Abstract
Approximately five percent of the Finnish population are Swedish-speaking and have higher socioeconomic position and longer life expectancy than the Finnish-speaking majority. Previous studies have not investigated whether Swedish-speaking Finns have lower risk of schizophrenia spectrum disorders (SSD) than Finnish-speaking Finns. We investigated this in a representative sample of 47 445 Finns born in 1972–1984. Hazard ratios of SSD between language groups were assessed with conditional proportional hazards regression. Sex, parental ages at birth, paternal employment around conception, parental psychosis and place and residence in the capital area were used as other explanatory variables. The prevalence of SSD was 0.7% in the Swedish-speaking minority and 1.5% in the Finnish-speaking majority. In the adjusted regression model, belonging to the Swedish-speaking minority was associated with lower risk of SSD (hazard ratio (HR) 0.41, 95% confidence interval (CI) 0.24–0.69). In a subset analysis by gender, the protective effect was evident among Swedish-speaking males (HR 0.32, 95% CI 0.15–0.68) but marginal in females (HR 0.75, 95% CI 0.41–1.37). Parental psychosis and place of birth in the capital area were associated with higher risk of SSD, whereas paternal employment at the time of conception was associated with lower risk of SSD. Our results support the role of social factors in the etiology of schizophrenia. Belonging to a minority with high socioeconomic status and social capital may be protective against schizophrenia, especially for males.
Keywords: schizophrenia spectrum disorders, minority status, social risk factors, urban birth
1. Introduction
The epidemiology of schizophrenia in Finland has a number of unique features. The lifetime prevalence of DSM-IV schizophrenia in Finland is one percent (Perälä et al., 2007), a higher rate than is reported in most other countries (Saha et al., 2005). A threefold difference in the prevalence of schizophrenia has been reported between Eastern and Northern Finland and Southwestern Finland (Perälä et al., 2008). Urban-rural differences have been negligible (Perälä et al., 2008), although a study analyzing birth cohorts from 1950 to 1969 found suggestive evidence that urban birth was starting to emerge as a risk factor in cohorts born in the 1960s (Haukka et al., 2001).
From the 13th century until 1809, Finland was a part of Sweden, and approximately five percent (5%) of the Finnish population are still Swedish-speaking, living principally in the Western and Southern coastal areas. Both Finnish and Swedish are official languages in Finland, and Swedish-speaking Finns are Finnish citizens born in Finland. Swedish-speaking Finns have higher socioeconomic position, education, income and wealth, are less often divorced or unemployed and have longer life expectancy than Finnish-speaking Finns (Sipilä and Martikainen, 2009). The difference in mortality risk between Swedish- and Finnish-speaking Finns is highest in alcohol-related causes, suicides, and accidents and violence, but less than half of this is attributable to socioeconomic and demographic factors (Sipilä and Martikainen, 2009). Reported differences in health may be partly explained by higher social participation and social capital in Swedish-speaking communities (Hyyppä and Mäki, 2003; Sipilä and Martikainen, 2009), but there are also differences in population genetics. While there is a substantial Scandinavian gene flow into the southwestern parts of Finland, this has not occurred in eastern Finland (Palo et al., 2009). Specifically, Swedish-speaking Finns living in the Western coastal areas are genetically close to Swedes (Salmela et al., 2011). However, in terms of both socioeconomic factors and health, the differences between Swedish-speaking and Finnish-speaking men are greater than the differences between Swedish-speaking and Finnish-speaking women (Saarela and Finnäs, 2004; Saarela, 2006; Sipilä and Martikainen, 2010). This gender difference is unlikely to be related to genetic factors.
Previous studies have not investigated whether the prevalence of schizophrenia differs between Finnish- and Swedish-speaking Finns, although in Sweden, Finnish first- and second-generation immigrants have over two-fold increased incidence of schizophrenia compared to the Swedish majority population (Leão et al., 2006). Therefore, we set out to investigate in a general population sample whether the Swedish-speaking Finns have lower risk of schizophrenia spectrum disorders (SSD) than the Finnish-speaking Finns.
