Abstract
Background Context
Although the high cost of spine surgery is generally recognized, there is little information about the extent to which payments vary across hospitals.
Purpose
To examine variation in episode payments for spine surgery in the national Medicare population. We also sought to determine root causes for observed variations in payment at high cost hospitals.
Study Design/Setting
All patients in the national fee for service Medicare population undergoing surgery for three conditions (spinal stenosis, spondylolisthesis, lumbar disc herniation) between 2005-2007.
Patient Sample
185,954 episodes of spine surgery performed between 2005-2007.
Outcome Measures
Payments per episode of spine surgery.
Methods
All patients in the national fee for service Medicare population undergoing surgery for three conditions (spinal stenosis, spondylolisthesis, lumbar disc herniation) between 2005-2007 were identified (n = 185,954 episodes of spine surgery). Hospitals were ranked on least to most expensive and grouped into quintiles. Results were risk- and price-adjusted using the empirical Bayes method. We then assessed the contributions of index hospitalization, physician services, readmissions and post-acute care to the overall variations in payment. This study was funded in part by a grant from the National Institutes of Aging. There are no conflicts of interest associated with this study.
Results
Episode payments for hospitals in the highest quintile were more than twice as high as those made to hospitals in the lowest quintile ($34,171 vs $15,997). After risk- and price-adjustment, total episode payments to hospitals in the highest quintile remained $9,210 (47%) higher. Procedure choice, including the use of fusion, was a major determinant of the total episode payment. After adjusting for procedure choice, however, hospitals in the highest quintile continued to be 28% more expensive than those in the lowest. Differences in the use of post-acute care accounted for most of this residual variation in payments across hospitals. Hospital episode payments varied to a similar degree after subgroup analyses for disc herniation, spinal stenosis and spondylolisthesis. Hospitals expensive for one condition were also found to be expensive for services provided for other spinal diagnoses.
Conclusions
Medicare payments for episodes of spine surgery vary widely across hospitals. As they respond to the new financial incentives inherent in healthcare reform, high cost hospitals should focus on the use of spinal fusion as well as post-acute care.
Level of Evidence
II (Prognostic)
Keywords: Medicare payments, spine surgery, health policy
Introduction
It is well known that the treatment of spinal conditions is expensive, both due to the large numbers of patients who experience spine related problems and the high costs associated with the management of these issues.1 In the first decade of the 21st century, an estimated 3.6 million fusion-based procedures alone were performed in the spine, at a cost of more than $287 billion.2 Within the Medicare population, the rate of complex spinal surgery has increased nearly 15-fold since 20023, and the cost burden associated with spinal disorders is now thought to exceed that of diabetes as well as cardiovascular disease1,4. A sizable proportion of expenses associated with spinal care are incurred as a result of spine surgery, where a lack of consensus regarding accepted indications for procedural utilization results in wide variation in the type of surgery performed for similar conditions.1,3,5,6
Although variation in rates of surgery are widely recognized, episode payments for patients undergoing spine surgery may vary to a similar extent. Recent analyses of coronary artery bypass grafting, colectomy and total hip arthroplasty have appreciated differences in payment to high cost hospitals upwards of 50% as compared to low cost facilities.7,8,9 Payments for spine surgery could vary even more based on differences in the use of complex interventions and fusion-based procedures, which are both known to elevate the cost of spinal care.1,3,4,5 Moreover, disagreements regarding indications for the use of post-acute care may further compound differences in payments across hospitals.
In this context, we examined Medicare payments around episodes of surgery for three common spinal disorders. Additionally, we also planned to assess the types of services most responsible for differences in payments across hospitals based on the type of procedure performed and the use of post-acute care.
Methods
This investigation was performed using complete Medicare claims data for a sample of patients who underwent inpatient procedures from January 2005 to November 2007. Episodes of surgical care were defined as beginning on the date of admission for the spinal procedure and ending 30-days following the date of hospital discharge. In order to ensure that complete postoperative payment data was available for all procedures in the cohort, surgeries performed in December of 2007 were excluded from review. In addition, individuals enrolled in Medicare managed care plans, patients under age 65 or aged greater than 99 and those who were not enrolled in both Medicare Part A and Part B at the time of their procedure were also excluded from further analysis.
