Summary
Background
Schizencephaly is a rare developmental malformation of the central nervous system associated with cell migration disturbances. Schizencephaly can be uni- or bilateral and is divided into two morphological types. The cleft is defined as type I (“closed lips”) if there are fused clefts in cerebral mantle. In type II (“open lips”) the clefts are separated and filled with cerebrospinal fluid connecting lateral ventricle with the subarachnoid space.
Material/Methods
We retrospectively analysed data of patients hospitalized in the Clinical Pediatric Neurology Department of Provincial Hospital No. 2 in Rzeszow between 1998–2011. Clinical data and imaging exams were analysed in the group of children with confirmed schizencephaly.
Results
Schizencephaly was recognized in 32 children. Diagnosis was made in children at the ages between 2 weeks and 15 years – the majority of older children were born before the year 2000. Diagnostic imaging, most often magnetic resonance imaging, was performed in all of the children. In most cases coexistence of other CNS malformations was discovered. In only one patient there were no neurological symptoms, most of the children presented different developmental disorders and neurological symptoms – most often cerebral palsy and epilepsy. In the group of children with bilateral and type II schizencephaly certain symptoms occurred more often.
Conclusions
Schizencephaly is a rare central nervous system developmental disorder, which is very often associated with other severe brain malformations and in most of the cases subsequent multiple neurological symptoms. The method of choice in diagnosis of schizencephaly is magnetic resonance, which shows the degree and type of cleft, coexisting abnormalities and allows differential diagnosis. With the increased availability of this method it is possible to recognize schizencephaly more often and earlier.
MeSH Keywords: Autonomic Nervous System Diseases, Central Nervous System Diseases, Malformations of Cortical Development
Background
Schizencephaly is a developmental malformation of the central nervous system associated with cell migration disturbances. Depending on the level of morphological disturbances we distinguish open and closed schizencephaly which can be uni- or bilateral. Type I (fused/closed lips) runs from deep structures to the surface of the brain without connection to the ventricular system, whereas type II (open/separated lips) connects ventricles with subarachnoid space [1–4].
It is a rare malformation with an estimated incidence of up to 1.5:100,000 live births and 1:650 to 1:1,650 among children suffering from epilepsy [3,4]. There is no known gender predilection [2] and the majority of cases are sporadic [5].
The etiopathogenesis of this defect is not completely understood. It is believed that intrauterine ischemia or expression of genetic factor damaging germinal matrix and impairing cellular migration in 6–7 weeks of intrauterine life may also play a role in the development of schizencephaly [5].
Clefts most often involve frontal or parietal lobes especially in the region of Sylvian fissure and are lined with a layer of grey matter [6].
Schizencephaly often coexists with other brain abnormalities such as ventricular enlargement, polymicrogyria, grey matter heterotopy, dysgenesis/agenesis of the corpus callosum and in up to 50% cases lack of septum pellucidum [7]. Additionally, co-occurrence of this disorder and septo-optic dysplasia (de Morsier syndrome, Hoyt-Kaplan-Grumbach syndrome) was also described. Septo-optic dysplasia is a rare syndrome of congenital malformations comprising optic nerve hypoplasia, hypopituitarism and septum pellicidum agenesis [8].
Schizencephaly can be visualized in ultrasonography (USG) and computer tomography (CT) but the method of choice is magnetic resonance (MR), which has the greatest sensitivity in detection of this condition [9].
The most common clinical manifestations of schizencephaly are motor disorders or epileptic seizures and their severity depends on location and extent of schizencephaly [10].
Aim
The aim of this report was to assess the prevalence of schizencephaly among children hospitalized in the Clinical Pediatric Neurology Department of Provincial Hospital No 2 in Rzeszow between 1998 and 2011, analysis of diagnostic imaging, evaluation of diagnostic algorithm to recognize congenital developmental brain malformation, especially brain tissue clefts and accompanying disorders, as well as recognition of most prevalent neurological symptoms and developmental disorders coexisting with this condition.