2. Materials and methods
2.1. Study population
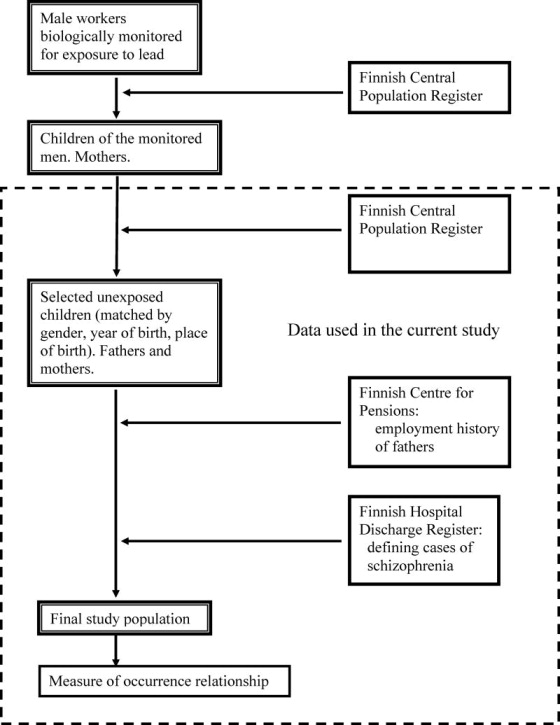
The study population consisted of a large population-based comparison group for offspring of a cohort of male workers biologically monitored for occupational exposure to lead from 1973 through 1983 (Figure 1). The cohort of biologically monitored men has been previously established by the Finnish Institute of Occupational Health (FIOH) (Anttila et al., 1995). We linked this cohort with The Population Information System (PIS) maintained by the Population Register Centre to identify the children of the monitored men and the mothers of the children. After excluding children with unknown birthplace, those born abroad and those whose mothers spoke a language other than Finnish or Swedish, altogether 11,863 children of monitored men, born in 1972–1984, remained. We then identified population comparison offspring and their parents from the same registry. For each offspring of the monitored men, we selected four population comparison offspring, matching for gender, the date of birth, and two were also matched for place of birth. Four comparison children were found for each exposed child in all except seven instances resulting in 47,455 offspring. In order to study whether Swedish-speaking minority status is associated with the risk of schizophrenia and other psychotic disorders we restricted the study to these population comparison offspring. Thus, children who were not offspring of the monitored men were eligible for the present study. With every other aspect, our study population can be considered as a random sample of Finns born in 1972–84. In particular, the proportion of males (50.8% in the study and 51.2% of newborns in Finland) and the proportion of Swedish-speaking (5.2% in the study and 5.3% in Finland) correspond well with the official population statistics during 1972–79 (Official Statistics of Finland). From PIS, we also collected information for the offspring and the parents on date of birth, possible dates of emigration or death, place of birth, place of residence, and first language. First language is defined by the parents and formally registered during the two months following birth.
Figure 1.
Identification of the study population and register data sources used in the study
2.2. Case ascertainment from The Finnish Hospital Discharge Register
We linked the data on 47 455 offspring and their parents with The Finnish Hospital Discharge Register (FHDR) to identify people who had been hospitalized for a schizophrenia spectrum disorder (SSD, consisting of non-affective psychosis or schizotypal personality disorder; ICD-10 F20-29, ICD-8 and ICD-9 295, 297–299). During 1979 to 2010, we identified 710 cases in the offspring, 1 012 in the fathers, and 1 302 cases in the mothers. Date of onset of SSD was defined as the first hospitalization date for psychotic or schizotypal personality disorder.
FHDR covers all public and private hospitals in Finland. For each inpatient stay, data on beginning and ending dates, primary and up to three subsidiary diagnoses, and hospital identification code are listed. The registry was computerized in 1968, since when information is available. Diagnostic criteria have changed over time. ICD-8 was in use 1969 to 1986. Between 1987 and 1995, psychiatric disorders were diagnosed according to the DSM-III-R criteria but using the ICD-9 codes, and the ICD-10 codes and criteria have been in use since 1996. In Finland, almost half of the patients who are eventually diagnosed with schizophrenia first receive a diagnosis of another psychotic disorder, typically acute and transient psychosis or psychotic disorder not otherwise specified, at the first admission (Kiviniemi et al., 2010). Because of this, we used the broad classification of SSD, including all nonaffective psychotic disorders and schizotypal personality disorder (ICD-8 and ICD-9 295, 297–299, ICD-10 F20-29).
2.3. Variables considered in the analyses
Maternal and paternal ages around the time of assumed conception were categorized into four groups. They were statistically adjusted to account for the established association between advanced paternal age and schizophrenia (Goriely et al., 2013), and the possible association between young maternal age and schizophrenia (McGrath et al., 2014).
Place of birth and residence were categorized into the Helsinki capital area and rest of Finland. This categorization was chosen for two reasons: first, it is the only city area in Finland that corresponds in size to the main city areas in other Nordic countries that have been associated with the highest schizophrenia risk in previous Nordic studies (Mortensen et al., 1999, Harrison et al., 2003). Secondly, the Swedish-speaking population in the capital area forms a minority that is less homogeneous than the one living in the Western coastal area where the Swedish-speaking population constitutes a majority within several municipalities.
