Abstract
The idea of a progression in suicide phenomena, from death wishes to suicide attempts and completed suicides, is quite old and widely present in literature. This model of interpreting suicidality has great relevance in preventative approaches, since it gives the opportunity of intercepting suicidal trajectories at several different stages. However, this may not be the case for many situations, and the hypothesis of a continuum can be true only in a limited number of cases, probably embedded with a specific psychopathological scenario (e.g. depression) and with a frequency that should not permit generalisations. This paper reviews the available evidence about the existence and validity of this construct, and discusses its practical implications.
Key words: suicidal behaviour, suicide, process, continuum, prevention strategy.
Introduction
Considerations of suicidality as a phenomenon developing along a continuum arose several decades ago as an opposition to - at the time conventional - static medical models, which focused mainly on completed suicides with little or no attention to the events and processes that lead to these deaths.1 Among others, Mikawa and Paykel et al. called for a new, process-oriented definition of suicidal behaviour that reflected the dynamic interactions of environmental and personal factors.2,3 Since then, it has become a widely accepted model of suicidality, reflected in a wealth of research studies based on these conceptualisations.4 Within the new definition, suicide became conceptualised as a process or a continuum of ideations/behaviours developing from mild to more severe forms of suicidality, most often including the following stages: suicidal ideation, suicide plan, suicide attempt, and completed suicide.
In recent years, additional distinctions between specific sub-stages have developed. For example, suicidal ideation refers to cognitions that can vary from transient thoughts about the worthlessness of life and death wishes to concrete plans for killing oneself and obsessive preoccupation with self-destruction.5 Thus, Silverman and colleagues suggested the following division of suicide ideation based on the severity of the subject's intent to die: the casual, transient, passive, active, and/or persistent thoughts of suicide.6 Additionally, several authors differentiate between planned and unplanned - or impulsive - suicide attempts.7–9
Internationally, there is a growing body of work investigating the prevalence of suicidal ideations and/or attempts in large population cohorts,10,11 providing reliable accounts of the dimensions of these phenomena. However, the nature of transitions between these stages remains poorly understood, as only a limited number of studies to date have investigated temporal links between suicidal features of different severity. In particular, there is scarcity of epidemiological studies with longitudinal designs that would allow for follow-up of developments of suicidality in subjects expressing suicide-related thoughts at the first assessment.
This paper is organised in four sub-sections. Firstly, we will describe different models of risk factors that contribute to individual's vulnerability for development of suicide-related outcomes. Secondly, we will present findings of a few prominent studies which assessed the prevalence of persons in the general population experiencing specific stages on the continuum of suicidality. Thirdly, we will summarise available empirical knowledge on the determinants of transition along the suicidal continuum (escalation from suicidal thoughts to attempted or completed suicide). Lastly, we discuss the clinical implications of these concepts from the standpoint of suicide prevention.
Pathways to suicide: the bio-psycho-social model
Suicide is not simply a reaction to a time-limited crisis, but involves the individual's entire life experience, including his sociocultural milieu (Maris RW, 1981).12
The quote above is taken from a landmark work by Ronald W. Maris, entitled Pathways to Suicide: a Survey of Self-Destructive Behaviours (1981).12 While three decades have passed since the release of his theory, it remains one of the most comprehensive biopsycho-social models explaining risk factors for suicide. The central idea of Maris' work is the concept of a suicidal career, stating that suicide can never be completely explained by acute, situational factors; instead, it develops over time and against certain social, psychological and genetic conditions. The model was developed based on the results of a large case-control study of 266 cases of completed suicide, investigating the role of a wide range of predictors of suicidal outcomes covering the entire life span (separated into individuals' background, early life, mid-life and late-life).
A general model of suicidal behaviour, later developed by Maris et al.,13 recognises any suicidal outcome as a complex and interactive effect of many inter-related factors. The four main domains involved in the development of suicidality include: psychiatric, biological, psychological and social circumstances. Over the course of development of one's suicidality, a variety of predisposing factors influences its escalation, such as age, sex, race, history of psychiatric illness in parents, and broader social environments (either stimulating or destructive).
