Abstract
Background
I.v. 0.9% sodium chloride (normal saline) is frequently used to treat ED patients with acute alcohol intoxication despite the lack of evidence for its efficacy.
Objective
The study aims to compare treatment with i.v. normal saline and observation with observation alone in ED patients with acute alcohol intoxication.
Methods
A single-blind, randomised, controlled trial was conducted to compare a single bolus of 20 mL/kg i.v. normal saline plus observation with observation alone. One hundred and forty-four ED patients with uncomplicated acute alcohol intoxication were included. The study was conducted in one tertiary and one urban ED in Queensland, Australia. Primary outcome was ED length of stay (EDLOS). Secondary outcomes were treatment time, breath alcohol levels, intoxication symptom score, level of intoxication and associated healthcare costs.
Results
Both groups were comparable at baseline: blood alcohol content (BAC) was similar between treatment and control groups (0.20 % BAC vs 0.19 % BAC, P = 0.44) as were initial intoxication symptom scores (22.0 vs 22.3, P = 0.90). Both groups had a similar EDLOS (287 min vs 274 min, P = 0.89; difference 13 min [95% CI −37–63]) and treatment time (244 min vs 232 min, P = 0.94; difference 12 min [95% CI −31–55]). Change of breath alcohol levels, intoxication score and level of intoxication were not significantly different between the two groups. Patients in the treatment group had an additional healthcare cost of A$31.92 compared with control.
Conclusions
I.v. normal saline therapy added to observation alone does not decrease ED length of stay compared with observation alone. Intoxication symptom scores and general state of intoxication were similar in both groups. The present study suggests that either approach is reasonable, but observation alone might be preferred as it is less resource intensive.
Keywords: alcohol intoxication, intravenous administration, length of stay
Introduction
I.v. 0.9% sodium chloride solution (normal saline) is frequently used to treat ED patients with acute alcohol intoxication despite the lack of evidence for its efficacy.1,2 The theory behind this practice is that the administration of i.v. normal saline not only counteracts the dehydrating effects of alcohol, but might also have a dilutional effect on the level of alcohol and its metabolites, reducing its neuro-depressive effects,1 making the patient sober faster and therefore spend less time in the ED.
However, a small experimental study showed that there was no difference in rates of alcohol clearance in patients given a 1 L bolus of i.v. normal saline compared with those who did not receive this intervention.3 Furthermore, i.v. normal saline hydration as a treatment for alcohol intoxication in the ED is not discussed nor advocated in major emergency medicine references.4,5
Despite the lack of evidence, alcohol-intoxicated patients are still routinely treated with i.v. normal saline in many EDs around the world.6,7 Justification for its use should be explored to ascertain that the health and economic benefits outweigh the potential harms (such as infection and fluid overload8).
Our foremost aim is to provide evidence to an area where routine care is variable. The present study compares a single i.v. bolus of normal saline based on weight (20 mL/kg) and observation against observation alone in patients with acute uncomplicated alcohol intoxication requiring observation in an ED setting.
Methods
Study design
This was a two-centre, single-blinded, parallel-group study conducted in a health service district in Queensland, Australia. The trial was registered under Australian and New Zealand Clinical Trials Register number 12611000938909. No changes in trial design were made.
This study was approved by both the local institutional human research ethics committee and the Queensland Civil Administrative Tribunal for waiver of consent. A patient information sheet was given to each patient upon completion of the trial. Patients were allowed to retrospectively withdraw their consent.
Study setting and population
The first hospital has a tertiary ED, servicing a 570-bed major metropolitan teaching hospital. The second hospital has an urban ED, servicing a 270-bed general hospital. Attendance in 2011 was 67 000 and 50 000, respectively.
The study population comprised of adults aged 18 to 50 years of age, presenting with uncomplicated alcohol intoxication requiring observation. Potential patients were identified by the triage nurse and assessed by either an emergency registrar or consultant for eligibility (Box 1). Demographic information, alcohol intake and other concomitant recreational drugs used were taken from the patient, and relevant collateral history from the accompanying person or ambulance officer.