We lack information on occupation or socio-economic status of the parents. However, because unemployment is less common in the Swedish-speaking Finns than in the Finnish-speaking Finns (Sipilä and Martikainen, 2009) we considered the possible confounding role of paternal employment in the studied language-SSD association (Wicks et al., 2010). Employment status (employed vs. other, including unemployed, student or pensioned) of the father at the time of conception was defined comparing date of birth and the dates of employment obtained from the Finnish Centre for Pensions.
Parental history of psychosis was defined as hospitalization for SSD or affective psychosis (bipolar I disorder or major depressive disorder with psychotic features, corresponding to ICD-10 codes F30, F31, F32.3, F33.3; Finnish ICD-9 codes 2961E, 2962, 2963, 2964, 2967A, or Finnish ICD-8 codes 296.00, 296.10, 296.20, 296.30, 296.88, 296.99) based on FHDR information.
2.4. Ethical permissions
The Ethics Committee of the Finnish Institute of Occupational Health approved the study (ETR 01/2008 and ETR 3/2013). Permissions to use the data from registers of the National Institute for Health and Welfare, the Finnish Centre for Pensions and the Population Register Centre were obtained from the respective organizations.
2.5. Statistical analyses
Our data of 47 445 offspring and parents consist of 11 863 matched sets of participants. We therefore analyzed the data on SSD using conditional proportional hazards regression stratifying by matched set (Rothman et al., 2008, Greenland, 2008). The outcome parameter is a hazard ratio with 95% confidence intervals. We followed the study population from date of birth until emigration, death, first hospitalization for SSD or 2010, whichever came first. All analyses were carried out using the Statistical Analysis System 9.2 program (SAS Institute Cary, USA).
To gain more insight into the role of language, gender, and urban place of birth in the onset of SSD, we also conducted analyses in subsets according to the gender of the offspring and place of birth (Helsinki Capital area versus rest of Finland). When analyzing place of birth, we stratified by gender and year of birth only.
3. Results
The characteristics of the study population are presented in Table 1. About five percent of all offspring were Swedish speaking, but the proportion of Swedish speaking SSD cases was only 2.5%. Schizophrenia spectrum disorder was more common in the offspring born or living in the Helsinki Capital area than in other parts of Finland. A parental history of psychosis was associated with an increased risk of SSD in the offspring.
Table 1.
Descriptive characteristics of the sample
| Characteristic | Total sample, N (%) | Schizophrenia spectrum disorder in the offspring |
|---|---|---|
|
| ||
| Offspring: | ||
|
| ||
| Gender | ||
| Male | 24,121 (50.8) | 426 (60.0) |
| Female | 23,324 (49.2) | 284 (40.0) |
|
| ||
| Language | ||
| Finnish | 45,026 (94.9) | 692 (97.5) |
| Swedish | 2,419 (5.1) | 18 (2.5) |
|
| ||
| Place of birth | ||
| Helsinki Capital area | 8,157 (17.2) | 178 (25.1) |
| Other parts of Finland | 39,288 (82.8) | 532 (74.9) |
|
| ||
| Place of residence | ||
| Helsinki Capital area | 11,092 (23.4) | 199 (28.0) |
| Other parts of Finland | 36,353 (76.6) | 511 (72.0) |
|
| ||
| Parents: | ||
|
| ||
| Age of the mother | ||
| 13–19 | 4,396 (9.4) | 74 (10.4) |
| 20–29 | 31,460 (66.2) | 462 (68.8) |
| 30–39 | 10,401 (22.3) | 162 (22.8) |
| 40–48 | 476 (1.0) | 13 (1.8) |
|
| ||
| Age of the father | ||
| 13–19 | 1,115 (2.5) | 19 (2.7) |
| 20–29 | 28,410 (60.8) | 400 (56.3) |
| 30–39 | 14,204 (30.4) | 231 (32.5) |
| 40–74 | 2,015 (4.3) | 41 (5.8) |
| missing | 951 (2.0) | 19 (2.7) |
|
| ||
| Parental psychosis | ||
| Yes | 2,276 (4.4) | 118 (16.6) |
| No | 45,169 (95.2) | 592 (83.4) |
|
| ||
| Father employed around the time of conception | ||
| Yes | 42,612 (87.7) | 592 (83.4) |
| No | 5833 (12.3) | 118 (16.6) |
The unadjusted and adjusted hazard ratios on the risk of schizophrenia spectrum disorder according to the language of the offspring are presented in Table 2. Swedish speaking children were less likely to develop SSD (0.7%) than Finnish speaking children (1.5%): adjusted hazard ratio (aHR) was 0.41; 95% CI (CI): 0.24–0.69. Parental psychoses were strongly related to SSD in the offspring. Father’s employment, defined for the time of conception, was related to decreased risk of SSD in the offspring. Offspring born in Helsinki Capital area had an increased risk of SSD compared to offspring born in other parts of Finland.