The Medicare Provider Analysis and Review (MedPAR) file for the dataset was queried by International Classification of Diseases, 9th Revision (ICD-9) code to identify patients who were treated with a primary diagnosis of spinal stenosis (721.42, 721.91,724.02), spondylolisthesis (738.4, 756.11, 756.12) or lumbar disc herniation (722.10, 724.4). As a means of enhancing the statistical reliability of payment estimates, individuals who were residents of nursing homes prior to surgery and those who had their surgeries performed at institutions that treated less than 30 total cases of the condition under consideration were excluded from the cohort. For similar reasons, patients whose procedures were performed by physicians other than a neurosurgeon or orthopaedic surgeon based on physician specialty code, or where the specialty of the operative surgeon could not clearly be determined, were also removed. Records of identified individuals were then linked to other Centers for Medicare and Medicaid Services (CMS) files that contained claims related to the performance of surgery, physician fees and post-acute care, a category comprised of payments for acute/long-stay rehabilitation hospital, skilled nursing facility, outpatient services, home health care, hospice and durable medical equipment.
For each patient included in the cohort, surgical procedure was determined by ICD-9 procedure codes and categorized as decompression (e.g. discectomy, laminotomy or laminectomy without fusion) or fusion (e.g. posterolateral fusion or anterior, posterior or transforaminal interbody fusion, or 360 degree fusion). Demographic information was also obtained, including age, sex and race. The presence of medical co-morbidities was recorded, including diabetes, congestive heart failure, coronary artery disease and renal insufficiency, as well as an overall modified Elixhauser co-morbidity score.10 Payment information was then collected for all types of service from the time of hospital admission for the primary surgical procedure until thirty days following the date of hospital discharge. Only actual Medicare payments, and not submitted charges, were considered in this study. Total payment data was stratified into four components: payments related to the index hospitalization, physician fees, readmissions, and post-acute care. Payments were then price-standardized using methods previously described9,11 to account for intended differences in payment rates by CMS (by year, regional wage and prices and Graduate Medical Education expenses).
Statistical Analysis
Within each spinal diagnosis, hospitals were initially ranked according to total episodic payments and categorized into quintiles. Hospital payment quintiles were then reassigned after accounting for price standardization and again following price, indication and case-mix adjustment, where clustering of patients at different hospitals according to demographic, co-morbidity, and illness severity characteristics was taken into account. Case-mix adjustment was performed using multiple linear regression that adjusted for patients' sex, race, age, illness severity at the time of admission, spinal diagnosis and length of stay prior to surgery. In order to reduce the potential for confounding due to unmeasured differences in illness acuity and costliness at baseline, services incurred in the six months prior to surgery were also accounted for. All adjustments were performed using the empirical Bayes method, in order to generate the most conservative estimates of payment variation across hospitals.
Once price, indication and case-mix adjusted hospital quintiles were established for each of the three spinal disorders, differences in payment between hospitals in the 1st (lowest payment) and 5th (highest payment) quintiles were assessed, evaluating the contributions of the index hospitalization, readmission, physician services and post-acute care to overall expense. Additionally, comparisons were made between hospitals in the 1st and 5th quintiles after adjusting for the performance of fusion-based procedures. Lastly, we evaluated the hospital-level correlation between price, indication and case-mix adjusted payments for the treatment of disc herniation, spinal stenosis and spondylolisthesis.
All statistical testing was performed using Statistical Analysis Software (SAS) version 9.3 (SAS Institute, Cary, NC) with significance set, a-priori, at p-values <0.05. The University of Michigan investigational review board determined that this study was exempt from regulatory review.
Results
Our study cohort consisted of 185,954 episodes of spine surgery performed between 2005-2007. Overall, the average total payment per episode of spine care was $24,100, which reduced to $23,877 after price, case-mix and indication adjustment. Actual episode payments to hospitals in the highest quintile were more than twice as high (113%) as payments made to hospitals in the lowest quintile ($34,171 vs $15,997, Table 1). After price-, case-mix, and indication adjustment, total episode payments to hospitals in the highest quintile remained 47% ($9,210) higher ($28,952 vs $19,742) and were still 28% ($6,020) greater after controlling for procedure (Table 1).