Particular risk factors, that determine the transition from trait suicidality towards heightened risks for completed suicide, include: mental disorders (in particular affective, anxiety/panic and personality disorders), alcohol and drug abuse, inadequate social support, impulsivity and cognitive rigidity, and work-related problems. However, harmful effects of these factors can be countered by protective influences of physical and mental health, social integration and good coping skills. As a next stage in the proposed model, a vulnerable individual enters into an acute suicidal crisis or a suicide zone, which represents a convergence of multiple risk and protective factors that temporarily, yet significantly, increase the risk for suicide-related outcome. Authors maintain that the precipitating events, which seemingly trigger or aggravate completed suicidal acts, are rarely a single negative life event or stressor. Rather, they represent a gradual accumulation of many interactive risk factors, increasing one's vulnerability over a long time. An additional concept introduced by this model is the feedback loop, suggesting that those in the suicide zone who do not complete suicide, often either cycle back to a stage of increased vulnerability for eventual suicide at a later stage, or alternatively develop greater resilience through protective factors and thus interrupt the progression of their suicidal career.
Distal versus proximal suicide risk factors
The stress-diathesis model of suicide risk conceptualises risk factors as either distal or proximal.14 Distal risk factors are background characteristics or underlying vulnerabilities that heighten a person's risk for suicide anytime in life and include developmental, personality, biological, and genetic variables, along with impulsive-aggressive personality traits. Distal risk factors affect the threshold for suicide and increase an individual's risk when faced with proximal risk factors, which are more immediate antecedent to the suicidal event itself, and may include life events, stress, acute intoxication, etc.15 The specificity of risk factors may be less important than their cumulative burden on a vulnerable individual. The complex contributions and interactions among risk and protective suicide factors reflect fluid processes that change with time and individual experience (as is evident in the previously described model by Maris et al.).13 Risk and protective factors can be further distinguished in internal and external, based on whether they originate from an individual or the environment.15
Prevalence of suicide ideation, plans and attempts
Acquiring an accurate picture of the prevalence of these phenomena is difficult, since information on suicide ideations and plans cannot be collected in any routine fashion. For observation of transitions in specific stages of suicidal behavior, frequent serial data would need to be obtained but that would represent technically an extremely challenging enterprise, even in clinical populations. Data on suicide attempts can be obtained through records of hospitalizations and presentations to emergency departments; however, it is a well-known fact that the majority of people who engage in non-fatal self-harming acts do not seek medical attention in its aftermath.16 In Australia, for example, data on hospitalizations for suicide attempts exist but they are event based, not person-based, which further hinders the elaboration of population-based rates.17 Therefore, the optimal way of gauging the exact dimensions of prevalence of suicidal thoughts, plans and attempts is through large epidemiological community surveys. International literature offers a reasonable number of such studies, and we here present findings from a few of them.
In 2005, Bertolote and colleagues published data from the largest international study on suicidal behaviour conducted to date: the WHO Multisite Intervention Study on Suicidal Behaviour (SUPRE-MISS).10 In this study, community surveys were distributed to about 70,000 respondents in 10 countries, enquiring - among others - about the lifetime prevalence of suicide ideation, plans and attempts. Results varied significantly across sites: prevalence of suicide ideation ranged between 2.6 and 25.4%, plans between 1.1 and 15.6%, and suicide attempts between 0.4 and 4.2%. Another international survey, conducted in 17 developed and developing countries, yielded lifetime prevalence for suicide ideation of 9.2%, 3.1% for suicide plans and 2.7% for suicide attempts.11 One of the largest community surveys ever performed in a single country was carried out by De Leo et al. in 2005:18 results of this study are presented in Table 1, along with results of two Australian National Surveys of Mental Health and Wellbeing (NSMHWB).17,19
Table 1. Lifetime prevalence of suicide ideation, plan and attempts in Australian general population.
| De Leo et al. 200518 | Pirkis et al. 200019 | Johnston et al. 200917 | |
|---|---|---|---|
| Survey | SUPRE-MISS | NSMHWB | NSMHWB |
| Sample | 11,572 | 10,641 | 8841 |
| Life weariness (%)* | 21.1 | N/A | N/A |
| Suicide ideation (%)° | 10.4 | 16.0 | 13.3 |
| Suicide plan (%) | 4.4 | N/A | 4.0 |
| Suicide attempt (%) | 4.2 | 3.6 | 3.2 |
SUPRE-MISS, World Health Organization Multisite Intervention Study on Suicidal Behaviour; NSMHWB, Australian National Surveys of Mental Health and Wellbeing; N/A, not assessed.