Box 1. Patient eligibility.
| Inclusion criteria | Adults aged 18–50 years of age Uncomplicated alcohol intoxication (no injuries, overdose, or psychiatric conditions requiring ongoing investigation or treatment) Unremarkable physical examination |
| Exclusion criteria | Age <18 years or >50 years Intellectual impairment (i.e. acquired brain injury, mental retardation) Known pregnancy Aggressive behaviour beyond reasonable attempts at de-escalation and deemed a potential threat to staff safety Patients later found to have significant injuries (i.e. head injury) or concomitant conditions (i.e. overdose) requiring further investigation or treatment Airway support more than a nasopharyngeal airway or oropharyngeal airway (i.e. endotracheal intubation) |
Study protocol
The treating doctor was the available emergency consultant, registrar or resident. The treating doctor was responsible for the enrolment and randomisation using sequentially-numbered opaque envelopes (SNOSE), ordering of i.v. fluids, haematological and biochemical tests, ongoing review, and decision for discharge. The treating nurse was either a registered nurse (RN) or an enrolled nurse trained to administer the Observational Assessment of Alcohol Intoxication (OAAI) tool,9 general intoxication scale, breath alcohol analyser machine and i.v. fluid.
Eligible patients were randomised to either a single i.v. bolus of 20 mL/kg normal saline infusion, in combination with observation (treatment group) or observation alone (observation group). No placebo was used. The treating doctor estimated the patient's weight if the patient was unable to do so. The calculated total dose of i.v. normal saline was given through a gravity-fed, vented i.v. drip chamber with air filter spike, tubing set, and at least 20 gauge or greater i.v. cannula through a large peripheral vein.
Observation consisted of a monitored bay with oxygen saturation, blood pressure and heart rate. Hourly Glasgow Coma Scale10 measurements and respiratory rate observations were performed according to hospital protocol. Clinical deterioration requiring resuscitation was defined as a persistent heart rate over 110/min, or a blood pressure less than 90/60 mmHg for at least 30 min.
Primary outcome measures
The primary end-point, emergency department length of stay (EDLOS), was defined from triage time to actual discharge time. Discharge from the ED occurred through one of the following ways, congruent with current local practice:
Treating doctor's judgment of the patient's fitness for discharge: Glasgow Coma Scale Score of 15, ambulatory with minimal support, no ongoing requirement for resuscitation, and no condition or injury requiring further investigation or treatment.
A responsible non-intoxicated adult available to take the patient home.
The patient absconded or left against medical advice.
Secondary outcome measures
Treatment time was defined as the time from being assessed by a treating doctor or nurse, until the time the patient was deemed ready for discharge by the treating doctor. This was chosen to reflect the possibility of other factors contributing to a patient's length of stay.
The International Classification of Diseases-10 Y91 codes11 were used to define the 10 signs of alcohol intoxication: smell of alcohol, conjunctival injection, impairments in speech, motor coordination, judgment, mood, behaviour, emotion, cooperation and horizontal gaze nystagmus. Each of the 10 signs of alcohol intoxication was evaluated by the treating nurse by using the 5-point rating scale (0–4) adapted from the OAAI tool used in the World Health Organization Collaborative Study on Alcohol and Injuries.9 Points from each sign of alcohol intoxication were then added together to form an intoxication score ranging from 0 to 40.
General state of intoxication of the patient was assessed by the treating RN using a 5-point scale ranging from very severe, severe, moderate, mild, to not intoxicated at all. Changes in general state of intoxication at 2 h were analysed into three groups: −3 and −2, −1 and 0 (no change), and 1 and 2. Groups were compared using χ2.
Serum ethanol level was measured using enzymatic rate Beckman-Coulter reagent synchron DXI 600 analyser-slope test (Brea, CA, USA). Breath alcohol level was measured using a Lion Alcolmeter 400® breath alcohol analyser (Vale of Glamorgan, UK) using mg/L breath alcohol content (BrAC) as the unit of measurement. The analyser was used according to the Lion Laboratories' manual of operation.
The health economic impact was defined as the cost of treating alcohol-intoxicated patients in the study. This included staff utilisation, tests and other physical resources.
