Abstract
Background
Bipolar disorder (BD) is a devastating disorder with a strong genetic component. While the frontolimbic profile of individuals suffering from BD is relatively well-established, there is still disagreement over the neuroanatomical features of unaffected BD offspring.
Material and methods
Brain volumetric measures were obtained for 82 children and adolescents including 18 unaffected BD offspring (10.50±3.37 years), 19 BD offspring suffering from psychiatric disorders (12.87±3.28 years) and 45 healthy controls (HC-10.50±3.37 years). Clinical diagnoses were established according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria. Cortical reconstruction and volumetric segmentation were performed with the Freesurfer image analysis suite. Profile analyses compared frontolimbic volumes across groups. Age, gender, testing site, ethnicity and intracranial volume were entered as covariates.
Results
The right amygdala was significantly larger in unaffected BD offspring compared to BD offspring with psychiatric disorders and HC. Volumes of striatal, hippocampal, cingulate, and temporal regions were comparable across groups.
Discussion
The size of the amygdala may be a marker of disease susceptibility in offspring of BD parents. Longitudinal studies are needed to examine rates of conversion to BD as related to specific pre-morbid brain abnormalities.
Keywords: bipolar disorder, offspring, amygdala, volume, Freesurfer
Introduction
Bipolar disorder (BD) is a devastating illness with deleterious functional and social consequences for both the affected individuals and their families (1, 2). This serious illness has a substantial genetic component (3) with heritability estimates ranging from 70% to 80% (4, 5). Alongside the genetic vulnerability to bipolar disorder in BD offspring the prevalence of mood disorders is in the range of 5% to 67% compared to 0% to 38% in offspring of healthy individuals (6–9). In spite of the abundant research in BD, there is still no neural marker of genetic susceptibility for this serious disease.
Volumetric differences in brain areas involved in affect regulation and emotion processing, such as the prefrontal cortex, the amygdala, the striatum, the anterior cingulate, and the hippocampus, have been consistently regarded as potential markers for BD (10–18). Adolescents with BD have been found to exhibit smaller orbitofrontal regions, anterior cingulate and medial temporal regions compared to their healthy counterpart (19). By contrast, knowledge of the neuroanatomy of BD offspring is limited. Two studies showed that unaffected BD offspring exhibit smaller hippocampus and parahippocampus volumes, as well as enlarged right inferior frontal gyrus compared to age-matched healthy children (20, 21). By contrast, other studies found comparable prefrontal, striatal, amygdala, hippocampus and subgenual cortex volumes between affected and unaffected BD offspring and healthy controls (22–26). The inconsistencies in the current literature may also be associated to the variety of techniques (manual tracing, semi and fully automated brain segmentation with voxel-based morphometry) used to demarcate brain structures. As a result, the location of some of the brain regions may differ across studies. Other potential explanations for these mixed findings could be related to the heterogeneity of the mood disorders suffered by affected BD offspring, the severity of the mood symptoms and the illness duration.
The meaning of these brain abnormalities in relation to the genetic susceptibility for BD has yet to be characterized. While the volumetric reductions could be linked to neurotoxic mechanisms induced by BD (27) the enlargement in brain volume has been related to neuroprotective mechanisms (28). For instance, lithium-treated BD patients have been shown to have larger amygdala, hippocampus and posterior subgenual geniculate cortex volumes than unmedicated BD patients (29–31). These findings suggest that lithium counteracts the loss of brain tissue associated with BD, possibly via mechanisms of neuroplasticity (32). It becomes apparent that more research is needed to validate current findings and lead to relevant clinical recommendations.
The aim of this study was to compare the volumes of frontolimbic brain structures between affected and unaffected offspring of BD parents using the surface-based method Freesurfer. To the best of our knowledge, no published study has exploited this methodological approach to characterize the neuroanatomy of BD offspring. Based on previous findings we hypothesized that brain volumes would be smaller in BD offspring with psychiatric disorders compared to unaffected BD offspring and healthy individuals.
Methods and materials
Subjects
Participants were recruited from inpatient and outpatient clinics of the University of Texas Health Science Center at San Antonio (UTHSCSA) and at the University of North Carolina at Chapel Hill (UNC). The recruitment strategies were the same between the two clinical sites. The affected parent of participating offspring was required to complete a Structured Clinical Interview for DSM Disorders (SCID) to confirm the diagnosis of BD. If the diagnosis was confirmed, BD offspring were considered to be eligible to participate in the study. The study protocol was approved by the local Institutional Review board and informed consent was obtained from all the participants.
The sample (N = 82 children and adolescents) included 18 unaffected offspring of a BD parent (10.50±3.37 years, 9 males), 19 BD offspring with psychiatric disorders (12.87±3.28 years, 10 males), and 45 healthy controls (HC-12.73±3.37 years, 23 males). The affected BD sample included children and adolescents with BD (2), BD not otherwise specified (NOS) (7), generalized anxiety disorder (GAD – 3), Adjustment disorder (1), Major depressive disorder (2), Major Depressive Disorder Not Otherwise specified (2), and Attention Deficit Hyperactivity Disorder (ADHD - 2). 7 of the 19 affected BD offspring were on psychiatric medication (atypical antipsychotics, antidepressants, anticonvulsants, stimulants) at the time of assessment. Participating offspring and healthy controls were aged between 6 and 17 years, had no history of substance abuse in the previous 6 months and no current medical problems. BD offspring with psychiatric disorders included individuals suffering from BD, depression, mood dysregulation, anxiety and attention deficit hyperactivity disorder (ADHD). Healthy controls with a history of any Axis I disorder in first-degree relatives and use of psychoactive medication less than 2 weeks prior to the start of the study were excluded. Female participants of reproductive age underwent a urine pregnancy test. All participants underwent a urine drug screen to exclude illegal drug use.
