Abstract
Abuse and neglect in childhood are well-established risk factors for later psychopathology. Past research has suggested that childhood emotional abuse may be particularly harmful to psychological development. The current cross-sectional study employed multiple regression techniques to assess the effects of childhood trauma on adulthood depression and emotion dysregulation in a large sample of mostly low-income African Americans recruited in an urban hospital. Bootstrap analyses were used to test emotion dysregulation as a potential mediator between emotional abuse in childhood and current depression. Childhood emotional abuse significantly predicted depressive symptoms even when accounting for all other childhood trauma types, and we found support for a complementary mediation of this relationship by emotion dysregulation. Our findings highlight the importance of emotion dysregulation and childhood emotional abuse in relation to adult depression. Moving forward, clinicians should consider the particular importance of emotional abuse in the development of depression, and future research should seek to identify mechanisms through which emotional abuse increases risk for depression and emotion dysregulation.
Keywords: Emotional abuse, Emotion dysregulation, Depression
Abuse and neglect in childhood have been consistently linked to a range of mental health problems later in life. Childhood maltreatment is a risk factor for later depression, panic disorder, social phobia, generalized anxiety, substance abuse, posttraumatic stress disorder (PTSD), and personality disorders, to name a few (Bradley et al., 2008; Fossati, Madeddu, & Maffei, 1999; Johnson, Cohen, Brown, Smailes, & Bernstein, 1999; Medrano, Zule, Hatch, & Desmond, 1999; Safren, Gershuny, Marzol, Otto, & Pollack, 2002; Yehuda, Halligan, & Grossman, 2001). Given the well-established association between childhood maltreatment and later psychological problems, it is important to examine the specific pathways whereby early maltreatment increases risk. One way to do this is to look at the differential impacts of different types of maltreatment on subsequent development of psychopathology.
In examining particular types of childhood maltreatment, researchers have historically focused most on physical and sexual abuse and paid less attention to emotional abuse. Despite this relative lack of research on emotional abuse, there is growing evidence suggesting its importance relative to other abuse types with respect to various negative outcomes. For example, emotional abuse was the only type of childhood maltreatment that predicted women's unhealthy adult eating attitudes when controlling for neglect, physical abuse, and sexual abuse (Kent, Waller, & Dagnan, 1999). A large study of risk factors for relationship violence in undergraduates showed similar results, as childhood emotional abuse emerged as a stronger predictor of both perpetration and victimization compared with childhood physical abuse, sexual abuse, and domestic violence exposure (Berzenski & Yates, 2010). Furthermore, a cross-sectional study of young adults (Teicher, Samson, Polcari, & McGreenery, 2006) examined the effects of physical, sexual, and emotional abuse on several psychiatric measures. When the authors examined individuals who had experienced only one of these three abuse types, they found that exposure to only emotional abuse (specifically parental verbal aggression) was consistently strongly related with all outcome measures, especially dissociation.
Relative to other maltreatment types, emotional abuse in childhood has also been found to be a strong predictor of depression and depressive symptoms. For instance, in a large study of health maintenance organization members, childhood emotional abuse was a stronger predictor of recent and lifetime history of depressive disorders than every other adverse childhood experience examined, including physical and sexual abuse (Chapman et al., 2004). Similarly, one study showed that women healthcare professionals with a history of psychological abuse had significantly higher depression symptom scores compared with non-abused women (Ferguson & Dacey, 1997). In a sample of adult psychiatric outpatients, depression diagnoses were more strongly related to emotional abuse than to physical or sexual abuse (Gibb, Chelminski, & Zimmerman, 2007). Finally, in a sample of women presenting to a primary care practice, childhood emotional abuse and neglect were significant predictors of depressive symptoms, even after partialling out the variance accounted for by physical abuse, sexual abuse, and lifetime trauma exposure (Spertus, Yehuda, Wong, Halligan, & Seremetis, 2003). Taken together, these studies suggest emotional abuse is an important risk factor for depression.
Despite the growing literature suggesting a robust relationship between childhood emotional abuse and later mental health problems, potential mediators in this complex relationship are not well understood. Wright, Crawford, and Del Castillo (2009) propose that the link between childhood emotional abuse and later psychopathology can be understood in the context of attachment theory by examining negative schemas, damaging beliefs about the self and others that can arise as a result of such abuse. The authors found that some of these damaging beliefs, specifically schemas of vulnerability to harm, self-sacrifice, and defectiveness/shame, partially mediated the relationship between child emotional abuse and later symptoms of anxiety and depression. Similarly, a longitudinal study by Calvete (2014) using the same measure of maladaptive schemas showed that the relationship between depression scores and emotional bullying, which is another type of emotional maltreatment, was mediated by early maladaptive schemas, specifically disconnection/rejection, in a sample of adolescents.
In examining mechanisms whereby childhood abuse might increase risk for later depression, other studies have focused on particular negative cognitions and cognitive styles. Maciejewski and Mazure (2006) found in a case-control study that the association between childhood emotional abuse and adult onset depression was mediated by fear of criticism and rejection, a subtype of sociotropy that the authors found specifically mediated this relationship, while another subtype of sociotropy, preference for affiliation, did not. Another cognition, hopelessness, was found to be a mediator between childhood emotional abuse and depression in a longitudinal study of adolescents recruited in primary care offices (Courtney, Kushwaha, &Johnson, 2008).