Have you ever thought life s not worth living?
Have you ever seriously thought about committing suicide?
The 2009 NSMHWB also assessed 12-month prevalence for ideation, plans, and attempts. These occurred among 2.3%, 0.6% and 0.4% of the population, respectively. Compared to results of the NSMHWB survey conducted in 2000, the 12-month prevalence of suicide ideation seems to have declined by 1.1%, while rate of attempts stayed unchanged.17,19
Escalation of suicidality along a continuum
Existing literature provides evidence for the fact that suicidality develops along a continuum ranging from less severe forms (thoughts of death or suicide ideation) to most severe expressions of the intent to die (serious suicide attempts or completed suicides).3,20,21 However, the particularities of transitions through these stages remain insufficiently understood due to the scarcity of methodologically sound (in particular prospective) studies examining the development of different suicide-related phenomena. The following section will summarise the available empirical knowledge on this subject.
One key-study on the development of suicidality over time was performed by Kessler et al.22 This epidemiological cross-sectional study was the first to measure the likelihood of transitioning between different stages of suicidality; authors reported that 34% suicide ideators progress to developing a suicide plan, 72% progress from having a suicide plan to an attempt, and 26% from ideation to an unplanned attempt. Risk for these progressions is highest in the first year following onset of the prior condition. This observation was replicated in a study conducted in metropolitan China,23 which also reported comparable conditional probabilities among ideators to develop a suicide plan (29%) or make a suicide attempt (32%) - the latter risk was higher for ideators with a plan than those engaging in impulsive attempts. However, Australian data suggest that only 12% of ideators progress to making a suicide attempt.19 A review of studies that have reported the ratios of ideation to attempt has shown these to vary between 4:1 and 13:1.24 The proportion of ideators who complete suicide is even smaller, estimated to be somewhere between 1:100 and 1:2000.24,25 In a survival analysis of suicide risk in a cohort of 1573 suicide attempters, followed for 5 years by Nordstrom and colleagues,26 the suicide mortality was 6% - almost twice as prevalent among the males as in females - with the highest risk observed during the first year.
It is apparent that suicidal ideation is considerably greater, in terms of incidence and prevalence, than suicide attempts. Furthermore, thoughts of suicide are often somewhat transient,27 in particular during adolescence.28 This has led some authors to question the relevance of these thoughts in predicting the risks for development of more progressed expressions of suicidality.29 However, there is some support for the fact that suicidal thinking in adolescence, even of an ostensibly low severity, predicts suicidal ideation and attempts in adulthood.30 Similar results were obtained from clinical cohorts, demonstrating that even mild suicidal ideation can lead to progressively more frequent and lethal risk behaviours.31 While only a fraction of suicide ideators proceed to attempted or completed suicide, it is generally believed that majority of attempters and completers experience suicidal ideation and develop a suicide plan before engaging in self-harming acts. Indeed, in the already quoted community survey conducted in Australia,18 only 0.8% of participating suicide attempters reported the absence of previous suicidal ideation. Among older adolescents with a history of suicide attempts, proportion of respondents who also evidenced suicidal ideation was somewhat lower, yet still close to 90%.32 In contrast, international literature provides several accounts of attempted and completed suicides, particularly in young people, which do not involve a progression in stages of suicidality. For example, Hoberman and Garfinkel found that in a sample of 229 cases of completed suicides among adolescents,33 only 28% evidenced a plan to commit suicide, while definite preparation for death was apparent in only 8% of suicides. Similar results were provided by Hall and colleagues,34 who interviewed 100 patients hospitalised after a serious suicide attempt. Authors found that only 29 of these patients reported having persistent and serious suicidal thoughts prior to their attempt, while 69 had only fleeting thoughts of suicide or no suicidal thoughts at all. Only 14 patients reported a specific suicide plan. In Estonia, 28% of suicide attempters did not indicate to have ever had thoughts about committing suicide or to ever have made a plan.10