Table 2.
Risk of schizophrenia spectrum disorder according to the language of the offspring. Five univariable models for covariates and a multivariable model adjusted for all the covariates in the table.
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| N | Schizophrenia spectrum disorder N (%) | HR | 95% CI | HR | 95% CI | |
|
| ||||||
| Characteristics of the offspring: | ||||||
|
| ||||||
| Language | ||||||
| Finnish | 45,026 | 692 (1.5) | 1.0 | ref. | 1.0 | ref. |
| Swedish | 2,419 | 18 (0.7) | 0.44 | 0.26 – 0.73 | 0.41 | 0.24 – 0.69 |
|
| ||||||
| Place of birth | ||||||
| Helsinki Capital area | 8,157 | 178 (2.2) | 1.55 | 1.23 – 1.95 | 1.45 | 1.14 – 1.85 |
| Other parts of Finland | 39,288 | 532 (1.4) | 1.0 | ref. | 1.0 | ref. |
|
| ||||||
| Characteristics of the parents: | ||||||
|
| ||||||
| Parental psychosis | ||||||
| Yes | 2,276 | 118 (5.2) | 3.94 | 2.95 – 5.26 | 3.81 | 2.84 – 5.10 |
| No | 45,169 | 592 (1.3) | 1.0 | ref. | 1.0 | ref. |
|
| ||||||
| Age of the mother | ||||||
| 13–19 | 4,470 | 74 (1.7) | 1.16 | 0.84 – 1.59 | 1.14 | 0.82 – 1.59 |
| 20–29 | 31,923 | 461 (1.4) | 1.0 | ref. | 1.0 | ref. |
| 30–39 | 10,563 | 162 (1.5) | 0.95 | 0.74 – 1.21 | 0.96 | 0.75 – 1.24 |
| 40–48 | 489 | 13 (2.7) | 1.52 | 0.72 – 3.20 | 1.49 | 0.69 – 3.20 |
| Age of the father | ||||||
| 13–19 | 1,174 | 19 (1.6) | 1.06 | 0.59 – 1.91 | 1.03 | 0.56 – 1.91 |
| 20–29 | 28,810 | 400 (1.4) | 1.0 | ref. | 1.0 | ref. |
| 30–39 | 14,435 | 231 (1.6) | 1.25 | 1.01 – 1.56 | 1.31 | 1.04 – 1.64 |
| 40–74 | 2,056 | 41 (2.0) | 1.21 | 0.79 – 1.87 | 1.20 | 0.77 – 1.87 |
| Missing | 970 | 19 (2.0) | 1.47 | 0.84 – 2.56 | 1.04 | 0.56 – 1.94 |
|
| ||||||
| Father employed around the time of conception | ||||||
| Yes | 42,612 | 592 (1.4) | 0.68 | 0.53 – 0.86 | 0.70 | 0.54 – 0.92 |
| No | 5,833 | 118 (2.0) | 1.0 | ref. | 1.0 | ref. |
In the subset analyses by gender, the low risk of SSD in Swedish speaking offspring compared to Finnish speaking offspring was evident in men (aHR 0.32, CI: 0.15–0.68), but was only marginal in women (aHR 0.75, CI: 0.41–1.37). Place of birth in the Helsinki Capital area was a risk factor in both genders. In the separate analyses for people residing in the capital area or in the rest of Finland, it turned out that place of birth in the Capital area was a risk factor only among those residing in the Capital area. Based on small numbers, being Swedish speaking was associated with a low risk of SSD in the Capital area, but also suggestively among offspring residing elsewhere. (Table 3.)
Table 3.
Risk of schizophrenia in offspring for language and place of birth according to gender and place of residence. The models are adjusted for parental psychoses and age, and father’s employment.
