Highlights
-
•
We explore brain mechanisms of cognitive reappraisal in youth with autism.
-
•
Youth with autism are capable of modulating their emotional response to disgust.
-
•
They exhibit atypical brain activity in amygdala and insula compared to controls.
-
•
We report altered functional connectivity between amygdala and prefrontal cortex.
-
•
These findings have implications for treatment of emotion dysregulation in autism.
Abbreviations: ASD, autism spectrum disorder; TD, typically developing
Keywords: Autism spectrum disorder, Children and adolescents, Emotion regulation, Cognitive reappraisal, Functional magnetic resonance imaging, Amygdala
Abstract
Despite substantial clinical and anecdotal evidence for emotion dysregulation in individuals with autism spectrum disorder (ASD), little is known about the neural substrates underlying this phenomenon. We sought to explore neural mechanisms for cognitive reappraisal in children and adolescents with ASD using functional magnetic resonance imaging (fMRI). We studied 16 youth with ASD and 15 age- and IQ-matched typically developing (TD) comparison youth. Participants were instructed in the use of cognitive reappraisal strategies to increase and decrease their emotional responses to disgusting images. Participants in both groups displayed distinct patterns of brain activity for increasing versus decreasing their emotions. TD participants showed downregulation of bilateral insula and left amygdala on decrease trials, whereas ASD participants showed no modulation of insula and upregulation of left amygdala. Furthermore, TD youth exhibited increased functional connectivity between amygdala and ventrolateral prefrontal cortex compared to ASD participants when downregulating disgust, as well as decreased functional connectivity between amygdala and orbitofrontal cortex. These findings have important implications for our understanding of emotion dysregulation and its treatment in ASD. In particular, the relative lack of prefrontal-amygdala connectivity provides a potential target for treatment-related outcome measurements.
1. Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by a triad of deficits: impairments in reciprocal social interactions, restricted and repetitive patterns of behavior, and delayed or absent communicative skills (APA, 2000). Emotion dysregulation is common in ASD, frequently manifesting as tantrums, meltdowns, or social withdrawal (Laurent and Rubin, 2004). Children with ASD utilize fewer adaptive affect regulation strategies than typically developing (TD) children (Konstantareas and Stewart, 2006), and are more likely to display maladaptive regulation techniques (e.g. avoidance) and less likely to utilize constructive strategies (e.g. cognitive reappraisal; Jahromi et al., 2012). Emotional outbursts in children with ASD exacerbate difficulties in social functioning and are distressing to caregivers (Ozsivadjian et al., 2012). Thus, elucidating mechanisms underlying emotion regulatory processes in ASD is important for furthering our understanding of the disorder and may facilitate development of more targeted treatments for emotion dysregulation (Mazefsky et al., 2012).
One emotion regulation strategy that has received substantial attention in the extant scientific literature is cognitive reappraisal, which occurs after production of an emotional response, and includes reinterpretation of an emotion-laden stimulus to modify one's emotional response (Gross, 1998, Gross and Munoz, 1995, Gross and Thompson, 2007, Ochsner and Gross, 2005). Prior studies have extensively addressed neural mechanisms of cognitive reappraisal in healthy adults, suggesting a role for prefrontal and cingulate networks in implementing regulatory processes that in turn modulate activity in limbic regions implicated in emotional experience, including the amygdala (Beauregard et al., 2001, Blair et al., 2007, Kanske et al., 2011, Kim and Hamann, 2007, Levesque et al., 2003, Mak et al., 2009, Ochsner et al., 2004, Ochsner et al., 2012, Ochsner and Gross, 2007, Phan et al., 2005, Phillips et al., 2008, Urry et al., 2006). In contrast to adults, there are few studies of neural correlates of cognitive reappraisal in TD children and adolescents (Dennis and Hajcak, 2009, Levesque et al., 2004, McRae et al., 2012, Pitskel et al., 2011). Because cognitive behavioral therapy is increasingly used to treat individuals on the ASD spectrum (Danial and Wood, 2013, Sukhodolsky et al., 2013) and cognitive reappraisal skills are a key target of cognitive behavioral therapy approaches (Ball et al., 2013, Goldin et al., 2013, Shurick et al., 2012) we reasoned that a study of the neural correlates of cognitive reappraisal in ASD would be valuable to the field. To our knowledge, no neuroimaging studies to date have employed a cognitive reappraisal paradigm in ASD.
We sought to explore neural mechanisms subserving cognitive reappraisal of disgust in children and adolescents (collectively referred to as youth) with ASD, in comparison to TD youth. We specifically focused on the cognitive reappraisal of disgust for three reasons, two methodological and the other theoretical. First, many of the studies examining cognitive reappraisal have used a range of aversive pictures drawn from the International Affective Picture System (IAPS; Lang et al., 2008). These images can reflect direct threats (human, animal), disgusting images, as well as images reflecting violence and anger. We wanted a thematically homogeneous picture set which would be more likely to engage similar neural circuitry across images. Second, we questioned whether previous work, in attempting to adapt the IAPS images to children, had employed images that were less intense, possibly engaging approach motivation in some children, particularly boys (see McManis et al., 2001). By focusing on disgust we expected we could employ more intense images, which were still acceptable for a child study (i.e., injury or death (adult work) vs. road kill (present study)). Third, disgust images are known to engage insular activity (Chapman and Anderson, 2012) and deficits in functional connectivity of the insula have been specifically implicated in ASD (Ebisch et al., 2011, Uddin and Menon, 2009). In particular, a meta-analytic examination of 24 studies on social information processing and 15 non-social studies (Di Martino et al., 2009) suggested that a distributed system involving the ACC and the anterior insula was hypoactive for individuals with autism. Thus we focused on bilateral insula and amygdala, regions of a priori interest because of their implicated roles in processing negative (particularly disgusting) stimuli (Calder et al., 2000, Ibañez et al., 2010, Lane et al., 1997, Phillips et al., 1997, Schafer et al., 2005, Wicker et al., 2003) and emotion regulation (Eippert et al., 2007, Harenski and Hamann, 2006, Kober et al., 2010, Koenigsberg et al., 2010, McRae et al., 2010, Ochsner et al., 2002, Ohira et al., 2006, Schaefer et al., 2002), respectively.
Broadly speaking a large body of data examines the role of amygdala-prefrontal cortex (PFC) function in emotion regulation among typical populations (Zotev et al., 2013). Particularly important for the present study is a growing body of work suggesting atypical PFC-amygdala function in ASD. For instance, some studies suggest reduced vmPFC-amygdala connectivity in ASD (e.g. Swartz et al., 2013). Another group demonstrated reduced resting state functional connectivity between mPFC and both amygdala and insula (von dem Hagen et al., 2013). Conversely, others show greater vmPFC-amygdala functional connectivity (Monk et al., 2010), as well as differential patterns of functional connectivity of the amygdala with a range of cortical regions including the posterior and dorsal cingulate cortex, superior temporal sulcus, and inferior frontal gyrus (Murphy et al., 2012).
We hypothesized that compared to TD youth, those with ASD would exhibit diminished modulation of amygdala and insula during cognitive reappraisal of disgust, and reduced functional connectivity between these regions and prefrontal cortex (PFC).
2. Materials and methods
2.1. Participants
We studied 22 youth with ASD and 24 TD controls. Participants were recruited via local schools, Internet advertising, flyers placed in public locations (campus buildings, libraries), and from the Yale Center for Translational Developmental Neuroscience participant registry. Additionally, participants from past studies who expressed an interest in being considered for future studies were contacted by phone. Individuals were excluded from participation if, by parent report, they had experienced brain injury, brain disease, brain malformation, seizures, epilepsy, hearing or vision loss, motor impairment, or severe allergies. Other exclusion criteria included intellectual disability or learning disability, and, for the typically developing group, parental concern about possible signs of autism or developmental problems, or the presence of a sibling with autism.
