Abstract
This report describes an alternative technique for Petit hernia repair. The treatment of lumbar hernias should follow the concept of tension-free surgery, and the preperitoneal space can be the best place for prosthesis placement. An obese patient had a bulge in the right lumbar region, which gradually grew and became symptomatic, limiting her daily activities and jeopardizing her quality of life. She had previously undergone 2 surgical procedures with different incisions. We created a preperitoneal space and attached a mesh in this position. Another prosthesis was placed on the muscles, with a suitable edge beyond the limits of the defect. There were no complications. It has been described as a safe and tension-free repair for Petit hernia. In larger defects, a second mesh can be used to prevent further enlargement of the triangle and also to provide additional protection beyond the bone limits.
Key words: Hernia, Lumbar hernia, Open repair, Prosthetic mesh repair
Dorsal or lumbar hernias are found in the posterior abdominal wall at the level of the lumbar region. This condition is uncommon, and there are no major series of such cases reported in the literature. They can be classified as congenital or acquired conditions. Acquired hernias are almost always unilateral and have etiopathogenic factors such as obesity, coughing, repeated physical activity, and parietal weakening.1–3
The most common site for the occurrence of lumbar hernias is in the superior lumbar triangle (Grynfeltt) and less commonly in the inferior lumbar triangle (Petit).1 Surgical treatment of lumbar hernias is always recommended because of the risks of entrapment and strangulation.4 There is still ongoing discussion regarding which is the best surgical technique to be employed. It has been described that approximation of the limits of the hernia may be sufficient for small hernias, while in most cases the use of mesh is recommended. The growth in laparoscopic repair of abdominal wall hernias has brought on the use of the preperitoneal space (sublay). In this site, using mesh requires skill and experience in order to create sufficient space and to ensure proper placement of the mesh beyond the limit of the bones in the Petit‘s triangle. We present an alternative technique for tension-free repair of lumbar hernias when the use of laparoscopy is not recommended.
Case Report
N.S.G. is a retired, white, 65-year-old woman. Her body mass index was 42 kg/m2, and she had a background of having undergone hysterectomy 7 years before for fibroids, and cystectomy and uretero-enterostomy 5 years before for bladder cancer. Her stoma was located to the right of the midline in the lower abdomen. The patient came into the emergency room complaining of back pain related to a bulging in her right lumbar region. She reported having noticed this bulge as a result of physical exertion about 6 years earlier. It was asymptomatic, but progressively increased, and at that time caused difficulty in walking and jeopardized the patient's daily activities. In the abdomen were scars of Pfannenstiel and median infraumbilical incisions. On physical examination, a bulge of approximately 10 cm protruding in the right dorsal region and above the iliac crest was noticed during valsalva maneuver. It was reducible by manipulation with no signs of strangulation, and it was not possible to delimit a hernia ring.
Ultrasonography showed a defect in the abdominal wall in the right posterolateral lumbar region measuring about 6.4 × 5.5 cm, with herniation of small intestine and adipose tissue. With a diagnosis of a Petit's dorsal hernia, surgical treatment was recommended.
Surgical Technique
The patient was placed in a left lateral position. A transverse incision was made approximately 10 cm above the iliac crest and alongside the paraspinal musculature. Subcutaneous dissection revealed a large hernia sac protruding along the lower portion of the latissimus dorsi muscle, the superior edge of the iliac crest, and medial to the external oblique muscle (Fig. 1).
Fig. 1.
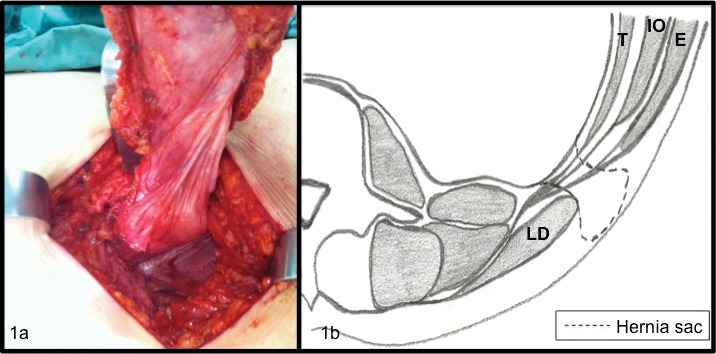
(a) Large hernia sac after dissection of the subcutaneous tissue. (b) Scheme representing a transverse anatomical view of the hernia sac protruding through the Petit's triangle. T, transversum abdominis muscle; IO, internal oblique muscle; E, external oblique muscle; LD, latissimus dorsi muscle.