Another possible mediator between emotional abuse in childhood and later depression is emotion regulation problems. The term emotion regulation can be ambiguous because different authors tend to use it in slightly different ways (Gross & Thompson, 2007), but one highly cited definition of emotion regulation is “the ability to respond to the ongoing demands of experience with the range of emotions in a manner that is socially tolerable and sufficiently flexible to permit spontaneous reactions as well as the ability to delay spontaneous reactions as needed” (Cole, Michel, & Teti, 1994, p. 76). Theory and research suggest that deficits in emotion regulation are both associated with and predictive of psychopathology, including depression (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Cole & Hall, 2008). A growing body of literature suggests that much of the capacity for emotion regulation develops early in life, in an interpersonal context; a caregiver and child experience synchronous emotional exchanges, regulating one another's emotional states (Feldman & Greenbaum, 1997). Based on converging evidence across studies and methodologies, the quality of these caregiver-child exchanges is thought to be an important determinant of the child's later ability to regulate his or her own emotions (see Cole, Martin, & Dennis, 2004, for a full discussion).
Within this context of caregiver sensitivity, childhood maltreatment, including emotional abuse, could constitute a rupture in the development of healthy emotion regulation abilities. Several studies indeed suggest that childhood maltreatment is associated with subsequent problems with emotion regulation (Alink, Cicchetti, Kim, & Rogosch, 2009; Burns, Jackson, & Harding, 2010; Maughan & Cicchetti, 2002). Shipman et al. (2007) found that there are differences in emotion regulation strategies between children of physically maltreating mothers and those with non-maltreating mothers. Compared with non-maltreating mothers, maltreating mothers provided less validation and emotion coaching and more invalidation during an interaction task in which they talked about emotionally arousing situations with their child. This relative lack of emotion socialization by the maltreating mothers mediated the relationship between maltreatment status and children's adaptive emotion regulation strategies. Maltreated children also showed more emotion dysregulation, specifically lability and negativity, than non-maltreated children.
As previously discussed, experiencing emotional abuse is often a strong predictor of later pathology relative to other types of maltreatment, and a few studies suggest this may also hold true in predicting emotion dysregulation. For example, emotional abuse was a stronger predictor of emotion regulation difficulties than both sexual and physical abuse in a sample of undergraduate women (Burns et al., 2010). In this sample, emotional abuse was notably also more strongly correlated with posttraumatic stress symptoms than both sexual and physical abuse. Another study suggested that emotional nonacceptance, a subtype of emotion dysregulation, was more strongly related to childhood emotional abuse than to sexual or physical abuse (Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007).
This relationship between childhood emotional abuse and emotion dysregulation maybe due to the quality of the emotional abuse, such that emotionally abusive interactions with caregivers foster impaired development of healthy regulatory strategies in abused children, and studies examining particular facets of these interactions have shown this to be the case. For example, Berlin and Cassidy (2003) found in a longitudinal study that mothers' self-reported control of their preschoolers' emotional expressiveness at baseline was related to both their child's attachment style and to their child's emotion regulation at follow up around two years later. In a task designed to elicit mild stress and emotional reactions, children whose mothers reported more control over the child's total emotional expressiveness were significantly less likely to share their sadness. Children with mothers reporting more control over positive expressiveness were less likely to express and share sadness, and those whose mothers reported more control over negative expressiveness were more likely to suppress their anger. In this way, there was a specificity to the effect of the quality of the mother's control of children's emotions relative to the child's expressiveness during the task at follow-up. The children's selected emotion regulation strategy during this task, either expression or suppression, was related to the mothers' control over the child's expressiveness earlier in life.
The specificity of type of emotional abuse in relation to later regulatory strategies was also shown in a study examining emotional invalidation (Krause, Mendelson, & Lynch, 2003). The authors showed that childhood emotional invalidation by parents, including punishment, minimization, and distress in response to negative emotion was associated with chronic emotional inhibition in adulthood. Participants with a history of such invalidation reported higher levels of ambivalence over emotional expression, thought suppression, and avoidant stress responses. Participants who experienced childhood emotional invalidation also reported higher levels of depression and anxiety. To the extent that emotionally abusive caregivers' responses to their children's emotions lead to unhealthy regulatory strategies (or inhibit the development of healthy strategies) in the abused as these studies suggest, emotional abuse necessarily constitutes a risk factor for emotion dysregulation. Based on these studies, there is growing evidence for the relationship among childhood emotional abuse, emotion dysregulation, and depression.
Knowing that emotional abuse and emotion dysregulation both relate to depression is only the first step in understanding their roles in the development of depression. The current study aimed to examine interrelationships among emotion dysregulation, childhood emotional abuse, and adult depression symptoms with validated measures in a mostly low-income, African American sample. Moreover, we sought to examine the potential mediating role of emotion dysregulation in the relationship between childhood emotional abuse and adult depression.
We hypothesized that childhood emotional abuse would be more strongly correlated with both depression scores and emotion dysregulation, relative to other forms of childhood trauma. Second, given the literature on the importance of childhood emotional abuse, we hypothesized that emotional abuse would be a significant predictor of depression in one predictive model and emotion dysregulation in another, even after accounting for four other childhood trauma types. In the model predicting depression, we hypothesized that emotional abuse would still significantly predict depression symptoms, even after accounting for emotion dysregulation. Third, we hypothesized that emotion dysregulation would mediate the relationship between childhood emotional abuse and adult depression symptoms. This would likely be a complementary mediation, similar to Baron and Kenny's partial mediation, per conventions established by Zhao, Lynch, and Chen (2010).