Clinical measures
Psychiatric diagnosis was established using the Kiddie-Sads-Present and Lifetime Version (K-SADS-PL) interview (33) based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria, and confirmed subsequently in a clinical evaluation with a research psychiatrist. All parents who reported previous BD I diagnosis had their diagnosis ascertained by the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders Axis I (SCID I) (34). The affective state was assessed with the Hamilton Depression Rating Scale (HAM-D) - 21 items and the Young Mania Rating Scale (YMRS) (35). At enrollment participants were asked to complete the Pubertal Development Scale (36), a self-report questionnaire comprising 5 statements rated on a 5-point Likert scale.
MRI data acquisition and preprocessing
All images were acquired on a Siemens 3 T Trio scanner using an axial three-dimensional, T1 weighted MP-RAGE (Magnetization Prepared Rapid Acquisition gradient echo) sequence (repetition time 22 msec; echo time 3 msec; flip angle 13 degrees, slice thickness 0.8 mm), while at UNC, images were obtained on a Siemens 3 T Allegra scanner by means of an axial three-dimensional, T1 weighted MP-RAGE sequence (repetition time 17.5 ms; echo time 4 msec; flip angle 8 degrees, slice thickness 0.8 mm). Cortical reconstruction and volumetric segmentation were performed with the Freesurfer image analysis suite (Freesurfer v5.00, http://surfer.nmr.mgh.harvard.edu) (37, 38). Freesurfer estimates cortical and subcortical volumes via a whole brain segmentation procedure (38). This method is based on an atlas containing probabilistic information on the location of structures (38). The post-processing outputs for each subject were examined visually to ensure processing accuracy and image quality and no manual edits were required. Freesurfer volumetric measures have been shown to have satisfactory test-retest reliability across scanner manufacturers and across field strengths (39). As part of the intersubject registration, Freesurfer uses a surface geometry approach which improves the reliability of the matching of homologous cortical regions. Furthermore, the intersubject registration is based on the white matter surface geometry rather than the gray matter. This approach excludes coregistration errors associated with the morphometric anomalies observed in BD, such as brain atrophy (9).
Statistical Analyses
Statistical analyses were performed using Statistical Analysis System Software, version 9.1 (SAS Institute, Cary, NC) and SPSS statistical software, version 10.0 (ISI ResearchSoft, Berkeley, CA). The Shapiro-Wilks test was conducted to check whether the data distribution approached normality. PROC POWER in SAS was used for power calculations. One-way analysis of variance (ANOVA), and chi-square of independence tests (χ2) were conducted to compare demographic and clinical characteristics across groups. Profile analyses compared the volumes of 20 regions of interest (frontal and temporal poles, caudate, pallidum, putamen, amygdala, fusiform gyrus, parahippocampus, hippocampus, anterior cingulate gyrus) in the right and left hemisphere. The anterior cingulate gyrus included the caudal and rostral components of the anterior cingulate for each hemisphere. Intracranial volume, age, gender, testing site and ethnicity were entered as covariates into the model. The threshold of statistical significance was set at p < 0.05 and an FDR correction for multiple comparisons was used.
Results
Subject demographics
There were no significant differences in ICV and pubertal development between the three groups but unaffected BD offspring were younger than HC and BD offspring with psychiatric disorders (F(2,79) = 3.66, p = .03). As illustrated in Table 1 unaffected BD offspring had lower YMRS and HAM-D scores than BD offspring with mood disorders.
Table 1.
Demographic measures comparisons between healthy controls, affected and unaffected BD offspring.
| Unaffected BD offspring |
Affected BD offspring |
Healthy individuals | |
|---|---|---|---|
| Sample (N) | 18 | 19 | 45 |
| Age (in years, M±SD) | 10.50±3.37 | 12.87±3.28* | 12.73±3.32 |
| Sex (M) | 9 | 10 | 23 |
| YMRS - (M±SD) | .33±.65 | 3.28±4* | - |
| HAM-D – (M±SD) | 1.25±1.89 | 5.75±5.65* | - |
| Age at illness onset (in years, M±SD) | - | 8.2±2.78 | - |
| Pubertal Development Scale (M±SD) | 10.58±5.25 | 10.84±5.09 | 11.71±4.96 |
| Ethnicity (N) | |||
| Caucasian | 17 | 16 | 24 |
| Hispanic | 0 | 2 | 8 |
| African American | 0 | 1 | 7 |
| American Indian | 0 | 0 | 2 |
| Asian | 1 | 0 | 2 |
| Hawaiian/Pacific islander | 0 | 0 | 2 |
| Two or more ethnicities | 0 | 1 | 0 |
| Participants on medication (N) | 0 | 7 | 0 |
Abbreviations: YMRS = Young Mania Rating Scale; HAM-D = Hamilton Rating Depression Scale;
p ≤0.05.
