Abstract
Background
Initial orthograde root canal therapy (RCT) is used to treat dentoalveolar pathosis. The affect RCT has on pain intensity has been frequently reported, but the affect on other dimensions of pain has not. Also, the lack of large prospective studies involving diverse groups of patients and practitioners that are not involved in data collection suggest that there are multiple opportunities for bias to be introduced when this data is systematically aggregated.
Method
This prospective observational study assessed pain intensity, duration, and its interference with daily activities among RCT patients. Sixty-two practitioners (46 general dentists, 16 endodontists) in the National Dental Practice-Based Research Network enrolled patients requiring RCT. Patient reported data were collected before, immediately following, and one week after treatment using the Graded Chronic Pain Scale.
Results
Enrollment of 708 patients was completed over 6 months with 655 patients (93%) providing one-week follow-up data. Prior to treatment, patients reported a mean (±standard deviation) worst pain intensity of 5.3±3.8 (0-10 scale), 50% had “severe” pain (≥7), and mean days in pain and days pain interfered with activities were 3.6±2.7 and 0.5±1.2, respectively. Following treatment, patients reported a mean worst pain intensity of 3.0±3.2, 19% had “severe” pain, and mean days in pain and days with pain interference were 2.1±2.4 and 0.4±1.1, respectively. All changes were statistically significant (p<0.0001).
Conclusions
RCT is an effective treatment for patients experiencing pain, significantly reducing pain intensity, duration, and related interference. Further research is needed to reduce the proportion of patients reporting “severe” post-operative pain.
Keywords: Endodontics, Evidence-Based Dentistry, Root Canal, Research, Quality of Care, Postoperative Pain, Pain Measurement, Pain
Introduction
Initial orthograde root canal therapy (RCT) is a common dental procedure with estimates suggesting that more than 15 million are performed each year in the United States (1). Often RCT is used to address a patient's complaint of tooth pain (2). RCT has been demonstrated to be effective at addressing tooth-related disease, with 79-95% of technically measured outcomes being deemed successful (3, 4).
With pain as the outcome of interest, many researchers have used measures that combine subjective patient reports with behavioral actions and clinician-based observations (5). For example, endodontic flare-up has been defined as “pain or swelling or a combination of both”, occurring within “a few hours to a few days after…treatment,” and includes “…disruption of the patient's lifestyle, such that the patient initiates contact with the dentist” (6). While this outcome captures important information regarding practice-related burden, it does not adequately capture patient-centered experiences, which is the most desirable outcome to measure in dentistry (7) and is standard in pain-related research (8).
There have been a number of studies that have reported on change in pain intensity associated with RCT (9-13), as well as several reviews (5, 14). These studies include the use of a variety of pain intensity measures and post-treatment time points, thus providing robust results on this topic. Taken at face value this would suggest that further research on the topic is not needed, but the studies within this body of literature have multiple limitations that inhibit generalizability of the results to community practice. Examples of these limitations include small numbers of patients (15), single site designs (16), conducted in an academic institutional setting (12), care provided by a limited number of dentists (17), analyses that include more than one endodontic procedure per person (9), subjective data collected by the treatment provider (18), and ambiguous reporting of study methodologies (19). Since aggregating data from multiple studies with limitations has the potential to introduce significant biases (20, 21), there is the need to perform large well-conducted prospective observational studies to address clinically meaningful outcomes to ascertain more accurate estimates of the effects of RCT. Furthermore, it is uncertain how other aspects of the pain experience are affected by RCT. Specifically, while multiple studies have reported on the effect that RCT has on the duration of pain following treatment, no studies have compared the effect RCT has on pain duration and interference in daily living by measuring these pain-related factors before and after treatment using standard methods. Measuring multiple dimensions of the pain experience provides greater insight about the problem (22) and provides corroborating evidence of the effect RCT has on the condition of interest. For these reasons, we conducted a large multi-site prospective observational study in a practice-based setting to assess the direction and magnitude of change, from the pre-operative to post-operative period, in pain intensity, pain duration, and pain-related interference in daily living associated with RCT.
Methods
Brief Overview of the Study
This research was conducted within the National Dental Practice-Based Research Network (23, 24); details are provided at http://nationaldentalpbrn.org/. The study methods have been previously reported (25) and pertinent points are presented below, conforming to STROBE guidelines. In brief, this prospective observational study included 62 member dentists (46 general practitioners [GP] and 16 endodontic specialists [ES]) from five geographical regions: Alabama/Mississippi, Florida/Georgia, Minnesota, Oregon/Washington, and Denmark/Sweden. Participating dentists from the network volunteered to conduct this study in their practices. Project staff met with each dentist to explain the study protocol. Dentists enrolled their patients seeking dental care over a 6-month period. Ethical review board approval from each region, as well as the University of Minnesota, was obtained prior to initiation of this research. Informed consent was obtained from patients and study procedures were in accordance with institutional oversight.