Children with ASD were diagnosed via expert clinical judgment supplemented with the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000) and the Autism Diagnostic Interview–Revised (ADI-R; Lord et al., 1994) (Table 1). Experienced personnel administered the Differential Abilities Scale (DAS; Hale and Willis, 2008), a measure of IQ, to all participants. Parents completed the Social Responsiveness Scale (SRS; Constantino and Todd, 2003) assessing their child's behavior. Prior to group analyses, we excluded participants with excessive motion during the scan (7 TD, 6 ASD), concern for a neuropsychiatric clinical diagnosis (1 TD), and outlying data in contrasts of interest raising serious concern that the task was performed incorrectly (1 TD; the outlier's values fell outside of two standard deviations of the mean in both insula regions (right insula: mean: 0.118, SD: 0.54, outlier value: −1.388; left insula: mean: 0.102, SD: 0.54, outlier value: −1.036). Our final sample consisted of 15 TD participants (9–17 years, mean 13.03 ± 2.20, 9 male) and 16 participants with ASD (9–17 years, mean 13.82 ± 2.41, 12 male). Findings from the TD group have been previously presented (Pitskel et al., 2011). We obtained informed parental consent and written assent from each participant according to a protocol approved by the Yale School of Medicine Human Investigations Committee.
Table 1.
Baseline characteristics.
| Measure | Group |
|||
|---|---|---|---|---|
| TD |
ASD |
|||
| Mean (SEM) | Range | Mean (SEM) | Range | |
| IQ | ||||
| n | 15 | 15 | ||
| Verbal | 106.46 (3.59) | 86–126 | 108.13 (5.89) | 79–161 |
| Nonverbal | 98.33 (3.83) | 76–127 | 102.33 (5.82) | 77–166 |
| Overall | 101.87 (4.03) | 78–131 | 102.40 (6.18) | 76–165 |
| ADI-R | ||||
| n | 12 | |||
| Social | 12.00 (1.15) | 13–27 | ||
| Communication and language | 17.42 (0.96) | 13–23 | ||
| Restricted and repetitive behaviors | 5.17 (0.96) | 0–10 | ||
| ADOS (module 3) | ||||
| n | 14 | |||
| Social and communication* | 9.43 (0.97) | 3–17 | ||
| Stereotyped repetitive behaviors | 2.93 (0.25) | 2–5 | ||
| SRS | ||||
| n | 14 | 14 | ||
| Raw total score** | 27.64 (6.19) | 2–85 | 92.43 (6.79) | 59–126 |
Values expressed as Mean (SEM). IQ data are as measured by the Developmental Abilities Scale (DAS). Abbreviations: Autism Diagnostic Interview-Revised (ADI-R), Autism Diagnostic Observation Schedule (ADOS), Social Responsiveness Scale (SRS). *One ASD participant score did not meet ASD cutoff; diagnosis was confirmed via ADI-R and expert clinical judgment. **ASD > TD, p < .0001.
2.2. Experimental design
Stimuli consisted of two types of pictures, neutral and disgusting, selected from the International Affective Picture System (Lang et al., 2008) and supplemented from an in-house set of images depicting moldy food, people vomiting, roadkill, etc. Details of experimental design and pre-task training can be found in Supplemental Materials and Figure S1. Briefly, participants viewed an instruction indicating one of three tasks (look, increase, or decrease) as well as a strategy prompt to aid in task execution. Participants next viewed a disgusting or neutral image, and then rated their emotional response on a 5-point Likert scale, followed by a “relax” prompt. There were 4 conditions: look-neutral, look-gross, decrease-gross, and increase-gross; participants completed 9 trials of each condition in an event-related design. Prior to the experiment, all participants received individual task training delivered by trained personnel outside the scanner.
2.3. Imaging protocol
Images were collected on a Siemens 3 T Tim Trio scanner located in the Yale University Magnetic Resonance Research Center. High-resolution T1-weighted anatomical images were acquired using an MPRAGE sequence parallel to the AC-PC line (TR = 1230 ms; TE = 1.73 ms; flip angle = 9°; FOV = 256 mm; image matrix 2562; 1 × 1 × 1 mm). Whole-brain functional images were acquired using a single-shot, gradient-recalled echo planar pulse sequence parallel to the AC-PC line (TR = 2000 ms; TE = 25 ms; flip angle = 60°; FOV = 220 mm; image matrix = 642; voxel size = 3.4 × 3.4 × 4.0 mm; 34 slices) sensitive to BOLD contrast. Runs consisted of acquisition of 407 successive brain volumes.
2.4. Data analysis
2.4.1. Behavioral data
To assess differences in emotion regulation task performance between groups, we averaged behavioral ratings grouped by experimental condition in each participant. We then compared these average ratings via repeated-measures ANOVA. We utilized group-wise paired-samples t-tests to compare behavioral responses within groups.
2.4.2. Image preprocessing
Imaging data were preprocessed and analyzed using the BrainVoyager QX 2.0.8 software package (Brain Innovation, Maastricht, The Netherlands). Preprocessing of functional data included slice time correction, 3-dimensional rigid-body motion correction (using trilinear-sinc interpolation), spatial smoothing with a FWHM 4-mm Gaussian kernel, linear-trend removal, and temporal high-pass filtering (fast-Fourier transform based with a cutoff of 3 cycles/time course). Functional data sets were coregistered to high-resolution, within-session, T1-weighted anatomical images which were in turn normalized to Talairach space (Talairach and Tournoux, 1988), to create 4-dimensional data sets. We used an in-house script to identify (and exclude) participants for whom, after removing volume acquisitions where movement between two volumes or integrated movement over 4 volumes exceeded 1 mm, more than 25% of data was removed from any experimental condition (7 TD, 6 ASD).
2.4.3. Whole brain analyses
To investigate whole brain task-related activity in the ASD group, as previously reported for the TD participants (Pitskel et al., 2011), we performed a random-effects general linear model (GLM)-based analysis. GLM task regressors were defined as boxcar functions with values of “1” during each type of image presentation (look-neutral, look-gross, decrease-gross, increase-gross; predictors of interest) and “0” otherwise, as well as three additional boxcar functions with values of “1” during instruction, affect rating, and “relax” periods (predictors of no interest) and “0” otherwise. The instruction regressor encompassed both instruction and strategy presentation. These boxcar functions were convolved with a double-gamma hemodynamic response function (HRF). To further account for motion during each scan, functions of 3 directions and 3 translations of movement from each participant were included in each single-participant GLM-based analysis. All whole-brain analyses were restricted to only voxels located within the Montreal Neurological Institute (MNI) brain normalized to Talairach space. For each whole-brain analysis, we assessed results at an uncorrected statistical threshold of p < .05, corrected for multiple comparisons with a cluster threshold calculated to correspond to α < .05 via the BrainVoyager cluster-threshold estimator plugin performing 1000 iterations of a Monte-Carlo simulation (Forman et al., 1995, Xiong et al., 1995).
To identify brain regions differentially modulated during the experimental paradigm as a function of group membership, we performed three separate 2 × 2 analyses of covariance (ANCOVAs) for each contrast of interest (Condition: look-gross vs. look-neutral OR decrease-gross vs. look-gross OR increase-gross vs. look-gross, Group: ASD vs. TD) with age as a covariate. For each whole-brain analysis, results were assessed at a statistical threshold of p< .05 with a cluster threshold corresponding to α< .05 as calculated via the BrainVoyager cluster-threshold estimator plugin.
2.4.4. Region of interest analyses
We performed more specific region of interest (ROI) analyses in bilateral insula and amygdala. We defined structural ROIs of bilateral amygdala and insula from the Talairach database (Lancaster et al., 1997, Lancaster et al., 2000) and combined these regions into one mask. We then performed two separate 2 × 2 ANCOVAs (Condition: decrease-gross vs. look-gross OR increase-gross vs. look-gross, Group: ASD vs. TD) with age as a covariate, restricted to voxels within this mask at a statistical threshold of p < .05 with a cluster threshold of 4 contiguous functional voxels. We used a more liberal cluster threshold as the ROIs already limited the number of statistical comparisons in the interaction analyses.
2.4.5. Functional connectivity analysis
We performed psychophysiological interaction (PPI) analyses (Friston et al., 1997) in each participant group to assess task-related functional connectivity related to emotion downregulation. We selected right amygdala as the seed region because it showed significant (and largely overlapping) activation to gross (versus neutral) pictures independently in each participant group (p < .01). Preceding connectivity analyses, the global mean was removed from each volume to remove physiological artifacts (Fox et al., 2005). PPI regressors for each participant were created from the new functional data sets by multiplying the preprocessed, normalized seed region time course by the difference of the two task regressors (decrease-gross > look-gross) convolved with the HRF. For each participant, the resulting PPI function along with the region time course and original 7 task regressors and 6 motion parameters were included in a multi-participant random-effects GLM-based analysis. A voxel-wise single-factor ANCOVA was performed to compare groups on parameter estimates for the PPI regressor, using age as a covariate. We compared mean values of the PPI regressor by group in each region to determine the directionality of the group difference.