Brain volumes
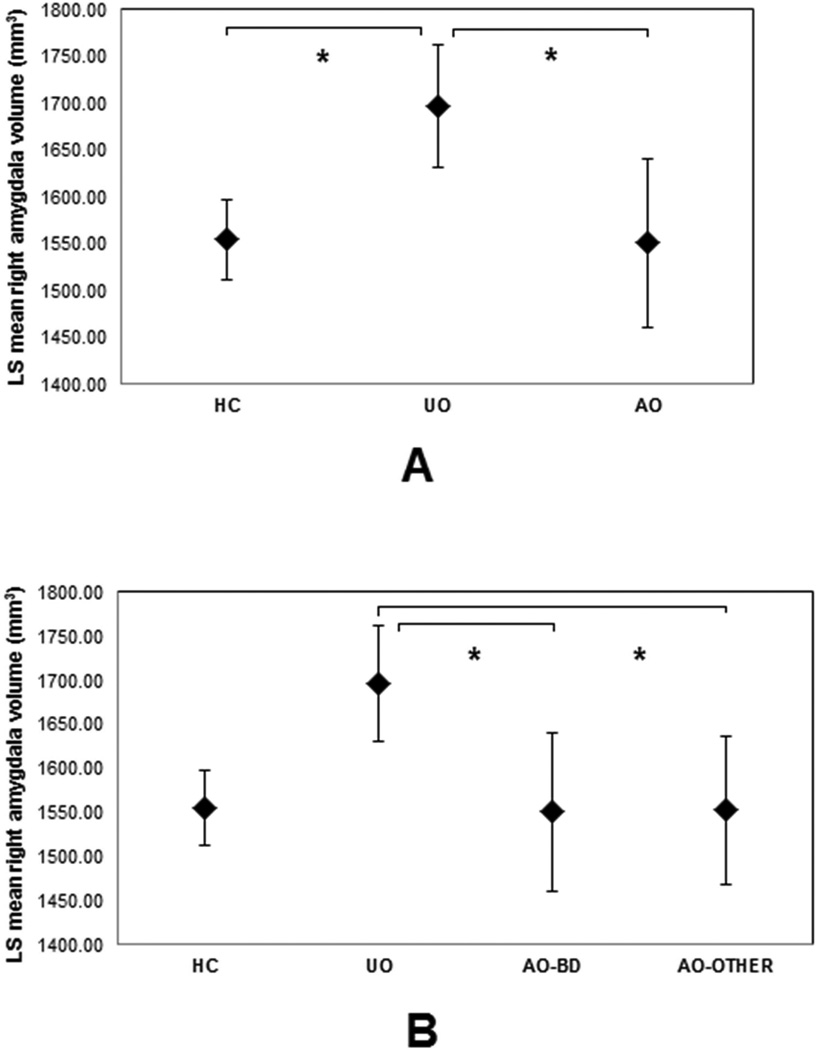
Multiple comparison analyses found volumetric differences in the right amygdala (F(2,70) = 8.29, FDR corrected p = 0.0117, η2 = 0.1019) whereby unaffected BD offspring showed a larger volume compared to affected BD offspring and HC. Exploratory analyses comparing unaffected offspring (UO) to offspring with BD (AO-BD, including offspring with BD NOS) and other mood disorders (AO-Others) showed a significantly enlarged right amygdala in unaffected offspring. By contrast the amygdala volumes of offspring with BD were comparable to those of HC (Figure 1). The left amygdala, the right caudate, the right fusiform and the right frontal poles showed a group effect at an uncorrected p<.05 but did not survive multiple testing correction. Volumes of striatal, hippocampal, cingulate, and temporal regions were comparable across groups (Table 1S).
Figure 1.
Least squares means of right amygdala volumes (mm3) with age, gender, ethnicity and ICV as covariates in healthy controls (HC), unaffected (UA) and affected offspring (AO-BD) (Panel A), and in AO-BD and offspring with other mood disorders (AO-Other) (Panel B). Vertical bars denote 95% confidence intervals. *p<.05.
Post-hoc power analysis
Power analysis revealed a 94% chance of detecting volumetric differences in the right amygdala in a sample of 82 subjects, at a corrected p-value of 0.015 (Table 2S).
Discussion
The present study aimed to evaluate the volumetric differences between BD offspring with psychiatric disorders and unaffected high-risk BD offspring aged between 6 and 17 years using a whole-brain, surface-based approach with the Freesurfer image analysis suite. This innovative technique was selected to provide a more precise anatomical definition of the brain regions compared with manual tracing of brain regions and better matching of homologous cortical regions than voxel-based morphometry (VBM) techniques. The most compelling result of this study is that, relative to BD offspring with psychiatric disorders and healthy controls, unaffected offspring of BD parents exhibit larger amygdala volumes in the right hemisphere.
A number of studies have emphasized the role of the amygdala in the pathophysiology of BD (40, 41). However, findings of volumetric studies in BD are mixed and the size of the amygdala has been reported to be both decreased (42–45), unchanged (46–48) and increased (49–51). Smaller volumes in the left and right amygdala were found in BD children previously treated with psychotropic medication (52), while other studies did not detect any amygdalar abnormalities in either monozygotic twins discordant for BD (53), BD offspring (54) or unaffected relatives of BD (55, 56). Notably, a longitudinal study showed a delayed amygdalar development in adolescents who had recently experienced their first manic episode (46). In this study remitted individuals displayed larger amygdala volumes than those who had not achieved full recovery by 1 year (as measured by the Modified Longitudinal Interval Follow-up Examination) (46). The latter finding suggests that BD patients have a distinct neurodevelopmental trajectory and that a larger amygdala volume may be associated with greater chances of remission.