| Characteristics | N | Schizophrenia spectrum disorder N (%) | HR | 95% CI |
|---|---|---|---|---|
|
| ||||
| Male: | 24,121 | |||
|
| ||||
| Language | ||||
| Finnish | 22,908 | 419 (1.8) | 1.0 | ref. |
| Swedish | 1,213 | 7 (0.6) | 0.32 | 0.15 – 0.68 |
|
| ||||
| Place of birth | ||||
| Helsinki Capital area | 4,124 | 114 (2.8) | 1.79 | 1.44 – 2.22 |
| Other parts of Finland | 19,997 | 312 (1.6) | 1.0 | ref. |
|
| ||||
| Female: | 23,324 | |||
|
| ||||
| Language | ||||
| Finnish | 22,118 | 273 (1.2) | 1.0 | ref. |
| Swedish | 1,206 | 11 (0.9) | 0.75 | 0.41 – 1.37 |
|
| ||||
| Place of birth | ||||
| Helsinki Capital area | 4,033 | 64 (1.6) | 1.40 | 1.06 – 1.85 |
| Other parts of Finland | 19,291 | 220 (1.1) | 1.0 | ref. |
|
| ||||
| Place of residence in Helsinki Capital area: | 11,092 | |||
|
| ||||
| Language | ||||
| Finnish | 10,495 | 197 (1.9) | 1.0 | ref. |
| Swedish | 597 | 2 (0.3) | 0.16 | 0.04 – 0.66 |
|
| ||||
| Place of birth | ||||
| Helsinki Capital area | 5,692 | 140 (2.5) | 2.30 | 1.69 – 3.12 |
| Other parts of Finland | 5,400 | 59 (1.1) | 1.0 | ref. |
|
| ||||
| Place of residence in other parts of Finland: | 36,353 | |||
|
| ||||
| Language | ||||
| Finnish | 34,531 | 495 (1.4) | 1.0 | ref. |
| Swedish | 1,822 | 16 (0.9) | 0.63 | 0.39 – 1.04 |
|
| ||||
| Place of birth | ||||
| Helsinki Capital area | 2,465 | 38 (1.5) | 1.11 | 0.80 – 1.55 |
| Other parts of Finland | 33,888 | 473 (1.4) | 1.0 | ref. |
There were a number of partial losses to follow-up due to emigration or death in our data. Altogether 700 (1.5%) offspring, including two Finnish-speaking persons with an SSD diagnosis, emigrated during the study period. Most of the emigrations took place after 2000 between ages 17–37. The number of offspring deaths (including 42 SSD cases) were 915 (2.0%) and 36 (1.5%) in Finnish and Swedish speaking offspring respectively. As a sensitivity analysis, we investigated whether starting the follow-up from age 15 would change the results, but this did not have any effect on the findings.
4. Discussion
We found that the Swedish-speaking minority in Finland has a lower risk of schizophrenia spectrum disorders (SSD) than the Finnish-speaking majority. This effect was especially evident among men. These results are in keeping with several previous studies demonstrating better health and socioeconomic status in the Swedish-speaking minority in Finland as compared to the Finnish-speaking majority (Sipilä and Martikainen, 2009). While previous studies have not investigated mental health, the largest mortality risk differential between the Swedish-speaking minority and the Finnish-speaking majority is in mortality due to suicide and alcohol-related causes (Sipilä and Martikainen, 2009).
With a few exceptions, like the Hutterite communities in North America (Nimgaonkar et al., 2000), minority status tends to be associated with increased risk of schizophrenia (Selten et al., 2013). It has been suggested that this relates to a long-term exposure to the experience of social defeat or exclusion (the social defeat hypothesis) (Selten et al., 2013) or to cumulative social disadvantage often related to a minority status (Morgan et al., 2008). In many ways, Swedish-speaking Finns are characterized by a cumulative social advantage. Previous studies have found a lower frequency of negative childhood experiences, higher social support and participation, lower rates of divorce and unemployment and higher sense of coherence in the Swedish-speaking compared to Finnish-speaking Finns (Volanen et al., 2006; Paljärvi et al. 2009). Our result suggests that a beneficial social environment may provide resilience even to severe mental disorders.
The protective role of Swedish-speaking minority status was stronger for men than for women. One explanation could be that social and socioeconomic factors may be more important determinants of mental health in men than in women. For example, education, income, socioeconomic status as defined by occupation, employment status, marital status and area of residence together explained approximately 40% of the elevated suicide risk in the Finnish-speaking majority for men, but only 7% in women in the study by Sipilä and Martikainen (2009). A Swedish study comparing the risk of psychiatric disorders in native Swedes and different immigrant groups found similar results regarding psychotic disorders. The crude risk of psychotic disorders was almost two-fold higher in both female and male Finnish immigrants. Adjustment for various socioeconomic factors reduced the hazard ratio considerably more in men than in women (Westman et al., 2006). The same pattern was observed in several other immigrant groups in Sweden (Westman et al., 2006). However, a recent European study found few differences between men and women in factors affecting mental well-being (Dreger et al., 2014). In addition, the same gender difference in language-groups in Finland has been observed in other areas of health, like stroke (Lammintausta et al. 2009), myocardial infarction (Lammintausta et al., 2011) and mortality (Sipilä and Martikainen, 2009), and in wages and wealth (Saarela and Finnäs, 2004; Saarela, 2006). Nevertheless, further research is needed on the possible contribution of social environment to gender differences in schizophrenia.