Method
Procedure
Participants in this study were recruited as part of the Grady Trauma Project, a 5-year NIH-funded study of risk and resilience factors related to PTSD (Binder et al., 2008; Bradley et al., 2008; Gillespie et al., 2009). Participants were recruited from the General Medical and Obstetric/Gynecological Clinics at a publicly funded, nonprofit healthcare system that serves a low-income population in Atlanta, Georgia. Interviewers approached participants waiting for appointments. Participants were read each question by a trained interviewer who recorded their responses onto a tablet computer. Participants thus completed a battery of self-report measures assessing trauma history, childhood abuse, and associated symptoms including emotion dysregulation and depression. All measures were obtained by verbal interview and the entire interview took 45–75 min to complete (dependent in large part on the extent of the participant's trauma history and symptoms). Each person was paid $15 for participation in this phase of the study. Eligibility requirements for the study included the ability to give informed consent, and written and verbal informed consent was obtained for all participants. All procedures in this study were approved by the Emory University's Institutional Review Board and the Grady Health Care System Research Oversight Committee. The presented data were collected between 2005 and 2013.
Participants
The sample included only participants who completed all measures relevant to our analyses, for a total of 3,902 study participants. The participants in the sample were predominantly women (68.9%) with ages ranging from 18 to 81 years (M = 39.34, SD = 13.76). The majority (92.7%) of participants were African American. The majority of the participants had a low income, with 33.8% reporting a household monthly income less than $500, 25.8% reporting a household monthly income between $500 and $1,000, 24.5% reporting a household monthly income between $1,000 and $2,000, and the remaining 12.3% reporting a household monthly income of $2,000 or higher. Compared with participants who did not complete all measures, those who did complete all three key measures were slightly more often men (30.93% vs. 25.45%), slightly younger (mean age 39.35 vs. 41.06), and very slightly more African American (93.24% vs. 92.52%). Those who completed all measures did not differ significantly from those who did not on level of income or education. As reported elsewhere (Gillespie et al, 2009), this sample reports a high level of childhood maltreatment and trauma exposure.
Measures
Childhood Trauma Questionnaire (CTQ; Bernstein et al, 2003). The CTQ is a 28-item self-report questionnaire that has shown acceptable reliability and validity in both clinical and community populations (Bernstein et al., 2003) and within the current population (Binder et al., 2008). Bernstein et al. (2003) found moderate levels of agreement between therapist observation ratings and CTQ scores (as high as .59 for physical abuse) and good internal consistency scores across a range of samples (physical abuse = 0.83–0.86, emotional abuse = 0.84–0.89, and sexual abuse = 0.92–0.95). In our sample, internal consistency scores were good (physical abuse = 0.81, physical neglect = 0.66, sexual abuse = 0.94, emotional abuse = 0.84, emotional neglect = 0.87). The CTQ has also shown adequate convergent validity in that CTQ scores significantly correlate with scores on the Childhood Trauma Interview (Bernstein, Fink, Handelsman, & Foote, 1994). The CTQ retrospectively measures frequency of childhood traumatic incidents classified into five categories: physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect. Trauma frequency ratings are made on a five-point Likert scale: never true, rarely true, sometimes true, often true, and always true. As such, childhood maltreatment frequency was measured continuously, yielding a total childhood trauma score and five subscores for each of the five categories.
Emotion Dysregulation Scale, short version [EDS; (Powers, Stevens, Fani, & Bradley, submitted for publication)]. The Emotion Dysregulation Scale, short version is a 12-item self-report scale adapted from the Emotion Dysregulation Scale (Bradley et al., 2011). This short version demonstrates good construct validity with the Emotion Dysregulation Scale (Powers, Stevens, Fani, & Bradley, submitted for publication). Items are scored on a 7-point Likert scale and assess domains of emotional experiencing (e.g., “Emotions overwhelm me,” “When I feel angry, I get really angry”), cognition (e.g., “When I'm upset, I have trouble seeing or remembering anything good about myself,” “When I'm feeling bad, I have trouble remembering anything positive; everything just feels bad”), and behavior (e.g., “When my emotions are strong, I often make bad decisions”). There is not a specific time-frame for this measure; rather, participants are instructed to “rate the extent to which the following items describe you.” This self-report measure of emotion dysregulation relates as expected to a range of psychopathology criterion variables including PTSD, substance abuse problems, depression, suicide history, and subjective sense of adaptive functioning (Bradley et al., 2011). This short version demonstrated high internal consistency in this sample (α = 0.94).
Beck Depression Inventory, Second Edition [BDI-II; (Beck, Steer, & Brown, 1996)]. The Beck Depression Inventory is a widely used, 21-item, self-report measurement of depressive symptoms. Each of the items measures the presence and severity of depressive symptoms that are rated on a scale from 0 to 3. In our sample, internal consistency across BDI items was high (α = 0.93).