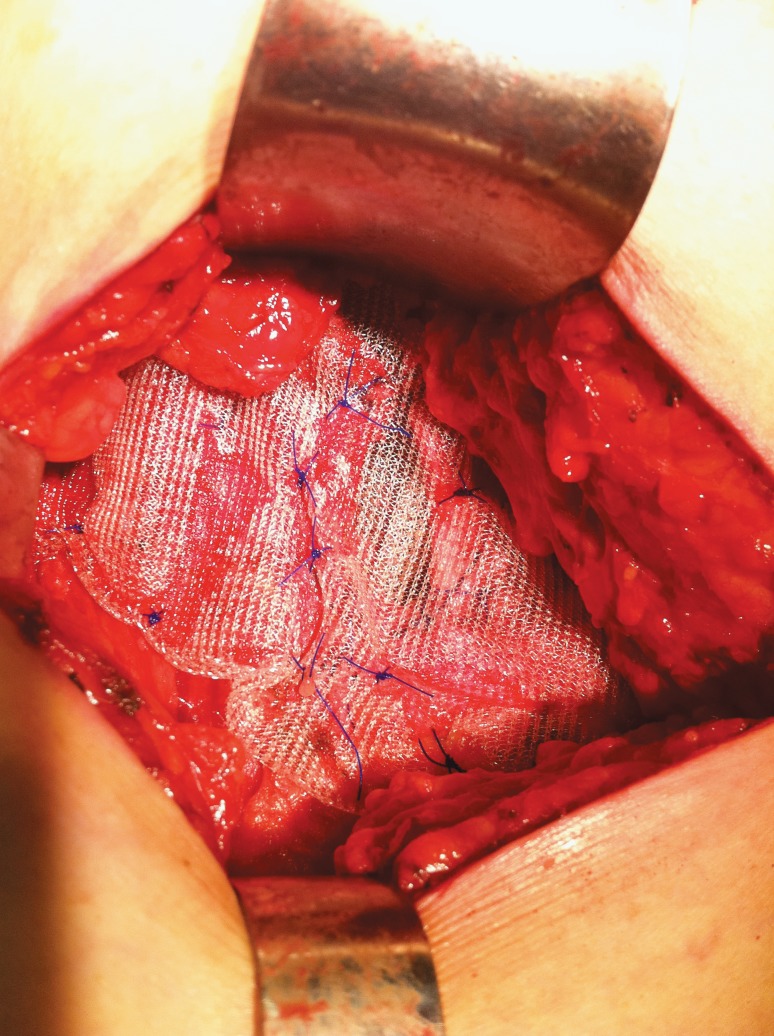
The hernia sac was completely dissected from its limits and reduced. Without harming the hernia sac, a preperitoneal plane was created just below the muscles that delimit the Petit's triangle. A heavyweight polypropylene mesh was inserted into this space. The fixing stitches were made with 2/0 polypropylene by transfixing the external oblique muscle and the latissimus dorsi, thus allowing a correct mesh opening in this space (Fig. 2). The edges of the Petit‘s triangle were then brought together at their limits to reduce the hernia defect. Another mesh was placed on the muscles, in the “onlay” position, covering the lower limit above the iliac crest and attached by making several simple stitches (Fig. 3). A suction drain was left in a subcutaneous position. Subcutaneous approximation was performed with absorbable monofilament sutures. Intradermal stitches were made in the skin, and a pressure dressing was applied.
Fig. 2.
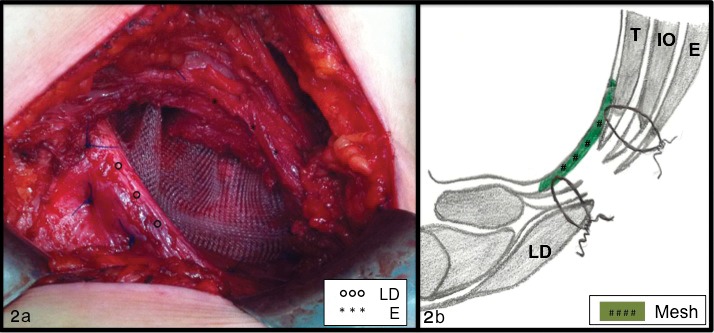
(a) Petit's triangle after placement of sublay mesh. (b) Scheme representing a transverse anatomical view of the position of the sublay mesh and the transfixing stitches. E, external oblique muscle; LD, latissimus dorsi muscle.