Randomisation
The randomisation sequence was generated using http://www.randomizer.org. Stratification was conducted for site. We used block randomisation with blocks of 10. After being transferred to SNOSE, the randomisation sequence was then kept in a confidential, secure location. The randomisation sequence was concealed from the statistician, research assistant and health personnel assessing and enrolling patients. Each sealed envelope contained the allocated intervention. Statistician blinding was implemented by de-identification of data before analyses by the statistician.
Data collection
Recruitment for the trial was conducted between October 2011 and May 2012. Each participant underwent analyses of breath alcohol level, and an i.v. cannula was inserted, unless the patient was uncooperative or too combative for safe placement of an i.v. cannula. Routine full blood count, biochemical screen and serum ethanol levels were collected. Repeat breath alcohol levels were taken at 2 h and at discharge. Patients were also asked to voluntarily submit urine samples for screening of cannabinoids, amphetamines, opiates, cocaine and benzodiazepines. Patients were classified as taking other illicit drugs when they have either admitted to or they have tested positive on a urine drug screen.
End-point data for EDLOS and treatment time were collected on a data collection sheet. Resource utilisation for treating alcohol-intoxicated patients were taken from self-reported staff time and medical records (total number of normal saline bags, cannulas and tubing sets). Number and cost per type of laboratory blood test ordered were collected from the hospital pathology service.
All participants were offered a referral to the Drugs and Alcohol Brief Intervention Team for follow up at a later date. Participants who self-discharged were dealt with according to hospital policy and the Queensland Guardianship Act, independent of the study protocol.
Data analysis
To detect a reduction in EDLOS of 2 h with a 5% significance level and a power of 80%, a sample size of 72 per group was required. This sample size was based on local data, where the historical average length of stay of patients with a primary diagnosis of alcohol intoxication or as a secondary diagnosis between November 2008 and November 2009 was a little over 7 h (439 min). We hypothesised that the average length of stay would be reduced by 2 h to 319 min in patients who received i.v. saline.
Statistical analysis was conducted with spss v17 (SPSS, Chicago, IL, USA). A two-tailed, unequal variance Student's t-test was used to compare groups, except where measurements were not normally distributed a Mann–Whitney U-test was used instead. Pearson χ2-test was used to detect differences in proportions. Intention-to-treat analyses were used. No interim analysis was conducted. We assumed that all missing data were missing at random and censored them in the analysis. This trial was reported using the CONSORT statement (http://www.consort-statement.org).
The economic evaluation used was a cost-minimisation analysis from the perspective of direct costs to the hospital. All costs were current as at 1 June 2012, and are reported in 2012 Australian dollars (A$1 ≈ US$1 ≈ GBP £0.63). Assumptions for the calculation of the economic impact included the following:
Results
Characteristics of study subjects
During the study period, 626 patients presented with alcohol intoxication as their primary diagnosis (Fig. 1a), with 425 patients eligible by age criteria. Of these 425 patients, 164 patients were assessed for inclusion, with 144 eligible for enrolment (Fig. 1b).
Figure 1.