Patient Eligibility and Recruitment
Dentists approached consecutive eligible patients for participation in this study. Inclusion criteria were: i) patient age 19-70 years; and ii) having a permanent tooth requiring RCT. Exclusion criteria were: i) iatrogenic pulpal exposure (i.e., cases of carious pulp exposure were included); ii) patient previously enrolled in this study (i.e., each patient could contribute only 1 tooth to the study); iii) previous endodontic treatment that could make it uncertain whether pain was associated with the prior treatment or the study treatment; iv) obvious cognitive impairments (e.g., prior stroke with communication deficits, dementia, mental disability); v) inability to read, understand, and complete the baseline patient questionnaire provided in English (or one of two Scandinavian languages in Denmark/Sweden); and vi) anticipated lack of availability to provide six-month follow-up information. Participation was voluntary and refusal to participate did not impact care.
Data Collection
Data collection occurred 1) immediately before initiation of treatment to assess the pre-operative state, 2) immediately following treatment to assess the intra-operative experience, and 3) one week after treatment to assess the post-operative state. The Graded Chronic Pain Scale was used to measure pain intensity using a 0 (no pain) to 10 (pain as bad as could be) rating scale, as well as pain-related interference with daily activities using a 0 (no interference) to 10 (unable to carry on any activities) rating scale and days in the past week kept from usual activities (26). The original instrument was modified with the recall period being one week, to make the pre-operative and post-operative durations equal for comparison purposes.
All data were collected by confidential paper-based, standardized questionnaires. Patients completed pre-operative questionnaires in the dental office and were placed in a sealed envelope by the patient, to conceal their responses from the practitioner and others in the dental office. The patient's, together with the practitioner's questionnaires, were submitted by the dental office to each regional coordinator at least on a weekly basis. The one-week post-operative questionnaires were completed by patients away from the dental office and mailed to each regional coordinator. Data collection forms are available at http://nationaldentalpbrn.org/peer-reviewed-publications.php. In addition to the pain-related outcome measures listed above, these questionnaires collected information about patient, tooth, and procedure characteristics.
Statistical Procedures
Descriptive statistics (means, standard deviations (SDs), frequencies, proportions) were used to examine characteristics of the study population overall (Table 1). Changes in tooth pain intensity, days with tooth pain, and interference in daily life were determined based on the post-operative minus the pre-operative measure; thus positive values correspond to an increase in pain (days) over time and negative values with a decrease in pain (days) over time. Only patients reporting both pre-operative and post-operative data were included in these calculations. When more than one appointment was required to complete the RCT, the highest measure of pain intensity or number of days or level of interference reported across the appointments was assigned for the post-operative measure; taking medication for pain during the week after RCT was set to ‘yes’ if taken after any of the appointments. For pain ratings, the significance of the pre- to post-operative change was assessed using the one-sample paired t-test. Since this test assumes that the change is normally distributed, a nonparametric analog (signed rank test) was applied to the ranked data for confirmatory purposes to ensure that the results were not an artifact of the analysis method (data not shown). McNemar's test was used to assess the significance of the change for binary-scaled measures, such as whether or not a patient was taking medications for tooth pain. This approach takes into account that the proportions are not derived from independent samples, which introduces possible correlations between the pre- and post-operative measures.
Table 1. Patient, tooth, and procedure characteristics.