Fig. 3.
Final aspect with onlay mesh.
The drain was removed on the second postoperative day, and the patient was discharged the following day. The patient has been followed to date, and no complications have been reported regarding the healing of the wound. Upon the latest checkup, 10 months after surgery, esthetic appearance was satisfactory and there were no signs of recurrence. The patient has remained asymptomatic, and daily activities have been resumed without any restrictions.
Discussion
Lumbar hernias are rather uncommon, and around 300 primary cases have been reported.5 Petit's triangle, or the inferior triangle, comprises at its lower portion the edge of the iliac crest, laterally the oblique external edge, and on its medial face the lateral edge of the latissimus dorsum muscle. Some variations have been described, mainly regarding its size.3,6
Because it is more common, most studies report cases of lumbar hernias through the Grynfeltt‘s triangle. In the 11 cases of Zhou et al, 7 all of them had hernias of the superior lumbar triangle, and in 1 case there were hernias at both anatomical sites. It is acceptable to extrapolate these results to the cases of Petit‘s hernia due to similar pathophysiology, risk factors, and anatomy, and mainly due to the scarcity of specific publications.
Lumbar hernias can be divided into 2 categories: congenital or acquired. The latter type is more common, and it may also be divided into primary and secondary subcategories. This article presented a hernia of the lumbar lower triangle, which was primary and acquired. Despite previous surgical operations that may have favored the development of hernias, no incision was carried out on the site of the bulge.8
Some authors7,9 believe that surgical treatment of lumbar hernias should be based on the size of the defect, and surgery, therefore, should be performed only in cases of hernias with small defects. However, we believe that repair of these hernias should follow the trend of the treatment of inguinal hernias, based on the evidence of the superiority of tension-free repair and the possibility of using the extraperitoneal space, as has been demonstrated by laparoscopy. The orifice of the triangle, which is originally virtual, becomes a 3-dimensional space after the destruction caused by the hernia content. Only a repair with the placement of a sublay mesh protects the muscles and the intermuscular spaces. The mesh should be placed so as to cover the entire defect, and its distal limits should be at least 5 cm from each edge. Obeying the principle of Pascal, the intra-abdominal pressure will be distributed to the preperitoneal space by means of the mesh, thus protecting the hernia orifice. Some authors argue that the intra-abdominal pressure alone is enough to hold the mesh in place.10,11 In this case, transfixing stitches were used in order to ensure the positioning of the mesh and also to open it in the appropriate space. The use of several stitches can increase postoperative pain,12 so few well-spaced stitches should be made, transfixing the firm tissues, but with knots without tension in order to avoid entrapment of the nerves.
In laparoscopic repair, performing the placement of the mesh under direct view seems to ensure the proper placement of it. The lower edge of the defect comprises a bone limit that complicates the implementation of mesh by anterior repair. As an alternative, Carbonell et al13 presented the use of anchor bone fixation, but this requires specific materials and can cause postoperative pain. In this case, we used another onlay mesh, covering the defect and crossing the edge of the iliac crest. The mesh was also affixed along the edges of the triangle to avoid enlargement of the triangle. This surgical technique can be compared with the Prolene Hernia System (PHS) for inguinal hernias. It was first described in 1998; since then, its use has spread, and good results can be found in the literature.14
Laparoscopy seems to bring the advantages of performing a minimally invasive technique without jeopardizing the outcome of treatment of lumbar hernias. In this case, due to previous surgical interventions, it was deemed that greater benefits were to be obtained with an anterior approach. The retroperitoneum space can also be accessed directly by using retroperitoneoscopy. This technique uses totally extraperitoneal surgical artifices for the repair of inguinal hernias, and dissection of the this space is performed by using optical with the help of 5-mm forceps.15,16
We proposed treating a lumbar hernia through the Petit's triangle, with a tension-free repair by placement of a 2-layer mesh. Sublay mesh is considered the most important aspect in such a repair, and it follows the principles of the laparoscopic approach. The placement of another onlay prosthesis increases protection on the lower edge of the iliac crest, and its placement should be considered, especially in larger defects, in order to avoid separation of the muscles that delineate the triangle.