Given a priori hypotheses based on previous work on emotion regulation demonstrating a relationship between lateral PFC and amygdala activity (Blair et al., 2007, Ochsner et al., 2002, Wager et al., 2008) analyzed voxels were limited to lateral PFC, delineated by bilateral inferior, middle and superior frontal gyri as defined by the Talairach database (Lancaster et al., 1997, Lancaster et al., 2000). Results were assessed at a statistical threshold of p< .05 with a cluster threshold of 20 contiguous functional voxels, corresponding to α< .05 as calculated by the BrainVoyager cluster-threshold estimator plugin.
3. Results
3.1. Behavioral data
TD and ASD groups did not differ in age (t(29) = −1.0, p = .35) or IQ (Verbal: t(28) = −.3, p = .75; Nonverbal: t(28) = −.5, p = .63; Overall: t(28) = −.04, p = .97). As expected, there was a mean difference in SRS scores between groups, with ASD participants scoring significantly higher (greater social impairments) than TD participants (t(26) = −7.1, p < .0001). For affect ratings in response to the emotion regulation task, repeated-measures ANOVA revealed a significant effect of condition (F(1,29) = 135.7, p< .001) but no main effect of group (F(1,29) = .007, p = .936) or group by condition interaction (F(1,29) = .003, p = .960). Average disgust ratings of gross pictures were significantly higher than disgust ratings of neutral pictures (t(15) = 25.5, p < .001), and disgust ratings were significantly lower for gross pictures when participants were asked to decrease (t(15) = −6.3, p < .001), and significantly higher for gross pictures when participants were asked to increase (t(15) = 7.2, p< .001) versus look (Fig. 1).
Fig. 1.
Mean affect ratings as a function of group and condition. Error bars represent standard error of the mean (SEM).
3.2. Imaging data
3.2.1. Whole brain analyses
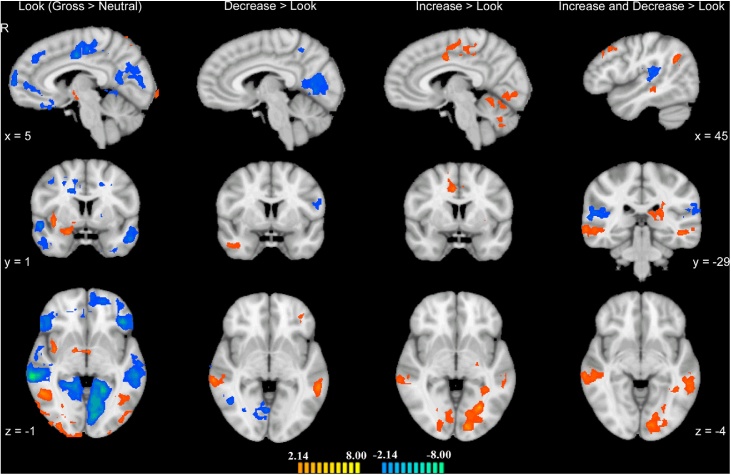
Whole-brain contrasts of interest in the ASD group revealed an extensive network of brain regions activated during emotion processing and regulation (Fig. 2, Table S1). Across both groups, whole-brain ANCOVAs revealed a number of regions demonstrating significant Group × Condition interactions in the three contrasts of interest (look-neutral vs. look-gross, decrease-gross vs. look-gross, and increase-gross vs. look-gross; Table S2).
Fig. 2.
ASD brain activation in each of the three contrasts look-gross > look-neutral, decrease-gross > look-gross, increase-gross > look-gross, as well as the conjunction of the two regulation contrasts. Orange indicates positive-going activation; blue negative-going activation. All activations are at a threshold of p < .05. Images are displayed in radiologic convention. Talairach coordinates displayed to the left apply to the first three columns; those displayed on the right apply to the right-most column. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
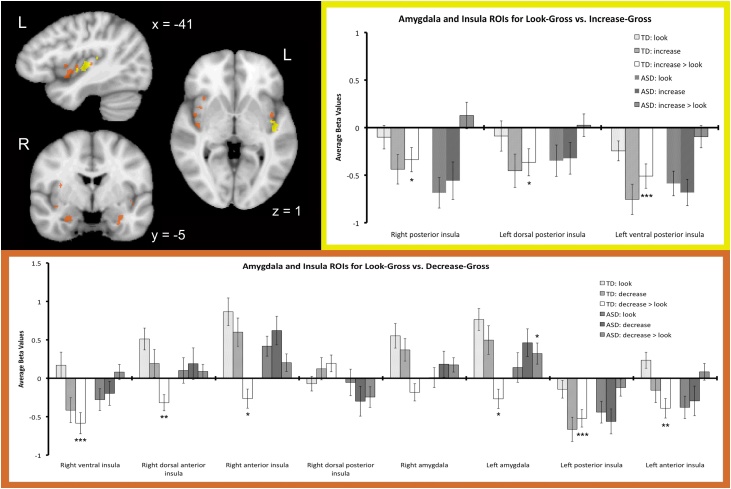
3.2.2. Region of interest analyses
Two Group × Condition ANCOVAs (Condition: decrease-gross vs. look-gross OR increase-gross vs. look-gross, Group: ASD vs. TD) performed across participant groups within structurally defined ROIs in bilateral insula and amygdala revealed subregions of bilateral insula and amygdala showing a significant group by condition interaction to decrease-gross versus look-gross trials. In addition, subregions of bilateral insula showed a significant group by condition interaction to increase-gross versus look-gross trials (Table 2, Fig. 3). Post-hoc one-sample t-tests of average difference beta values are presented in Table S3, separately for the decrease-gross vs. look-gross comparisons and increase-gross vs. look-gross comparisons. For the decrease-gross vs. look-gross comparisons, these analyses revealed that TD participants decreased activity in left amygdala and all but one insula region (right dorsal posterior insula), while ASD participants exhibited no modulation in insula regions and an increase in activity in left amygdala during decrease trials. Post-hoc one-sample t-tests for increase-gross vs. look-gross (Table S3) indicated that TD participants exhibited a significant decrease in bilateral insula activation, whereas ASD participants showed no modulation of these regions. One potential factor contributing to differences in the decrease-gross/increase-gross versus look gross conditions for the ROIs identified in Fig. 3 was the initial reactivity during the look gross condition. This issue was addressed directly with a post-hoc analysis comparing beta difference values across ASD and TD participants for the contrast look-negative versus look-neutral for each ROI (Table S4). Of the 11 sub-regions of insula and amygdala examined, four indicated significantly greater reactivity for the TD group (right ventral insula, left anterior insula, and bilateral amygdala, uncorrected tests). Thus some of the group differences we observed for the regulation condition may reflect effects of initial reactivity.
Table 2.
Brain regions within bilateral insula and amygdala exhibiting a significant group by condition interaction to decrease-gross or increase-gross versus look-gross trials, covarying for age.
| Brain Region | X | Y | Z | Size | F(1,28) | p |
|---|---|---|---|---|---|---|
| Decrease versus look | ||||||
| Right ventral insula | 38 | −11 | −6 | 679 | 14.82 | 0.000628 |
| Right dorsal anterior insula | 38 | 7 | 3 | 161 | 8.35 | 0.007373 |
| Right anterior insula | 32 | 16 | 0 | 131 | 9.00 | 0.00562 |
| Right dorsal posterior insula | 28 | −11 | 12 | 251 | 9.79 | 0.004074 |
| Right amygdala | 23 | −5 | −18 | 166 | 9.38 | 0.004817 |
| Left amygdala | −32 | −5 | −18 | 200 | 12.46 | 0.001458 |
| Left posterior insula | −34 | −23 | 9 | 356 | 9.04 | 0.005518 |
| Left anterior insula | −37 | 4 | 6 | 598 | 12.61 | 0.001379 |
| Increase versus look | ||||||
| Right posterior insula | 32 | −20 | 8 | 149 | 7.00 | 0.013219 |
| Left dorsal posterior insula | −34 | −23 | 15 | 282 | 7.32 | 0.011483 |
| Left ventral posterior insula | −43 | −14 | 3 | 699 | 14.26 | 0.000764 |
Results were obtained at a statistical threshold of p < .05 with a cluster threshold of 4 contiguous functional voxels. Coordinates represent peak voxel and are reported in Talairach space. Cluster size is reported in structural voxels.