The unaffected BD offspring included in this study were significantly younger than HC and affected BD offspring. Although the Pubertal Development Scale scores were comparable across groups, this age difference may indicate that our participants were at different stages of physical and brain development. Indeed, studies on the brain maturation of healthy children and adolescents show that the growth trajectory of the amygdala correlates positively with both pubertal and chronological age (57). While in females the volume of the amygdala has been found to increase in early puberty and then decrease at later pubertal stages, in males the amygdala volumes continue to increase until the end of puberty. Similar findings were observed in Bramen et al.’s study (58), in which gender and stage of physical sexual maturity were the best predictors of the volumes of the right hippocampus and the amygdala bilaterally. The authors argued that the positive association between sexual maturity and brain volumes could be related to the beneficial effects of pubertal hormone levels on biological processes underlying brain maturation, such as synaptic pruning, synaptogenesis and myelination (59). Further, it has been shown that while the caudate nucleus exhibits a progressive decrease in volume during puberty (60), the amygdala and the hippocampus (60) along with the frontal regions and the lenticular nuclei continue to mature during the adolescence and early adulthood (61). Unfortunately, to date, there is no longitudinal data on brain development in high-risk BD offspring. Thus, based on the typical trajectory of brain growth and the young age of the unaffected BD offspring, one would have expected to observe larger amygdalar volumes in HC and BD offspring with mood disorders. The enlargement in the right amygdala found in the unaffected BD offspring group is therefore surprising as it cannot be solely attributed to age and/or puberty-related brain changes. A longitudinal study investigating the changes in brain development in BD offspring is certainly needed to shed some light on the timing of the disruptions in brain maturation and their role in the development of BD.
It is important to take into account the young age of the unaffected BD offspring (10.50±3.37 years) in relation to their risk for BD. Indeed, Merikangas et al.’s study in 61,392 adults in 11 countries across Americas, Europe, and Asia showed that the onset of the BD spectrum disorders may occur anytime between the late teens and early 30s. Further, the majority of BD patients, in particular those of BD type I, have been found to develop the disease before the age of 25 (62, 63). Thus, one cannot exclude the possibility that the unaffected offspring included in this study will develop a mental illness in the next 10–15 years.
The lack of significant volumetric alteration in the amygdala of affected BD offspring compared to HC is intriguing. A possible explanation for this result is related to the psychotropic medication as it has been suggested to increase brain volumes in pediatric and adult populations with BD (64). Notably, in our study 36% of the participants (7 out of 19) was medicated. As such this variable may have influenced our results. Alternatively, the enlarged amygdala finding could be due to the fact that our cohort of affected BD offspring was heterogeneous and comprised individuals with BD and other mood disorders. To address this research question we compared the right amygdala volumes of unaffected offspring to those of offspring with BD and other mood disorders and found that unaffected BD offspring exhibited larger amygdala volumes compared to both groups of affected BD offspring and HC. Despite the small sample size of the 3 groups of BD offspring and the limited statistical power of this analysis this preliminary result is compelling as it supports the hypothesis that the size of the amygdala may be a marker of disease susceptibility in offspring of BD parents.
A strength of our study is certainly the consistence and reliability of the psychiatric diagnostic process across study sites. Further, affected and unaffected BD offspring were unrelated. The latter factor excludes possible bias related to the non-independence of observations due to nested sampling. For instance, in Hajek et al.’s 2009 study healthy BD offspring exhibited a larger caudate nucleus compared with HC. However, when the authors corrected the analyses for non-independence of sample observations (due to the inclusion of multiple individuals belonging to the same family), the results did not reach statistical significance (65). Additionally, in our study, unaffected offspring were drug-naïve and free from comorbidities or illnesses on separate diagnostic axes and affected BD offspring were characterized by a relatively short illness duration. Moreover, although we scanned participants at UNC and UTHSCSA, the MRI scanners were of same strength and manufacturer. From a statistical point of view, post-hoc power analyses showed that with a sample of 82 subjects we had sufficient power (94%) to detect volumetric differences in the right amygdala (Table 2S). Thus, it is unlikely that the enlarged amygdalar volume observed in our unaffected BD offspring was due to a limited sample size. Furthermore, our study found that the volumes of striatal, hippocampal, cingulate, and temporal regions were comparable across groups. These findings are consistent with previous studies in high-risk individuals and children and adolescents with BD that show no significant differences in hippocampal volumes compared to healthy controls (42, 43, 66–68). Similarly, caudate volumes were reported to be normal in pediatric BD patients (27, 69).
Nethertheless, a potential limitation of the current study is related to the variety of psychiatric disorders in the affected BD offspring group. Owing to the cross-sectional nature of this study it is also unclear whether the abnormalities observed in unaffected BD offspring are genetically determined or rather due to transitory biological mechanisms (e.g. cascade of inflammatory processes (70), possibly preceding the onset of a psychiatric disease. As part of our methodology we corrected our analyses for potential confounding variables such as age, gender, ethnicity, testing site and intracranial volume. This statistical approach may have not been sufficient to correct for age-related brain changes as the association between age and brain growth is not always linear and differs across brain regions (71, 72). Further, some of these covariates (e.g. ethnicity) may account for a minimal proportion of the brain volume differences across groups. Thus, the inclusion of these variables in our statistical model may have reduced the statistical efficiency of our analyses. An alternative approach could have been to perform analyses on subsamples of HC and BD created by pairing each case with a control of the same age, sex and ethnicity. However, this method would have required a larger sample size to be able to screen out matching participants.
To the best of our knowledge this is the first surface-based MRI study that identified significant differences in the volume of the right amygdala between unaffected offspring and offspring with mood disorders. A future longitudinal study should investigate the trajectory of amygdala growth in BD offspring to understand the course of illness progression in high-risk individuals.
Supplementary Material
Highlights.
We used a whole-brain surface-based approach.
Unaffected BD offspring had larger amygdala volumes than affected BD offspring.
Unaffected BD offspring had larger amygdala volumes than healthy controls.