Material and Methods
A retrospective analysis of data from 32 patients (11 girls (34%) and 21 boys (66%)) hospitalized in Clinical Pediatric Neurology Department of Provincial Hospital No 2 in Rzeszow from 1998 to 2011 was conducted. Schizencephaly in those patients was confirmed with neuroimaging and full access to their medical documents was obtained.
Out of about 21,000 patients hospitalized in the above-mentioned ward during that time schizencephaly was recognized with MR and/or CT in 32 patients (0.15% of hospitalized children) at the age of 2 weeks to 15 years.
All 32 analyzed children underwent neuroimaging: MR in 30 (94%) children and CT in 9 (28%), out of which 2 (6%) had CT only. Some had cranial ultrasound scan and magnetic resonance angiography (MRA). MR was conducted in T1- and T2-weighed images in axial, coronal and sagittal planes with Elscint Privilege 0.5T scanner since 1998 and with Achieva Philips 1.5T scanner since 2009. Until the year 2004, CTs were performed with Philips TOMOSCAN LX scanner and then with GE Light Speed Ultra 8 slice scanner and a protocol of sequential acquisition with 2,5 mm section thickness parabasally and 5 mm section thickness for the rest of the brain.
Results
Among patients hospitalized in Clinical Pediatric Neurology Department of Provincial Hospital No 2 in Rzeszow from 1998 to 2011, schizencephaly was recognized in neuroimaging of 32 children. In total, 45 clefts were visualized – 26 (58%) open and 19 (42%) closed type (Figures 1 and 2).
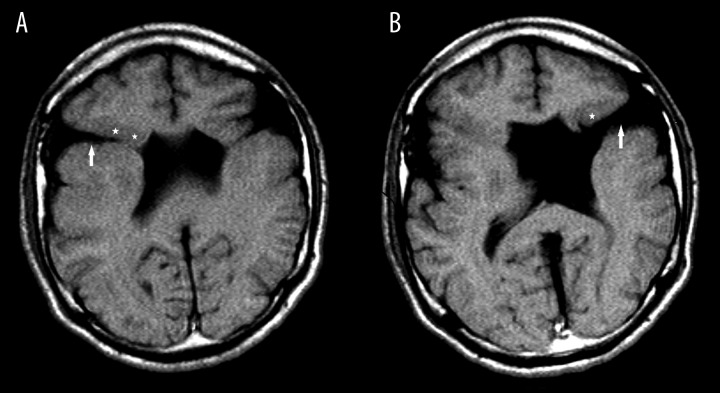
Figure 1.
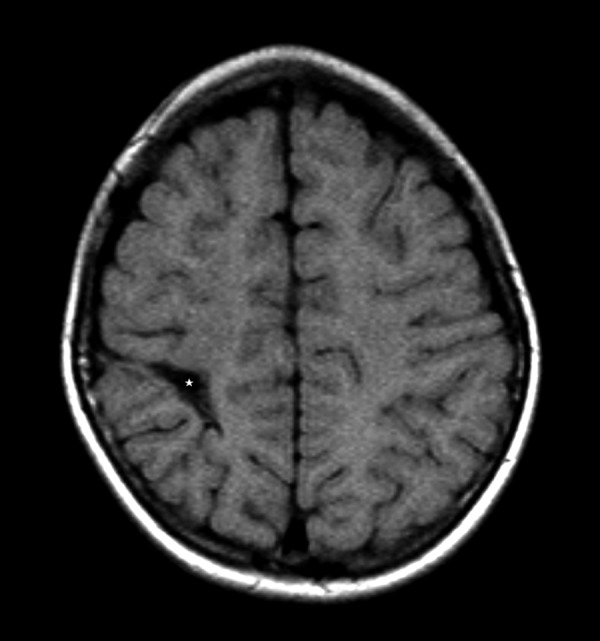
MRI image of unilateral “closed lips” schizencephaly in the right parietal region (star) – axial T1-weighted image.