Data analysis
These analyses were conducted with only the sample of individuals for whom there was complete data on the CTQ BDI, and EDS. Initial analyses included bivariate correlations between BDI scores, EDS scores, and all five CTQ subscores. Next, to test our hypothesis that relative to other childhood trauma types, emotional abuse would emerge as a strong predictor of emotion dysregulation and depression, we planned two hierarchical regressions with these two measures as outcome variables and all five CTQ subscales as predictors. In the final model predicting depression, we included emotion dysregulation scores to assess the impact of emotion dysregulation on depression when accounting for the effects childhood trauma.
To formally examine the role of emotion dysregulation as a potential mediator of the relationship between childhood emotional abuse and current depression symptoms, we planned a simple mediation analysis with bootstrapping techniques using a macro developed by Preacher and Hayes (2008; see http://afhayes.com/spss-sas-and-mplus-macros-and-code.html#indirect). This allowed us to generate 5,000 bootstrap samples to generate a 95% bias-corrected confidence interval of the indirect effect a × b. In our mediation analysis, the a path represented the path from childhood emotional abuse to emotion dysregulation, and the b path represented the impact of the mediator, emotion dysregulation, on depression. Output from the macro also included path c, the direct impact of childhood emotional abuse on adulthood depression, and c′, the impact of emotional abuse on depression when accounting for emotion dysregulation. The product of a × b represents the indirect effect, and if the confidence interval for this indirect effect calculated by the bootstrap analysis does not include zero, the indirect effect is significant and mediation is established. This approach does not assume normally distributed indirect effects, and for this and other reasons it is more powerful and more accurate in testing mediation than the commonly used Sobel test and causal steps approach (Hayes, 2009; Zhao et al., 2010). Our hypothesis required a mediation analysis using current depression symptoms as the target dependent variable and emotion dysregulation as the potential mediator. Importantly, this mediational analysis cannot confirm causality because of the cross-sectional nature of the data (Kraemer, Kiernan, Essex, & Kupfer, 2008).
Results
In this sample, 19.2% of participants reported a history of moderate or severe childhood emotional abuse, 20.2% reported mild emotional abuse, and the other 60.7% reported no history of childhood emotional abuse. Mean BDI scores in our sample were 13.81. The mean score on the EDS was 37.52. Correlations between emotion dysregulation scores, CTQ subscores, and BDI scores are presented in Table 1. Analyses confirmed several of our hypotheses. All variables were correlated, and, as predicted, childhood emotional abuse was moderately correlated with both current emotion dysregulation and current depression symptoms. Furthermore, emotional abuse was more strongly correlated with these outcome variables than every other childhood trauma type. Current emotion dysregulation and depression symptoms were also strongly correlated.
Table 1.
Correlations*** among childhood trauma types, depressive symptoms, and emotion dysregulation.
| Variable | n | M | SD | 1 – PA | 2 – PN | 3 – SA | 4 – EN | 5 – EA | 6 – BDI |
|---|---|---|---|---|---|---|---|---|---|
| 1. CTQ phyiscal abuse (PA) | 3,901 | 8.03 | 3.95 | – | |||||
| 2. CTQ physical neglect (PN) | 3,902 | 7.05 | 3.17 | 0.49 | – | ||||
| 3. CTQ sexual abuse (SA) | 3,899 | 7.61 | 4.94 | 0.47 | 0.36 | – | |||
| 4. CTQ emotional neglect (EN) | 3,902 | 9.15 | 5.02 | 0.54 | 0.63 | 0.41 | – | ||
| 5. CTQ emotional abuse (EA) | 3,902 | 8.76 | 4.71 | 0.68 | 0.56 | 0.52 | 0.68 | – | |
| 6. BDI total | 3,902 | 13.80 | 11.89 | 0.33 | 0.29 | 0.30 | 0.37 | 0.45 | – |
| 7. EDS total | 3,902 | 76.12 | 40.60 | 0.28 | 0.25 | 0.24 | 0.30 | 0.39 | 0.64 |
Note. CTQ= Childhood Trauma Questionnaire; BDI = Beck Depression Inventory; EDS = Emotion Dysregulation Scale.
All correlations were significant at p <.001.
Hierarchical multiple regression revealed that childhood emotional abuse was a significant predictor of both emotion dysregulation and depression (see Table 2). Consistent with our predictions, emotional abuse was still a significant predictor of depression even after accounting for emotion dysregulation and every other childhood trauma type. In predicting both depression and emotion dysregulation, neither physical abuse nor physical neglect was a significant predictor in the final models after accounting for emotional abuse and emotional neglect.
Table 2.