Findings presented above demonstrate that while suicidal thoughts may be frequent, they are by no means definite motivators for attempted and completed suicides. So what factors distinguish between ideators who act on their suicidal thoughts from those who do not? As has been noted by Brezo et al.,35 to increase the specificity and predictive value in identifying individuals at risk for more serious suicidal behaviours, it is important to consider the properties of suicidal thoughts themselves but also the presence of other contributing factors. Marusic and Farmer proposed that all stages of suicidal behaviours, as well as transitions between these stages,36 are influenced by genetic and environmental influences and their reciprocal interactions. An example of the interactions between genes and environment on the development of passive suicide ideation is the observation that individuals genetically predisposed to depression may themselves seek high-risk environments where an occurrence of threatening events is more likely. Alternatively, depression-prone persons may view the environment as more hostile and threatening than the average person. In addition, authors introduce traits of impulsivity and aggression, both also influenced by genetic proneness and (unfavourable) environmental circumstances, as key factors determining the fatality of an attempted suicide.36
Approximately two-thirds (66%) of people who have seriously considered killing themselves report having a prior psychiatric disorder; this percentage is even higher among persons who go on to make a suicide plan (77%) or suicide attempt (80%).9 History of mental disorders is higher among respondents who make a planned attempt (83%) compared to an unplanned attempt (74%), suggesting that the latter may be influenced to a greater extent by other factors, such as stressful life events.9 Despite these recent findings, surprisingly little is known about what aspect of suicidal behaviour mental disorders actually predict. Some epidemiological studies suggest that mental disorders predict the onset of suicide ideation, but may have weaker effects in predicting suicide plans or attempts among people with suicide ideation.37 It has also been reported that depression predicts suicide ideation, but not suicide plans or attempts among those with ideation. Instead, disorders characterized by severe anxiety/agitation (e.g. post-traumatic stress disorder) and poor impulse-control (e.g. conduct disorder, substance disorders) offer more accurate predictions into which suicide ideators go on to make a plan or attempt.9 An additional factor marking the progress from suicide ideators to suicide attempters has been found to be unemployment,19 while the investigation of traumatising events on escalation of suicidality has yet not yielded any conclusive evidence.38
The above mentioned large community survey, conducted in Australia,18 aimed to explore whether suicidal behaviour develops along a continuum of progressively ascending severity or it fluctuates in its intensity. Respondents with a lifetime history of suicide plan or attempt were presented with a visual image (Figure 1), which depicted two possible scenarios detailing the development of suicidal thoughts and behaviours over time: a continuum hypothesis (presented as orange line) and a fluctuating hypothesis (presented as blue line). Subjects were asked to select which of the two patterns of suicidality depicted in the figure best approximated their own experience. Results showed that only 20.0% of suicide planners and attempters reported their suicidal process to be developing continuously in severity over an extended period of time. In contrast, 57.1% of participants declared that their suicidal process was not continuous, but rather fluctuated irregularly before they attempted suicide or were close to attempting suicide. No significant predictors of the respondents' declarations were found. A further aim of the same study was to assess if individuals experience all levels of suicidal ideation and behaviour leading up to their highest reported level. Data showed that only 53% of participants presented all levels of suicidal ideation preceding the one with the highest severity. Individuals who had a diagnosis of depression prior to their suicidal behaviour, and reported that their act was not an impulsive one, were five times more likely to have experienced all the hypothetical stages of the suicidal process that their counterparts. A study performed in Iran by Ghazinour et al.39 also asked participating suicide attempters if prior to their attempt they had experienced the following suicide-related thoughts with a steadily increasing severity: life weariness, death thoughts, death wishes, and suicide ideation. Only 20% of individuals reported they had experienced all these thoughts, which adds further support to the notion that the course of suicidal ideation and suicidal attempts is rarely continuous.
Figure 1.
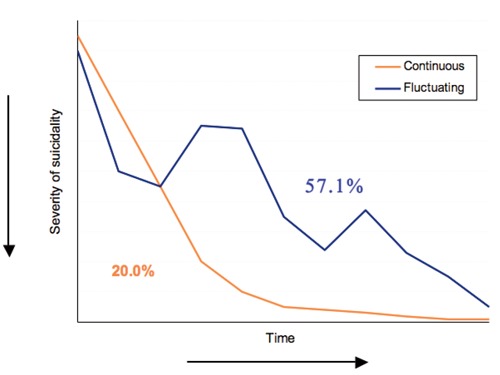
Progression of severity of suicidality over time.