Amygdalar volumes may be markers of disease susceptibility in BD offspring.
Acknowledgments
We thank Dr Benson Mwangi for helpful discussions concerning this work.
Professor J. C. Soares has received grants/research support from Forrest, BMS, Merck, Stanley Medical Research Institute, NIH 69774 and has been a speaker for Pfizer and Abbott. Dr. Sanches has served on the speakers’ bureau for Astra Zeneca and has received research support from Janssen.
Role of the funding source
This work was supported by NIH grant 1R01MH69774 and Pat Rutherford, Jr Chair in Psychiatry at UTHealth.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures
Drs Bauer, Suchting, Green, El Fangary and Zunta-Soares have no conflicts of interest
Contribution
JCS, GZS and MS designed the study and collected the data. IB wrote the first draft of the manuscript and IB, NE, RS and CG undertook the statistical analyses. All authors contributed to and have approved the final manuscript.
Contributor Information
Isabelle E. Bauer, University of Texas Health Science Center at Houston, Department of Psychiatry and Behavioral Sciences, Houston, TX, United States.
Marsal Sanches, University of Texas Health Science Center at Houston, Department of Psychiatry and Behavioral Sciences, Houston, TX, United States.
Robert Suchting, University of Texas Health Science Center at Houston, Department of Psychiatry and Behavioral Sciences, Houston, TX, United States.
Charles E. Green, University of Texas Health Science Center at Houston, Department of Psychiatry and Behavioral Sciences, Houston, TX, United States.
Nadia M. El Fangary, University of Texas Health Science Center at Houston, Department of Psychiatry and Behavioral Sciences, Houston, TX, United States.
Giovana B. Zunta–Soares, University of Texas Health Science Center at Houston, Department of Psychiatry and Behavioral Sciences, Houston, TX, United States.
Jair C. Soares, University of Texas Health Science Center at Houston, Department of Psychiatry and Behavioral Sciences, Houston, TX, United States.
References
- 1.Mathers CD, Fat DM, Boerma J. World Health Organization; 2008. The global burden of disease: 2004 update. [Google Scholar]
- 2.Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. The Lancet. 2013;381(9878):1672–1682. doi: 10.1016/S0140-6736(13)60857-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Craddock N, Sklar P. Genetics of bipolar disorder. The Lancet. 2013;381(9878):1654–1662. doi: 10.1016/S0140-6736(13)60855-7. [DOI] [PubMed] [Google Scholar]
- 4.Kieseppa T, Tuulio-Henriksson A, Haukka J, Van Erp T, Glahn D, Cannon TD, et al. Memory and verbal learning functions in twins with bipolar-I disorder, and the role of information-processing speed. Psychological medicine. 2005;35(2):205–215. doi: 10.1017/s0033291704003125. [DOI] [PubMed] [Google Scholar]
- 5.McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Archives of general psychiatry. 2003;60(5):497–502. doi: 10.1001/archpsyc.60.5.497. [DOI] [PubMed] [Google Scholar]
- 6.Rasic D, Hajek T, Alda M, Uher R. Risk of Mental Illness in Offspring of Parents With Schizophrenia, Bipolar Disorder, and Major Depressive Disorder: A Meta-Analysis of Family High-Risk Studies. Schizophrenia bulletin. 2013;40(1):28–38. doi: 10.1093/schbul/sbt114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang K, Steiner H, Dienes K, Adleman N, Ketter T. Bipolar offspring: a window into bipolar disorder evolution. Biological psychiatry. 2003;53(11):945–951. doi: 10.1016/s0006-3223(03)00061-1. [DOI] [PubMed] [Google Scholar]
- 8.DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disorders. 2001;3(6):325–334. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- 9.Duffy A, Horrocks J, Doucette S, Keown-Stoneman C, McCloskey S, Grof P. The developmental trajectory of bipolar disorder. The British Journal of Psychiatry. 2013;204(2):122–128. doi: 10.1192/bjp.bp.113.126706. [DOI] [PubMed] [Google Scholar]
- 10.Lim CS, Baldessarini RJ, Vieta E, Yucel M, Bora E, Sim K. Longitudinal neuroimaging and neuropsychological changes in bipolar disorder patients: Review of the evidence. Neuroscience & Biobehavioral Reviews. 2013;37(3):418–435. doi: 10.1016/j.neubiorev.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Houenou J, Frommberger J, Carde S, Glasbrenner M, Diener C, Leboyer M, et al. Neuroimaging-based markers of bipolar disorder: evidence from two meta-analyses. J Affect Disord. 2011;132(3):344–355. doi: 10.1016/j.jad.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 12.Sassi RB, Brambilla P, Hatch JP, Nicoletti MA, Mallinger AG, Frank E, et al. Reduced left anterior cingulate volumes in untreated bipolar patients. Biological psychiatry. 2004;56(7):467–475. doi: 10.1016/j.biopsych.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Soares JC, Mann JJ. The anatomy of mood disorders—review of structural neuroimaging studies. Biological psychiatry. 1997;41(1):86–106. doi: 10.1016/s0006-3223(96)00006-6. [DOI] [PubMed] [Google Scholar]
- 14.Hajek T, Carrey N, Alda M. Neuroanatomical abnormalities as risk factors for bipolar disorder. Bipolar disorders. 2005;7(5):393–403. doi: 10.1111/j.1399-5618.2005.00238.x. [DOI] [PubMed] [Google Scholar]