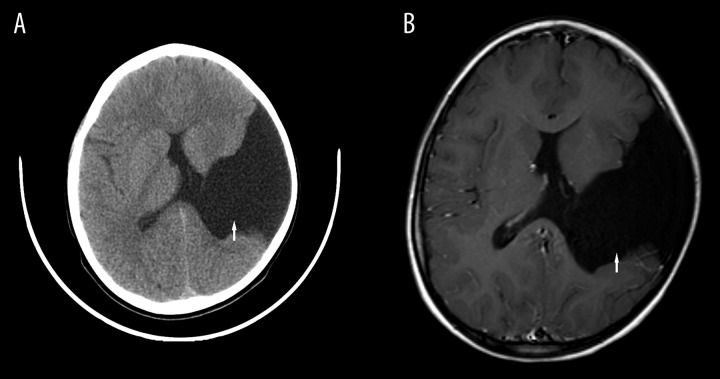
Figure 2.
MRI image of bilateral frontal lobe schizencephaly (arrows) and grey matter heterotopia in the vicinity (stars). (A) Type I right-sided schizencephaly – T1-weighted axial plane image. (B) Type II left-sided schizencephaly – T1-weighted axial plane image.
Unilateral schizencephaly was recognized in 19 children (59%) and bilateral in 13 (41%). Among unilateral cases, the open type was confirmed in 7 children (37%), and closed in 12 (63%) patients. Open bilateral schizencephaly was present in 8 children (62%), closed in 2 children (15%) and mixed type in 3 (23%) (Table 1).
Table 1.
Incidence of uni-/bilateral schizencephalies and I, II, mixed types.
| Type of schizencephaly | Unilateral | Bilateral | |||
|---|---|---|---|---|---|
| No. of patients (%) | 19 (59%) | 13 (41%) | |||
| Type | Open lip | Closed lip | Open lip | Closed lip | Mixed |
| No. of patients (%) | 7 (37%) | 12 (63%) | 8 (62%) | 2 (15%) | 3(23%) |
In the analyzed sample the majority of clefts (42%) were located frontoparietally. Additionally, they were also present in frontal, parietal, parietotemporal and frontoparietotemporal regions, and in one child in the occipital region.
MR and CT scans were conducted in the Clinical Department of Radiology. In 23 children (72%) MR was conducted as the first, and in 9 children (28%) CT scan was the first procedure that visualized schizencephaly. Among those, in 2 (6%) children that was the only examination performed in the Clinical Department of Radiology in Provincial Hospital No 2 in Rzeszow, and in 7 (21%) MRI scan was carried out afterwards – in 3 children (9%) schizencephaly was identified on both scans, in 4 children (12%) CT did not reveal schizencephaly but MR confirmed the diagnosis. In CT schizencephaly was visible in 56% scans. In 44% cases it was impossible to make a correct diagnosis, but it was obtained with the use of MR scans (Table 2).
Table 2.
CT and MR examinations performed in children with schizencephaly and their results (undiagnosed schizencephaly −, diagnosed schizencephaly +).
| Examination performed | % of children with schizencephaly | Results |
|---|---|---|
| CT | 28% (6% only CT scan) | 44% CT − |
| 56% CT + | ||
| MR | 94% (72% only examination) | 100% MR + |
In 4 patients (about 12% children) diagnosing schizencephaly with CT presented difficulties. In two cases it was described as dilated pericerebral fluid spaces, and in one patient as an arachnoid cyst (Figures 3 and 4); in one case vascular malformation was suspected. In subsequent MR scans schizencephaly was recognized and other malformations including vascular were ruled out.
Figure 3.
Schizencephaly in the frontoparietotemporal region (arrow) – in the CT scan, diagnosed as arachnoid cyst; a subsequent MRI scan allowed adequate diagnosis. (A) Axial CT scan. (B) Axial plane T1-weighted image.
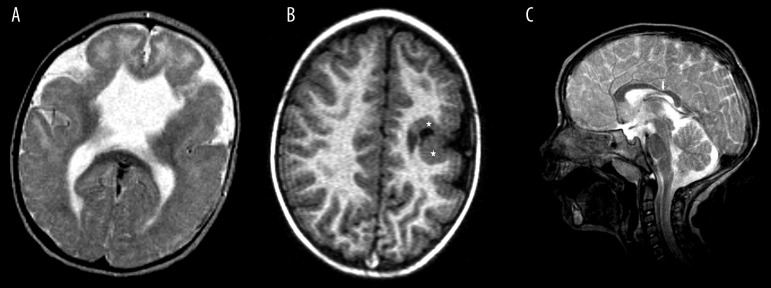
Figure 4.