Table 1.
Average total Medicare payments& around episodes of care for three common spinal conditions, 2005-2007.
| All Spinal Diagnoses | 1st Quintile | 2nd Quintile | 3rd Quintile | 4th Quintile | 5th Quintile | Difference btw 1-5 | Percent Difference |
|---|---|---|---|---|---|---|---|
| Actual Payment | 15997 | 20427 | 23277 | 26609 | 34171 | 18174 | 113 |
| Payment after price adjustment | 17305 | 21290 | 23535 | 26123 | 31119 | 13814 | 79 |
| Payment after price, case-mix and indication adjustment | 19742 | 22100 | 23443 | 25140 | 28952 | 9210 | 47 |
| Payment after price, case-mix, indication and procedure (fusion vs decompression) adjustment | 21270 | 22736 | 23578 | 24506 | 27290 | 6020 | 28 |
-Rounded to the nearest dollar
Table 2 summarizes the demographic characteristics for patients in each quintile of risk-adjusted episode payment. Patients in the highest payment-quintile were more likely to have three or more Elixhauser co-morbidities and to be African-American. Differences in patient characteristics across quintiles were small as compared to differences in payments.
Table 2.
Characteristics of the patients undergoing spine surgery between 2005-2007, by quintiles of payments to hospitals.
| Diagnosis | Overall | 1st Quintile | 2nd Quintile | 3rd Quintile | 4th Quintile | 5th Quintile | P-value for Difference Between 1-5 |
|---|---|---|---|---|---|---|---|
| All Spinal Diagnoses | |||||||
| Mean Cost (price, case-mix and indication adjusted) | $23,877 | $19,742 | $22,100 | $23,443 | $25,140 | $28,952 | <0.001 |
| Age (mean) | 74.4 | 74.5 | 74.3 | 74.4 | 74.4 | 74.3 | 0.004 |
| Male Sex (%) | 40.3 | 42.2 | 40.5 | 39.7 | 39.7 | 39.3 | <0.001 |
| African-American (%) | 3.6 | 2.3 | 3.7 | 3.7 | 4.0 | 4.3 | <0.001 |
| Three or more Elixhauser Co-morbidities (%) | 22.8 | 20.5 | 21.8 | 22.6 | 23.5 | 25.1 | <0.001 |
| Surgical Indication | |||||||
| Disc Herniation (%) | 30.1 | 41.3 | 30.8 | 29.7 | 26.0 | 23.7 | <0.001 |
| Spinal stenosis (%) | 30.1 | 28.4 | 28.5 | 29.7 | 31.2 | 32.1 | <0.001 |
| Spondylolisthesis (%) | 39.8 | 30.4 | 40.7 | 41.5 | 42.8 | 44.2 | <0.001 |
| Patients with a fusion-based procedure (%) | 40.7 | 23.8 | 37.1 | 40.3 | 46.6 | 50.6 | <0.001 |
Evaluation of the differences in payment for components of care within surgical episodes revealed that index hospitalization (39%) and post-acute care (39%) accounted for the greatest proportion of payment variation between highest- and lowest-payment hospitals (Figure 1). Physician services accounted for only 12% of the payment difference between hospitals in the 1st and 5th quintiles and payments related to readmission were responsible for even less (10%).
Figure 1.