- 15.Brambilla P, Nicoletti MA, Harenski K, Sassi RB, Mallinger AG, Frank E, et al. Anatomical MRI study of subgenual prefrontal cortex in bipolar and unipolar subjects. Neuropsychopharmacology. 2002;27(5):792–799. doi: 10.1016/S0893-133X(02)00352-4. [DOI] [PubMed] [Google Scholar]
- 16.Hajek T, Carrey N, Alda M. Neuroanatomical abnormalities as risk factors for bipolar disorder. Bipolar disorders. 2005;7(5):393–403. doi: 10.1111/j.1399-5618.2005.00238.x. [DOI] [PubMed] [Google Scholar]
- 17.Strakowski SM, Adler CM, Almeida J, Altshuler LL, Blumberg HP, Chang KD, et al. The functional neuroanatomy of bipolar disorder: a consensus model. Bipolar Disord. 2012;14(4):313–325. doi: 10.1111/j.1399-5618.2012.01022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma V, Menon R, Carr TJ, Densmore M, Mazmanian D, Williamson PC. An MRI study of subgenual prefrontal cortex in patients with familial and non-familial bipolar I disorder. Journal of affective disorders. 2003;77(2):167–171. doi: 10.1016/s0165-0327(02)00109-x. [DOI] [PubMed] [Google Scholar]
- 19.Wilke M, Kowatch RA, DelBello MP, Mills NP, Holland SK. Voxel-based morphometry in adolescents with bipolar disorder: first results. Psychiatry research. 2004;131(1):57–69. doi: 10.1016/j.pscychresns.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Ladouceur CD, Almeida JR, Birmaher B, Axelson DA, Nau S, Kalas C, et al. Subcortical gray matter volume abnormalities in healthy bipolar offspring: potential neuroanatomical risk marker for bipolar disorder? Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(5):532–539. doi: 10.1097/CHI.0b013e318167656e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hajek T, Cullis J, Novak T, Kopecek M, Blagdon R, Propper L, et al. Brain structural signature of familial predisposition for bipolar disorder: replicable evidence for involvement of the right inferior frontal gyrus. Biological psychiatry. 2012;73(2):144–145. doi: 10.1016/j.biopsych.2012.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hajek T, Gunde E, Slaney C, Propper L, MacQueen G, Duffy A, et al. Amygdala and hippocampal volumes in relatives of patients with bipolar disorder: a high-risk study. Canadian Journal of psychiatry. 2009;54(11):726–733. doi: 10.1177/070674370905401102. [DOI] [PubMed] [Google Scholar]
- 23.Hajek T, Novak T, Kopecek M, Gunde E, Alda M, Höschl C. Subgenual cingulate volumes in offspring of bipolar parents and in sporadic bipolar patients. European archives of psychiatry and clinical neuroscience. 2010;260(4):297–304. doi: 10.1007/s00406-009-0077-2. [DOI] [PubMed] [Google Scholar]
- 24.Hajek T, Gunde E, Bernier D, Slaney C, Propper L, Grof P, et al. Subgenual cingulate volumes in affected and unaffected offspring of bipolar parents. Journal of affective disorders. 2008;108(3):263–269. doi: 10.1016/j.jad.2007.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hajek T, Gunde E, Bernier D, Slaney C, Propper L, MacQueen G, et al. Pituitary volumes in relatives of bipolar patients. European Archives of Psychiatry and Clinical Neuroscience. 2008;258(6):357–362. doi: 10.1007/s00406-008-0804-0. [DOI] [PubMed] [Google Scholar]
- 26.Singh MK, DelBello MP, Adler CM, Stanford KE, Strakowski SM. Neuroanatomical characterization of child offspring of bipolar parents. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(5):526–531. doi: 10.1097/CHI.0b013e318167655a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang K, Karchemskiy A, Barnea-Goraly N, Garrett A, Simeonova DI, Reiss A. Reduced Amygdalar Gray Matter Volume in Familial Pediatric Bipolar Disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(6):565–573. doi: 10.1097/01.chi.0000159948.75136.0d. [DOI] [PubMed] [Google Scholar]
- 28.Singh MK, Chang KD. Brain Structural Response in Individuals at Familial Risk for Bipolar Disorder: A Tale of Two Outcomes. Biological psychiatry. 2013;73(2):109–110. doi: 10.1016/j.biopsych.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 29.Foland LC, Altshuler LL, Sugar CA, Lee AD, Leow AD, Townsend J, et al. Increased volume of the amygdala and hippocampus in bipolar patients treated with lithium. Neuroreport. 2008;19(2):221–224. doi: 10.1097/WNR.0b013e3282f48108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hajek T, Bauer M, Simhandl C, Rybakowski J, O'Donovan C, Pfennig A, et al. Neuroprotective effect of lithium on hippocampal volumes in bipolar disorder independent of long-term treatment response. Psychological medicine. 2013;44(3):507–517. doi: 10.1017/S0033291713001165. [DOI] [PubMed] [Google Scholar]
- 31.Mitsunaga MM, Garrett A, Howe M, Karchemskiy A, Reiss A, Chang K. Increased subgenual cingulate cortex volume in pediatric bipolar disorder associated with mood stabilizer exposure. Journal of child and adolescent psychopharmacology. 2011;21(2):149–155. doi: 10.1089/cap.2010.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Savitz J, Nugent AC, Bogers W, Liu A, Sills R, Luckenbaugh DA, et al. Amygdala volume in depressed patients with bipolar disorder assessed using high resolution 3T MRI: the impact of medication. Neuroimage. 2010;49(4):2966–2976. doi: 10.1016/j.neuroimage.2009.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaufman J, Birmaher B, Brent D, Rao U, Ryan N. Kiddie-Sads-present and Lifetime version (K-SADS-PL) Pittsburgh: University of Pittsburgh, School of Medicine; 1996. [Google Scholar]
