Abstract
Colon cast passage, which is the spontaneous passage of a full-thickness, infarcted colonic segment per rectum, is a rare occurrence. The main cause is acute ischemic colitis resulting from a circulation compromise. Most of the colon cast cases reported were secondary to abdominal aortic aneurysm repairs or colorectal surgery. We report a case of an 80-year-old woman with ischemic colitis who excreted a 20-cm colon cast. In most cases that involve a colon cast containing a muscle layer component, invasive therapy is required owing to colonic obstruction or stenosis. However, in the present case, the colon cast consisted only of a mucosa layer and was not associated with severe stenosis or obstruction; therefore, it was successfully treated by conservative therapy. Histologic examination of the colon segment may be crucial in determining the appropriate treatment.
Key words: Colon cast, Ischemic colitis, Endoscopy
Colon cast passage, which is the excretion of a full-thickness, infarcted colonic segment per rectum, is a rare occurrence that might perplex physicians. The defecation of such a necrotic bowel segment has been observed in acute ischemic colitis caused by a circulation compromise. Most of the colon cast cases reported were secondary to abdominal aortic aneurysm repairs or colorectal surgery. Herein, we report our experience with a patient presenting with ischemic colitis, who spontaneously passed a sigmoid colon cast. We also review 22 previously reported colon cast cases.
Case Report
An 80-year-old woman presented to the emergency department complaining that she had defecated a 40-cm corded piece of dark-red tissue, without severe symptoms, after taking laxatives. She had been experiencing loss of appetite and had a tendency toward constipation. Her medical history included hypertension, trigeminal nerve lesion, and angina pectoris.
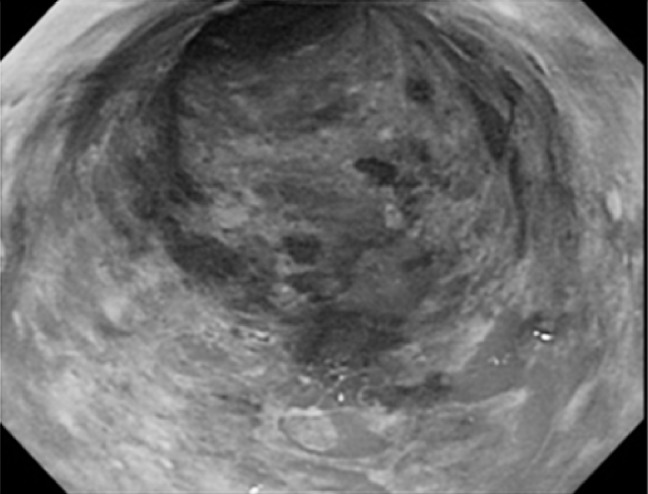
Laboratory data revealed a white blood cell count of 7.8 × 103 and a hematocrit of 31.9%. The rest of the laboratory test results, including levels of serum albumin, hepatic and pancreatic enzymes, and electrolytes, were within normal limits. On physical examination, there was a slight tenderness in the lower abdomen without guarding or rebound on palpation. We observed approximately 20 cm of a necrotic bowel segment (colon cast) protruding from her anus (Fig. 1).
Fig. 1.