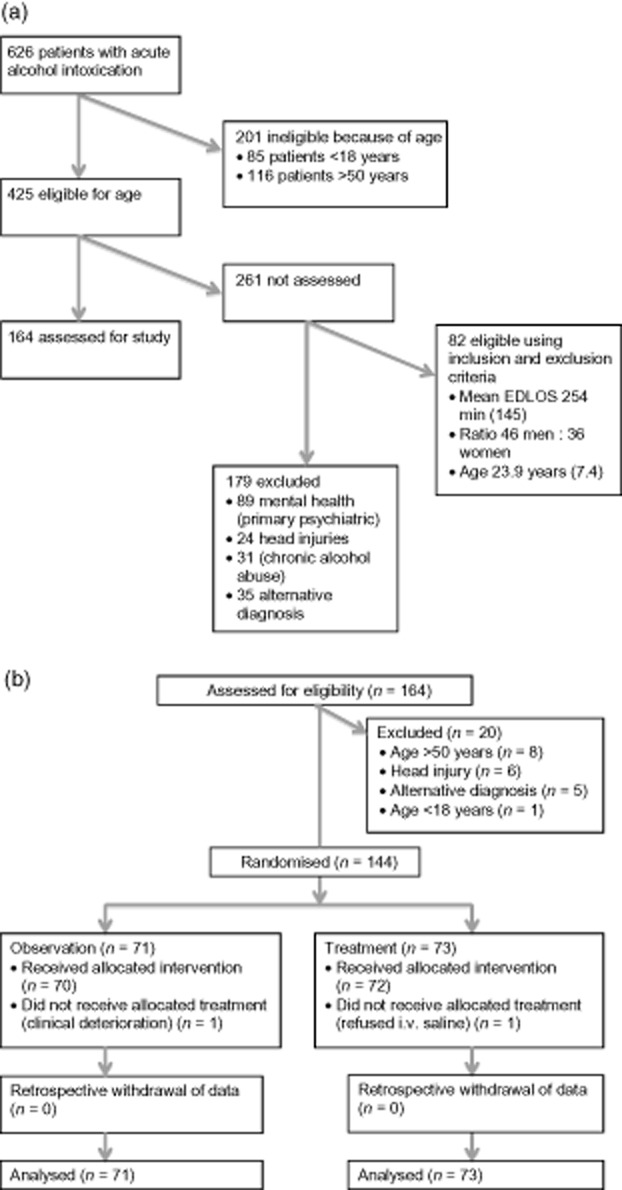
(a) Flow diagram (1 October 2011–15 May 2012). (b) Flow diagram. EDLOS, emergency department length of stay.
Of the 144 randomised patients, 73 were allocated to the treatment group and 71 to the observation group (Fig. 1b). No requests for withdrawal of data were received from any of the study participants after discharge from the ED. There was only one patient from each group that crossed over. There was one patient from the control group that required a 20 mL/kg i.v. saline infusion for persistent tachycardia greater than 110/min for at least 30 min after arrival in the ED. The tachycardia was attributed to dehydration from vomiting by the treating clinician. The patient's tachycardia settled down after the 20 mL/kg i.v. saline infusion.
Both treatment and observation groups were similar in terms of baseline characteristics such as sex, age, weight, height, standard drinks consumed, intake of other drugs, and blood alcohol content (Table 1).
Table 1.
Baseline demographics for all patients and subgroups with alcohol intoxication
| Demographics | Treatment – 20 mL/kg NaCl + observation | Control (observation alone) |
|---|---|---|
| All patients (n = 144) | ||
| No. (%) male | 39/73 (53) | 42/71 (59) |
| Age (years) | 24.9 (8.4) (n = 73) | 24.3 (7.4) (n = 71) |
| Weight (kg) | 70.2 (14.3) (n = 72) | 70.7 (13.8) (n = 64) |
| Height (cm) | 171.5 (8.6) (n = 62) | 171.0 (10.7) (n = 58) |
| Standard drinks consumed | 11.1 (6.6) (n = 44) | 10.8 (3.8) (n = 38) |
| Intake of other drugs (%) | 48/73 (66) | 46/71 (65) |
| Blood alcohol content (%) | 0.195 (0.07) (n = 59) | 0.185 (0.63) (n = 53) |
| Breath alcohol level (%) | 0.167 (0.07) (n = 56) | 0.172 (0.06) (n = 58) |
| Intoxication score at initial presentation (OAAI) | 22.1 (10.5) (n = 71) | 22.3 (9.6) (n = 68) |
Values are mean (SD) unless stated otherwise. EDLOS, emergency department length of stay; NaCl, sodium chloride solution; OAAI, Observational Assessment of Alcohol Intoxication.10
Main results
Patients treated with i.v. normal saline had an EDLOS of 287 min compared with those observed alone who had an EDLOS of 274 min. There was no significant difference found between the two groups (difference of 14 min, 95% CI −37 to 63 min, P = 0.89).
Secondary outcomes, including treatment time, was similar between treatment and control (244 min vs 232 min, P = 0.94), as were absolute change, percentage change, rate of change in OAAI scores at 2 h and rate of change in OAAI scores at discharge (Table 2).
Table 2.