- 34.First MB, Spitzer RL, Gibbon M, Williams JB. Clinician Version. Administration Booklet: American Psychiatric Pub; 2012. Structured Clinical Interview for DSM-IVo Axis I Disorders (SCID-I) [Google Scholar]
- 35.Young R, Biggs J, Ziegler V, Meyer D. A rating scale for mania: reliability, validity and sensitivity. The British Journal of Psychiatry. 1978;133(5):429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 36.Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17(2):117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- 37.Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis: I. Segmentation and surface reconstruction. Neuroimage. 1999;9(2):179–194. doi: 10.1006/nimg.1998.0395. [DOI] [PubMed] [Google Scholar]
- 38.Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33(3):341–355. doi: 10.1016/s0896-6273(02)00569-x. [DOI] [PubMed] [Google Scholar]
- 39.Han X, Jovicich J, Salat D, van der Kouwe A, Quinn B, Czanner S, et al. Reliability of MRI-derived measurements of human cerebral cortical thickness: the effects of field strength, scanner upgrade and manufacturer. Neuroimage. 2006;32(1):180–194. doi: 10.1016/j.neuroimage.2006.02.051. [DOI] [PubMed] [Google Scholar]
- 40.Whalley HC, Sussmann JE, Chakirova G, Mukerjee P, Peel A, McKirdy J, et al. The neural basis of familial risk and temperamental variation in individuals at high risk of bipolar disorder. Biological psychiatry. 2011;70(4):343–349. doi: 10.1016/j.biopsych.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 41.Brambilla P, Harenski K, Nicoletti M, Sassi RB, Mallinger AG, Frank E, et al. MRI investigation of temporal lobe structures in bipolar patients. Journal of Psychiatric Research. 2003;37(4):287–295. doi: 10.1016/s0022-3956(03)00024-4. [DOI] [PubMed] [Google Scholar]
- 42.Blumberg HP, Kaufman J, Martin A, Whiteman R, Zhang JH, Gore JC, et al. Amygdala and hippocampal volumes in adolescents and adults with bipolar disorder. Archives of General Psychiatry. 2003;60(12):1201–1208. doi: 10.1001/archpsyc.60.12.1201. [DOI] [PubMed] [Google Scholar]
- 43.DelBello MP, Zimmerman ME, Mills NP, Getz GE, Strakowski SM. Magnetic resonance imaging analysis of amygdala and other subcortical brain regions in adolescents with bipolar disorder. Bipolar disorders. 2004;6(1):43–52. doi: 10.1046/j.1399-5618.2003.00087.x. [DOI] [PubMed] [Google Scholar]
- 44.Chen BK, Sassi R, Axelson D, Hatch JP, Sanches M, Nicoletti M, et al. Cross-sectional study of abnormal amygdala development in adolescents and young adults with bipolar disorder. Biological Psychiatry. 2004;56(6):399–405. doi: 10.1016/j.biopsych.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 45.Durston S, Hulshoff Pol HE, Casey B, Giedd JN, Buitelaar JK, Van Engeland H. Anatomical MRI of the developing human brain: what have we learned? Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(9):1012–1020. doi: 10.1097/00004583-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 46.Bitter SM, Mills NP, Adler CM, Strakowski SM, DelBello MP. Progression of amygdala volumetric abnormalities in adolescents after their first manic episode. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(10):1017–1026. doi: 10.1016/j.jaac.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moorhead TW, McKirdy J, Sussmann JE, Hall J, Lawrie SM, Johnstone EC, et al. Progressive gray matter loss in patients with bipolar disorder. Biol Psychiatry. 2007;62(8):894–900. doi: 10.1016/j.biopsych.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 48.Delaloye C, Moy G, de Bilbao F, Weber K, Baudois S, Haller S, et al. Longitudinal analysis of cognitive performances and structural brain changes in late-life bipolar disorder. International journal of geriatric psychiatry. 2011;26(12):1309–1318. doi: 10.1002/gps.2683. [DOI] [PubMed] [Google Scholar]
- 49.Brambilla P, Harenski K, Nicoletti M, Sassi RB, Mallinger AG, Frank E, et al. MRI investigation of temporal lobe structures in bipolar patients. J Psychiatr Res. 2003;37(4):287–295. doi: 10.1016/s0022-3956(03)00024-4. [DOI] [PubMed] [Google Scholar]
- 50.Altshuler LL, Bartzokis G, Grieder T, Curran J, Jimenez T, Leight K, et al. An MRI study of temporal lobe structures in men with bipolar disorder or schizophrenia. Biological psychiatry. 2000;48(2):147–162. doi: 10.1016/s0006-3223(00)00836-2. [DOI] [PubMed] [Google Scholar]
- 51.Strakowski SM, DelBello MP, Sax KW, Zimmerman ME, Shear PK, Hawkins JM, et al. Brain magnetic resonance imaging of structural abnormalities in bipolar disorder. Archives of General Psychiatry. 1999;56(3):254–260. doi: 10.1001/archpsyc.56.3.254. [DOI] [PubMed] [Google Scholar]
- 52.Chang K, Karchemskiy A, Barnea-Goraly N, Garrett A, Simeonova DI, Reiss A. Reduced amygdalar gray matter volume in familial pediatric bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(6):565–573. doi: 10.1097/01.chi.0000159948.75136.0d. [DOI] [PubMed] [Google Scholar]