Approximately 20 cm of a necrotic bowel segment (colon cast) protruding from the patient's anus
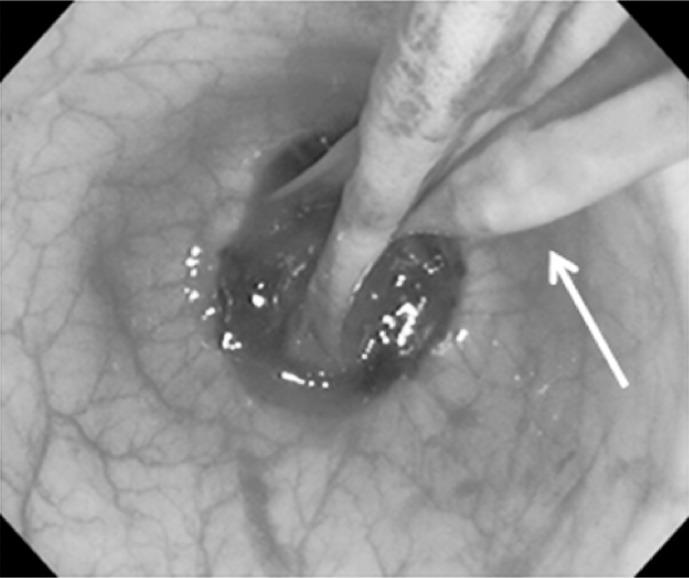
An emergency colonoscopy revealed that the sigmoid colonic mucosa located between 40 and 20 cm from the anal verge was edematous and congested. Colonoscopy could not be performed past 40 cm from the anal verge because the patient complained of pain. The dark-red segment of tissue she passed before admission was considered a colon cast because the colonic mucosa of the corresponding segment was desquamated (Fig. 2). The residual segment of the colon cast was still attached to the sigmoid colonic wall (Fig. 3).
Fig. 2.
Colonoscopy finding of deciduous sigmoid colon epithelium with edema and congestion
Fig. 3.
Colonoscopic finding of residual colon cast (arrows).
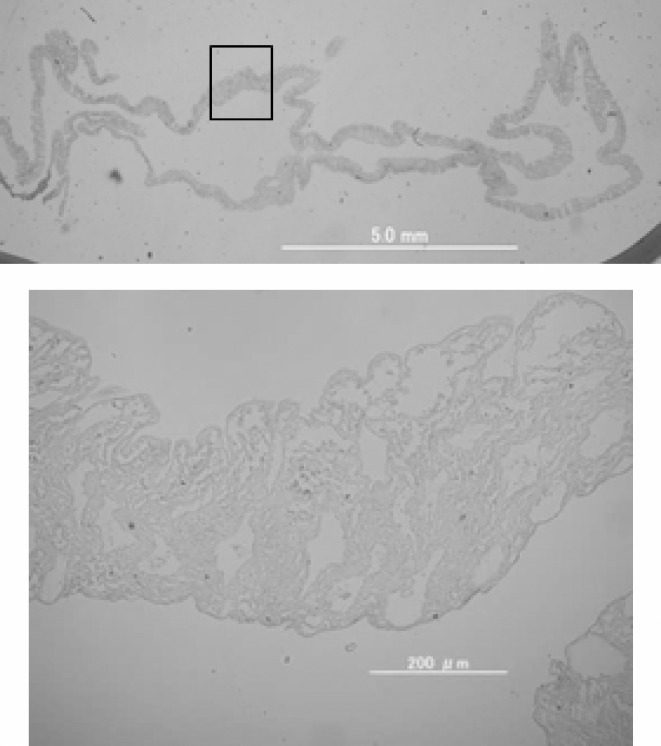
Histologic examination of the passed material indicated that the mucus layer had dissected from the colon, resulting in necrosis (Fig. 4). The segment did not contain submucosal and muscle tissues. Her stool was negative for Clostridium difficile (CD) and CD toxin. Computed tomography demonstrated thickening of the wall of the sigmoid colon, but no free intraperitoneal air, free fluid, fecal contamination, aortic aneurysm, or thrombi in superior or inferior mesenteric arteries were detected.
Fig. 4.
Histologic examination (×12.5, ×100) revealed infarcted mucosa in the discharged colon cast.