MRI features of the common abnormalities associated with schizencephaly. (A) Agenesis of septum pellucidum – axial T2-weighted image. (B) Gray matter heterotopy in the vicinity of schizencephalic cleft (stars)– axial plane T1-weighted image. (C) Dysgenesis of the corpus callosum (arrow) – sagittal plane, T2-weighted image.
In the whole sample at the Clinical Department of Radiology in Provincial Hospital No 2 in Rzeszow schizencephaly was recognized in children aged 2 weeks to 15 years. A total number of 22 children (69%) were born after 2000 – average age of schizencephaly diagnosis in that group was 18 months. Schizencephaly was also recognized in 10 children (31%) born before 2000 – in that group average age of diagnosis was 11 years.
In the analyzed sample, in the majority of children (30 patients – 94%) the visualized schizencephaly was concomitant with other malformations including most often ventricular deformation in 24 patients (75%), corpus callosum developmental disorders in 18 patients (56%), septum pellucidum agenesis or dysgenesis in 10 patients (31%), microgyria in 5 patients (15.5%), gray matter heterotopy in 3 children (9%) and pericerebral or pericerebellar fluid space dilation in 16 children (50%). In isolated cases additional syndromes co-occurred: Dandy-Walker syndrome in one child, tuberous sclerosis in one, and Chiari type II malformation in another (Table 3).
Table 3.
Developmental disorders of CNS connected with schizencephaly.
| Developmental disorder | % of patients |
|---|---|
| Ventricular deformation | 75% |
| Impairment of corpus callosum development | 56% |
| Pericerebral or pericerebellar fluid spaces dilation | 50% |
| Septum pellucidum agenesis or dysgenesis | 31% |
| Microgyria | 15.5% |
| Gray matter heterotophy | 9% |
| Dandy-Walker syndrome | 3% |
| Chiari type II malformation | 3% |
| Tuberous sclerosis | 3% |
One child suffered from a syndrome of congenital cerebral defects with accompanying cleft lip and palate. In one case a sibling was diagnosed with neurodegenerative disease.
Schizencephalic patients presented various neurological disorders during hospitalization (Table 4), most often – in 22 children (69%) psychomotor retardation, epilepsy in 16 patients (50%), cerebral palsy in 15 children (47%), hemiplegia in 8 children (25%), tetraplegia in 10 (31%), mostly spastic. Hydrocephalus occurred in 7 children (22%) and microcephaly in 2 patients (6%). Only one child (unilateral closed cleft within the right occipital lobe) repeatedly hospitalized due to genitourinary malformation (hydronephrosis) showed no neurological symptoms and CT followed by MRI were performed for emotional disorders of the child.
Table 4.
The most frequent neurological symptoms in the group of children with schizencephaly.
| Neurological symptom | No. of patients (%) |
|---|---|
| Psychomotor retardation | 31 (97%) |
| Epilepsy | 16 (50%) |
| Cerebral palsy | 15 (47%) |
| Tetraplegia | 10 (31%) |
| Hemiplegia | 8 (25%) |
| Hydrocephalus | 7 (22%) |
| Microcephaly | 2 (6%) |
Comorbid neurological symptoms and CNS malformations occurred in every child with bilateral and open schizencephaly. They were less frequent in the group with unilateral schizencephaly (about 95% children). Hydrocephalus was more common in bilateral schizencephaly (23%) and in the group with open clefts (28%). Epilepsy was present in 16 children (50%), slightly more frequent in the group with bilateral schizencephaly (about 54%), including 1 child suffering from flexion spasms in the course of West syndrome which has a poor prognosis. Epilepsy was slightly more frequent in closed schizencephaly (53%) as compared to open-type schizencephaly (44%).