Fig. 3.
Top left: Regions of bilateral insula and amygdala exhibiting a significant group by condition interaction when covarying for age, for decrease-gross vs. look-gross (orange) and increase-gross vs. look-gross (yellow). Images are displayed in radiologic convention. Bar graphs: Mean beta values plotted by group alongside mean difference beta values for each region depicted above, for decrease-gross vs. look-gross (bottom, orange) and increase-gross vs. look-gross (top right, yellow). Error bars represent standard error of the mean (SEM). Asterisks denote mean difference beta values significantly different from zero (*p < .05, **p < .01, ***p < .001). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
3.2.3. Functional connectivity analysis
Our PPI analysis assessed task-related connectivity to right amygdala during decrease-gross vs. look-gross trials (Table 3, Fig. 4). Within lateral PFC, two regions of right ventrolateral PFC (vlPFC) showed greater functional connectivity to right amygdala during decrease-gross (compared to look-gross) trials in TD > ASD participants, while bilateral orbitofrontal cortex (OFC) and a region of left superior frontal gyrus (SFG) showed greater functional connectivity to right amygdala during decrease-gross (versus look-gross) trials in ASD > TD participants. Post-hoc analyses elucidating the direction of PPI differences demonstrated that group differences in all regions were driven by a main effect of PPI strength in TD participants only (Table S5).
Table 3.
Brain regions showing greater functional connectivity to right amygdala during decrease-gross compared to look-gross trials (PPI) that differed by group (TD versus ASD), covarying for age.
| Brain Region | X | Y | Z | Size | F(1,28) | p |
|---|---|---|---|---|---|---|
| TD>ASD | ||||||
| Right posterior vlPFC | 44 | 16 | 8 | 540 | 15.51 | 0.000495 |
| Right anterior vlPFC | 29 | 40 | 18 | 1008 | 11.53 | 0.002066 |
| ASD>TD | ||||||
| Right posterior OFC | 22 | 28 | −12 | 635 | 10.18 | 0.003489 |
| Right anterior OFC | 20 | 64 | 9 | 1053 | 15.76 | 0.000456 |
| Left anterior OFC | −40 | 52 | 0 | 1949 | 16.63 | 0.000341 |
| Left posterior OFC | −28 | 28 | −16 | 1111 | 13.54 | 0.000985 |
| Left premotor cortex | −31 | −8 | 60 | 553 | 12.62 | 0.001374 |
Results obtained by PPI analyses assessed at a statistical threshold of p < .05 with a cluster threshold of 20 contiguous functional voxels. Cluster size is reported in structural voxels. Abbreviations: orbitofrontal cortex (OFC); ventrolateral prefrontal cortex (vlPFC).
Fig. 4.
Regions showing greater functional connectivity to right amygdala during decrease-gross > look-gross trials (PPI) that differed by group (TD versus ASD). Amygdala seed regions for each group are displayed in yellow (TD) and green (ASD). Regions depicted in orange showed greater PPI strength in TD compared to ASD children; regions depicted in blue showed greater PPI strength in ASD compared to TD children. Analyses were limited to lateral prefrontal cortex, and activations were assessed at a threshold of p < .05 with a cluster threshold of 20 contiguous functional voxels. Images are displayed in radiologic convention. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
4. Discussion
4.1. Behavioral effects of cognitive reappraisal
Comparison of affect ratings suggests that children and adolescents with and without ASD experienced greater levels of disgust in response to disgusting versus neutral images. Additionally, they reported lower or higher levels of disgust when attempting to decrease or increase their emotional response, respectively. Moreover, groups did not differ on self-report ratings, indicating that youth with ASD reported being equally successful as their TD peers in regulating their emotions. As we provided task-specific training and coached participants on specific emotion regulation strategies, the lack of behavioral deficits in the ASD group is not at odds with reports of emotion dysregulation in more ecologically valid situations, but suggests that youth with ASD are capable of learning and performing an emotion regulation strategy in a controlled setting. The use of CBT with ASD patients is consonant with this idea (Danial and Wood, 2013, Sukhodolsky et al., 2013).
4.2. Brain mechanisms for cognitive reappraisal of disgust
Children and adolescents with ASD activated a broad network of regions when viewing disgusting relative to neutral images, including insula, amygdala, and thalamus, consistent with disgust-specific activation in overlapping regions in TD participants (Pitskel et al., 2011). That both participant groups activated regions implicated in disgust processing (Calder et al., 2000, Ibañez et al., 2010, Lane et al., 1997, Phillips et al., 1997, Schafer et al., 2005, Wicker et al., 2003) serves as an important manipulation check requisite to interpretation of results pertaining to regulation of disgust. Coupled with distinct patterns of neural modulation during upregulation and downregulation of disgust (Fig. 2), these results suggest that ASD participants effectively engaged in the task.
4.3. Modulation of insula and amygdala
ROI analyses revealed decreased activity in several areas of bilateral insula and amygdala during decrease trials in TD participants, consistent with prior studies demonstrating reduced activation of insula (Goldin et al., 2008, Harenski and Hamann, 2006) and amygdala (for review, see Ochsner et al., 2012) during effortful downregulation of emotion in TD adults. Given these regions’ role in affective processing, their modulation may reflect downregulation in emotional experience in line with diminished disgust ratings. As expected, ASD participants displayed no modulation of insula regions despite equivalent behavioral performance. Surprisingly, ASD participants exhibited upregulation of left amygdala activity during decrease trials. Prior studies have shown enhanced amygdala activation during affective rating of aversive images compared to simple recognition (Liberzon et al., 2000). Our findings could theoretically reflect increases in arousal related to task demand. This conjecture is intriguing but cannot be sufficiently addressed by the present study.
Regions of bilateral posterior insula exhibited a group by condition interaction for increase trials, with decreased activity during increase trials in TD participants. These regions overlap with bilateral posterior insula/superior temporal gyrus regions that we reported previously as showing decreased activation during regulation in TD youth, irrespective of direction of regulation (Pitskel et al., 2011). Therefore, we suspect that decreased activation in this region may play a role in the process of emotion regulation more generally.
4.4. Functional connectivity with right amygdala
Our PPI analyses revealed increased functional connectivity between right amygdala and right vlPFC in TD relative to ASD youth during downregulation of disgust. This finding is consistent with prior studies demonstrating decreased amygdala-PFC functional connectivity in ASD (Swartz et al., 2013, van dem Hagen et al., 2013). vlPFC has been consistently implicated in cognitive control of negative emotions in adults (Ochsner et al., 2012), and right vlPFC activity correlates with degree of reappraisal success, as mediated by the amygdala (Wager et al., 2008). Given our functional connectivity findings, coupled with evidence of successful downregulation of amygdala during decrease trials, we hypothesize that prefrontal-amygdala connectivity may be an index of top-down cognitive regulation of negative affect in TD children and adolescents.
Importantly, we observed a positive PPI association between vlPFC and amygdala in our TD group whereas other studies report a negative PPI association (Guyer et al., 2008, Townsend et al., 2013, Winecoff et al., 2011). One explanation for the positive association we observed is that there may be a developmental shift in prefrontal-amygdala function that accounts for differential patterns of connectivity. Recently, Gee et al. (2013) reported positive amygdala-medial prefrontal connectivity for participants younger than 10 years with the opposite pattern of connectivity (negative) present among adolescent and young adult participants. Admittedly, our sample was not as young as Gee et al. and spanned mid-adolescent participants as well. Moreover, few studies to date examine the regulation of disgust. It may be that the positive PPI association we observed is specific to disgust.