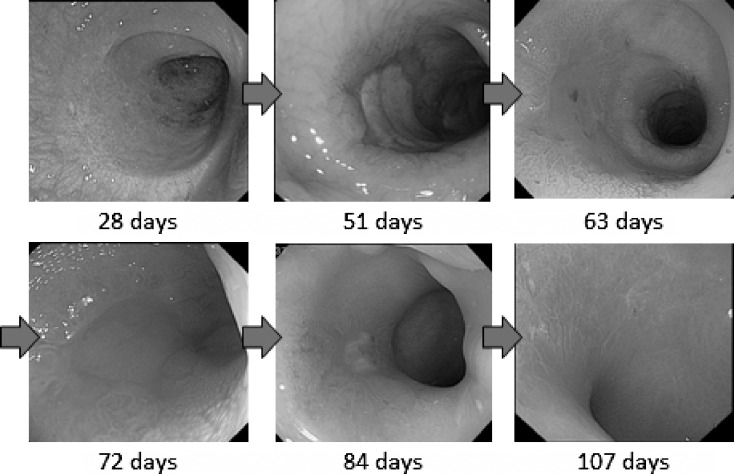
Initially, oral intake was withheld for 10 days for maintaining the rest of the digestive tract in optimal condition for mucosal tissue healing; subsequently, the patient successfully tolerated fluids and then food in 2 weeks. However, she began to present melena again when she started low-residue diets. Colonoscopy revealed persistent inflammation in the sigmoid colon; therefore, conservative treatment was continued for 2 months. Afterwards, periodic sigmoidoscopies were performed. The inflammation of the sigmoid colon progressively improved every week. Two months later, a follow-up colonoscopy demonstrated mucosal regeneration and a stenotic lumen in the sigmoid colon (Fig. 5). A water-soluble contrast enema revealed a slight stricture measuring approximately 4 cm in the sigmoid colon, although the patient was asymptomatic. The patient was discharged from the hospital 111 days after admission. At the 8-month follow-up, a barium enema revealed recovery of the intestinal tract stricture. Recurrence of colon cast has not occurred since then.
Fig. 5.
Periodic sigmoidoscopy demonstrated gradual mucosal regeneration.
Discussion
In 1984, Speakman and Turnbull1 first reported spontaneous anal passage of a full-thickness infarcted colonic segment, also known as a colon cast. This phenomenon has been described 22 times previously. Colon cast passage has been associated with a preceding circulatory disorder resulting in ischemic colitis. About 50% of these cases of colonic ischemia were secondary to blockage of the inferior mesenteric artery (IMA) in abdominal aortic aneurysm (AAA) repair surgeries1–5 and colorectal surgeries.6–8 Five of the remaining cases had no relation with vessel obstruction secondary to operations, but with ischemic colitis from preceding circulatory disorders.9–12
In the 22 previously reported cases of colon cast, the colon segment often originated from the left side of the colon, including the descending colon, sigmoid colon, and rectum, with the exception of 3 cases in which the segment originated from the ascending colon.1–17 Because of its peristaltic motion and vulnerability of the submucosal connecting tissue, the sigmoid colon appears to be a frequent site of colon cast development.13 Peristaltic motion of the sigmoid colon mobilizes intestinal contents toward the rectum 1 or 2 times per day. This movement induces high pressure on the large bowel.
In 12 of the 22 cases, blockage of the feeding arteries, including the IMA, was the main cause. In 5 of the 12 cases, the etiology was occlusion of the IMA during AAA repair. In the 7 remaining cases, colonic ischemia was caused by sacrifice of the main blood vessel (IMA in 5 cases) during colon cancer surgery. In another 10 cases, the causes included diabetic ketoacidosis, pancreatitis, trauma, graft-versus-host disease, and ischemic colitis secondary to arteriosclerotic cardiovascular disease in patients receiving anticoagulant drugs.4,9–13,16,17
In the present case, the patient had arteriosclerosis, as can be inferred from her prescribed medications including aspirin for prophylaxis of angina pectoris. Additionally, she had chronic constipation. The continuous elevated pressure on the large bowel and decrease in blood flow as a result of atherosclerosis were likely the causes of ischemic colitis in this case. Moreover, the elevated pressure on the large intestine and consequent vessel extension may have induced further circulatory compromise. The extended severe ischemic colitis was presumably the etiology of the colon cast in this case.