Intention-to-treat analyses
| Treatment (20 mL/kg 0.9% NaCl) | Control (observation alone) | Treatment difference and 95% CI of the difference | P-value | |
|---|---|---|---|---|
| Primary end-point (mean [SD] minutes) | (n = 73) | (n = 71) | ||
| EDLOS | 287 (171) | 274 (131) | 14 (−37 to 63) | 0.89 |
| Secondary end-points | ||||
| Treatment time | 244 (143) | 232 (116) | 12 (−31 to 55) | 0.94 |
| Observational Assessment of Alcohol Intoxication (OAAI) | (n = 61) | (n = 54) | ||
| Absolute change of total OAAI score at 2 h | −10 (9) | −7 (8) | −3 (−6 to 1) | 0.16 |
| Per cent change of total OAAI score at 2 h | −40 (33) | −33 (44) | −7 (−21 to 7) | 0.34 |
| Rate of change of total OAAI score (points/h) at 2 h | −4.8 (4.8) | −3.6 (4.2) | −1.2 (−3.0 to 0.6) | 0.16 |
| Rate of change of total OAAI score (points/h) at discharge | −3.6 (3.0) | −4.2 (3.0) | 0.6 (−0.6 to 2.4) | 0.31 |
| Breath alcohol level (% alcohol) | (n = 43) | (n = 44) | ||
| Absolute change of BAL at 2 h | −0.036 (0.03) | −0.013 (0.1) | −0.023 (−0.06 to 0.01) | 0.16 |
| Per cent change of BAL at 2 h | −19 (14) | −8 (69) | −11 (−33 to 10) | 0.74 |
| Rate of change (%/h) of BAL at 2 h | −0.02 (0.01) | −0.01 (0.05) | −0.01 (−0.03 to 0.01) | 0.16 |
| Rate of change (%/h) of BAL at discharge | −0.01 (0.04) | −0.02 (0.02) | 0.01 (−0.01 to 0.03) | 0.82 |
Values are means (SD) unless stated otherwise. Where the measurements were not normally distributed, a Mann–Whitney U-test was used instead of an independent sample t-test. BAL, breath alcohol level; CI, confidence interval; EDLOS, emergency department length of stay; NaCl, sodium chloride solution; treatment difference: treatment minus control.10
There was no perceived change in general state of intoxication at 2 h between the two groups (P = 0.82) when comparing three levels of change in level of intoxication (−3 and −2, −1 and 0, and 1 and 2).
Absolute change, per cent change and rate of change in breath alcohol level at 2 h were similar for each group (−0.036 mg/L BrAC and −0.013 mg/L BrAC, P = 0.16, −19% and −8%, P = 0.74, 0.02 mg/L BrAC/h and −0.01 mg/L BrAC/h, P = 0.16, respectively, Table 2).
On average, patients in the observation group used A$124.52 in resources (laboratory tests, materials, nursing and medical staff attendance), compared with an average cost of A$156.44 in the treatment group (difference A$31.92, Table 3). Laboratory test costs amounted to A$51.14 per patient and detected two clinically significant results that were also detected by a bedside glucometer test (i.e. over A$3500 per abnormal test). No haematological or biochemical abnormalities requiring intervention or further investigation were found.
Table 3.