It is also possible that genetic factors may explain some of the observed differences. However, two observations speak against a major contribution of genetic factors in the lower prevalence of SSD in Swedish-speaking Finns. First, genetic factors are unlikely to explain the observed gender difference in the Swedish-speaking population. Secondly, the Swedish speaking population living in the Western coastal area is genetically closest to the Swedish population (Salmela et al., 2011), whereas we observed the lowest risk among Swedish-speaking minority members residing in the Capital area. Regardless, the contribution of genetic factors cannot be excluded entirely.
Children born in the capital area had higher risk of schizophrenia than those born in other parts of Finland. This is the first instance in which urban birth has been clearly linked to schizophrenia in Finland, although a prior study observed the same trend in cohorts born in the 1960s (Haukka et al., 2001). After World War II, Finland experienced the most rapid industrialization in Europe, and there was considerable internal migration into the capital area from other parts of the country (Saarela, 2006). The process of spatial clustering into advantaged and more deprived neighborhoods has been ongoing in the capital area in the recent decades (Vaattovaara, 2002). Thus, it seems that the unfavorable conditions related to urban life that increase the risk of schizophrenia have emerged in the capital area of Finland during the last few decades.
Father’s employment at the time of conception was associated with lower risk of schizophrenia in our analysis. This is consistent with two other Nordic studies which found that parental unemployment during childhood was associated with increased risk of schizophrenia (Byrne et al. 2004, Wicks et al. 2010). Unfortunately, we did not have longitudinal data on parental employment, but this result adds to the literature suggesting that social circumstances at birth may be related to schizophrenia (Werner et al. 2007, Kwok 2014).
Differences in diagnostic assessment and treatment as well as loss of follow-up due to emigration are potential sources of outcome misclassification or selection bias. Differences in diagnostic assessment and treatment are likely to be minor in this case, however. Units providing treatment for the Swedish-speaking population are integrated into the service system and are not organized as separate hospitals, and the psychiatric training system is the same for Swedish- and Finnish-speaking doctors.
Emigration from Finland to Sweden has been common particularly in the 1960s and 1970s, and although the great majority represented the Finnish-speaking population, the proportion of Swedish-speaking emigrants was larger than their population share in Finland (Saarela, 2006). This could have affected our results if, among emigrants, there is a language-related difference in mental health problems that manifests after emigration. However, the effect of migration on our results is likely to be negligible given the small number of emigrants (n=700, 1.5%). In general, the Swedish-speaking Finns who immigrated to Sweden have better self-rated health, lower prevalence of retirement to disability pension and higher retirement age than Finnish-speaking immigrants (Kulla et al., 2010).
In conclusion, our results suggest that belonging to a minority group with high social capital may protect against SSD, and this effect may be more pronounced in men. Birth in the capital area was associated with increased and paternal employment at the time of conception with decreased risk of SSD. These results add to the growing literature on social factors in the etiology of schizophrenia.
Acknowledgments
We thank Ritva Luukkonen, Ph.D., for advice in the statistical analysis.
Funding
This study was funded by US NIH grant K01 MH080114 to Mark Opler (PI). Jaana Suvisaari was funded by the Sigrid Juselius Foundation. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Contributions
Authors Jaana Suvisaari, Mark Opler, Marja-Liisa Lindbohm and Markku Sallmén designed the study and wrote the protocol. Jaana Suvisaari managed the literature searches and analyses. Markku Sallmén undertook the statistical analyses, and Jaana Suvisaari wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflicts of interest
Jaana Suvisaari has served as a consultant for Janssen Cilag in a study that is not related to this manuscript and has received a lecturing fee from AstraZeneca. The other authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jaana Suvisaari, Email: jaana.suvisaari@thl.fi.
Mark Opler, Email: mark.opler@prophase.com.
Marja-Liisa Lindbohm, Email: marja-liisa.lindbohm@ttl.fi.
Markku Sallmén, Email: markku.sallmen@ttl.fi.