References
- 1.Wakhlu A, Wakhlu AK. Congenital lumbar hernia. Pediatr Surg Int. 2000;16((1–2)):146–148. doi: 10.1007/s003830050048. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy MC, Lemmon GW. Traumatic lumbar hernia: a seat belt injury. J Trauma. 1996;40(1):121–122. doi: 10.1097/00005373-199601000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Loukas M, Tubbs RS, El-Sedfy A, Jester A, Polepalli S, Kinsela C, et al. The clinical anatomy of the triangle of Petit. Hernia. 2007;11(5):441–444. doi: 10.1007/s10029-007-0232-5. [DOI] [PubMed] [Google Scholar]
- 4.Bathla L, Davies E, Fitzgibbons RJ, Jr, Cemaj S. Timing of traumatic lumbar hernia repair: is delayed repair safe? Report of two cases and review of the literature. Hernia. 2011;15(2):205–209. doi: 10.1007/s10029-009-0625-8. [DOI] [PubMed] [Google Scholar]
- 5.Moreno-Egea A, Baena EG, Calle MC, Martinez JAT, Albasini JLA. Controversies in the current management of lumbar hernias. Arch Surg. 2007;142(1):82–88. doi: 10.1001/archsurg.142.1.82. [DOI] [PubMed] [Google Scholar]
- 6.Standring S. Grays Anatomy. 39th ed. Edinburgh, UK: Elsevier/Churchill/Livingstone; 2005. pp. 734–735. ed. [Google Scholar]
- 7.Zhou X, Nve JO, Chen G. Lumbar hernia: clinical analysis of 11 cases. Hernia. 2004;8(3):260–263. doi: 10.1007/s10029-004-0230-9. [DOI] [PubMed] [Google Scholar]
- 8.Ng SSM, Ng NC, Liu AYW, Lee FY. Radiology for the surgeon: soft-tissue case 58. Can J Surg. 2006;49(2):129–130. [PMC free article] [PubMed] [Google Scholar]
- 9.Stamatiou D, Skandalakis JE, Skandalakis LJ, Mirilas P. Lumbar hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2009;75(2):202–207. [PubMed] [Google Scholar]
- 10.Garg CP, Sharma P, Patel G, Malik P. Sutureless meshplasty in lumbar hernia. Surg Innov. 2011;18(3):285–288. doi: 10.1177/1553350610397214. [DOI] [PubMed] [Google Scholar]
- 11.Edwards C, Geiger T, Bartow K, Ramaswamy A, Fearing N, Thaler K, et al. Laparoscopic trans-peritoneal repair of flank hernias: a retrospective review of 27 patients. Surg Endosc. 2009;23(12):2692–2696. doi: 10.1007/s00464-009-0477-4. [DOI] [PubMed] [Google Scholar]
- 12.Negro P, Basile F, Brescia A, Buonanno GM, Campanelli G, Canonico S. Open tension-free Lichtenstein repair of inguinal hernia: use of fibrin glue versus sutures for mesh fixation. Hernia. 2011;15(1):7–14. doi: 10.1007/s10029-010-0706-8. [DOI] [PubMed] [Google Scholar]
- 13.Carbonell AM, Kercher KW, Sigmon L, Matthews BD, Sing RF, Kneisl JS, et al. A novel technique of lumbar hernia repair using bone anchor fixation. Hernia. 2005;9(1):22–26. doi: 10.1007/s10029-004-0276-8. [DOI] [PubMed] [Google Scholar]
- 14.Woods B, Neumayer L. Open repair of inguinal hernia: an evidence-based review. Surg Clin N Am. 2008;88(1):139–155. doi: 10.1016/j.suc.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Habib E. Retroperitoneoscopic tension-free repair of lumbar hernia. Hernia. 2003;7(3):150–152. doi: 10.1007/s10029-002-0109-6. [DOI] [PubMed] [Google Scholar]
- 16.Moreno-Egea A, Aguayo JL. Ambulatory laparoscopic repair of inferior lumbar or Petit hernia. Surg Endosc. 2002;16(7):1107. doi: 10.1007/s00464-001-4250-6. [DOI] [PubMed] [Google Scholar]