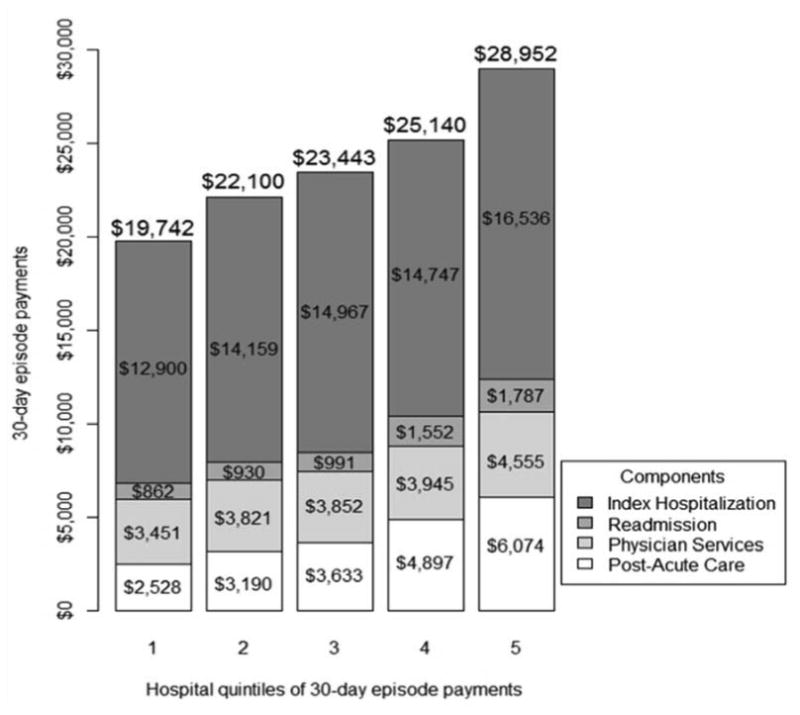
Differences in price-, case-mix, and indication adjusted payments to hospitals for episodes of spine surgery, 2005-2007.
Differences in payments for index hospitalization across quintiles were almost entirely eliminated once the performance of fusion was taken into account (Table 3). Among all spinal indications, residual differences in payment following adjustment for fusion-based procedures, were largely attributable (63%, $3,788) to differences in post-acute care. This was further magnified for the indication of disc herniation, where 85% ($2,443) of the variation in payments was accounted for by post-acute care. Additionally, following adjustment for fusion-based procedures, the percentage of payment variation attributable to hospital readmission also increased substantially, ranging from 20% ($1,412) in the setting of spondylolisthesis to 50% ($1,401) for disc herniation (Table 3).
Table 3. Average Medicare payments* for different components of care around surgical episodes, by indication, 2005-2007.
| Indication | 1st (Lowest Payment) | 5th (Highest Payment) | Difference btw 1-5 | Percent of total difference attributed to component of care& |
|---|---|---|---|---|
| All Spinal Indications | ||||
| Index Hospitalization | 14441 | 14961 | 520 | 9 |
| Readmission | 853 | 1939 | 1086 | 18 |
| Physician Services | 3619 | 4245 | 626 | 10 |
| Post-acute Care | 2357 | 6145 | 3788 | 63 |
| Total Episode | 21270 | 27290 | 6020 | 100 |
| Disc Herniation | ||||
| Index Hospitalization | 9646 | 8537 | -1109 | -39 |
| Readmission | 435 | 1836 | 1401 | 50 |
| Physician Services | 2572 | 2700 | 128 | 4 |
| Post-acute Care | 1344 | 3787 | 2443 | 85 |
| Total Episode | 13998 | 16860 | 2862 | 100 |
| Spinal Stenosis | ||||
| Index Hospitalization | 14360 | 13478 | -882 | -16 |
| Readmission | 788 | 2765 | 1977 | 37 |
| Physician Services | 3760 | 4051 | 291 | 5 |
| Post-acute Care | 2696 | 6679 | 3983 | 74 |
| Total Episode | 21604 | 26974 | 5370 | 100 |
| Spondylolisthesis | ||||
| Index Hospitalization | 19310 | 19705 | 395 | 6 |
| Readmission | 666 | 2078 | 1412 | 20 |
| Physician Services | 4465 | 5279 | 814 | 11 |
| Post-acute Care | 2807 | 7291 | 4484 | 63 |
| Total Episode | 27248 | 34351 | 7103 | 100 |
- After price, case-mix, indication and procedure (fusion vs decompression) adjustment and rounded to the nearest dollar
- Percent difference may not equal 100% due to rounding
Strong correlations (Figure 2) were appreciated between episode payments for the treatment of disc herniation and spinal stenosis (0.88), spinal stenosis and spondylolisthesis (0.87) and disc herniation and spondylolisthesis (0.78). Thus, it would appear that hospitals that were expensive for the treatment of one spinal condition were also expensive for services provided for other spinal diagnoses.