- 53.Noga JT, Vladar K, Torrey EF. A volumetric magnetic resonance imaging study of monozygotic twins discordant for bipolar disorder. Psychiatry research. 2001;106(1):25–34. doi: 10.1016/s0925-4927(00)00084-6. [DOI] [PubMed] [Google Scholar]
- 54.Karchemskiy A, Garrett A, Howe M, Adleman N, Simeonova DI, Alegria D, et al. Amygdalar, hippocampal, and thalamic volumes in youth at high risk for development of bipolar disorder. Psychiatry Research: Neuroimaging. 2011;194(3):319–325. doi: 10.1016/j.pscychresns.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McDonald C, Marshall N, Sham PC, Bullmore ET, Schulze K, Chapple B, et al. Regional brain morphometry in patients with schizophrenia or bipolar disorder and their unaffected relatives. American Journal of Psychiatry. 2006;163(3):478–487. doi: 10.1176/appi.ajp.163.3.478. [DOI] [PubMed] [Google Scholar]
- 56.Ivleva EI, Bidesi AS, Thomas BP, Meda SA, Francis A, Moates AF, et al. Brain gray matter phenotypes across the psychosis dimension. Psychiatry Research: Neuroimaging. 2012;204(1):13–24. doi: 10.1016/j.pscychresns.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goddings A-L, Mills KL, Clasen LS, Giedd JN, Viner RM, Blakemore S-J. The influence of puberty on subcortical brain development. Neuroimage. 2014;88:242–251. doi: 10.1016/j.neuroimage.2013.09.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bramen JE, Hranilovich JA, Dahl RE, Forbes EE, Chen J, Toga AW, et al. Puberty influences medial temporal lobe and cortical gray matter maturation differently in boys than girls matched for sexual maturity. Cerebral Cortex. 2011;21(3):636–646. doi: 10.1093/cercor/bhq137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sowell ER, Thompson PM, Tessner KD, Toga AW. Mapping continued brain growth and gray matter density reduction in dorsal frontal cortex: inverse relationships during postadolescent brain maturation. The Journal of Neuroscience. 2001;21(22):8819–8829. doi: 10.1523/JNEUROSCI.21-22-08819.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Toga AW, Thompson PM, Sowell ER. Mapping brain maturation. Trends in Neurosciences. 2006;29(3):148–159. doi: 10.1016/j.tins.2006.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sowell ER, Thompson PM, Holmes CJ, Jernigan TL, Toga AW. In vivo evidence for post-adolescent brain maturation in frontal and striatal regions. Nature neuroscience. 1999;2(10):859–861. doi: 10.1038/13154. [DOI] [PubMed] [Google Scholar]
- 62.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of general psychiatry. 2007;64(5):543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Akiskal HS. The prevalent clinical spectrum of bipolar disorders: beyond DSM-IV. Journal of clinical psychopharmacology. 1996;16(2):4S–14S. doi: 10.1097/00004714-199604001-00002. [DOI] [PubMed] [Google Scholar]
- 64.Phillips M, Travis M, Fagiolini A, Kupfer D. Medication effects in neuroimaging studies of bipolar disorder. American Journal of Psychiatry. 2008;165(3):313–320. doi: 10.1176/appi.ajp.2007.07071066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hajek T, Gunde E, Slaney C, Propper L, MacQueen G, Duffy A, et al. Striatal volumes in affected and unaffected relatives of bipolar patients–high-risk study. Journal of psychiatric research. 2009;43(7):724–729. doi: 10.1016/j.jpsychires.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 66.Chen BK, Sassi R, Axelson D, Hatch JP, Sanches M, Nicoletti M, et al. Cross-sectional study of abnormal amygdala development in adolescents and young adults with bipolar disorder. Biol Psychiatry. 2004;56(6):399–405. doi: 10.1016/j.biopsych.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 67.Hajek T, Gunde E, Slaney C, Propper L, MacQueen G, Duffy A, et al. Striatal volumes in affected and unaffected relatives of bipolar patients – high-risk study. Journal of Psychiatric Research. 2009;43(7):724–729. doi: 10.1016/j.jpsychires.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 68.Dickstein DP, Milham MP, Nugent AC, Drevets WC, Charney DS, Pine DS, et al. Frontotemporal alterations in pediatric bipolar disorder: results of a voxel-based morphometry study. Arch Gen Psychiatry. 2005;62(7):734–741. doi: 10.1001/archpsyc.62.7.734. [DOI] [PubMed] [Google Scholar]
- 69.Sanches M, Roberts RL, Sassi RB, Axelson D, Nicoletti M, Brambilla P, et al. Developmental abnormalities in striatum in young bipolar patients: a preliminary study. Bipolar Disord. 2005;7(2):153–158. doi: 10.1111/j.1399-5618.2004.00178.x. [DOI] [PubMed] [Google Scholar]
- 70.Berk M. Neuroprogression: pathways to progressive brain changes in bipolar disorder. The International Journal of Neuropsychopharmacology. 2009;12(04):441–445. doi: 10.1017/S1461145708009498. [DOI] [PubMed] [Google Scholar]
- 71.Lebel C, Walker L, Leemans A, Phillips L, Beaulieu C. Microstructural maturation of the human brain from childhood to adulthood. Neuroimage. 2008;40(3):1044–1055. doi: 10.1016/j.neuroimage.2007.12.053. [DOI] [PubMed] [Google Scholar]
- 72.Ziegler G, Dahnke R, Jancke L, Yotter RA, May A, Gaser C. Brain structural trajectories over the adult lifespan. Human brain mapping. 2012;33(10):2377–2389. doi: 10.1002/hbm.21374. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.