Hierarchical multiple regression predicting emotion dysregulation and depression.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| B (SE B) | β | B (SE B) | β | B (SE B) | β | B (SE B) | β | B (SE B) | β | |
| DV: emotion dysregulation (EDS) | ||||||||||
| Physical abuse | 1.10 (0.09) | 0.21*** | 0.86 (0.10) | 0.16*** | 0.63 (0.10) | 0.12 | 0.02 (0.11) | 0.00 | ||
| Physical neglect | 1.02 (0.12) | 0.15*** | 0.88 (0.12) | 0.13*** | 0.35 (0.13) | 0.05** | 0.16 (0.13) | 0.02 | ||
| Sexual abuse | 0.50 (0.08) | 0.12*** | 0.41 (0.08) | 0.10*** | 0.18 (0.08) | 0.04* | ||||
| Emotional neglect | 0.72 (0.09) | 0.17*** | 0.25 (0.09) | 0.06** | ||||||
| Emotional abuse | 1.40 (0.11) | 0.31*** | ||||||||
| R2 | .095 | .105 | .121 | .156 | ||||||
| F model | 204.86*** | 153.03*** | 133.58*** | 144.10*** | ||||||
| DV: depression symptoms (BDI) | ||||||||||
| Physical abuse | 0.75 (0.05) | 0.25*** | 0.56 (0.06) | 0.06*** | 0.38 (0.06) | 0.13*** | 0.02 (0.06) | 0.01 | 0.02 (0.05) | 0.01 |
| Physical neglect | 0.62 (0.06) | 0.17*** | 0.51 (0.07) | 0.14*** | 0.10 (0.17) | 0.03 | −0.01 (0.07) | 0.01 | −0.06 (0.06) | −0.02 |
| Sexual abuse | 0.40 (0.04) | 0.17*** | 0.33 (0.04) | 0.14*** | 0.20 (0.04) | 0.08*** | 0.14 (0.03) | 0.06*** | ||
| Emotional neglect | 0.55 (0.05) | 0.23*** | 0.27 (0.05) | 0.11*** | 0.20 (0.04) | 0.08*** | ||||
| Emotional abuse | 0.82 (0.06) | 0.33*** | 0.40 (0.05) | 0.16*** | ||||||
| Emotion dysregulation | 0.31 (0.01) | 0.54*** | ||||||||
| R2 | .128 | .149 | .178 | .217 | .466 | |||||
| F model | 286.48*** | 227.91*** | 210.13*** | 215.18*** | 566.10*** | |||||
Note. B = unstandardized regression coefficient; β = standardized regression coefficient.
p < .05.
p < .01.
p < .001.
To assess whether emotional abuse was a significantly stronger predictor of depression than other childhood trauma types, we examined 95% confidence intervals of betas for the relevant independent variables. In the final regression model, the 95% confidence intervals of the unstandardized betas for emotional abuse [0.30, 0.49] did not overlap with those for emotional neglect [0.11, 0.28] or sexual abuse [0.08, 0.21], indicating that childhood emotional abuse is significantly more strongly related to adulthood depression than all four other measured childhood trauma types. For physical abuse and neglect, 95% confidence intervals were not examined because they were not significant independent predictors of depression in the final model.
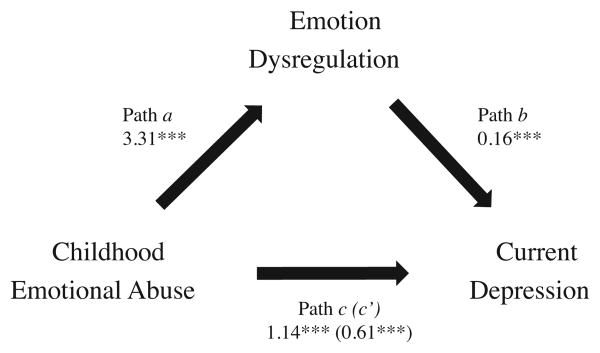
Because bivariate correlations and regression analyses confirmed the relationship of emotion dysregulation with both childhood emotional abuse and current depression symptoms, our analyses continued with the original hypothesized mediation model. The mediation model provided evidence supporting a mediation effect by emotion dysregulation on the relationship between childhood emotional abuse and current depression symptoms (see Fig. 1).
Fig. 1.
Mediation of relationship between childhood emotional abuse and current depressive symptoms through emotion dysregulation. Unstandardized coefficients are reported for each path. Path c′ is the effect of childhood emotional abuse on current depression while accounting for emotion dysregulation.
We found the mean indirect effect from the bootstrap analysis is positive and significant (a × b = 0.525), because the 95% confidence interval does not include zero [0.48, 0.55]. The direct effect c (1.14) is also significant (p <.001). Because a × b × c is positive (0.596), this is a complementary mediation, per conventions established by Zhao et al. (2010). The concept of a complementary mediation overlaps with (but is not perfectly analogous to) Baron and Kenny's (1986) partial mediation, as both the indirect and direct effects are significant in the model.
Discussion
This study examined the relationships among childhood emotional abuse, adulthood depression, and emotion dysregulation in a mostly low-income, African American sample. Results provided support for increased depression symptoms and increased emotion dysregulation as a function of childhood trauma, and analyses confirmed that emotion dysregulation may be one mechanism through which childhood emotional abuse increases risk for depression. Consistent with some previous literature, this study also provided support for the greater role of childhood emotional abuse compared to other early trauma types in its relationship with both emotion dysregulation and depression. Our findings indicate that taken together, emotion dysregulation and emotional abuse scores account for almost half the variance in current depressive symptoms.
The finding that emotional abuse is a stronger predictor of depression symptoms than other childhood trauma types, along with the finding (see Table 1) that emotional abuse scores are strongly correlated with every other childhood trauma type, is of particular significance, because these findings taken together suggest that emotional abuse may be a particularly impactful form of childhood trauma, and it may co-occur and often be inextricable from other types of childhood trauma. In light of these data, some of the negative effects attributed to physical and sexual abuse may possibly be shared with or even specific to emotional abuse. Our analyses (see Table 2) revealed an interesting example of this: when accounting for emotional abuse, neither physical abuse nor physical neglect was a significant predictor of depression or emotion dysregulation. These findings suggest that future research on the impacts of childhood trauma should include a measure of emotional abuse.