Estimated healthcare costs
| Test | Price (A$) | Observation only | I.v. fluids + Observation | ||
|---|---|---|---|---|---|
| Quantity, mean | Cost, mean (A$) | Quantity, mean | Cost, mean (A$) | ||
| Tests | |||||
| Blood alcohol content | 22.12 | 1 | 22.12 | 1 | 22.12 |
| Urea, electrolytes | 13.07 | 1 | 13.07 | 1 | 13.07 |
| Full blood count | 15.95 | 1 | 15.95 | 1 | 15.95 |
| Subtotal tests | 51.14 | 51.14 | |||
| Breath analyser | |||||
| Breath alcohol level | 0.04 | 3 | 0.12 | 3 | 0.12 |
| Mouth piece | 0.20 | 3 | 0.60 | 3 | 0.60 |
| Subtotal breath analyser | 0.72 | 0.72 | |||
| Material | |||||
| Saline 1 L bag | 2.80 | 0 | — | 1 | 2.80 |
| I.v. cannula | 1.99 | 1 | 1.99 | 1 | 1.99 |
| I.v. giving set | 4.70 | 0 | — | 1 | 4.70 |
| Needle-free valve | 2.00 | 1 | 2.00 | 1 | 2.00 |
| EDTA vial | 0.11 | 1 | 0.11 | 1 | 0.11 |
| Serum vial | 0.20 | 1 | 0.20 | 1 | 0.20 |
| Subtotal material | 4.30 | 11.80 | |||
| Staff | |||||
| Nursing (+ night differential) | 45.28 | 1.04 | 47.25 | 1.12 | 50.83 |
| Medical (+ night differential) | 48.72 | 0.43 | 21.11 | 0.86 | 41.95 |
| Subtotal staff | 68.36 | 92.78 | |||
| Grand total | 124.52 | 156.44 | |||
Discussion
We found that a single 20 mL/kg bolus infusion of i.v. 0.9% sodium chloride, together with observation, did not reduce ED length of stay of patients who had uncomplicated alcohol intoxication compared with those who were observed only. Similarly, treatment time was not significantly changed by administration of fluids. The present study suggests that administration of i.v. fluids has no effect on EDLOS, even when other factors such as delays in discharge are taken into consideration.
Treatment with a 20 mL/kg i.v. 0.9% sodium chloride infusion did not result in significant clinical improvement in intoxication scores compared with observation alone. Again, this is in discordance with the perception that i.v. fluids are thought to ‘sober up’ patients faster to enable earlier discharge.
Our study did not show a statistically significant difference on alcohol clearance at 2 h. However, absolute and per cent change in breath alcohol level (BAL) at 2 h showed a larger decrease in BAL in the treatment group compared with observation group. However, change in BAL was a secondary end-point, and the present study was not powered to detect a difference. Even with this trend of faster decrease in BAL in the treatment group, our emphasis was on conducting a real-world study with realistic discharge criteria that reflect current practice. BAL is one of the considerations, but the overall clinical level of intoxication and presence of an adult guardian often determine decision for discharge.
Comparing the costs of resources used, the treatment group used A$31.92 more. This difference is attributed to the cost of giving saline and the difference in staff time. Interestingly, if patients with alcohol intoxication were purely observed without laboratory blood tests or saline therapy, this could have saved an additional A$62.94 per patient. Assuming we observed all of our 3752 alcohol-related presentations in 2011 without any intervention (for the alcohol intoxication-related part of their presentation), our health district alone could potentially have saved over A$356 000 in 2011.
Limitations
The present study was randomised with comparable groups at baseline. However, the present study did not include a placebo in the observation group because of practical considerations. We chose to adhere to real-world practices where observation alone is a reasonable option for intoxicated patients. Along similar lines, it was impractical to blind staff or patients. A further limitation outside the control of this research was the patient load within the ED at the time of a patient's initial presentation. There were times when intoxicated patients were not included into the present study because of other patients requiring urgent attention. Eighty-two potentially eligible patients were not considered for inclusion (Fig. 1). This was mainly because of other clinical priorities. These missed eligible patients had similar demographics and EDLOS as the patients that were included, making selection bias unlikely. Data collected for self-reported staff time might have suffered from inaccuracies as a result of individual variances in self-perception of time. The logistics of measuring the exact time spent with each patient is challenging in a real-world setting. Despite these limitations, the present study is the first randomised study that provides real-world evidence on the use of i.v. 0.9% sodium chloride for alcohol-intoxicated patients.
Conclusions
There is no evidence that in alcohol-intoxicated patients a bolus of i.v. normal saline administration, together with observation, delivers better patient-oriented outcomes than observation alone. The use of cannulas, fluids and blood tests take time and resources that do not have an effect on clinically relevant outcomes. Although both treatment scenarios employed in the present study are safe and reasonable, we do not recommend routine prescription of i.v. fluids to patients presenting with uncomplicated acute alcohol intoxication to shorten their length of stay. Routine serum ethanol, full blood count and serum electrolytes are not indicated in these patients. BALs, with periodic monitoring of these patients, should suffice until sobriety or safe for discharge.
