Abstract
This study is a follow-up of inpatients diagnosed with severe depression/melancholia between 1956 and 1969. During this period, all inpatients at the Department of Psychiatry, University Hospital, Lund, were rated on a multidimensional diagnostic schedule on discharge. There were 471 patients born from 1920 onward. In the present follow-up, 2006 to 2010, 169 survivors could be traced. They were asked to participate in the study involving a telephone interview, in which a structured life chart was used. Of the patients contacted, 16 were ill or confused and 3 did not remember ever being depressed, leaving 150 who could participate. Seventy-five of these agreed to participate in the study. Long-term course of depression was evaluated by cluster analysis and compared to background variables, such as heredity for depression, perceived parental rearing behaviour, and treatment of index depressive episode. Using a cluster analysis the patients could be separated into six clusters describing the course: i) single or few episodes followed by long-lasting remission; ii) single or few episodes followed by long-lasting remission, although shorter; iii) single or few episodes followed by late recurrence; iv) single or few episodes, but more frequently ill, followed by late recurrence; v) several episodes followed by lasting remission; vi) chronic course of episodes. Remission or recurrence could therefore occur even after more than a decade. In summary, there was a short-term course with or without recurrence or a chronic course with or without late remission. Heredity for depression was significantly related to a chronic course with or without late remission.
Key words: severe depression, long-term course, remission, recovery.
Introduction
Depression is a common and serious condition. According to World Health Organization (WHO) it is the leading cause of disability counted in terms of years lived with disability and the third leading contributor to the global burden of disease (disability adjusted life years) in 2008.1
Many studies have been done in this field, including the Lundby Study which is a community study extending over 50 years and is often quoted. Recent data from this study has shown that the cumulative probability for developing a depression is 30.7% for women and 22.5% for men.2 The overall annual incidence was 3.5 per 1000 person/years. The Stirling County Study in Canada, a study comparable to Lundby, shows an overall annual incidence of 3.8 per 1000 person/years, remaining constant over 40 years.3
According to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM IV), mood disorders are subdivided into several groups.4 Depressions with melancholic and psychotic features are two of the most severe forms of major depressive disorder. In a study by Lafer et al.,5 17% of an outpatient sample of depressives met the criteria for melancholia according to DSM IV and in another report 15% of all depressed patients have had a depressive psychosis,6 with some overlap between the two groups.
Depression has been shown to have a poor outcome in many cases. The rate of recurrence is high, but number of episodes depends on the sampling of patients. As can be expected, community samples have shown a better outcome than hospital samples. The Lundby Study shows a recurrence rate of 40% for patients followed over forty years but a lower figure if the follow-up time is shorter.7 In contrast, a study carried out on 93 research inpatients shows that almost 80% relapsed within 5 years.8 The same study showed that the length of the period the patient was well between each episode decreases over time. In a review article, Angst et al. conclude that the rate of recurrence is 75–80% in all of the population of depressed patients and that recurrence often occurs within two years of the first episode.9 In a study by Kanai et al., less than half of the patients could expect to remain symptom-free for two years or more after recovery from a depressive episode.10 In a 23-year follow-up of a population-based cohort study, 50% recovered after first episode and had no future episodes.11 According to that study, 15% showed a chronic course.