The finding that childhood trauma, particularly emotional abuse, is predictive of emotion dysregulation is of particular importance because emotional abuse is less studied than other abuse types in relation to emotion dysregulation. A body of previous research suggests that the relationship between early emotional abuse and later depression results from children's early experiences in the context of their caregivers which, when adaptive, foster development of healthy emotion regulation strategies or, when maladaptive, foster development of unhealthy regulatory strategies and emotion dysregulation (Cole et al., 2004; Feldman & Greenbaum, 1997; Gratz et al., 2007; Shipman et al., 2007). When cognitive and behavioral strategies are used by parents to regulate children's emotions in some way, there may be a specificity in the relationship between maladaptive strategies used by parents and those strategies used by the developing child.
Our finding that emotion dysregulation mediated the relationship between childhood emotional abuse and later depression adds to a growing literature on emotion dysregulation as a mechanism whereby early trauma can lead to later psychopathology. In one such study, a history of childhood emotional invalidation was associated with chronic emotional inhibition (Krause et al, 2003), which may be characterized as a maladaptive pattern of emotion regulation. This emotional inhibition in adulthood fully mediated the relationship between childhood emotional invalidation and depression and anxiety in adulthood. It may be that certain types of emotion regulation patterns arise from childhood emotional abuse, which in turn places individuals at risk for increased depression symptoms. It is unclear whether emotion dysregulation is truly an independent risk factor for depression, and because our data are cross-sectional, this study cannot answer this question. However, depressive episodes can be conceptualized as arising from problems with emotion dysregulation (Campbell-Sills & Barlow, 2007), and there is some preliminary evidence highlighting the importance of emotion regulation difficulties in those with a history of depression relative to those with no depression history (Ehring, Fischer, Schnülle, Bösterling, & Tuschen-Caffier, 2008). However, prospective studies are needed to assess the extent to which emotion dysregulation is an independent risk factor for depression, and which aspects of emotion dysregulation are most important in this relationship, because past research indicates that different qualities of emotionally abusive environments may lead to specific deficits in emotion regulation.
Importantly, childhood emotional abuse still significantly predicted depression symptoms even after accounting for emotion dysregulation, suggesting this is only one of potentially many mechanisms in that path. Thus, clinical work focusing on the effects of early abuse should target multiple problems stemming from that abuse, including but clearly not limited to emotion dysregulation. One example of such clinical work is dialectical behavior therapy (DBT), typically conducted with individuals diagnosed with borderline personality disorder (BPD), in whom childhood trauma histories are very common (Ball & Links, 2009). In DBT, one of the four modules is specifically dedicated to improving emotion regulation skills (Shearin & Linehan, 1994), and there is preliminary evidence that DBT may be effective in treating depression (Harley, Sprich, Safren, Jacobo, & Fava, 2008; Lynch et al., 2007). Based on our study and others showing the relationship between childhood emotional abuse and emotion dysregulation, this effect may be due in part to the emphasis on emotion regulation in DBT. Developing other therapies that target emotion dysregulation may be helpful for more than just depression, because difficulties with emotion regulation span psychopathologies (Aldao et al., 2010). Just as clinicians have adopted treatments to address multiple facets of complex, trauma-related pathologies, future researchers can focus on other potential mediators between early trauma and depression, while taking into account emotion dysregulation and perhaps in turn studying mechanisms whereby early trauma leads to emotion dysregulation.
There are several limitations of note in this study. Because these data are cross-sectional, no firm conclusions can be drawn about causality or time of onset of depressive symptoms or emotion regulation problems. Prospective, longitudinal studies are required to make claims about causality and temporal onset of emotion dysregulation and depression symptoms. Because the EDS is a relatively new measure, its use in this study may be seen as a limitation. However, given its correlation of 0.60 (p < .01) with the well-validated Difficulties in Emotion Regulation Scale (Powers et al., submitted for publication), we are confident that use of this measure should yield valid results. Because we used self-report measures in our study, issues of self-report bias may impact the findings. Participants may be prone to underreporting childhood trauma in particular (Widom & Morris, 1997; Widom & Shepard, 1996). In addition, the external validity of these findings may be limited due to the homogeneity of the present sample, which comprised mostly low-income African American individuals. However, it should be noted that our findings on emotional abuse and emotion dysregulation were strikingly similar to other findings which emerged from samples very different from ours demographically (e.g. Burns et al., 2010).
The homogeneity of this sample may also been seen as a strength of this study, given the preponderance of studies in this area whose samples are composed of participants who are primarily white, women, well-educated, or some combination thereof. Examining these important mental health factors in a largely African American sample is important because African American individuals may be less likely to seek specialty mental health treatment than other groups (Alegría et al., 2002) and at the same time be more likely to discuss problems related to mental health in general medical settings, such as primary care clinics (Cooper-Patrick et al., 1999). It is important for health professionals to be mindful of factors that maybe related to depression and other mental health problems, particularly for individuals who may be less likely to access mental health services.