Discussion
Schizencephaly is a rare developmental malformation. In published epidemiological studies from 2005 conducted in Canada and United States its incidence was estimated at 1.54/100,000 births/year in the period of 1985–2001, per accumulated 4 million births [11]. In the analyzed years (1998–2011) in Provincial Hospital No 2, average diagnosis rate was 2–3 new schizencephaly cases a year.
In the previously published analyses this malformation occurred with similar frequency in both sexes [4]. In the study group it was more common in boys, who comprised 66% of all children. There was no documented family history of schizencephaly in the studied group of children, such schizencephaly is very rare [6].
In the study group the majority of clefts (about 80%) were located frontoparietally which is consistent with previous data [10]. In one child there was an isolated cleft within the occipital region, which is a very rare location [4]. It is estimated that bilateral schizencephaly is the rarer type; among unilateral clefts both types occur with similar frequency and in bilateral cases the open type is more common. Most often two clefts coexist but there was at least one case of co-occurrence of three clefts described [4,6,10]. Similarly to what is described in literature, in the analyzed sample the malformation was more likely to be unilateral and among cases of bilateral schizencephaly the open type was more common (Table 1).
Before MR became widely available, the basic method of neuroimaging was CT scan [4]. Currently, MR is regarded a method of choice in diagnosing CNS malformations. It allows to assess the extent, type of schizencephaly and reveals concomitant disorders [4,11]. MRI visualizes also the gray matter which lines the cleft and permits to differentiate it from porencephalic cyst and other acquired lesions as well as enables detection of concomitant disorders [12].
In a few children CT scan was performed as the first procedure – in that group schizencephaly remained unrecognized in about 44% of children. In two patients dilated pericerebral fluid spaces were described, an arachnoid cyst in one and vascular malformation in another one. In subsequent MR scans schizencephaly was recognized and other diagnoses including vascular malformations were excluded. In the majority of children MR was the first examination and schizencephaly was recognized in all patients which, if there are no contraindications, confirms the validity of this procedure as a method of choice in all children with suspected CNS malformations.
No data concerning the age of schizencephaly recognition was found. In the analyzed group there was a perceptible interrelation, i.e. among children born before 2000 schizencephaly was recognized at a later age (11 years on average) which may result from limited availability of advanced neuroimaging methods at that time (until 1998 the Department only had a CT scanner). Among children born after 2000 the age at which the first diagnostic procedure was conducted ranged from 2 weeks to 6 years. The more severe the comorbidity, the earlier the first diagnostic test was made. Average age was 18 months, which may be explained by the fact, that at that age abnormal development arouses great distress in caretakers and therefore the diagnostic process begins.
Both types of schizencephaly very often coexist with other CNS abnormalities [10]. The most common one is partial or complete agenesis of the septum pellucidum (up to 70%), agenesis of the corpus callosum, cortical dysgenesis and polymicrogyria [10]. A similar coincidence was found in the described group of children. Coexistence of these disorders may suggest a probable onset of these malformations in utero – at approximately 2nd month of intrauterine life when cellular migration during CNS formation takes place [5]. In the study group, there were also some cases with Dandy-Walker syndrome, Chiari type II malformation and tuberous sclerosis, which may prove schizencephaly to be a part of greater CNS malformations [5, 10, 13]. In the study group no septo-optic dysplasia was recognized although its prevalence in schizencephalic patients is estimated at 6–25% [5,8,10].
The clinical picture of schizencephaly is very heterogeneous. The main registered abnormalities comprise motor disorders, developmental delay and epileptic seizures. Most authors agree that clinical symptoms depend on the size and location of schizencephaly [10,13]. The conducted analysis revealed that neurological symptoms were absent in merely one child suffering from schizencephaly where the diagnosis of the pathology was incidental. The rest of the patients presented neurological disorders in the form of paresis and psychomotor retardation. Epilepsy, as described by previous authors, was recognized in half of the children [5,10,13]. In the published papers in most cases it had a mild course and did not impair the development of the child [10]. In the study group it was difficult to find such a tendency because every child with epilepsy suffered also from psychomotor retardation which was already present at the stage of diagnostics. Due to the fact that treatment of the majority of the patients is continued on an ad hoc basis and in outpatient clinics we did not have access to data concerning further course of illness. Among the analyzed children epilepsy was slightly more prevalent in bilateral schizencephaly cases. Flexion spasms in the course of West syndrome with poor prognosis were recognized in one child with bilateral schizencephaly. Hydrocephalus occurred in 22% of children with both types of schizencephaly but slightly more often in the group with bilateral open-type schizencephaly which is associated with a higher level of severity [5,10].