A combination of number of previous episodes, length of illness, and early onset age are the best predictors of the course in early adulthood.12 The risk and rate of recurrence increases with each episode throughout the entire life span, according to several authors.13–15 Post et al. describe a sensitisation process with longer, deeper and more frequent episodes and a more self-acting course over time.16 Time after the first episode seems to be an important factor for future course. It is very important to attain lasting recovery after the first episode,17 since an incomplete recovery from first lifetime episode of major depression can predict a more severe and chronic future course.18
The risk of developing a chronic course defined by persistent symptoms for two years or more, and no recovery over a period of five years, is said to be 12–14% among patients with major depressive disorder or bipolar disorder.9 In a review article, Scott concludes that chronic depression is multifactorial; females and patients with a family history are at higher risk, and the length of illness episodes is the most powerful predictor of chronicity.19
It is interesting that despite all these reports of poor outcome there are still some patients that reach recovery. A review article of follow-up studies of depressed patients concludes that the weighted average of patients from a psychiatric setting that recover and remain continuously well for at least ten years after index episode is 24%.20 In the Zurich follow-up, the corresponding figure is 26%.9 In a prospective study over ten years, patients have been reported to recover even after five years of illness.21 In another study one patient recovered after 15 years of continuous symptoms.22 In their study on severely depressed inpatients, Brodaty et al. suggest that patients with a chronic course over 15 years can show improvement when monitored for a longer period.23 However, recurrence after many years of wellness has also been reported - in one study 12 years after first admission,22 indicating that a patient never falls out of the risk group for recurrence and the risk of recurrence seems to remain constant over the life-span up to the age of 70 or more.24
Knowledge of the course of the condition is very important for both patient and doctor. Many studies have already been done, but to our knowledge little is known about the very long-term course of severe depression since few studies extend over a very long period.
This study is a follow-up of inpatients diagnosed with severe depression/melancholia in the 1950s and 1960s. The aim of the study was to describe the very long-term course of the disease in terms of numbers of episodes, total time ill and total time well, recurrence, chronic course and recovery. The late course of depression was of major interest, including the possibility of remaining well and possible changes with remission or recurrence late in course.
Materials and Methods
Sample
Between 1949 and 1969 all inpatients at the Department of Psychiatry, University Hospital, Lund, were rated on a multidimensional diagnostic schedule on discharge.25 The schedule comprised three parts, one symptomatic, one syndromatic, and one etiologic. The ratings were carried out by senior psychiatrists with at least three years of training. From 1956 onwards, the diagnosis severe depression/melancholia was used. This diagnosis was given to 1206 patients (700 women and 506 men) up to 1969. Of these patients, 471 were born in 1920 and later and could be expected to be alive and able to participate in the follow-up in 2006-2010. The patients were followed up via Central Bureau of Statistics Sweden until 1 May 2006. Of the patients, 196 had died and another 106 could not be traced. Of the remaining 169 who were contacted, 16 could not participate due to dementia or other illness and another three did not remember ever being depressed. This left 150 who could participate in the study, and of these 75 agreed to be interviewed (24 men and 51 women). Of those who refused, 25 said that everything had happened so long ago and they did not want to stir it up again, another 5 appeared to be still depressed and did not want to participate for that reason. Out of other non-participators one had a manic episode, one had been well for 25 years but was on Lithium and one reported a late relapse of depression. Consequently, there was some, though incomplete, information about 33 persons apart from those interviewed, that is in all information about 108 persons. Age and gender showed a similar distribution among those who did participate and those who declined.
In an earlier study,26 a sub-sample of 178 patients from the original sample of 1206 patients had retrospectively been compared to DSM IV.4 The results showed good correspondence, with at least 91% of the patients meeting the criteria for major depressive disorder with melancholic or psychotic features.
Interviews and case record evaluations method
The telephone interview was based on a structured life chart procedure proposed by Post.8 The questions concerned heredity for depression, social situation, physical illness, current medications, course of depression, cause of onset and cause of recovery/remission, treatment, suicide attempts, childhood rearing experience, smoking and alcohol, etc. The questions about childhood were based on perception of contact with mother and father, a brief version of a questionnaire developed by Perris et al.27 as used by Ehnvall et al.28 We asked about number of episodes and number of hospitalisations, age or year for each episode, length of episodes, length of time well between episodes, and whether they reached full or only partial remission in between episodes.
Severe depression was diagnosed for all patients during their index episode (prospectively) and sometimes there was a relapse of severe episodes with real impairment which required hospitalization, treatment with ECT or antidepressants and so on. Then episodes could be less severe. Remission could be partial or complete. In partial remission there was no need for hospitalisation, medication or contact with health care and the person was able to function in work and daily life and had little sense of being depressed. Some stated that they were completely recovered. Relapse was considered when the person was again incapacitated. A period of several months well was required before a relapse could be considered.