There is no doubt that past suicidal behaviour is related to future suicidal behaviour.40,41 In fact, non-fatal suicidal behaviour is the strongest known clinical predictor of eventual suicide.42 However, the question remains whether this relationship is non-spurious and possibly even causal, or is it accounted for by a set of third variables, such as enduring predispositions or various clinical conditions.20 Findings from studies comparing characteristics of persons who attempt or complete suicides are suggesting that these relationships may not be adequately explained by overlapping risk factors for the two acts.43,44 On the other hand, several authors are arguing the existence of causal links between suicidal features of different severity. This view has been supported by Post et al.,45 who first noticed that in depressed patients, the first episode of depression is more strongly connected to precipitating adverse life circumstances than later recurring episodes. Similarly, Beck theorised that previous suicidal experience sensitises suicide-related thoughts and behaviours and leads to the development of a suicidal mode.46 The more active these schemas and modes become (through the repetition of suicidal thoughts of actions), the more easily they are triggered (even in the absence of negative events), and the more severe are the subsequent suicidal episodes. Recently, neurological studies have provided further evidence for this concept by demonstrating that suicidal behaviour is a state-based condition stored in neural circuitry that can be quickly switched on by the recall of an experience of mental pain.47 Joiner concurs that initial suicidal behaviour sets processes into motion that spur later suicidal behaviours.48 He proposed two psychological processes explaining the link between past and future suicidal behaviour: cognitive sensitization and opponent processes. While the former aligns with Becks' cognitive theory (described above), the latter means that with repetition of suicidal behaviour, the painful and fear-inducing qualities of suicidality diminish, and opponent processes (e.g. calming and pain-relieving effects) may intensify. Indeed, obvious precipitating recent life events have been reported more frequently by first-ever than repeat self-harmers.49 However, this hypothesis has yet not been directly examined and prospective evidence is lacking.
A handful of studies to date have explored factors that help ameliorate suicidal thoughts over time. A study investigating persistence of suicidal ideation in a sample of Finnish subjects from the general population reported that 31% males and 41% females having suicidal thoughts at baseline assessment had stopped experiencing them 12 months later.50 A similar survey, performed in Great Britain, found that among 2.3% of adults that reported experiencing suicidal thoughts in the last year, 57% had recovered by the 18-month follow-up interview.25 Recovery was more likely in women and in those aged below 25 years or over 65 years. Further, improvement was strongly associated with absence of psychiatric illness, and favourable social and economic circumstances. A somewhat surprising discovery by these authors was that persons receiving antidepressants or counselling or who were in contact with health care professionals in the period between baseline and follow-up assessments, were in fact less likely to recover from suicidal thoughts.25,50
Results of these studies suggest that the course of suicidality is not necessarily chronic, as only a minority of suicidal thought develop over time with progressively increasing severity. An interesting observation has been derived from a study conducted in Iranian Kurds,39 where a much wider gap was noticed between occurrence of suicidal thoughts of any kind and frequency of suicide attempts, compared to other countries. Authors proposed that at the higher stages of the suicidal behaviour continuum, religious, cultural and societal norms might disrupt the transition along the continuum, acting as a barrier to acting on suicidal impulses. Observations that the evolution from thoughts to plans and attempts is influenced by the specific cultural settings has been confirmed in a large international study by the World Health Organization,10 suggesting the need for development of different, site-specific approaches to suicide prevention.
Implications for suicide prevention
An understanding of the transitions between less severe manifestations of suicidality (i.e. suicide ideation) to fatal or non-fatal suicidal acts has huge practical implications for timely identification of persons at risk and development of targeted suicide prevention strategies. This is especially important for clinical purposes, as clinicians are often faced with the task of determining the likelihood that a patient with suicide ideation will subsequently engage in a fatal or non-fatal suicidal act, so they can intervene at early stages of these dangerous trajectories.