The brevity of our functional runs was designed to accommodate a pediatric sample and particularly ASD participants. Ideally, directionality of association in a PPI analysis can be assessed from a single subject analysis where numbers of trials permit examination of patterns of association in single subjects (for an example, see Berkman et al., 2009, Fig. 4). What we can say from our data is that emotion regulation modulates connectivity between amygdala and vlPFC differently in ASD and TD participants, and our data are best viewed from the perspective of a group level analysis. That ASD participants exhibited less vlPFC-amygdala connectivity than their TD peers is one potential explanation for diminished modulation of amygdala activity in ASD.
In contrast, we observed increased functional connectivity between bilateral OFC and left posterior SFG and amygdala during decrease trials in participants with ASD compared to TD participants. Post-hoc analyses revealed that these findings were driven by decreased functional connectivity in TD participants, with no task-based connectivity modulation in ASD participants. As we had no hypotheses regarding negative PPI results, more directed investigation is necessary to confirm and explain this finding.
In sum, participants with ASD reported successful regulation of their emotions, but did not demonstrate typical patterns of neural modulation, suggesting that TD and ASD youth may recruit distinct brain regions to accomplish the same task. Whole-brain analyses (Table S2) revealed that no prefrontal cortical regions demonstrated group × condition interactions for the emotion regulation contrasts (i.e. decrease-gross vs. look-gross and increase-gross vs. look-gross, respectively). Taken together with our PPI findings, it is possible that in the present task, ASD youth recruit prefrontal cortex for top-down processing similarly to TD youth, and group differences in PFC-limbic circuitry are reflected in diminished downstream modulation of limbic regions in ASD. This hypothesis is speculative, and would be a worthy area of further study. Ultimately, underlying group differences in baseline neural reactivity may confer vulnerability to dysregulation in more demanding situations, consistent with clinical reports of emotion dysregulation in ASD (Konstantareas and Stewart, 2006, Laurent and Rubin, 2004, Jahromi et al., 2012, Ozsivadjian et al., 2012, Samson et al., 2012). Our exploratory analysis of initial reactivity (look-gross versus look-neutral) suggested that the ASD group was less reactive initially in some insular and amygdalar regions. Although emotion detection has been a target of clinical treatment in conjunction with CBT for some time, the way in which this is done may need to be uniquely addressed in ASD, with the issue of initial reactivity in mind. For instance, among the clinically anxious, some emphasis is placed on the meaning of arousal as a cue to cope and reappraise rather than a cue to escape. Among individuals with ASD, perhaps an earlier stage needs attention at the level of increasing interoceptive awareness that initiates, or serves a cue to deploy cognitive reappraisal strategies.
4.5. Limitations and future directions
We observed clear modulation of the amygdala and insula for reappraisal of disgust among TD participants, while both the ASD and TD groups provided comparable self-reports of emotion regulation success for disgust. Admittedly, as with all questionnaire data, demand characteristics could have influenced responding. The lack of neural modulation of key emotion circuitry in ASD begs the question of whether or not other factors account for our differential effects. First, we did not directly assess reading ability as a control variable, but rather relied on verbal instructions and a practice phase to ensure that all subjects understood the task. Though TD controls and ASD subjects were comparable on verbal IQ, it remains possible that potential differences in reading ability that were not directly measured could theoretically contribute to group differences in task-related brain activation. Future studies could assess reading achievement to account for this factor. Second, we cannot exclude the possibility that duration of looking or where subjects looked accounted for differences across TD and ASD participants. We are now including eye tracking to examine possible effects of looking time and gaze patterns on emotion regulation effects. Finally, the present study was limited by relatively small sample sizes, and warrants replication with larger samples in the future.
Our investigation focused on regulation of disgust. It is interesting to note that the experience of disgust has been linked to anxiety disorders (Davey et al., 2006, Olatunji et al., 2011, Olatunji and Sawchuk, 2005), including obsessive–compulsive disorder (Berle and Phillips, 2006, Schienle et al., 2005), specific phobias (Davey, 1994, Mulkens et al., 1996, Tolin et al., 1997, Woody and Teachman, 2000), and health anxiety (Davey and Bond, 2005). Furthermore, comorbid anxiety disorders are particularly prevalent in individuals with ASD (Bellini, 2004, Bellini, 2006, Kim et al., 2000, Kuusikko et al., 2008, Tantam, 2000, White et al., 2009). Cognitive reappraisal forms a core component of cognitive-based psychotherapies (Campbell-Sills and Barlow, 2007, Linehan et al., 2007, Taylor and Liberzon, 2007), which are often used to target anxiety disorders and more recently for treatment of anxiety in ASD (Lang et al., 2010, Moree and Davis, 2010, Ooi et al., 2008, Scarpa and Reyes, 2011, White et al., 2010, Wood et al., 2009). Therefore, expanding upon our present findings may further our understanding of deficits in emotion regulation as they pertain to anxiety, with important clinical implications for psychotherapeutic approaches to anxiety in ASD.
4.6. Conclusions
This is the first functional neuroimaging study of cognitive reappraisal in ASD. In this preliminary study we have demonstrated that children and adolescents with ASD are capable of learning and engaging in a cognitive reappraisal task in a controlled setting. In contrast to their TD peers, those with ASD display abnormal patterns of modulation of insula and amygdala, as well as decreased functional connectivity between amygdala and vlPFC during downregulation of disgust. These findings have important implications for our understanding of emotion dysregulation and its treatment in ASD. We have identified potential indices of emotion regulation deficits in ASD, and highlighted activity in brain regions which may be critical to successful emotion regulation in TD youth but which are abnormal in ASD. Future studies could target the regulation of other emotional states that may be problematic for those with ASD, including anxiety and irritability. Studies combining functional neuroimaging with therapeutic interventions could clarify the extent to which the neural mechanisms of emotion regulation predict and/or correlate with clinical outcomes.
Acknowledgements
This work was supported by grants from the National Institute of Mental Health [grant number MH071284 to K.A.P.; K01DA034125 to M.J.C.]; the John Merck Scholars Fund; the Simons Foundation [Individual Grant: Longitudinal Neurogenetics of Atypical Social Brain Development in Autism]; a Harris Professorship to K.A.P, and the Doris Duke Charitable Foundation [to Yale University to support N.B.P.].
Footnotes
Available online 19 August 2014
Supplementary material related to this article can be found, in the online version, at http://dx.doi.org/10.1016/j.dcn.2014.08.007.
Contributor Information
Naomi B. Pitskel, Email: Naomi.Pitskel@yale.edu.