| Characteristic | Overall |
|---|---|
|
| |
| Patient-Related Characteristics | |
|
| |
| Mean (SD) age in years | 47.8 (13) |
| Number missing | 13 |
|
| |
| Female gender: n (%) | 409 (59) |
| Number missing | 10 |
|
| |
| Ethnicity: n (%) | |
| Hispanic/Latino | 29 (4) |
| Non-Hispanic/Latino | 663 (96) |
| Number missing | 16 |
|
| |
| Race: n (%) | |
| White | 633 (91) |
| Black/African American | 38 (5) |
| Other | 28 (4) |
| Number missing | 9 |
|
| |
| Highest level of education completed: n (%) | |
| <College degree | 340 (49) |
| College degree or more advanced degree | 359 (51) |
| Number missing | 9 |
|
| |
| Annual household income: n (%) | |
| <$30,000 | 105 (16) |
| >$30,000 | 570 (84) |
| Number missing | 33 |
|
| |
| Patient has dental insurance/third party coverage: n (%) yes | 571 (81) |
| Number missing | 6 |
|
| |
| Tooth-Related Characteristics | |
|
| |
| Maxillary tooth: n (%) | 417 (59) |
| Number missing | 0 |
|
| |
| Posterior tooth: n (%) | 631 (89) |
| Molar | 434 (69) |
| Premolar | 197 (31) |
| Number missing | 0 |
|
| |
| Bleeding present upon opening the pulp chamber: n (%) yes | 359 (51) |
| Number missing | 0 |
|
| |
| Swelling associated with tooth: n (%) yes | 67 (10) |
| Number missing | 13 |
|
| |
| Tooth exhibits radiolucency of endodontic origin: n (%) yes | 302 (43) |
| Number missing | 7 |
|
| |
| Pulpal endodontic diagnoses: n (%) * | |
| Necrotic pulp | 377 (54) |
| Normal pulp or reversible pulpitis | 68 (10) |
| Irreversible pulpitis | 257 (37) |
| Number missing | 6 |
|
| |
| Apical endodontic diagnoses: n (%) * | |
| Normal apical tissue | 163 (24) |
| Symptomatic apical periodontitis | 364 (54) |
| Asymptomatic apical periodontitis | 42 (6) |
| Acute apical abscess | 45 (7) |
| Chronic apical abscess | 57 (8) |
| Number missing | 37 |
|
| |
| Procedure-Related Characteristics | |
|
| |
| Practitioner type: n (%) | |
| General practitioner | 295 (42) |
| Endodontic specialist | 413 (58) |
| Number missing | 0 |
|
| |
| Number of appointments needed to complete the root canal treatment: n (%) | |
| 1 appointment | 559 (79) |
| 2 appointments | 143 (20) |
| 3 appointments | 6 (1) |
| Number missing | 0 |
|
| |
| Practitioner considered procedure significantly more difficult than typical RCTs performed in practice: n (%) | |
| Yes | 92 (13) |
| No | 616 (87) |
| Number missing | 0 |
|
| |
| Practitioner's impression of quality of local anesthesia during procedure: n (%) | |
| Excellent, patient felt nothing | 471 (67) |
| Adequate, patient experienced non-painful sensations | 128 (18) |
| Marginal, patient experienced some pain | 97 (14) |
| Less than marginal, patient experienced a lot of pain | 6 (1) |
| Number missing | 6 |
Total percentage does not equal 100% due to rounding
All analyses were performed using the SAS software system, version 9.2. An alpha of 0.05 was used in assessing statistical significance. No imputation for missing values was undertaken.
Results
Patient, tooth, and procedure characteristics
The study sample comprised 708 patients, of which 655 (93%) provided 1-week post-operative data. The mean (±SD) age was 47.8±13.0, with a range of 19 to 70 years (Table 1). Females made up 59% of the patients. The majority of participants were white (91%), college educated (51%), had annual household incomes of ≥$30,000 (84%), and had dental insurance (81%). Treated teeth were 59% maxillary and 89% posterior.
Changes in Pain Intensity
Mean (±SD) change in worst and average pain intensity was -2.3±4.4 and -2.2±3.5, respectively (p<0.0001) (Table 2). The proportion of patients reporting severe (≥7) for worst pain intensity was reduced by 31% (p<0.0001), while the proportion reporting no pain (intensity=0) increased by 15% (p<0.0001); the results for current and average pain intensity over the past week were similar to those for worst pain intensity.
Table 2. Changes in pain intensities, duration of pain, medication intake for pain, and pain interference.