However, empirical knowledge on this topic remains so poor that it is practically impossible to predict the development of more severe stages of suicidality based on individual's reports of suicide ideation,51 even in combination with a plethora of other well-recognised risk factors for suicide. The idea of a continuum seems to apply only to certain cases (possibly long-lasting/chronic depression sufferers), which may not represent the majority of suicidal subjects. If this were true (but further research should confirm it), this would have important implication for both detection and prevention of suicide. For example, excessive reliance on screening programs for suicidality might bring to remarkable underestimation of risk, so that what is not captured today could be present tomorrow. From this point of view, detection of depressive symptomatology would seem to be more reliable in predicting future risks, even if straight comparisons by the two screening targets have never been directly presented in the literature. In addition, the absence of present suicidality or the denial of it can easily become the justification for reduced vigilance, even in persons of demonstrated suicidal potential and/or history of past suicidal behaviour. One such segment of population that warrants maximum prudence are psychiatric patients upon discharge from the hospital when they might be disguising their determination to suicide in order to avoid preventative efforts. This, and several other reasons previously noted in existing literature, contributes to very high rates of suicide among post-discharge patients.52,53 Monitoring of suicidal ideation/behaviour should therefore not rely heavily on such denials, yet still too often recording the absence of a suicide plan at discharge satisfies clinicians. While such actions put them on a safe shore from a medico-legal perspective, they certainly do not help saving lives.
Nevertheless, despite our inability to predict who will die by suicide, there are a number of clinical features that are, at the very least, statistically associated with subsequent suicide. Past suicidal thoughts and/or acts are undoubtedly the strongest of such features, and any person presenting with thoughts of suicide, especially if they are persistent and involve a strong intent to die, warrants immediate and constant professional attention.
References
- 1.Lester D. Suicide prevention: resources for the millennium. Philadelphia: Taylor and Francis; 2001. [Google Scholar]
- 2.Mikawa JK. An alternative to current analyses of suicidal behavior. Psychol Rep. 1973;32:323–30. doi: 10.2466/pr0.1973.32.1.323. [DOI] [PubMed] [Google Scholar]
- 3.Paykel ES, Myers JK, Lindenthal JJ, Tanner J. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124:460–9. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 4.De Leo D, Bertolote JM, Lester D. Self directed violence. In: Krug EG, Dahlberg LL, Mercy JJ, et al., editors. World report on violence and health. Geneva: World Health Organization; 2002. pp. 185–212. [Google Scholar]
- 5.Diekstra RFW, Garnefski N. On the nature, magnitude, and causality of suicidal behaviors: an international perspective. Suicide Life Threat Behav. 1995;25:36–57. [PubMed] [Google Scholar]
- 6.Silverman MM, Berman AL, Sanddal ND. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 2: suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav. 2007;37:264–77. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]
- 7.Conner KR. A call for research on planned vs. unplanned suicidal behavior. Suicide Life Threat Behav. 2004;34:89–98. doi: 10.1521/suli.34.2.89.32780. [DOI] [PubMed] [Google Scholar]
- 8.Jeon HJ, Lee J-Y, Lee YM, et al. Unplanned versus planned suicide attempters, precipitants, methods, and an association with mental disorders in a Korea-based community sample. J Affect Disord. 2010;127:274–80. doi: 10.1016/j.jad.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 9.Nock MK, Hwang I, Sampson NA, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO world mental health surveys. PLoS Medicine. 2009;6:e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bertolote JM, Fleischmann A, De Leo D, et al. Suicide attempts, plans, and ideation in culturally diverse sites: the WHO SUPRE-MISS community survey. Psychol Med. 2005;35:1457–65. doi: 10.1017/S0033291705005404. [DOI] [PubMed] [Google Scholar]