Michael J. Crowley, Email: Michael.Crowley@yale.edu.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- American Psychiatric Association . fourth ed. American Psychiatric Press; Washington, DC: 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Ball T.M., Ramsawh H.J., Campbell-Sills L., Paulus M.P., Stein M.B. Prefrontal dysfunction during emotion regulation in generalized anxiety and panic disorders. Psychol. Med. 2013;43:1475–1486. doi: 10.1017/S0033291712002383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauregard M., Levesque J., Bourgouin P. Neural correlates of conscious self-regulation of emotion. J. Neurosci. 2001;21:RC165. doi: 10.1523/JNEUROSCI.21-18-j0001.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorders. Focus Autism Other Dev. Disabl. 2004;19:78–86. [Google Scholar]
- Bellini S. The development of social anxiety in adolescents with autism spectrum disorders. Focus Autism Other Dev. Disabl. 2006;21:138–145. [Google Scholar]
- Berle D., Phillips E.S. Disgust and obsessive–compulsive disorder: an update. Psychiatry. 2006;69:228–238. doi: 10.1521/psyc.2006.69.3.228. [DOI] [PubMed] [Google Scholar]
- Berkman E.T., Burklund L., Lieberman M.D. Inhibitory spillover: intentional motor inhibition produces incidental limbic inhibition via right inferior frontal cortex. Neuroimage. 2009;47:705–712. doi: 10.1016/j.neuroimage.2009.04.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair K.S., Smith B.W., Mitchell D.G., Morton J., Vythilingam M., Pessoa L., Fridberg D., Zametkin A., Sturman D., Nelson E.E., Drevets W.C., Pine D.S., Martin A., Blair R.J. Modulation of emotion by cognition and cognition by emotion. Neuroimage. 2007;35:430–440. doi: 10.1016/j.neuroimage.2006.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calder A.J., Keane J., Manes F., Antoun N., Young A.W. Impaired recognition and experience of disgust following brain injury. Nat. Neurosci. 2000;3:1077–1078. doi: 10.1038/80586. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L., Barlow D.H. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross J.J., editor. Handbook of Emotion Regulation. Guilford Press; New York: 2007. pp. 542–559. [Google Scholar]
- Chapman H.A., Anderson A.K. Understanding disgust. Ann. N. Y. Acad. Sci. 2012;1251:62–76. doi: 10.1111/j.1749-6632.2011.06369.x. [DOI] [PubMed] [Google Scholar]
- Constantino J.N., Todd R.D. Autistic traits in the general population: a twin study. Arch. Gen. Psychiatry. 2003;60:524–530. doi: 10.1001/archpsyc.60.5.524. [DOI] [PubMed] [Google Scholar]
- Danial J.T., Wood J.J. Cognitive behavioral therapy for children with autism: review and considerations for future research. J. Dev. Behav. Pediatr. 2013;34:702–715. doi: 10.1097/DBP.0b013e31829f676c. [DOI] [PubMed] [Google Scholar]
- Davey G.C.L. Self-reported fears to common indigenous animals in a UK population: the role of disgust sensitivity. Br. J. Psychol. 1994;85:541–554. doi: 10.1111/j.2044-8295.1994.tb02540.x. [DOI] [PubMed] [Google Scholar]
- Davey G.C.L., Bickerstaffe S., MacDonald B.A. Experienced disgust causes a negative interpretation bias: a causal role for disgust in anxious psychopathology. Behav. Res. Ther. 2006;44:1375–1384. doi: 10.1016/j.brat.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Davey G.C.L., Bond N. Using controlled comparisons in disgust psychopathology research: the case of disgust, hypochondriasis and health anxiety. J. Behav. Ther. Exp. Psychiatry. 2005;37:4–15. doi: 10.1016/j.jbtep.2005.09.001. [DOI] [PubMed] [Google Scholar]
- Dennis T.A., Hajcak G. The late positive potential: a neurophysiological marker for emotion regulation in children. J. Child Psychol. Psychiatry. 2009;50:1373–1383. doi: 10.1111/j.1469-7610.2009.02168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Martino A., Ross K., Uddin L.Q., Sklar A.B., Castellanos F.X., Milham M.P. Functional brain correlates of social and nonsocial processes in autism spectrum disorders: an activation likelihood estimation meta-analysis. Biol. Psychiatry. 2009;65:63–74. doi: 10.1016/j.biopsych.2008.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebisch S.J., Gallese V., Willems R.M., Mantini D., Groen W.B., Romani G.L., Buitelaar J.K., Bekkering H. Altered intrinsic functional connectivity of anterior and posterior insula regions in high-functioning participants with autism spectrum disorder. Hum. Brain Mapp. 2011;32:1013–1028. doi: 10.1002/hbm.21085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eippert F., Veit R., Weiskopf N., Erb M., Birbaumer N., Anders S. Regulation of emotional responses elicited by threat-related stimuli. Hum. Brain Mapp. 2007;28:409–423. doi: 10.1002/hbm.20291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman S.D., Cohen J.D., Fitzgerald M., Eddy W.F., Mintun M.A., Noll D.C. Improved assessment of significant activation in functional magnetic resonance imaging (fMRI): use of a cluster-size threshold. Magn. Reson. Med. 1995;33:636–647. doi: 10.1002/mrm.1910330508. [DOI] [PubMed] [Google Scholar]
- Fox M.D., Snyder A.Z., Vincent J.L., Corbetta M., Van Essen D.C., Raichle M.E. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc. Natl. Acad. Sci. U. S. A. 2005;102:9673–9678. doi: 10.1073/pnas.0504136102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friston K.J., Buechel C., Fink G.R., Morris J., Rolls E., Dolan R.J. Psychophysiological and modulatory interactions in neuroimaging. Neuroimage. 1997;6:218–229. doi: 10.1006/nimg.1997.0291. [DOI] [PubMed] [Google Scholar]
- Gee D.G., Humphreys K.L., Flannery J., Goff B., Telzer E.H., Shapiro M., Hare T.A., Bookheimer S.Y., Tottenham N. A developmental shift from positive to negative connectivity in human amygdala-prefrontal circuitry. J. Neurosci. 2013;33:4584–4593. doi: 10.1523/JNEUROSCI.3446-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P.R., McRae K., Ramel W., Gross J.J. The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol. Psychiatry. 2008;63:577–586. doi: 10.1016/j.biopsych.2007.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P.R., Ziv M., Jazaieri H., Hahn K., Heimberg R., Gross J.J. Impact of cognitive behavioral therapy for social anxiety disorder on the neural dynamics of cognitive reappraisal of negative self-beliefs: randomized clinical trial. JAMA Psychiatry. 2013;70:1048–1056. doi: 10.1001/jamapsychiatry.2013.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross J.J. Antecedent- and response-focused emotion regulation: divergent consequences for experiencec expression, and physiology. J. Pers. Soc. Psychol. 1998;74:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross J.J., Munoz R.F. Emotion regulation and mental health. Clin. Psychol.-Sci. Pr. 1995;2:151–164. [Google Scholar]
- Gross J.J., Thompson R.A. Emotion regulation: conceptual foundations. In: Gross J.J., editor. Handbook of Emotion Regulation. Guilford Press; New York: 2007. pp. 3–24. [Google Scholar]
- Guyer A.E., Monk C.S., McClure-Tone E.B., Nelson E.E., Roberson-Nay R., Adler A.D., Fromm S.J., Leibenluft E., Pine D.S., Ernst M. A developmental examination of amygdala response to facial expressions. J. Cogn. Neurosci. 2008;20:1565–1582. doi: 10.1162/jocn.2008.20114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale J.B., Willis J.O. Differential ability scales-second edition. Psychology. 2008;45:838–858. [Google Scholar]
- Harenski C.L., Hamann S. Neural correlates of regulating negative emotions related to moral violations. Neuroimage. 2006;30:313–324. doi: 10.1016/j.neuroimage.2005.09.034. [DOI] [PubMed] [Google Scholar]
- Ibañez A., Gleichgerrcht E., Manes F. Clinical effects of insular damage in humans. Brain Struct. Funct. 2010;214:397–410. doi: 10.1007/s00429-010-0256-y. [DOI] [PubMed] [Google Scholar]
- Jahromi L.B., Meek S.E., Ober-Reynolds S. Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. J. Child. Psychol. Psychiatry. 2012;53:1250–1258. doi: 10.1111/j.1469-7610.2012.02560.x. [DOI] [PubMed] [Google Scholar]
- Kanske P., Heissler J., Schönfelder S., Bongers A., Wessa M. How to regulate emotion? Neural networks for reappraisal and distraction. Cereb. Cortex. 2011;21:1379–1388. doi: 10.1093/cercor/bhq216. [DOI] [PubMed] [Google Scholar]
- Kim J.A., Szatmari P., Bryson S.E., Streiner D.L., Wilson F.J. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism. 2000;4:117–132. [Google Scholar]
- Kim S.H., Hamann S. Neural correlates of positive and negative emotion regulation. J. Cogn. Neurosci. 2007;19:776–798. doi: 10.1162/jocn.2007.19.5.776. [DOI] [PubMed] [Google Scholar]
- Kober H., Mende-Siedlecki P., Kross E.F., Weber J., Mischel W., Hart C.L., Ochsner K.N. Prefrontal-striatal pathway underlies cognitive regulation of craving. Proc. Natl. Acad. Sci. U. S. A. 2010;107:14811–14816. doi: 10.1073/pnas.1007779107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenigsberg H.W., Fan J., Ochsner K.N., Liu X., Guise K., Pizzarello S., Dorantes C., Tecuta L., Guerreri S., Goodman M., New A., Flory J., Siever L.J. Neural correlates of using distancing to regulate emotional responses to social situations. Neuropsychologia. 2010;48:1813–1822. doi: 10.1016/j.neuropsychologia.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstantareas M.M., Stewart K. Affect regulation and temperament in children with autism spectrum disorder. J. Autism Dev. Disord. 2006;36:143–154. doi: 10.1007/s10803-005-0051-4. [DOI] [PubMed] [Google Scholar]
- Kuusikko S., Pollock-Wurman R., Jussila K., Carter A.S., Mattila M.L., Ebeling H., Pauls D.L., Moilanen I. Social anxiety in high-functioning children and adolescents with autism and Asperger syndrome. J. Autism Dev. Disord. 2008;38:1697–1709. doi: 10.1007/s10803-008-0555-9. [DOI] [PubMed] [Google Scholar]
- Lancaster J.L., Rainey L.H., Summerlin J.L., Freitas C.S., Fox P.T., Evans A.C., Toga A.W., Mazziotta J.C. Automated labeling of the human brain: a preliminary report on the development and evaluation of a forward-transform method. Hum. Brain Mapp. 1997;5:238–242. doi: 10.1002/(SICI)1097-0193(1997)5:4<238::AID-HBM6>3.0.CO;2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster J.L., Woldorff M.G., Parsons L.M., Liotti M., Freitas C.S., Rainey L., Kochunov P.V., Nickerson D., Mikiten S.A., Fox P.T. Automated Talairach Atlas labels for functional brain mapping. Hum. Brain Mapp. 2000;10:120–131. doi: 10.1002/1097-0193(200007)10:3<120::AID-HBM30>3.0.CO;2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane R.D., Reiman E.M., Ahern G.L., Schwartz G.E., Davidson R.J. Neuroanatomical correlates of happiness, sadness, and disgust. Am. J. Psychiatry. 1997;154:926–933. doi: 10.1176/ajp.154.7.926. [DOI] [PubMed] [Google Scholar]
- Lang, P.J., Bradley, M.M., Cuthbert, B.N., 2008. International Affective Picture System (IAPS): Affective Ratings of Pictures and Instruction Manual. Technical Report A-8. University of Florida, Gainesville, FL.