| Measures related to tooth pain | Timing of Measure | p-value | ||
|---|---|---|---|---|
|
| ||||
| Pre-operative | Post-operative | Change in pain-related measure+ | ||
| Pain Intensity Measures | ||||
|
| ||||
| Mean (SD) of worst pain intensity over the past week | 5.3 (3.8) | 3.0 (3.2) | -2.3 (4.4) | <0.0001* |
| Number missing | 16 | 56 | 69 | |
|
| ||||
| Worst pain intensity over the past week was ≥7 on 0-10 scale: n (%) | 322 (50) | 124 (19) | -31% | <0.0001† |
| Number missing | 69 | 69 | 69 | |
|
| ||||
| Worst pain intensity over the past week was 0 on 0-10 scale: n (%) | 154 (24) | 250 (39) | 15% | <0.0001† |
| Number missing | 69 | 69 | 69 | |
|
| ||||
| Mean (SD) of average pain intensity over the past week | 4.1 (3.2) | 1.9 (2.3) | -2.2 (3.5) | <0.0001* |
| Number missing | 15 | 56 | 68 | |
|
| ||||
| Average pain intensity over the past week was ≥7 on 0-10 scale: n (%) | 175 (27) | 37 (6) | -22% | <0.0001† |
| Number missing | 68 | 68 | 68 | |
|
| ||||
| Average pain intensity over the past week was 0 on 0-10 scale: n (%) | 162 (25) | 284 (44) | 19% | <0.0001† |
| Number missing | 68 | 68 | 68 | |
|
| ||||
| Mean (SD) current pain intensity | 2.8 (2.9) | 0.9 (1.8) | -1.8 (3.1) | <0.0001* |
| Number missing | 14 | 56 | 66 | |
|
| ||||
| Current pain intensity was ≥7 on 0-10 scale: n (%) | 92 (14) | 20 (3) | -11% | <0.0001† |
| Number missing | 66 | 66 | 66 | |
|
| ||||
| Current pain intensity was 0 on 0-10 scale: n (%) | 231 (36) | 451 (70) | 34% | <0.0001† |
| Number missing | 66 | 66 | 66 | |
|
| ||||
| Duration of Pain and Medication Intake | ||||
|
| ||||
| Mean (SD) days with tooth pain in past week | 3.6 (2.7) | 2.1 (2.4) | -1.5 (3.4) | <0.0001* |
| Number missing | 9 | 61 | 69 | |
|
| ||||
| Medication was taken for pain in past week: n (%) yes | 380 (60) | 371 (58) | -1.4% | 0.55† |
| Number missing | 71 | 71 | 71 | |
|
| ||||
| Pain interference | ||||
|
| ||||
| Interfered with daily activities in the past week, 0-10/10: mean (SD) | 1.8 (2.6) | 0.9 (2.0) | -0.9 (2.9) | <0.0001* |
| Number missing | 10 | 58 | 67 | |
|
| ||||
| Interfered with recreational activities in the past week, 0-10/10: mean (SD) | 1.6 (2.6) | 0.7 (1.9) | -0.8 (2.7) | <0.0001* |
| Number missing | 11 | 58 | 67 | |
|
| ||||
| Interfered with work activities in the past week, 0-10/10: mean (SD) | 1.4 (2.5) | 0.6 (1.7) | -0.8 (2.6) | <0.0001* |
| Number missing | 12 | 58 | 68 | |
|
| ||||
| Mean (SD) of summary rating of interference in daily life in the past week, on a scale of 0-10 | 1.6 (2.4) | 0.8 (1.8) | -0.8 (2.6) | <0.0001* |
| Number missing | 16 | 58 | 72 | |
|
| ||||
| Mean (SD) days pain interfered with daily life in the past week, 0-7/7: | 0.5 (1.2) | 0.4 (1.1) | -0.2 (1.4) | 0.0061* |
| Number missing | 12 | 68 | 78 | |
Assessed using a paired t-test
Assessed using McNemar's test
Calculations for changes in pain included patients with pre-operative and post-operative data
The signed rank test, a nonparametric analog to the paired t-test, was applied for confirmatory analyses. All results were similar and did not change the statistical significances observed (data not shown).
Change in worst pain intensity was examined by subgroups defined on the basis of their pre-operative pain levels. The plots report the proportions with specific changes, from a maximum decrease of -10 to a maximum increase in pain of +10 (Figure 1). In general, the majority of study participants experienced a decrease in pain intensity from the pre- to post-operative period, with relatively small proportions in each subgroup experiencing an increase in pain. Approximately 47% of the subgroup with no pre-operative pain experienced an increase in pain, although it was mild to moderate for most (78%). On average, patients with pre-operative pain intensities of ≥4 experienced considerable reductions in pain, while those with “mild” pain (1-3) had no change and those with no pre-operative pain experienced a modest but significant increase in pain (Table 3).
Figure 1. Plots Depicting Changes of Worst Pain Intensities Associated with RCT.