- 11.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maris RW. Pathways to suicide: a survey of self-destructive behaviours. Baltimore: Johns Hopkins University Press; 1981. [Google Scholar]
- 13.Maris RW, Berman AL, Maltsberger JT. Maris RW, Maris AL, Maltsberger JT, Yufit RI. Assessment and prediction of suicide. New York: Guilford Press; 1992. Summary and conclusions: what have we learned about suicide assessment and prediction? pp. 640–668. [Google Scholar]
- 14.Mann JJ, Waternaux C, Haas G, Malone K. Toward a clinical model of suicidal behaviour in psychiatric patients. Am J Psychiatry. 1999;156:181–9. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 15.Moscicki E. Identification of suicide factors using epidemiologic studies. Psychiatr Clin North Am. 1997;20:499–517. doi: 10.1016/s0193-953x(05)70327-0. [DOI] [PubMed] [Google Scholar]
- 16.Preti A, Tondo L, Sisti D, et al. Correlates and antecedents of hospital admission for attempted suicide: a nationwide survey in Italy. Eur Arch Psychiatry Clin Neurosci. 2010;260:181–90. doi: 10.1007/s00406-009-0037-x. [DOI] [PubMed] [Google Scholar]
- 17.Johnstnon AK, Pirkis JE, Burgess PM. Suicidal thoughts and behaviours among Australian adults: findings from the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry. 2009;43:635–643. doi: 10.1080/00048670902970874. [DOI] [PubMed] [Google Scholar]
- 18.De Leo D, Cerin E, Spathonis K, Burgis SH. Lifetime risk of suicide ideation and attempts in an Auatrialian community: prevalence, suicidal process, and help-seeking behaviour. J of Affect Disord. 2005;86:215–24. doi: 10.1016/j.jad.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Pirkis J, Burgess P, Dunt D. Suicidal ideation and suicide attempts among Australian adults. Crisis. 2010;21:16–25. doi: 10.1027//0227-5910.21.1.16. [DOI] [PubMed] [Google Scholar]
- 20.Joiner TE, Conwell Y, Fitzpatrick KK, et al. Four studies on how past and current suicidality relate even when everything but the kitchen sink is covaried. J Abnorm Psychol. 2005;114:291–303. doi: 10.1037/0021-843X.114.2.291. [DOI] [PubMed] [Google Scholar]
- 21.Scocco P, De Leo D. One-year prevalence of death thoughts, suicide ideation and behaviours in an elderly population. Int J Geriatr Psychiatry. 2002;17:842–6. doi: 10.1002/gps.691. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National comorbidity survey. Arch Gen Psychiatry. 1999;56:617–26. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 23.Lee S, Tsang A, Zhang MY, et al. Lifetime prevalence and inter-cohort variation in DSM-IV disorders in metropolitan China. Psychol Med. 2007;37:61–73. doi: 10.1017/S0033291706008993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McAuliffe CM. Suicidal Ideation as an articulation of intent: a focus for suicide prevention? Arch Suicide Res. 2002;6:323–38. [Google Scholar]
- 25.Gunnell D, Harbord R, Singleton N, et al. Factors influencing the development and amelioration of suicidal thoughts in the general population-cohort study. Br J Psychiatry. 2004;185:385–93. doi: 10.1192/bjp.185.5.385. [DOI] [PubMed] [Google Scholar]
- 26.Nordström P, Samuelsson M, Asberg M. Survival analysis of suicide risk after attempted suicide. Acta Psychiatr Scand. 1995;91:336–40. doi: 10.1111/j.1600-0447.1995.tb09791.x. [DOI] [PubMed] [Google Scholar]
- 27.Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. J Consult Clin Psychol. 2007;75:707–15. doi: 10.1037/0022-006X.75.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kovacs M, Goldston D, Gatsonis C. Suicidal behaviors and child-onset depressive disorders: A longitudinal investigation. J Am Acad Child Adolesc Psychiatry. 1993;32:8–20. doi: 10.1097/00004583-199301000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Schwenk TL. Is detecting suicidal ideation good. [Accessed on: October 25, 2010]; Available from: www.annfammed.org/cgi/eletters/3/6/529%3696.