Data on the extent of infarction of the colonic wall were available in 19 of the reported cases. The extent of infarction from the mucosa to the muscularis propria or subserosal layer was reported in 13 cases. Such cases required management with surgical resections because of colonic stenosis/obstruction or bowel perforation. However, 2 patients did not undergo surgery owing to their deteriorated status.
In 6 patients, the extent of infarction was limited to the mucosa/submucosa. Four of the 6 patients were successfully managed by conservative therapy with endoscopic dilation of strictures. Two patients had strictures at the colorectal anastomosis site after colorectal surgery and required surgical resections. Circulatory disorders affecting surgical manipulation may also cause stenosis of the colorectal anastomosis. Despite the submucosal layer of the colon casts in 2 cases, severe stricture might result at the anastomosis site.
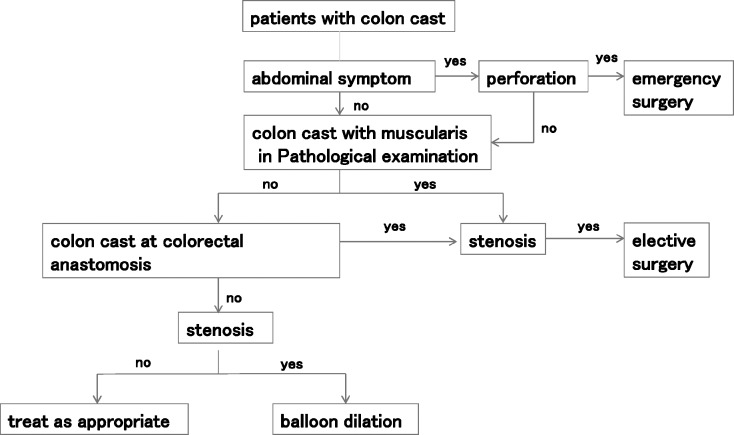
Many cases are asymptomatic, so initial conservative treatment should be chosen together with regular examinations in cases without digestive tract perforation. Histologic examination of the colon cast is important. When the specimen contains muscularis propria or the patients have colorectal anastomosis, we suggest following a surgical approach. We made a flowchart to describe the algorithm for the management of the cases with colon cast (Fig. 6).
Fig. 6.
The algorithm for the management of the cases with colon cast.
Conclusions
We report a case of colon cast passage in a patient with severe ischemic colitis successfully treated by conservative therapy. Our findings emphasize the importance of pathologic examination of the colon cast. The pathologic depth of the layer of the excreted colon cast may be crucial in determining the appropriate treatment. Patients with casts consisting of the mucosa/submucosa layer alone and without colorectal anastomosis may likely be successfully managed by conservative therapy. When the specimens contain muscularis propria or the patients have colorectal anastomosis, surgery should be considered.