Of those interviewed, 44 gave us permission to read their case records. Thirty-six of these case records could be found and read. In addition we had epicrises from index admission for all probands, including some of those for whom records were not found. Statistical analysis was first performed based on data received in the interviews. Thereafter, a validation was made against the data found in the subsample where information from the case records was also available.
Sociodemographic factors and physical illness are presented in Table 1.
Table 1. Socio-demographic characteristics and physical disease of the subjects interviewed.
| Males (n=24) | Females (n=51) | |
|---|---|---|
| Age at interview | 56-84 | 61-89 |
| Age at onset of depression | (12-42) | (13-42) |
| Marital state | ||
| Unmarried | 4 | 5 |
| Married/cohabitate | 13 | 22 |
| Divorced | 3 | 9 |
| Widow | 4 | 15 |
| Social group | ||
| Social group I | 2 | 0 |
| Social group II | 17 | 41 |
| Social group III | 4 | 2 |
| Physical disease | ||
| None | 3 | 7 |
| Disease related to old age* | 14 | 18 |
| Acute disease in younger days** | 5 | 17 |
| Chronic disease in younger days*** | 2 | 7 |
Such as artrosis or cardiac failure;
such as appendicitis or tbc;
such as rheumatoid arthritis or diabetes.
The average age at first episode was 27.25 years (±7.77). The average age at interview was 72.23 years (±7.93). The mean follow-up was 44.97 years (±3.96). A cluster analysis (see below) of depressive episodes was performed. The course of depression was further evaluated against heredity for depression, perceived parental rearing, and treatment of index depressive episode.
Statistics
We used a cluster analysis to divide the 75 interviewed patients into various clusters that would represent different outcomes of the course [Stata, special edition, 9.2 (www.stata.com) with commando cluster cen-troidlinkage which according to the manual performs hierarchical agglomerative centroid linkage cluster analysis].
Variables that could be used to group the patients were:
Number of well episodes and number of ill episodes;
Total length of all well episodes and total length of all ill episodes;
Length of the longest period of wellness and length of the total time of illness;
Length of the latest well episode and length of the latest ill episode.
Because some of these variables are strongly correlated with each other we first had to do a principal component analysis. This resulted in following usable variables:
Total time the patient was ill;
Total number of episodes ill;
Length of the longest time well;
Whether remission occurred at the time for the interview, and length of this remission.
Cluster analyses were performed with both partial and complete remission, but as it may be difficult to state complete remission, we have chosen to present the results for partial remission.
We also noted gender and whether there was a history of mania, schizophrenia or any period in life with substance abuse.
The local Ethics Committee, Lund University, approved the study. All probands had given their written informed consent to participate in the study.
Results
Self-reported course of depression
When all ill episodes, including all true episodes, were separated from well episodes, a cluster analysis using the variables described above gave six different groups describing six different long-term courses of severe depression.
The clusters are described in Table 2 and were as follows: i) cluster A single or few episodes followed by long-lasting remission: this cluster contained 15 persons, 6 men and 9 women; ii) cluster B single or few episodes followed by long-lasting remission, although shorter than A: this cluster contained 24 persons, 7 men and 17 women; iii) cluster C single or few episodes followed by late recurrence: this cluster contained 6 persons, 2 men and 4 women; iv) cluster D single or few episodes, similar to C but more frequently ill, followed by late recurrence: this cluster contained 6 persons, 1 man and 5 women; v) cluster E several episodes followed by lasting remission: this cluster contained 11 persons, 2 men and 9 women; vi) cluster F chronic course of episodes: this cluster contained 13 persons, 6 men and 7 women.