The current study adds to a growing literature suggesting that emotional abuse is an important and perhaps underappreciated type of childhood maltreatment. One potential outcome of such abuse, emotion dysregulation, may partially explain the relationship between early emotional abuse and later depression. Given that childhood emotional abuse may be a stronger correlate of some negative outcomes than other abuse types, and given the relative dearth of research on emotional abuse, we suggest future research on childhood maltreatment include emotional abuse in analyses to avoid potential confounding variables. In the same way, clinicians should be cognizant of the various outcomes of childhood emotional abuse, with particular emphasis on improved emotion regulation as a potential goal of therapy. Finally, future research is warranted on emotion dysregulation in the context of many psychopathologies, as this and other studies have consistently shown it to be a robust correlate and predictor of mental health problems. With this information, the field may continue to identify the pathways from childhood maltreatment to adult psychopathology and guide treatment and research accordingly.
Acknowledgments
We thank the Grady Trauma Project research staff and coordinators, Allen W. Graham and Angelo Brown, as well as the nurses in the Clinical Research Network of Grady Health Systems.
Footnotes
This work was supported by funding from the National Institutes of Health (MH071537), the National Institute of Child Health and Human Development (MH018264), Howard Hughes Medical Institute, and the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR000454.
References
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, Ortega AN. Mental health care for Latinos: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatric Services. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alink LR, Cicchetti D, Kim J, Rogosch FA. Mediating and moderating processes in the relation between maltreatment and psychopathology: Mother–child relationship quality and emotion regulation. Journal of Abnormal Child Psychology. 2009;37:831–843. doi: 10.1007/s10802-009-9314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball JS, Links PS. Borderline personality disorder and childhood trauma: Evidence for a causal relationship. Current Psychiatry Reports. 2009;11:63–68. doi: 10.1007/s11920-009-0010-4. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. Manual for the Beck Depression Inventory. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Berlin LJ, Cassidy J. Mothers' self-reported control of their preschool children's emotional expressiveness: A longitudinal study of associations with infant–mother attachment and children's emotion regulation. Social Development. 2003;12:477–495. [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Desmond D. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Berzenski SR, Yates TM. A developmental process analysis of the contribution of childhood emotional abuse to relationship violence. Journal of Aggression, Maltreatment & Trauma. 2010;19:180–203. [Google Scholar]
- Binder EB, Bradley RG, Liu W, Epstein MP, Deveau TC, Mercer KB, Nemeroff CB. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. Journal of the American Medical Association. 2008;299:1291–1305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley B, DeFife JA, Guarnaccia C, Phifer J, Fani N, Ressler KJ, Westen D. Emotion dysregulation and negative affect: Association with psychiatric symptoms. Journal of Clinical Psychiatry. 2011;72:685–691. doi: 10.4088/JCP.10m06409blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R, Binder E, Epstein M, Tang Y, Nair H, Liu W, Newport D. Influence of child abuse on adult depression: Moderation by the corticotropin-releasing hormone receptor gene. Archives of General Psychiatry. 2008;65:190–200. doi: 10.1001/archgenpsychiatry.2007.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns EE, Jackson JL, Harding HG. Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment & Trauma. 2010;19:801–819. [Google Scholar]
- Calvete E. Emotional abuse as a predictor of early maladaptive schemas in adolescents: contributions to the development of depressive and social anxiety symptoms. Child abuse & neglect. 2014;38(4):735–746. doi: 10.1016/j.chiabu.2013.10.014. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross JJ, editor. Handbook of emotion regulation. NewYork, NY: Guilford Press; 2007. pp. 542–559. [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders. 2004;82:217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Cole PM, Hall SE. Emotion dysregulation as a risk factor for psychopathology. In: Beauchaine T, Hinshaw S, editors. Developmental psychopathology. Hoboken, NJ: Wiley & Sons; 2008. pp. 265–298. [Google Scholar]
- Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75:317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Cole PM, Michel MK, Teti LOD. The development of emotion regulation and dysregulation: A clinical perspective. Monographs of the Society for Research in Child Development. 1994;59(2–3):73–102. [PubMed] [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Powe NR, Steinwachs DM, Eaton WW, Ford DE. Mental health service utilization by African Americans and Whites: The Baltimore epidemiologic catchment area follow-up. Medical Care. 1999;37:1034–1045. doi: 10.1097/00005650-199910000-00007. [DOI] [PubMed] [Google Scholar]
- Courtney EA, Kushwaha M, Johnson JG. Childhood emotional abuse and risk for hopelessness and depressive symptoms during adolescence. Journal of Emotional Abuse. 2008;8:281–298. [Google Scholar]
- Ehring T, Fischer S, Schnülle J, Bösterling A, Tuschen-Caffier B. Characteristics of emotion regulation in recovered depressed versus never depressed individuals. Personality and Individual Differences. 2008;44:1574–1584. [Google Scholar]