Acknowledgments
We are grateful to the doctors, nurses and administrative staff of both Southport and Robina ED. Appreciation is extended to Ms Chris Heenan for her invaluable work. We also thank Professor Paul Glasziou for his critical review of an early version of the manuscript. This project was funded by the Queensland Emergency Medicine Research Foundation. The sponsor did not have a role in study design, data collection, analysis or interpretation, or the manuscript writing.
Author contributions
SRSP contributed to the concept and design of the trial, implementation and management, analysis and interpretation of data, and writing of the manuscript. GK contributed to the design of the trial, data management, analysis and interpretation, and reviewing of the manuscript. MS advised on statistical analysis. JB and PAS contributed to the health economic analysis. GK is the guarantor.
Competing interests
GK is a Section Editor for Emergency Medicine Australasia.
References
- 1.Hindmarch PN, Land S, Wright J. Emergency physicians' opinions on the use of intravenous fluids to treat patients intoxicated with ethanol (alcohol): attitudes of emergency medicine physicians in the North East of England toward the use of intravenous fluids to treat individuals intoxicated with ethanol (alcohol) attending the emergency department compared with the scientific evidence. Eur. J. Emerg. Med. 2012;19:379–383. doi: 10.1097/MEJ.0b013e32834e909c. [DOI] [PubMed] [Google Scholar]
- 2.Sanaei-Zadeh H. Use of intravenous fluids for the treatment of patients intoxicated with ethanol (alcohol): is it a scientific-based practice? Eur. J. Emerg. Med. 2012;19:409–410. doi: 10.1097/MEJ.0b013e3283521265. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Mills T, Erato R. Intravenous saline has no effect on blood ethanol clearance. J. Emerg. Med. 1999;17:1–5. doi: 10.1016/s0736-4679(98)00120-6. [DOI] [PubMed] [Google Scholar]
- 4.Finnell J, Marx JA, Hockerberg RS. Alcohol-related disease [Internet] In: Rosen P, et al., editors. Rosen's Emergency Medicine: Concepts and Clinical Practice. Pennsylvania: Mosby Elsevier; 2010. pp. 2378–2394. [Cited 15 Jul.] Available from URL: http://www.mdconsult.com. [Google Scholar]
- 5.Moulds R, Brett J, Buckley N, et al. Alcohol overdose [Internet] Therapeutic Guidelines. 2008. [Cited 15 Jul 2010.] Available from URL: https://online-tg-org-au.cknservices.dotsec.com/ip/
- 6.Sellaturay S, Arya M, Makepeace J, Sellaturay P, Henry JA. Management of alcohol intoxication and aggressive behaviour: a tale of two cities. Curr. Med. Res. Opin. 2007;23:77–83. doi: 10.1185/030079906X159470. [DOI] [PubMed] [Google Scholar]
- 7.Yost DA. Acute care for alcohol intoxication. Be prepared to consider clinical dilemmas. Postgrad. Med. 2002;112:14–16. doi: 10.3810/pgm.2002.12.1361. , 21–2, 25–6. [DOI] [PubMed] [Google Scholar]
- 8.Holte K, Jensen P, Kehlet H. Physiologic effects of intravenous fluid administration in healthy volunteers. Anesth. Analg. 2003;96:1504–1509. doi: 10.1213/01.ANE.0000055820.56129.EE. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Collaborative study on alcohol and injuries: final report. 2007. WHO. [Cited 5 Apr 2010] Available from URL: http://www.who.int/substance_abuse/publications/alcohol/en/index.html.
- 10.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;304:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines [Internet] 1992. WHO. [Cited 8 Feb 2010] Available from URL: http://www.who.int/substance_abuse/terminology/icd_10/en/index.html.
- 12.Queensland Health. Nursing and midwifery wage rates – Queensland Health [Internet] 2012. [April ]. [Cited 5 Jun 2012.] Available from URL: http://www.health.qld.gov.au/hrpolicies/wage_rates/nursing.asp.
- 13.Queensland Health. Medical officers' base pay rates – queensland health [Internet] 2010. [Cited 5 Jun 2012.] Available from URL: http://www.health.qld.gov.au/medical/docs/payrates_2010.pdf.