Figure 2.
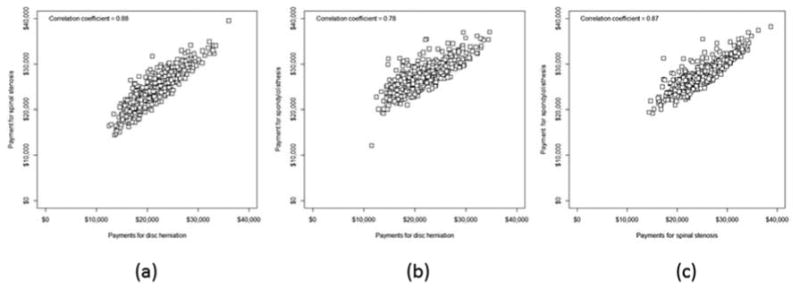
Relationship between price- and case-mix adjusted total episode payments to hospitals for disc herniation and spinal stenosis (a), disc herniation and spondylolisthesis (b) and spinal stenosis and spondylolisthesis (c).
Discussion
This study was performed to examine differences in Medicare payments for hospital and physician services, as well as post-acute care, within three common indications for spine surgery: lumbar disc herniation, spinal stenosis, and spondylolisthesis. Our results indicate that there is large variation in Medicare payments to hospitals around episodes of spine surgical care. Even after controlling for intentional differences in payments due to disparities in regional wages, indications for surgery and hospital case-mix, facilities in the highest-quintile received payments that were 47% higher on average than institutions in the lowest-quintile. When evaluating the underlying cause of variations in payment, particularly following procedure adjustment that accounted for the performance of fusion, a majority of the difference was attributable to potentially discretionary services such as post-acute care followed by payments related to readmission. Strong correlations at the hospital level were noted for payments irrespective of the indication, meaning that hospitals receiving the highest payments remained expensive regardless of the underlying condition treated.
To our knowledge, this is only the second study to specifically examine differences in Medicare payments to hospitals for episodes of spine surgical care. A previous analysis by this group documented comparable variations in overall payments.7 Unlike this study, however, it did not account for differences in specific types of surgery, surgical indication, or the use of fusion-based procedures.
Our main findings about the root causes of variation should not be surprising. The extent of variation in surgeon attitudes and beliefs regarding indications for the use of spinal fusion, as well as a lack of consensus around the extent to which patients require rehabilitation or skilled nursing care following spine surgical procedures appear to be the main drivers of differences in payment between the least and most expensive institutions. In many respects, this is reflective of ongoing controversies that persist within the spine surgical community.3,4,5
Our results should be viewed in light of several limitations. First, as with any study based on administrative data, there may be questions regarding incompleteness of risk adjustment across hospitals. Nonetheless, although the problem cannot be completely eliminated, we attempted to mitigate confounding across hospitals by adjusting for com-morbidities, previous expenditures as well as indications. Second, given that this investigation was performed using Medicare data, we realize that the findings may not be generalizable to the population under 65 or those using other types of healthcare insurance. Third, although we characterized variation in payments, such data may not be reflective of the true cost of care from the perspective of the health system. Last, this study was not designed to identify the appropriate or optimal rate of utilization of specific services. In other words, we cannot conclude that high-cost hospitals are overusing fusion-based procedures or that low-cost facilities are underutilizing similar services.
The results of our research have important implications for payers and policymakers. The substantial variation in overall episodic payments for spine surgery imply the potential for savings associated with bundled payment programs, or other risk-based reimbursement models, that have the net effect of reducing variation in payments around similar episodes of care. For example, if payments to hospitals in the most expensive quintile in this study were reduced to the national average per episode of care, a savings of over $162 million could be realized.
These findings also have meaning for hospitals and spine surgeons responding to incentives to optimize the cost-efficiency of spinal care. Realities post-reform indicate that healthcare facilities and practitioners will be well served by evaluating their practices against peers in the community as well as nationally.4,7,8 As the scientific evidence in support of the use of fusion for certain spinal conditions continues to evolve12,13, hospitals and surgeons with particularly high rates of fusion-based procedures may consider external benchmarking and recalibration of practice if appropriate. Similarly, the indications for use of post-acute care following spine surgery are not well established. While this topic remains ripe for further research, healthcare systems and surgeons should look for opportunities to reduce unnecessary use. Such approaches may prove to be important steps in the effort to reduce unwanted surgical variation in the treatment of spinal disorders and could also help to diminish clinical waste.