Table 2. Clusters describing the long-term course of depression.
| Cluster | Number of episodes | Time well | Time well since last episode | Comorbidity |
|---|---|---|---|---|
| A | 1-5 ill episodes | 96-99% | 44-54 years | None |
| N=15 | ||||
| 6 men | ||||
| 9 women | ||||
| B | 1-8 ill episodes | 88-99% | 28-42 years | 1 mania |
| N=24 | 1 subst abuse | |||
| 7 men | 1 schizophrenia | |||
| 17 women | ||||
| C | 2-4 ill episodes | 88-96% | 0-3 years | none |
| N= 6 | Late recurrence | 34-46 years | ||
| 2 men | Before recurrence | |||
| 4 women | ||||
| D | 2-6 ill episodes | 63-96% | 0-9 years | none |
| N=6 | Late recurrence | 19-31 years | ||
| 1 man | Before recurrence | |||
| 5 women | ||||
| E | 2-10 ill episodes | 32-96% | 12-29 years | 2 mania |
| N=11 | ||||
| 2 men | ||||
| 9 women | ||||
| F | 1-11 ill episodes | 0-85% | 0-9 years | 2 mania |
| N=13 | 1 subst abuse | |||
| 6 men | 2 schizophrenia | |||
| 7 women |
In summary, there was a short course with or without late recurrence or a chronic course with or without lasting remission. In other words both recurrence and remission could be seen very late in the course. It should be noted that none of the late recurrences required hospital admission and could probably not be considered severe. Examples of long-term course are presented in the form of life-charts in Figure 1.
Figure 1.
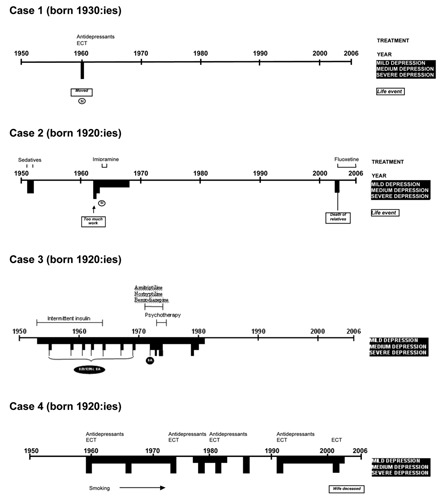
Life chart exemplifying four of the clusters: including severity of depression, treatment, suicide attempts, and life events. One case (number 3) from Brådvik and Crona 2009.32
The rates of different course for participants and those who declined but gave some information and are summed up in Table 3. The rates appear fairly similar when those who declined are included. A minimum of 64/150 persons (43%-those who declined included) reported long-term wellness.
Table 3. Number of patients who participated in the study compared to those who declined but gave information of course (percent).
| Subjects interviewed (N=75) | Subjects who gave some information (N=108) | |
|---|---|---|
| Few episodes | 39 (52) | 64 (59) |
| Long-term recovery | ||
| Few episodes | 12 (16) | 13 (12) |
| Late reccurrence | ||
| Chronic course | 11 (15) | 12 (11) |
| Lasting remission | ||
| Chronic course | 13 (17) | 19 (18) |
Background factors
Heredity shows an odds ratio of 5.09 (confidence interval=1.8, 14.6), P=0.002 for chronic course as compared to no or unknown heredity. Perceived negative childhood rearing showed no increased odds ratio for chronic course of depression. Thus heredity rather than negative experiences of childhood was related to chronic course of depression.
Socio-demographic factors, such as marital status and socioeconomic class did not differentiate between chronic and non-chronic course and neither did physical illness.
Treatment of depression
There were similar rates in adequate treatment at index admission between short-term and chronic course, 47/51 (92%), versus 21/24 (88%). In all, 65/79 (82%) of the episodes were adequately treated. Only one person in cluster A was on antidepressants and five in cluster B. In cluster C one person was taking antidepressants and two were on Lithium. Consequently, long-term remission was mostly achieved without present medication.
Case records
Twenty-six of the 37 case records that were read showed a very good correlation to the cluster analysis. Six people had moved and were reported to have continuous case records elsewhere, which would fit with their chronic course, and five persons in clusters D and E reported later recurrences not described in the records, indicating that they had applied for help elsewhere. This means that more episodes were reported in the interviews than were found in the case records. We did not find any episodes described in the case records that were not reported in the interviews.
