweiler NB, Brecx M, Reich E, Sculean A, Netuschil L. The effect of dental restorative materials on dental biofilm. Eur J Oral Sci. 2002;110:48–53. doi: 10.1046/j.0909-8836.2001.101160.x. [DOI] [PubMed] [Google Scholar]
- 92.Scotti R, Kantorski KZ, Monaco C, Valandro LF, Ciocca L, Bottino MA. SEM evaluation of in situ early bacterial colonization on a Y-TZP ceramic: A pilot study. Int J Prosthodont. 2007;20:419–22. [PubMed] [Google Scholar]
- 93.Bremer F, Grade S, Kohorst P, Stiesch M. In vivo biofilm formation on different dental ceramics. Quintessence Int. 2011;42:565–74. [PubMed] [Google Scholar]