References
- Anttila A, Heikkilä P, Pukkala E, Nykyri E, Kauppinen T, Hernberg S, Hemminki K. Excess lung cancer among workers exposed to lead. Scand J Work Environ Health. 1995;21(6):460–469. doi: 10.5271/sjweh.62. [DOI] [PubMed] [Google Scholar]
- Byrne M, Agerbo E, Eaton WW, Mortensen PB. Parental socio-economic status and risk of first admission with schizophrenia- a Danish national register based study. Soc Psychiatry Psychiatr Epidemiol. 2004;39(2):87–96. doi: 10.1007/s00127-004-0715-y. [DOI] [PubMed] [Google Scholar]
- Dreger S, Buck C, Bolte G. Material, psychosocial and sociodemographic determinants are associated with positive mental health in Europe: a cross-sectional study. BMJ Open. 2014;4(5):e005095. doi: 10.1136/bmjopen-2014-005095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Applications of stratified analysis methods. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. 3. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008. pp. 283–302. [Google Scholar]
- Goriely A, McGrath JJ, Hultman CM, Wilkie AO, Malaspina D. “Selfish spermatogonial selection”: a novel mechanism for the association between advanced paternal age and neurodevelopmental disorders. Am J Psychiatry. 2013;170(6):599–608. doi: 10.1176/appi.ajp.2013.12101352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison G, Fouskakis D, Rasmussen F, Tynelius P, Sipos A, Gunnell D. Association between psychotic disorder and urban place of birth is not mediated by obstetric complications or childhood socio-economic position: a cohort study. Psychol Med. 2003;33(4):723–731. doi: 10.1017/s0033291703007591. [DOI] [PubMed] [Google Scholar]
- Haukka J, Suvisaari J, Varilo T, Lönnqvist J. Regional variation in the incidence of schizophrenia in Finland: a study of birth cohorts born from 1950 to 1969. Psychol Med. 2001;31(6):1045–1053. doi: 10.1017/s0033291701004299. [DOI] [PubMed] [Google Scholar]
- Hyyppä MT, Mäki J. Social participation and health in a community rich in stock of social capital. Health Educ Res. 2003;18(6):770–779. doi: 10.1093/her/cyf044. [DOI] [PubMed] [Google Scholar]
- Kiviniemi M, Suvisaari J, Pirkola S, Häkkinen U, Isohanni M, Hakko H. Five-year mortality in first-onset schizophrenia in Finland with special reference to regional differences. Psychiatr Serv. 2010;61(3):272–279. doi: 10.1176/ps.2010.61.3.272. [DOI] [PubMed] [Google Scholar]
- Kulla GE, Ekman SL, Heikkilä AK, Sarvimäki AM. Differences in self-rated health among older immigrants - a comparison between older Finland-Swedes and Finns in Sweden. Scand J Public Health. 2010;38(1):25–31. doi: 10.1177/1403494809354792. [DOI] [PubMed] [Google Scholar]
- Kwok W. Is there evidence that social class at birth increases risk of psychosis? A systematic review. Int J Soc Psychiatry. 2014 doi: 10.1177/0020764014524737. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Lammintausta A, Lehtonen A, Immonen-Räihä P, Kaarisalo M, Torppa J, Airaksinen KE, Salomaa V. Stroke morbidity in Swedish- and Finnish-speaking populations of Turku, Finland. Scand Cardiovasc J. 2009;43(2):117–22. doi: 10.1080/14017430802389537. [DOI] [PubMed] [Google Scholar]
- Lammintausta A, Immonen-Räihä P, Lehtonen A, Räihä I, Harald K, Torppa J, Airaksinen JK, Salomaa V. Myocardial infarction events and cardiovascular risk factor levels in Finnish- and Swedish-speaking populations of Finland. Ann Med. 2011;43(7):562–9. doi: 10.3109/07853890.2010.526136. [DOI] [PubMed] [Google Scholar]
- Leão TS, Sundquist J, Frank G, Johansson LM, Johansson SE, Sundquist K. Incidence of schizophrenia or other psychoses in first- and second-generation immigrants: a national cohort study. J Nerv Ment Dis. 2006;194(1):27–33. doi: 10.1097/01.nmd.0000195312.81334.81. [DOI] [PubMed] [Google Scholar]
- McGrath JJ, Petersen L, Agerbo E, Mors O, Mortensen PB, Pedersen CB. A comprehensive assessment of parental age and psychiatric disorders. JAMA Psychiatry. 2014;71(3):301–309. doi: 10.1001/jamapsychiatry.2013.4081. [DOI] [PubMed] [Google Scholar]
- Morgan C, Kirkbride J, Hutchinson G, Craig T, Morgan K, Dazzan P, Boydell J, Doody GA, Jones PB, Murray RM, Leff J, Fearon P. Cumulative social disadvantage, ethnicity and first-episode psychosis: a case-control study. Psychol Med. 2008;38(12):1701–15. doi: 10.1017/S0033291708004534. [DOI] [PubMed] [Google Scholar]
- Mortensen PB, Pedersen CB, Westergaard T, Wohlfahrt J, Ewald H, Mors O, Andersen PK, Melbye M. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340(8):603–608. doi: 10.1056/NEJM199902253400803. [DOI] [PubMed] [Google Scholar]