Discussion
Main findings
This is a naturalistic study of the very long-term course of severe depression. In this study, patients diagnosed with severe depression/ melancholia in the 1950s or 60s were followed up by telephone interview, and case records were read. In general there is an increased mortality in severe depression,29,30 but those who were still alive 37 to 53 years after their first episode were traced. The long-term course of severe depression can best be described in terms of single or few episodes followed by long-lasting remission with or without late recurrence, several episodes followed by late remission, or a chronic course of episodes without remission.
In a naturalistic study of hospital admissions for severe depression (melancholia and psychosis) from 1875 to 1924 in Wales, a positive outcome with fewer admissions later in life was also found, which supports the view that there are not always life-long recur-rences.31 However, that study only dealt with hospital admissions and concerned the pre-treatment era.
Single or few episodes followed by long-lasting remission
There was a high number (39/75) of single or few episodes with full long-lasting remission. This number is higher than in the Zurich follow-up,9 where over 70% failed to recover from their depressive disorder over the 25-year follow-up period, i.e. only 30% recovered. This is interesting since we have studied severely depressed patients who may be expected to have a worse course than patients with Major Depressive Disorder as in the Zurich follow-up. Late onset, meaning debut of depression after the age of 50, has been shown to increase the risk of recurrence and also a chronic course according to Angst et al.9 This could be one explanation for us seeing more single or few episodes in our study, since those who were older when the study started are not included in this third follow-up because they had already died or were too old to participate.
Late recurrence
Two clusters of patients had a very late recurrence, in all 12/75. After one, two, or more episodes they recovered for many years and then had a recurrence in old age. This supports the view of Lee et al., which was that patients never escape entirely from the risk of readmis-sion.22 In their study one patient was readmitted after 12 years of being well. We saw recurrence after much longer, in one case a women with a single episode had a recurrence after 48 years. However, depression is fairly common among older people, and often secondary to physical illness, loneliness, etc. We could not tell whether the late recurrences that we saw in our study were a true recurrence to their earlier depressive history or if it was secondary to other circumstances. Maybe people with a history of depression, even if only a single episode in younger age, have an increased vulnerability to develop a depression caused by different circumstances related to ageing. It should be noted that late recurrence was usually non-severe.
Several episodes followed by lasting recovery
A very interesting, and probably the most unexpected, finding was that long-term recovery is possible after a severe course with several episodes over long time. This cluster contained 11/75 of the sample. They have all had a course with a long period of illness followed by lasting remission. In an earlier article we have described two individual cases where lasting recovery for 30 and 25 years was seen after a depressed period without full inter-episode remission for 16 and 29 years respec-tively.32 Other studies support this outcome,22,23 but in both of these the follow-up time was shorter and in the latter patients less severely ill. Patients with major depressive disorder are a larger group of depressed patients and we have studied only severely depressed people for whom a worse course might be expected. In this study we have shown that remission is possible in several cases even if the course and depression has been chronic, in other words the proposed kindling phenomenon may be reversed after a long time. 16
Chronic course of episodes
Along with other studies we found that many patients develop a chronic course of depression with several episodes and without full remission in between. The number of patients that develop a chronic course is said to be 12–15%,9,19 and the number was similar in our study (13/75, 17%). It appears that chronic course could extend over several decades in some unfortunate cases, to our knowledge longer than has previously been shown. In the cluster analysis (Table 2) there was a wide range of time being well in the chronic group, 0–85%, which is puzzling. This group was therefore studied in detail. In one case there was a long-lasting first episode and a lasting latest episode as the person was still clearly depressed when interviewed. This person was well 85% of the time but was also considered to have a chronic course. The remaining twelve persons in this cluster had repeated episodes all through their lives and appeared to be ill much more than 15% of the time.
There was a significant relationship between heredity of depression and chronic course of depression but no relationship between perceived unhappy childhood and chronic course. This supports the view of severe depression being mainly endogenous in nature, and it was previously called endogenous depression. A correlation between heredity of depression and chronic course, and episode length of more than two years, has also been reported by Scott,19 which to some extent corresponds with the present findings.