Conclusions
In the study group unilateral closed schizencephaly was prevalent. Most often it was located frontoparietally.
Schizencephaly is sometimes difficult to recognize therefore MR should be the method of choice in that respect.
Schizencephaly often coexists with other abnormalities. Finding such symptoms should be followed by a detailed analysis of examination in order to exclude schizencephaly.
Neurological disorders are present in the majority of schizencephalic patients and the symptoms are more severe in bilateral and open clefts.
References
- 1.Sikorska J, Kluczewska E. Zaburzenia rozwojowe ośrodkowego układu nerwowego. In: Walecki J, editor. Postępy neuroradiologii. Polska Fundacja Upowszechniania Nauki; Warszawa: 2007. p. 214. [in Polish] [Google Scholar]
- 2.Lempert TE, Gaensler EH. Neuroradiologia pediatryczna. In: Brant WE, Helms CA, editors. Podstawy diagnostyki radiologicznej. Medipage; Warszawa: 2007. pp. 255–56. [in Polish] [Google Scholar]
- 3.Hunter AG. Brain. In: Stevenson RE, Hall JG, editors. Human malformations and related anomalies. Oxford University Press; 2006. pp. 648–51. [Google Scholar]
- 4.Granata T, Battaglia G. Schizencephaly. In: Sarnat HB, Curatolo P, editors. Malformations of the nervous system. Handbook of Clinical Neurology. Elsevier B.V.; Amsterdam: 2008. pp. 235–46. [DOI] [PubMed] [Google Scholar]
- 5.Denis D, Chateil JF, Brun M, et al. Schizencephaly: clinical and imaging features in 30 infantile cases. Brain Dev. 2000;22(8):475–83. doi: 10.1016/s0387-7604(00)00173-x. [DOI] [PubMed] [Google Scholar]
- 6.Barkovich JA.Congenital malformations of the brain and skull Barkovich JA.), Pediatric Neuroimaging 4th editionLippincott Williams and Wilkins; Philadelphia: 2005291–386. [Google Scholar]
- 7.Nyberg DA, McGahan JP. Diagnostic Imaging of Fetal Anomalies. Lippincott Williams and Wilkins; Philadelphia: 2003. pp. 221–90. [Google Scholar]
- 8.Gasparetto EL, Warszawiak D, de Carvalho Neto AD, et al. Septo-optic dysplasia plus: case report. Arq Neuropsiquiatr. 2003;61(3A):671–76. doi: 10.1590/s0004-282x2003000400028. [DOI] [PubMed] [Google Scholar]
- 9.Vishal K, Saggar K. Schizencephaly. JK Science: Journal of Medical Education & Research. 2009;11(2):108. [Google Scholar]
- 10.Hayashi N, Tsutsumi Y, Barkovich AJ. Morphological features and associated anomalies of schizencephaly in the clinical population. Neuroradiology. 2002;44(5):418–27. doi: 10.1007/s00234-001-0719-1. [DOI] [PubMed] [Google Scholar]
- 11.Curry CJ, Lammer EJ, Nelson V, et al. Schizencephaly: heterogenous etiologies in a population of 4 milion California births. Am J Med Genet A. 2005;137A(2):181–89. doi: 10.1002/ajmg.a.30862. [DOI] [PubMed] [Google Scholar]
- 12.Van Runge M. Rezonans magentyczny w praktyce klinicznej. Elsevier Urban & Partner; Wrocław: 2007. pp. 108–9. [in Polish] [Google Scholar]
- 13.Granata T, Freri E, Caccia C, et al. Schizencephaly: clinical spectrum, epilepsy, and pathogenesis. J Child Neurol. 2005;20:313–18. doi: 10.1177/08830738050200040801. [DOI] [PubMed] [Google Scholar]