- 30.Reinherz HZ, Tanner JL, Berger SR, et al. Adolescent suicidal ideation as predictive of psychopathology, suicidal behavior, and compromised functioning at age 30. Am J Psychiatry. 2006;163:1226–332. doi: 10.1176/ajp.2006.163.7.1226. [DOI] [PubMed] [Google Scholar]
- 31.Pfeffer CR, Klerman GL, Hurt SW, et al. Suicidal children grow up: rates and psychosocial risk factors for suicide attempts during follow-up. J Am Acad Child Adolesc Psychiatry. 1993;32:106–13. doi: 10.1097/00004583-199301000-00016. [DOI] [PubMed] [Google Scholar]
- 32.Andrews JA, Lewinsohn PM. Suicidal attempts among older adolescents: prevalence and co-occurrence with psychiatric disorders. J Am Acad Child Adolesc Psychiatry. 1992;31:655–62. doi: 10.1097/00004583-199207000-00012. [DOI] [PubMed] [Google Scholar]
- 33.Hoberman HH, Garfinkel BD. Completed suicide in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1988;27:689–95. doi: 10.1097/00004583-198811000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Hall RC, Platt DE, Hall RC. Suicide risk assessment: a review of risk factors for suicide in 100 patients who made severe suicide attempts. Psychosomatics. 1999;40:18– 27. doi: 10.1016/S0033-3182(99)71267-3. [DOI] [PubMed] [Google Scholar]
- 35.Brezo J, Paris J, Tremblay R, et al. Identifying correlates of suicide attempts in suicidal ideators: a population-based study. Psychol Med. 2007;37:1551–62. doi: 10.1017/S0033291707000803. [DOI] [PubMed] [Google Scholar]
- 36.Marusic A, Farmer A. Toward s new classification of risk factors for suicide behaviour. Crisis. 2001;22:66–70. doi: 10.1027//0227-5910.22.2.43. [DOI] [PubMed] [Google Scholar]
- 37.Borges G, Angst J, Nock MK, et al. Risk factors for the incidence and persistence of suicide-related outcomes: a 10-year follow-up study using the national comorbidity surveys. J Affect Disord. 2008;105:25–33. doi: 10.1016/j.jad.2007.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stein DJ, Chiu WT, Hwang I, et al. Cross-national analysis of the associations between traumatic events and suicidal behavior: findings from the WHO World Mental Health Surveys. Plos One. 2010;5:e10574. doi: 10.1371/journal.pone.0010574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghazinour M, Mofidi N, Richter J. Continuity from suicidal ideations to suicide attempts? An investigation in 18–55 years old adult Iranian Kurds. Soc Psychiatry Psychiatr Epidemiol. 2010;45:973–81. doi: 10.1007/s00127-009-0136-z. [DOI] [PubMed] [Google Scholar]
- 40.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181:193–9. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 41.Suominen K, Isometsä E, Suokas J, et al. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161:562–3. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- 42.Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 1997;170:205–28. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 43.Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31:837–45. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- 44.DeJong TM, Overholser JC, Stockmeier CA. Apples to oranges? A direct comparison between suicide attempters and suicide completers. J Affect Disord. 2010;124:90–7. doi: 10.1016/j.jad.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- 46.Beck AT. In: Beyond belief: a theory of modes, personality, and psychopathology. Frontiers of cognitive therapy. Salkovskis PM, editor. New York: Guilford; 1996. pp. 1–25. [Google Scholar]
- 47.Reisch T, Seifritz E, Esposito F, et al. An fMRI study on mental pain and suicidal behavior. J Affect Disord. 2010;126:321–5. doi: 10.1016/j.jad.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 48.Joiner TE. The trajectory of suicidal behaviour over time. Suicide Life Threat Behav. 2002;32:33–41. doi: 10.1521/suli.32.1.33.22187. [DOI] [PubMed] [Google Scholar]
- 49.Arensman E, Kerkhof AJFM. Classification of attempted suicide: a review of empirical studies, 1963–1993. Suicide Life Threat Behav. 1996;26:46–64. [PubMed] [Google Scholar]
- 50.Hintikka J, Pesonen T, Saarinen P, et al. Suicidal ideation in the Finnish general population. A 12-month follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2001;36:590–4. doi: 10.1007/s127-001-8198-x. [DOI] [PubMed] [Google Scholar]
- 51.Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide: sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1096 patients with affective disorders. Arch Gen Psychiatry. 1991;48:418–22. doi: 10.1001/archpsyc.1991.01810290030004. [DOI] [PubMed] [Google Scholar]
- 52.De Leo D, Heller T. Intensive case management in suicide attempters following discharge from inpatient psychiatric care. Aust J Primary Health. 2007;13:49–59. [Google Scholar]
- 53.De Leo D, Sveticic J. Suicides in psychiatric patients: what are we doing wrong? Epidemiol Psichiatr Soc. 2010;19:8–15. [PubMed] [Google Scholar]