Three people in the total sample had developed schizophrenia. This is a much lower figure than in a study by Lee et al.,22 whose sample contained a high incidence of other disorders (schizoaffective disorder, schizophrenia and alcoholism) and few had a pure unipolar recurrent history. Five persons had mania, which corresponds with another study reporting that 4.4 % of the depressed inpatients will develop a bipolar disorder,33 though in a recent consensus meeting a long-term risk above 10% was estimated, including hypomania.34 Only two persons reported substance abuse.
Strength and limitations
To the best of our knowledge no one has described the very long-term course of severe depression, and that is what makes this study unique. Two community studies are of similar length of follow-up, the Lundby Study (50 years) and the Stirling County Study (40 years),3,7 but neither is quite compatible to the present study, which deals with severe depression and describes the course of the depression apart from incidence of recurrence. There is also the Zurich follow-up study that started in 1959 and focused on patients diagnosed with major depression or bipolar disorder, which is also a wider concept of depression.9 Our sample is a fairly homogeneous group of patients diagnosed with a first episode severe depression in the ages 13 to 45. In an earlier study, the correspondence with DSM IV criteria for Major Depressive Disorder with melancholic or psychotic features was shown to be good.26 Furthermore, no late onset depression is included and no depression secondary to senile dementia or stroke included, which is a strength.
This study has some limitations. Along with the great advantage of having a long follow-up time, we have to deal with limitations such as recall bias. Most of the people in the study were old and said they did not remember exact facts about earlier happenings. Telephone interviews alone cannot give a complete picture of the course, but in most cases the telephone interviews showed good agreement with the case records and we believe our results are valuable. Also there were somewhat more episodes reported in the interviews than were found in the case records, showing that people do not tend to forget an episode of depression. Another limitation is the high number of people not wanting to participate, and only 50% agreed. However, this was not a low number considering the long time that had passed. Information about the course of illness was available also for 33 persons who declined, that is in all 72% made a report on the course of illness. There were similar rates of course when those who declined but gave some information were included. However, long-term wellness or chronic course were probably more easily reported and may be somewhat overrepresented. Still, it is quite safe to conclude that between 43% and 59% remained well after one or a few episodes. However, we know less about how representative the other clusters are, and they may only exemplify possible courses of depression. We found out that recurrence may occur after several decades and that remission/recovery is possible after several decades, but we cannot conclude how often it may happen.
We have chosen to present the results for partial remission rather than complete recovery. It would be more difficult to decide when someone is completely recovered and there is a true change from severe depression and they are on the whole non-depressed. Basically the same clusters were received for both analyses but with somewhat smaller numbers of positive outcome.
Finally, it should to be mentioned is that cluster analyses ideally require replication to demonstrate reliability. With a small sample it is not possible to divide the sample into two parts and repeat the cluster analysis. Thus, it is quite possible that another study would find a different set of clusters than that found here.
Conclusions
The long-term course of severe depression can best be described as single or few episodes followed by long-lasting remission, single or few episodes followed by late recurrence, several episodes followed by lasting remission or chronic course of episodes. In summary, there was a short-term course with or without recurrence or a chronic course with or without late remission. At least 43% stayed well for a long time after few episodes. Heredity for depression appears to be a risk factor for chronic course.
Acknowledgements:
Arne Frank assisted with the register follow-up. Kristina Hansen assisted with the case record evaluation. Mats Berglund gave valuable comments. Anna Lindgren, Mathematical Statistics, Centre of Mathematical Sciences, provided statistical advice. Leslie Walke revised the language. Eva Skagert prepared the figures.