- Lang R., Regester A., Lauderdale S., Ashbaugh K., Haring A. Treatment of anxiety in autism spectrum disorders using cognitive behaviour therapy: a systematic review. Dev. Neurorehabil. 2010;13:53–63. doi: 10.3109/17518420903236288. [DOI] [PubMed] [Google Scholar]
- Laurent A.C., Rubin E. Challenges in emotional regulation in Asperger syndrome and high-functioning autism. Top. Lang. Disord. 2004;24:286–297. [Google Scholar]
- Levesque J., Eugene F., Joanette Y., Paquette V., Mensour B., Beaudoin G., Leroux J.M., Bourgouin P., Beauregard M. Neural circuitry underlying voluntary suppression of sadness. Biol. Psychiatry. 2003;53:502–510. doi: 10.1016/s0006-3223(02)01817-6. [DOI] [PubMed] [Google Scholar]
- Levesque J., Joanette Y., Mensour B., Beaudoin G., Leroux J.M., Bourgouin P., Beauregard M. Neural basis of emotional self-regulation in childhood. Neuroscience. 2004;129:361–369. doi: 10.1016/j.neuroscience.2004.07.032. [DOI] [PubMed] [Google Scholar]
- Liberzon I., Taylor S.F., Fig L.M., Decker L.R., Koeppe R.A., Minoshima S. Limbic activation and psychophysiologic responses to aversive visual stimuli. Interaction with cognitive task. Neuropsychopharmacology. 2000;23:508–516. doi: 10.1016/S0893-133X(00)00157-3. [DOI] [PubMed] [Google Scholar]
- Linehan M.M., Bohus M., Lynch T.R. Dialectical behavior therapy for pervasive emotion dysregulation: theoretical and practical underpinnings. In: Gross J.J., editor. Handbook of Emotion Regulation. Guilford Press; New York: 2007. pp. 581–605. [Google Scholar]
- Lord C., Risi S., Lambrecht L., Cook E.H., Jr., Leventhal B.L., DiLavore P.C., Pickles A., Rutter M. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J. Autism Dev. Disord. 2000;30:205–223. [PubMed] [Google Scholar]
- Lord C., Rutter M., Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J. Autism Dev. Disord. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Mak A.K., Hu Z.G., Zhang J.X., Xiao Z., Lee T.M. Sex-related differences in neural activity during emotion regulation. Neuropsychologia. 2009;47:2900–2908. doi: 10.1016/j.neuropsychologia.2009.06.017. [DOI] [PubMed] [Google Scholar]
- Mazefsky C.A., Pelphrey K.A., Dahl R.E. The need for a broader approach to emotion regulation research in autism. Child Dev. Perspect. 2012;6:92–97. doi: 10.1111/j.1750-8606.2011.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManis M.H., Bradley M.M., Berg W.K., Cuthbert B.N., Lang P.J. Emotional reactions in children: verbal, physiological, and behavioral responses to affective pictures. Psychophysiology. 2001;38:222–231. [PubMed] [Google Scholar]
- McRae K., Gross J.J., Weber J., Robertson E.R., Sokol-Hessner P., Ray R.D., Gabrieli J.D., Ochsner K.N. The development of emotion regulation: an fMRI study of cognitive reappraisal in children, adolescents, and young adults. Soc. Cogn. Affect. Neurosci. 2012;7:11–22. doi: 10.1093/scan/nsr093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRae K., Hughes B., Chopra S., Gabrieli J.D., Gross J.J., Ochsner K.N. The neural bases of distraction and reappraisal. J. Cogn. Neurosci. 2010;22:248–262. doi: 10.1162/jocn.2009.21243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk C.S., Weng S.J., Wiggins J.L., Kurapati N., Louro H.M., Carrasco M., Maslowsky J., Risi S., Lord C. Neural circuitry of emotional face processing in autism spectrum disorders. J. Psychiatry Neurosci. 2010;35:105–114. doi: 10.1503/jpn.090085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moree B., Davis T.E., III Cognitive-behavioral therapy for anxiety in children diagnosed with autism spectrum disorders: modification trends. Res. Autism Spectr. Disord. 2010;4:346–354. [Google Scholar]
- Mulkens S.A.N., de Jong P.J., Merckelbach H. Disgust and spider phobia. J. Abnorm. Psychol. 1996;105:464–468. doi: 10.1037//0021-843x.105.3.464. [DOI] [PubMed] [Google Scholar]
- Murphy, E.R., Foss-Feig, J., Kenworthy, L., Gaillard, W.D., Vaidya, C.J., 2012. Atypical functional connectivity of the amygdala in childhood autism spectrum disorders during spontaneous attention to eye-gaze. Autism Res. Treat. 2012, 652408. [DOI] [PMC free article] [PubMed]
- Ochsner K.N., Bunge S.A., Gross J.J., Gabrieli J.D. Rethinking feelings: an fMRI study of the cognitive regulation of emotion. J. Cogn. Neurosci. 2002;14:1215–1229. doi: 10.1162/089892902760807212. [DOI] [PubMed] [Google Scholar]
- Ochsner K.N., Gross J.J. The cognitive control of emotion. Trends Cogn. Sci. 2005;9:242–249. doi: 10.1016/j.tics.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Ochsner K.N., Gross J.J. The neural architecture of emotion regulation. In: Gross J.J., editor. Handbook of Emotion Regulation. Guilford Press; New York: 2007. pp. 87–109. [Google Scholar]
- Ochsner K.N., Ray R.D., Cooper J.C., Robertson E.R., Chopra S., Gabrieli J.D., Gross J.J. For better or for worse: neural systems supporting the cognitive down- and up-regulation of negative emotion. Neuroimage. 2004;23:483–499. doi: 10.1016/j.neuroimage.2004.06.030. [DOI] [PubMed] [Google Scholar]
- Ochsner K.N., Silvers J.A., Buhle J.T. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Ann. N. Y. Acad. Sci. 2012;1251:E1–E24. doi: 10.1111/j.1749-6632.2012.06751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohira H., Nomura M., Ichikawa N., Isowa T., Iidaka T., Sato A., Fukuyama S., Nakajima T., Yamada J. Association of neural and physiological responses during voluntary emotion suppression. Neuroimage. 2006;29:721–733. doi: 10.1016/j.neuroimage.2005.08.047. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Cisler J., McKay D., Phillips M.L. Is disgust associated with psychopathology? Emerging research in the anxiety disorders. Psychiatry Res. 2011;175:1–10. doi: 10.1016/j.psychres.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Sawchuk C.N. Disgust: characteristic features social manifestations, and clinical implications. J. Soc. Clin. Psychol. 2005;24:932–962. [Google Scholar]
- Ooi Y.P., Lam C.M., Sung M., Tan W.T., Goh T.J., Fung D.S., Pathy P., Ang R.P., Chua A. Effects of cognitive-behavioural therapy on anxiety in children with high-functioning autistic spectrum disorders. Singapore Med. J. 2008;49:215–220. [PubMed] [Google Scholar]
- Ozsivadjian A., Knott F., Magiati I. Parent and child perspectives on the nature of anxiety in children and young people with autism spectrum disorders: a focus group study. Autism. 2012;16:107–121. doi: 10.1177/1362361311431703. [DOI] [PubMed] [Google Scholar]
- Phan K.L., Fitzgerald D.A., Nathan P.J., Moore G.J., Uhde T.W., Tancer M.E. Neural substrates for voluntary suppression of negative affect: a functional magnetic resonance imaging study. Biol. Psychiatry. 2005;57:210–219. doi: 10.1016/j.biopsych.2004.10.030. [DOI] [PubMed] [Google Scholar]