Footnotes
Disclaimers: Some authors are employees of the U.S. Federal Government and the United States Army. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the United States government. Dr. Andrew Schoenfeld is a Robert Wood Johnson Foundation Clinical Scholar. Dr. John Birkmeyer is supported by a grant from the National Institutes of Aging (1P01AG19783-01). The Robert Wood Johnson Foundation and the Department of Veterans Affairs were not directly involved in study design, data acquisition and interpretation, or manuscript preparation or review. Any opinions expressed herein do not necessarily reflect the opinions of the Robert Wood Johnson Foundation, the U.S. government or the Department of Veterans Affairs. Dr. Birkmeyer is a consultant and has equity interest in ArborMetrix Inc, which provides software and analytics for measuring hospital quality and efficiency. The company had no role in this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Andrew J. Schoenfeld, Email: ajschoen@neomed.edu, Robert Wood Johnson Clinical Scholars Program, University of Michigan, 2800 Plymouth Road, Building 10, RM G016, Ann Arbor, MI 48109.
Mitchel B. Harris, Department of Orthopaedic Surgery, Brigham and Women's Hospital, Harvard Medical School, 75 Francis Street, Boston, MA 02115.
Haiyin Liu, Center for Healthcare Outcome and Policy, University of Michigan, 2800 Plymouth Road, Building 16, Ann Arbor, MI 48109.
John D. Birkmeyer, Center for Healthcare Outcome and Policy, University of Michigan, 2800 Plymouth Road, Building 16, Ann Arbor, MI 48109.
References
- 1.Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299:656–664. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 2.Goz V, Weinreb JH, McCarthy I, et al. Perioperative complications and mortality after spinal fusions. Spine. 2013;38:1970–1976. doi: 10.1097/BRS.0b013e3182a62527. [DOI] [PubMed] [Google Scholar]
- 3.Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen E, Tong KB, Laouri M. Surgical treatment patterns among Medicare beneficiaries newly diagnosed with lumbar spinal stenosis. Spine J. 2010;10:588–594. doi: 10.1016/j.spinee.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 5.Schoenfeld AJ, Weiner BK, Smith HE. Regional variation and spine care: An historical perspective. Spine. 2011;36:1512–1517. doi: 10.1097/BRS.0b013e31822418ae. [DOI] [PubMed] [Google Scholar]
- 6.Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ., Jr Risk factors for immediate postoperative complications and mortality following spine surgery: A study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93:1577–1582. doi: 10.2106/JBJS.J.01048. [DOI] [PubMed] [Google Scholar]
- 7.Birkmeyer JD, Gust C, Baser O, et al. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010;45:1783–1795. doi: 10.1111/j.1475-6773.2010.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller DC, Ye Z, Gust C, Birkmeyer JD. Anticipating the effects of accountable care organizations for inpatient surgery. JAMA Surg. 2013;148:549–554. doi: 10.1001/jamasurg.2013.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller DC, Gust C, Dimick JB, et al. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff. 2011;30:2107–2115. doi: 10.1377/hlthaff.2011.0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don't drive regional Medicare spending variations. Health Aff. 2010;29:537–543. doi: 10.1377/hlthaff.2009.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kornblum MB, Fischgrund JS, Herkowitz HN, Abraham DA, Berkower DL, Ditkoff JS. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine. 2004;29:726–733. doi: 10.1097/01.brs.0000119398.22620.92. [DOI] [PubMed] [Google Scholar]
- 13.Pearson AM, Lurie JD, Tosteson TD, Zhao W, Abdu WA, Weinstein JN. Who should undergo surgery for degenerative spondylolisthesis? Treatment effect predictors in SPORT. Spine. 2013;38:1799–1811. doi: 10.1097/BRS.0b013e3182a314d0. [DOI] [PMC free article] [PubMed] [Google Scholar]