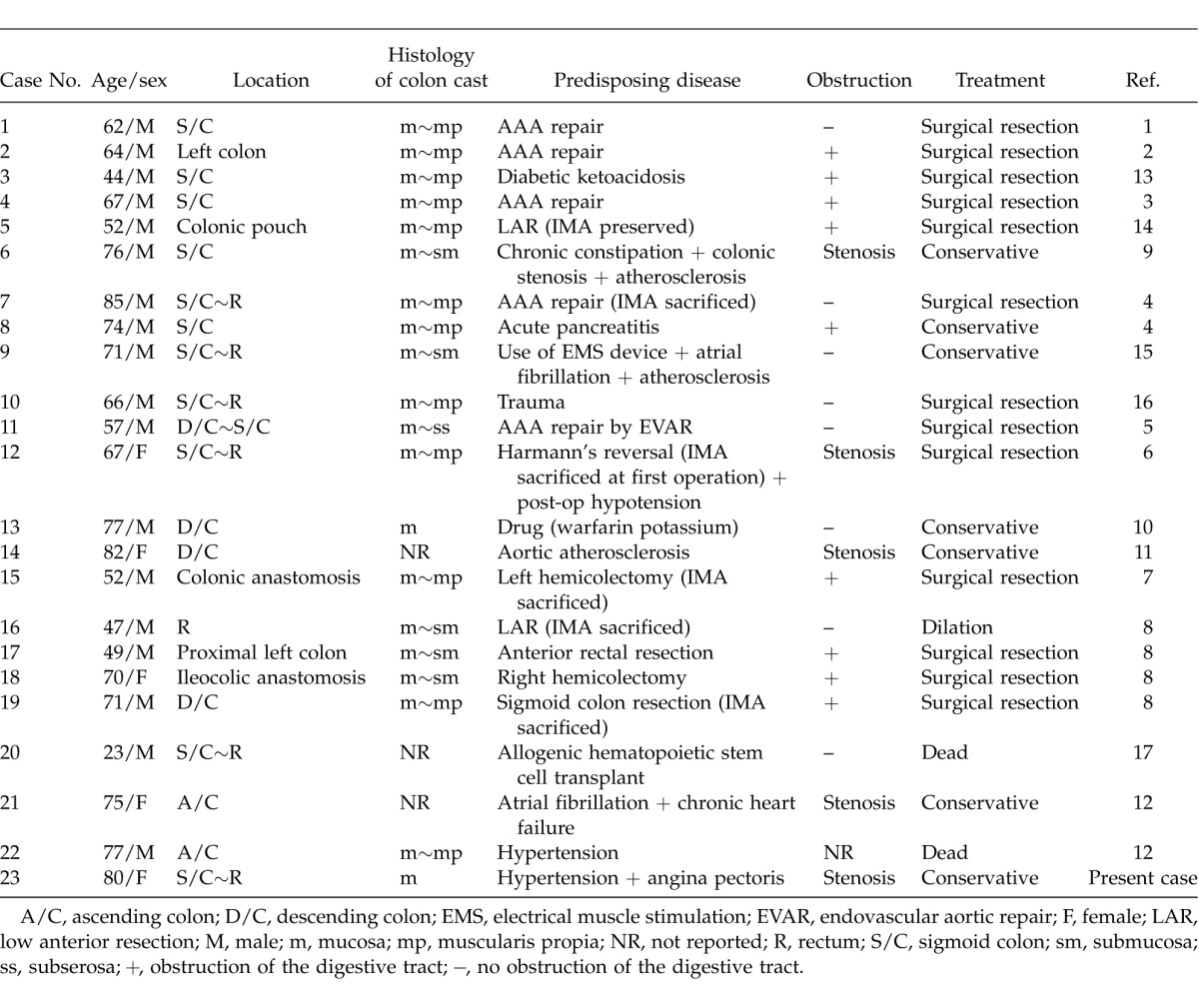
Table 1.
Clinical and pathological features of patients with colon cast
Acknowledgments
Shinya Abe and other coauthors have no conflict of interest.
References
- 1.Speakman MJ, Turnbull AR. Passage of a colon ‘cast' following resection of an abdominal aortic aneurysm [abstract] Br J Surg. 1984;71(12):935. doi: 10.1002/bjs.1800711207. [DOI] [PubMed] [Google Scholar]
- 2.Gregory PJ, Barrett G. Spontaneous passage of a colon ‘cast' in a patient with ischaemic colitis [abstract] Br J Surg. 1987;74(5):436. doi: 10.1002/bjs.1800740541. [DOI] [PubMed] [Google Scholar]
- 3.Sado S, Fujii H, Yamamoto K, Yamamoto M, Nakagawa M, Watanabe I. A case of ischemic colitis with defecation of a colon “cast” following surgery for an abdominal aortic aneurysm. J Jpn Soc Colorectal Dis. 1989;42(6):1089–1093. [Google Scholar]
- 4.Ardigo GJ, Longstreth GF, Weston LA, Walker FD. Passage of a large bowel cast caused by acute ischemia: report of two cases. Dis Colon Rectum. 1998;41(6):793–796. doi: 10.1007/BF02236272. [DOI] [PubMed] [Google Scholar]
- 5.Beattie GC, Soong CV, Hannon RJ. Rectal passage of full-thickness infarcted left colon post-endovascular stenting of abdominal aortic aneurysm—report of a case. EJVES Extra. 2005;10(6):132–135. [Google Scholar]
- 6.Foley CL, Taylor CJ, Aslam M, Reddy KP, Birch HA, Owen ER. Failure of conservative management after the passage of a distal colonic “cast”: report of a case. Dis Colon Rectum. 2005;48(5):1090–1093. doi: 10.1007/s10350-004-0863-x. [DOI] [PubMed] [Google Scholar]
- 7.Biondi A, Persiani R, Rausei S, Cananzi FC, Zoccali M, Vecchioli A. Large bowel auto-amputation and passage of a colon ‘cast' after left hemicolectomy. Int J Colorectal Dis. 2008;23(5):551–552. doi: 10.1007/s00384-007-0394-8. [DOI] [PubMed] [Google Scholar]
- 8.Erguney S, Yavuz N, Ersoy YE, Teksoz S, Selcuk D, Ogut G. Passage of “colonic cast” after colorectal surgery: report of four cases and review of the literature. J Gastrointest Surg. 2007;11(8):1045–1051. doi: 10.1007/s11605-007-0194-z. [DOI] [PubMed] [Google Scholar]