References
- 1.World Health Organization. Depression. What is depression? Available from: http://www.who.int/mental_health/management/depression/definition/en/
- 2.Mattisson C, Bogren M, Nettelbladt P, et al. First incidence depression in the Lundby Study: a comparison of the two time periods 1947-1972 and 1972-1997. J Affect Dis. 2005;87:151–60. doi: 10.1016/j.jad.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Murphy JM, Laird NM, Monson RR, et al. Incidence of depression in the Stirling County Study: historical and comparative perspectives. Psychol Med. 2000;30:505–14. doi: 10.1017/s0033291799002044. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. (DSM IV) Fourth Edition. DSM- IV Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 5.Lafer B, Nierenberg AA, Rosenbaum JF, Fava M. Outpatients with DSM-III-R versus DSM-IV melancholic depression. Compr Psychiatry. 1996;37:37–9. doi: 10.1016/s0010-440x(96)90048-6. [DOI] [PubMed] [Google Scholar]
- 6.Sadock BJ, Sadock VA. Kaplan & Sadock's Comprehensive Textbook of Psychiatry. 7th edition. Baltimore: Lippincott, Williams & Wilkins; 2000. Mood Disorders; pp. 1284–1440. [Google Scholar]
- 7.Mattisson C, Bogren M, Horstmann V, et al. The long-term course of depressive disorders in the Lundby Study. Psychol Med. 2007;111:883–91. doi: 10.1017/S0033291707000074. [DOI] [PubMed] [Google Scholar]
- 8.Roy-Byrne P, Post RM, Uhde TW, et al. The longitudinal course of recurrent affective illness: life chart data from research patients at the NIMH. Acta Psychiatr Scand. 1985;317(Suppl1):1–34. doi: 10.1111/j.1600-0447.1985.tb10510.x. [DOI] [PubMed] [Google Scholar]
- 9.Angst J, Kupfer DJ, Rosenbaum J. Recovery from depression: risk or reality? Acta Psychiatr Scand. 1996;93:413–9. doi: 10.1111/j.1600-0447.1996.tb10671.x. [DOI] [PubMed] [Google Scholar]
- 10.Kanai T, Takeuchi H, Furukawa TA, et al. Time to recurrence after recovery from major depressive episodes and its predictors. Psychol Med. 2003;33:839–45. doi: 10.1017/s0033291703007827. [DOI] [PubMed] [Google Scholar]
- 11.Eaton WW, Shao H, Nestadt G, et al. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry. 2008;65:513–20. doi: 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pettit JW, Lewinsohn PM, Roberts RE, et al. The long-term course of depression: development of an empirical index and identification of early adult outcomes. Psychol Med. 2009;39:403–12. doi: 10.1017/S0033291708003851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kessing LV, Andersen EW, Andersen PK. Predictors of recurrence in affective disorder - analyses accounting for individual heterogeneity. J Affect Dis. 2000;57:139–45. doi: 10.1016/s0165-0327(99)00080-4. [DOI] [PubMed] [Google Scholar]
- 14.Kessing LV, Hansen MG, Andersen PK, Angst J. The predictive effect of episodes on the risk of recurrence in depressive and bipolar disorders - a life-long perspective. Acta Psychiatr Scand. 2004;109:339–44. doi: 10.1046/j.1600-0447.2003.00266.x. [DOI] [PubMed] [Google Scholar]
- 15.Solomon DA, Keller MB, Leon AC, et al. Multiple recurrences of major depressive disorder. Am J Psychiatry. 2000;157:229–33. doi: 10.1176/appi.ajp.157.2.229. [DOI] [PubMed] [Google Scholar]
- 16.Post RM, Rubinow DR, Ballenger JC. Conditioning and sensitisation in the longitudinal course of affective illness. Br J Psychiatry. 1986;149:191–201. doi: 10.1192/bjp.149.2.191. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg JF, Harrow M. Consistency of remission and outcome in bipolar and unipolar mood disorders: a 10-year prospective follow-up. J Affect Dis. 2004;81:123–31. doi: 10.1016/S0165-0327(03)00161-7. [DOI] [PubMed] [Google Scholar]