- Phillips M.L., Ladouceur C.D., Drevets W.C. A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Mol. Psychiatry. 2008;13:833–857. doi: 10.1038/mp.2008.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M.L., Young A.W., Senior C., Brammer M., Andrew C., Calder A.J., Bullmore E.T., Perrett D.I., Rowland D., Williams S.C., Gray J.A., David A.S. A specific neural substrate for perceiving facial expressions of disgust. Nature. 1997;389:495–498. doi: 10.1038/39051. [DOI] [PubMed] [Google Scholar]
- Pitskel N.B., Bolling D.Z., Kaiser M.D., Crowley M.J., Pelphrey K.A. How grossed out are you? The neural bases of emotion regulation from childhood to adolescence. Dev. Cogn. Neurosci. 2011;1:324–337. doi: 10.1016/j.dcn.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samson A.C., Huber O., Gross J.J. Emotion regulation in Asperger's syndrome and high-functioning autism. Emotion. 2012;12:659–665. doi: 10.1037/a0027975. [DOI] [PubMed] [Google Scholar]
- Scarpa A., Reyes N.M. Improving emotion regulation with CBT in young children with high functioning autism spectrum disorders: a pilot study. Behav. Cogn. Psychother. 2011;39:495–500. doi: 10.1017/S1352465811000063. [DOI] [PubMed] [Google Scholar]
- Schaefer S.M., Jackson D.C., Davidson R.J., Aguirre G.K., Kimberg D.Y., Thompson-Schill S.L. Modulation of amygdalar activity by the conscious regulation of negative emotion. J. Cogn. Neurosci. 2002;14:913–921. doi: 10.1162/089892902760191135. [DOI] [PubMed] [Google Scholar]
- Schafer A., Schienle A., Vaitl D. Stimulus type and design influence hemodynamic responses towards visual disgust and fear elicitors. Int. J. Psychophysiol. 2005;57:53–59. doi: 10.1016/j.ijpsycho.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Schienle A., Schafer A., Stark R., Walter B., Vaitl D. Relationship between disgust sensitivity, trait anxiety and brain activity during disgust induction. Neuropsychobiology. 2005;51:86–92. doi: 10.1159/000084165. [DOI] [PubMed] [Google Scholar]
- Shurick A.A., Hamilton J.R., Harris L.T., Roy A.K., Gross J.J., Phelps E.A. Durable effects of cognitive restructuring on conditioned fear. Emotion. 2012;12:1393–1397. doi: 10.1037/a0029143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukhodolsky D.G., Bloch M.H., Panza K.E., Reichow B. Cognitive-behavioral therapy for anxiety in children with high-functioning autism: a meta-analysis. Pediatrics. 2013;132:e1341–e1350. doi: 10.1542/peds.2013-1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz J.R., Wiggins J.L., Carrasco M., Lord C., Monk C.S. Amygdala habituation and prefrontal functional connectivity in youth with autism spectrum disorders. J. Am. Acad. Child Adolesc. Psychiatry. 2013;52:84–93. doi: 10.1016/j.jaac.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talairach J., Tournoux P. Thieme Medical; New York: 1988. Co-Planar Stereotaxic Atlas of the Human Brain: 3-Dimensional Proportional System: An Approach to Cerebral Imaging. [Google Scholar]
- Tantam D. Psychological disorder in adolescents and adults with Asperger syndrome. Autism. 2000;4:47–62. [Google Scholar]
- Taylor S.F., Liberzon I. Neural correlates of emotion regulation in psychopathology. Trends Cogn. Sci. 2007;11:413–418. doi: 10.1016/j.tics.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Tolin D.F., Lohr J.M., Sawchuk C.N., Lee T.C. Disgust and disgust sensitivity in blood-injection-injury and spider phobia. Behav. Res. Ther. 1997;35:949–953. doi: 10.1016/s0005-7967(97)00048-x. [DOI] [PubMed] [Google Scholar]
- Townsend J.D., Torrisi S.J., Lieberman M.D., Sugar C.A., Bookheimer S.Y., Altshuler L.L. Frontal-amygdala connectivity alterations during emotion downregulation in bipolar I disorder. Biol. Psychiatry. 2013;73:127–135. doi: 10.1016/j.biopsych.2012.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin L.Q., Menon V. The anterior insula in autism: under-connected and under-examined. Neurosci. Biobehav. Rev. 2009;33:1198–1203. doi: 10.1016/j.neubiorev.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urry H.L., van Reekum C.M., Johnstone T., Kalin N.H., Thurow M.E., Schaefer H.S., Jackson C.A., Frye C.J., Greischar L.L., Alexander A.L., Davidson R.J. Amygdala and ventromedial prefrontal cortex are inversely coupled during regulation of negative affect and predict the diurnal pattern of cortisol secretion among older adults. J. Neurosci. 2006;26:4415–4425. doi: 10.1523/JNEUROSCI.3215-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van dem Hagen E.A., Stoyanova R.S., Baron-Cohen S., Calder A.J. Reduced functional connectivity within and between ‘social’ resting state networks in autism spectrum conditions. Soc. Cogn. Affect. Neurosci. 2013;8:694–701. doi: 10.1093/scan/nss053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wager T.D., Davidson M.L., Hughes B.L., Lindquist M.A., Ochsner K.N. Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron. 2008;59:1037–1050. doi: 10.1016/j.neuron.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S.W., Albano A.M., Johnson C.R., Kasari C., Ollendick T., Klin A., Oswald D., Scahill L. Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism. Clin. Child Fam. Psychol. Rev. 2010;13:77–90. doi: 10.1007/s10567-009-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S.W., Oswald D., Ollendick T., Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin. Psychol. Rev. 2009;29:216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wicker B., Keysers C., Plailly J., Royet J.P., Gallese V., Rizzolatti G. Both of us disgusted in my insula: the common neural basis of seeing and feeling disgust. Neuron. 2003;40:655–664. doi: 10.1016/s0896-6273(03)00679-2. [DOI] [PubMed] [Google Scholar]
- Winecoff A., Labar K.S., Madden D.J., Cabeza R., Huettel S.A. Cognitive and neural contributors to emotion regulation in aging. Soc. Cogn. Affect. Neurosci. 2011;6:165–176. doi: 10.1093/scan/nsq030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood J., Drahota A., Sze K., Har K., Chiu A., Langer D. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. J. Child Psychol. Psychiatry. 2009;50:224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woody S.R., Teachman B.A. Intersection of disgust and fear: normative and pathological views. Clin. Psychol.-Sci. Pr. 2000;7:291–311. [Google Scholar]
- Xiong J., Gao J.H., Lancaster J.L., Fox P.T. Clustered pixels analysis for functional MRI activation studies of the human brain. Hum. Brain Mapp. 1995;3:287–301. [Google Scholar]
- Zotev V., Phillips R., Young K.D., Drevets W.C., Bodurka J. Prefrontal control of the amygdala during real-time fMRI neurofeedback training of emotion regulation. PloS One. 2013;8:e79184. doi: 10.1371/journal.pone.0079184. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.