- 9.Yoshiji H, Nakae D, Sugiya R, Mizumoto Y, Tsutsumi M, Hiriguchi K. Spontaneous passage of a colon cast in the absence of abdominal aneurysm. J Gastroenterol. 1994;29(1):80–83. doi: 10.1007/BF01229079. [DOI] [PubMed] [Google Scholar]
- 10.Ogino H, Kubo S, Misawa T, Nasu T, Ihara Y, Sasamoto Y. A case of the passage of a stripped colonic mucosa. Gastroenterol Endosc. 2005;47(1):22–27. [Google Scholar]
- 11.Eriguchi Y, Tsunada S, Amemori S, Watanabe K, Fujise T, Kikkawa A. A case of relapsed ischemic colitis with colon cast–like stripped mucosa. Jpn J Gastroenterol. 2006;103(10):1152–1156. [PubMed] [Google Scholar]
- 12.Takeuchi N, Miki K, Fujita K, Takata M, Nishibori Y, Maruyama T. Two case reports of ischemic colitis with a colon cast developed after circulatory compromise. Heart. 2011;43(10):1350–1356. [Google Scholar]
- 13.Masuda T, Fukumoto T. A case of severe ischemic colitis developing, complete intestinal obstruction after conservative treatment [in Japanese with English abstract] Gastroenterol Endosc. 1988;30(10):2326–2330. [Google Scholar]
- 14.Sakanoue Y, Kusunoki M, Shoji Y, Kusuhara K, Yamamura T, Utsunomiya J. Passage of a colon “cast” after anoabdominal rectal resection: report of a case. Dis Colon Rectum. 1990;33(12):1044–1046. doi: 10.1007/BF02139222. [DOI] [PubMed] [Google Scholar]
- 15.Tsujimoto T, Takano M, Ishikawa M, Tsuruzono T, Matsumura Y, Kitano H. Onset of ischemic colitis following use of electrical muscle stimulation (EMS) exercise equipment. Intern Med. 2004;43(8):693–695. doi: 10.2169/internalmedicine.43.693. [DOI] [PubMed] [Google Scholar]
- 16.Moriwaki Y, Kanaya K, Yamamoto T, Sugiyama M. A case of ischemic colitis with colon cast due to lower abdominal trauma with pelvic fracture. Jpn J Gastroenterol Surg. 2004;37(12):1914–1919. [Google Scholar]
- 17.Al Ashgar H, Peedikayil M, Chaudhri N, Al-Ghamdi A. Defecation of a “colon cast” as a rare presentation of acute graft-versus-host disease. Ann Saudi Med. 2009;29(3):231–233. doi: 10.4103/0256-4947.51783. [DOI] [PMC free article] [PubMed] [Google Scholar]