- Feldman R, Greenbaum CW. Affect regulation and synchrony in mother-infant play as precursors to the development of symbolic competence. Infant Mental Health Journal. 1997;18:4–23. [Google Scholar]
- Ferguson KS, Dacey CM. Anxiety, depression, and dissociation in women healthcare providers reporting a history of childhood psychological abuse. Child Abuse & Neglect. 1997;21:941–952. doi: 10.1016/s0145-2134(97)00055-0. [DOI] [PubMed] [Google Scholar]
- Fossati A, Madeddu F, Maffei C. Borderline personality disorder and childhood sexual abuse: A meta-analytic study. Journal of Personality Disorders. 1999;13:268–280. doi: 10.1521/pedi.1999.13.3.268. [DOI] [PubMed] [Google Scholar]
- Gibb BE, Chelminski I, Zimmerman M. Childhood emotional, physical, and sexual abuse, and diagnoses of depressive and anxiety disorders in adult psychiatric outpatients. Depression and Anxiety. 2007;24:256–263. doi: 10.1002/da.20238. [DOI] [PubMed] [Google Scholar]
- Gillespie C, Bradley B, Mercer K, Smith A, Conneely K, Gapen M, Ressler K. Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry. 2009;31:505–514. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, Lejuez C. A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behavior Therapy. 2007;38:256–268. doi: 10.1016/j.beth.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Thompson RA. Emotion regulation: Conceptual foundations. Handbook of emotion regulation. 2007;3 [Google Scholar]
- Harley R, Sprich S, Safren S, Jacobo M, Fava M. Adaptation of dialectical behavior therapy skills training group for treatment-resistant depression. The Journal of Nervous and Mental Disease. 2008;196:136–143. doi: 10.1097/NMD.0b013e318162aa3f. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. [Google Scholar]
- Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Archives of General Psychiatry. 1999;56:600. doi: 10.1001/archpsyc.56.7.600. [DOI] [PubMed] [Google Scholar]
- Kent A, Waller G, Dagnan D. A greater role of emotional than physical or sexual abuse in predicting disordered eating attitudes: The role of mediating variables. International Journal of Eating Disorders. 1999;25:159–167. doi: 10.1002/(sici)1098-108x(199903)25:2<159::aid-eat5>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27:S101. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause ED, Mendelson T, Lynch TR. Childhood emotional invalidation and adult psychological distress: The mediating role of emotional inhibition. Child Abuse & Neglect. 2003;27:199–213. doi: 10.1016/s0145-2134(02)00536-7. [DOI] [PubMed] [Google Scholar]
- Lynch TR, Cheavens JS, Cukrowicz KC, Thorp SR, Bronner L, Beyer J. Treatment of older adults with co-morbid personality disorder and depression: A dialectical behavior therapy approach. International Journal of Geriatric Psychiatry. 2007;22:131–143. doi: 10.1002/gps.1703. [DOI] [PubMed] [Google Scholar]
- Maciejewski PK, Mazure CM. Fear of criticism and rejection mediates an association between childhood emotional abuse and adult onset of major depression. Cognitive Therapy and Research. 2006;30:105–122. [Google Scholar]
- Maughan A, Cicchetti D. Impact of child maltreatment and interadult violence on children's emotion regulation abilities and socioemotional adjustment. Child Development. 2002;73:1525–1542. doi: 10.1111/1467-8624.00488. [DOI] [PubMed] [Google Scholar]
- Medrano MA, Zule WA, Hatch J, Desmond DP. Prevalence of childhood trauma in a community sample of substance-abusing women. American Journal of Drug and Alcohol Abuse. 1999;25:449–462. doi: 10.1081/ada-100101872. [DOI] [PubMed] [Google Scholar]
- Powers A, Stevens J, Fani N, Bradley B. Construct validity of a short, self report instrument assessing emotional dysregulation. doi: 10.1016/j.psychres.2014.10.020. submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;4:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Safren SA, Gershuny BS, Marzol P, Otto MW, Pollack MH. History of childhood abuse in panic disorder, social phobia, and generalized anxiety disorder. Journal of Nervous and Mental Disease. 2002;190:453–456. doi: 10.1097/00005053-200207000-00005. [DOI] [PubMed] [Google Scholar]
- Shearin EN, Linehan M. Dialectical behavior therapy for borderline personality disorder: Theoretical and empirical foundations. Acta Psychiatrica Scandinavica. 1994;89(s379):61L–68. doi: 10.1111/j.1600-0447.1994.tb05820.x. [DOI] [PubMed] [Google Scholar]
- Shipman KL, Schneider R, Fitzgerald MM, Sims C, Swisher L, Edwards A. Maternal emotion socialization in maltreating and non-maltreating families: Implications for children's emotion regulation. Social Development. 2007;16:268–285. [Google Scholar]
- Spertus IL, Yehuda R, Wong CM, Halligan S, Seremetis SV. Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse & Neglect. 2003;27:1247–1258. doi: 10.1016/j.chiabu.2003.05.001. [DOI] [PubMed] [Google Scholar]
- Teicher M, Samson J, Polcari A, McGreenery C. Sticks, stones, and hurtful words: Relative effects of various forms of childhood maltreatment. American Journal of Psychiatry. 2006;163:993–1000. doi: 10.1176/ajp.2006.163.6.993. [DOI] [PubMed] [Google Scholar]
- Widom CS, Morris S. Accuracy of adult recollections of childhood victimization, part 2: Childhood sexual abuse. Psychological Assessment. 1997;9:34. [Google Scholar]
- Widom CS, Shepard RL. Accuracy of adult recollections of childhood victimization: Part 1. Childhood physical abuse. Psychological Assessment. 1996;8:412. [Google Scholar]
- Wright MOD, Crawford E, Del Castillo D. Childhood emotional maltreatment and later psychological distress among college students: The mediating role of maladaptive schemas. Child Abuse & Neglect. 2009;33:59–68. doi: 10.1016/j.chiabu.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Development and Psychopathology. 2001;13:733–753. doi: 10.1017/s0954579401003170. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37:197–206. [Google Scholar]