- 18.Judd LL, Paulus MJ, Schettler PJ, et al. Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? Am J Psychiatry. 2000;157:1501–4. doi: 10.1176/appi.ajp.157.9.1501. [DOI] [PubMed] [Google Scholar]
- 19.Scott J. Chronic Depression. Br J Psychiatry. 1988;153:287–97. doi: 10.1192/bjp.153.3.287. [DOI] [PubMed] [Google Scholar]
- 20.Piccinelli M, Wilkinson G. Outcome of depression in psychiatric settings. Br J Psychiatry. 1994;164:297–304. doi: 10.1192/bjp.164.3.297. [DOI] [PubMed] [Google Scholar]
- 21.Mueller TI, Keller MB, Leon AC, et al. Recovery after 5 years of unremitting major depressive disorder. Arch Gen Psychiatry. 1996;53:794–9. doi: 10.1001/archpsyc.1996.01830090040006. [DOI] [PubMed] [Google Scholar]
- 22.Lee AS, Murray RM. The long-term outcome of Maudsley depressives. Br J Psychiatry. 1988;153:741–71. doi: 10.1192/bjp.153.6.741. [DOI] [PubMed] [Google Scholar]
- 23.Brodaty H, Luscombe G, Peisah C, et al. A 25-year longitudinal, comparison study of the outcome of depression. Psychol Med. 2001;31:1347–59. doi: 10.1017/s0033291701004743. [DOI] [PubMed] [Google Scholar]
- 24.Angst J, Gamma A, Sellaro R, et al. Recurrence of bipolar disorders and major depression. A life-long perspective. Eur Arch Psychiatry Clin Neurosc. 2003;253:236–40. doi: 10.1007/s00406-003-0437-2. [DOI] [PubMed] [Google Scholar]
- 25.Essen-Möller E, Wohlfahrt S. Suggestion for the amendment of the official Swedish classification of mental disorders. Psychol Med. 1947;1:308–11. doi: 10.1017/s0033291700042276. [DOI] [PubMed] [Google Scholar]
- 26.Brådvik L, Berglund M. Treatment and suicide in severe depression. A case-control study on antidepressant therapy at last contact before suicide. J ECT. 2000;16:399–408. doi: 10.1097/00124509-200012000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Perris C, Jacobsson L, Lindström H, et al. Development of a new inventory assessing memories of parental rearing behaviour. Acta Psychiatr Scand. 1980;61:265–74. doi: 10.1111/j.1600-0447.1980.tb00581.x. [DOI] [PubMed] [Google Scholar]
- 28.Ehnvall A, Palm-Beskow A, Beskow J, Agren H. Perception of rearing circumstances relates to course of illness in patients with therapy-refractory affective disorders. J Affect Disord. 2005;86:299–303. doi: 10.1016/j.jad.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Berglund M, Nilsson K. Mortality in severe depression. A prospective study including 103 suicides. Acta Psychiatr Scand. 1987;76:372–80. doi: 10.1111/j.1600-0447.1987.tb05621.x. [DOI] [PubMed] [Google Scholar]
- 30.Brådvik L, Berglund M. Late mortality in severe depression. Acta Psychiatr Scand. 2001;103:111–16. doi: 10.1034/j.1600-0447.2001.00212.x. [DOI] [PubMed] [Google Scholar]
- 31.Harris M, Farquhar F, Healy D, et al. The incidence and prevalence of admissions for melancholia in two cohorts (1875-1924 and 1995-2005) J Affect Disord. 2011;34:45–51. doi: 10.1016/j.jad.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 32.Brådvik L, Crona L. Long-lasting recovery in chronic severe depression. Follow-up of two cases, 46 and 50 years after their first admissions for depression. Am J Case Reports. 2009;10:31–5. [Google Scholar]
- 33.Kessing LV. The effect of the first manic episode in affective disorder: a case register study of hospitalised episodes. J Affect Dis. 1999;53:233–9. doi: 10.1016/s0165-0327(98)00126-8. [DOI] [PubMed] [Google Scholar]
- 34.Goodwin GM, Anderson I, Arango C, et al. ECNP consensus meeting. Bipolar depression. Nice, Eur Neuropsychopharm. 2007;18:535–49. doi: 10.1016/j.euroneuro.2008.03.003. [DOI] [PubMed] [Google Scholar]