- Nimgaonkar VL, Fujiwara TM, Dutta M, Wood J, Gentry K, Maendel S, Morgan K, Eaton J. Low prevalence of psychoses among the Hutterites, an isolated religious community. Am J Psychiatry 2000. 2000;157(7):1065–70. doi: 10.1176/appi.ajp.157.7.1065. [DOI] [PubMed] [Google Scholar]
- Official Statistics of Finland VI A: 144. Population 1979. Structure of Population and Vital Statistics, Whole country and provinces. Central Statistical Office of Finland; Helsinki: 1981. [Google Scholar]
- Paljärvi T, Suominen S, Koskenvuo M, Winter T, Kauhanen J. The differences in drinking patterns between Finnish-speaking majority and Swedish-speaking minority in Finland. Eur J Public Health. 2009;19(3):278–84. doi: 10.1093/eurpub/ckp007. [DOI] [PubMed] [Google Scholar]
- Palo JU, Ulmanen I, Lukka M, Ellonen P, Sajantila A. Genetic markers and population history: Finland revisited. Eur J Hum Genet. 2009;17(10):1336–1346. doi: 10.1038/ejhg.2009.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perälä J, Suvisaari J, Saarni S, Kuoppasalmi K, Isometsä E, Pirkola S, Partonen T, Tuulio-Henriksson A, Hintikka J, Kieseppä T, Härkänen T, Koskinen S, Lönnqvist J. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64(1):19–28. doi: 10.1001/archpsyc.64.1.19. [DOI] [PubMed] [Google Scholar]
- Perälä J, Saarni SI, Ostamo A, Pirkola S, Haukka J, Härkänen T, Koskinen S, Lönnqvist J, Suvisaari J. Geographic variation and sociodemographic characteristics of psychotic disorders in Finland. Schizophr Res. 2008;106(2–3):337–347. doi: 10.1016/j.schres.2008.08.017. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Design Strategies to Improve Study Accuracy. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. 3. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008. pp. 168–182. [Google Scholar]
- Saarela J, Finnäs F. Interethnic wage variation in the Helsinki area. Finnish Economic Papers. 2004;17(1):35–48. [Google Scholar]
- Saarela J. Wealth in two ethnic groups: The role of internal migration background. Finnish Yearbook of Population Research. 2006;42:43–64. [Google Scholar]
- Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmela E, Lappalainen T, Liu J, Sistonen P, Andersen PM, Schreiber S, Savontaus ML, Czene K, Lahermo P, Hall P, Kere J. Swedish population substructure revealed by genome-wide single nucleotide polymorphism data. PLoS One. 2011;6(2):e16747. doi: 10.1371/journal.pone.0016747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selten JP, van der Ven E, Rutten BP, Cantor-Graae E. The social defeat hypothesis of schizophrenia: an update. Schizophr Bull. 2013;39(6):1180–6. doi: 10.1093/schbul/sbt134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sipilä P, Martikainen P. Language-group mortality differentials in Finland in 1988–2004: assessment of the contribution of cause of death, sex and age. Eur J Public Health. 2009;19(5):492–498. doi: 10.1093/eurpub/ckp074. [DOI] [PubMed] [Google Scholar]
- Sipilä P, Martikainen P. Language-group mortality differentials in Finland: the effects of local language composition. Health Place. 2010;16(3):446–451. doi: 10.1016/j.healthplace.2009.11.014. [DOI] [PubMed] [Google Scholar]
- Vaattovaara M. Future developments of residential differentiation in the Helsinki Metropolitan Area: Are we following the European model? Yearbook of Population Research in Finland. 2002;38:107–123. [Google Scholar]
- Volanen SM, Suominen S, Lahelma E, Koskenvuo M, Silventoinen K. Sense of coherence and its determinants: a comparative study of the Finnish-speaking majority and the Swedish-speaking minority in Finland. Scand J Public Health. 2006;34(5):515–25. doi: 10.1080/14034940600585812. [DOI] [PubMed] [Google Scholar]
- Werner S, Malaspina D, Rabinowitz J. Socioeconomic status at birth is associated with risk of schizophrenia: population-based multilevel study. Schizophr Bull. 2007;33(6):1373–1378. doi: 10.1093/schbul/sbm032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westman J, Johansson LM, Sundquist K. Country of birth and hospital admission rates for mental disorders: a cohort study of 4.5 million men and women in Sweden. Eur Psychiatry. 2006;21(5):307–314. doi: 10.1016/j.eurpsy.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Wicks S, Hjern A, Dalman C. Social risk or genetic liability for psychosis? A study of children born in Sweden and reared by adoptive parents. Am J Psychiatry. 2010;167(10):1240–1246. doi: 10.1176/appi.ajp.2010.09010114. [DOI] [PubMed] [Google Scholar]