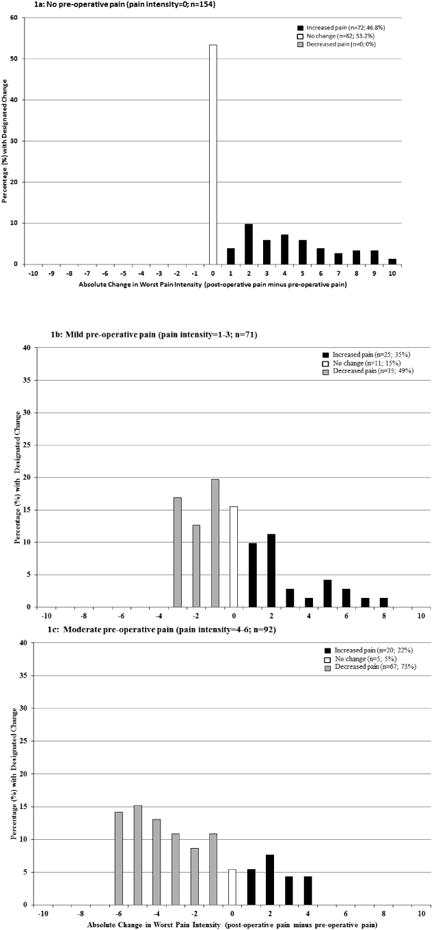
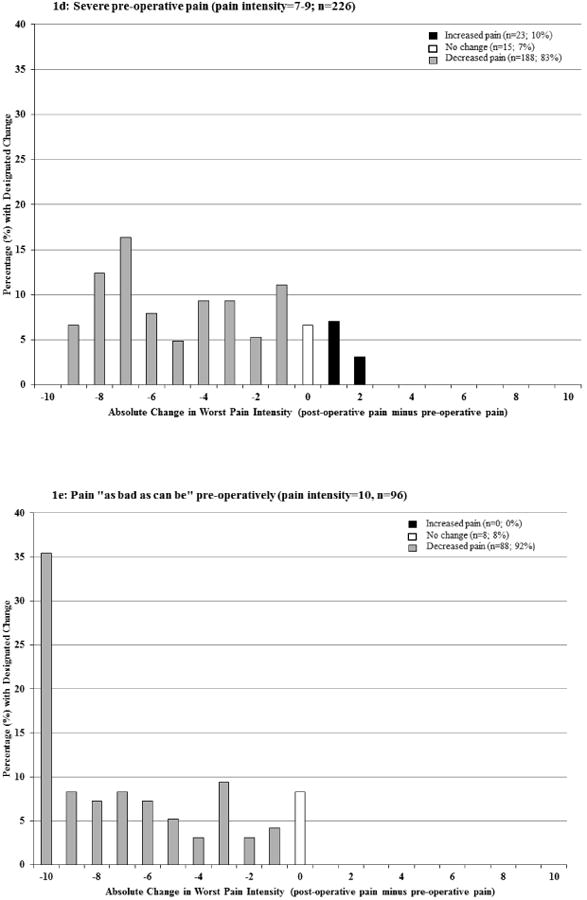
Table 3. Changes worst pain intensity overall and according to pre-operative worst pain intensity.
| worst pain intensity 1-week pre-operative | N | Mean (95% CI) Worst Pain Intensity | P-value* | ||
|---|---|---|---|---|---|
| Pre-operative | Post-operative | Change in pain intensity | |||
| 0 (None) | 154 | 0 (NA) | 2.1 (1.6, 2.5) | 2.1 (1.6, 2.5) | <0.0001 |
| 1-3 (Mild) | 71 | 2.1 (1.9, 2.3) | 2.2 (1.6, 2.8) | 0.1 (-0.5, 0.7) | 0.75 |
| 4-6 (Moderate) | 92 | 5.2 (5.0, 5.3) | 2.9 (2.3, 3.6) | -2.2 (-2.8, -1.6) | <0.0001 |
| 7-9 (Severe) | 226 | 8.0 (7.9, 8.1) | 3.8 (3.3, 4.2) | -4.2 (-4.6, -3.8) | <0.0001 |
| 10 (As bad as can be) | 96 | 10 (NA) | 3.3 (2.6, 4.0) | -6.7 (-7.4, -6.0) | <0.0001 |
| Overall | 639 | 5.3 (5.0, 5.6) | 3.0 (2.8, 3.2) | -2.3 (-2.6, -2.0) | <0.0001 |
NA=95% CI is not applicable since all pre-operative pain intensity measures in the category are a single fixed value with no variability; 69 participants were missing worst pain intensity information at the pre- and/or post-operative visit and excluded from this analysis.
Assessed using a paired t-test
worst pain intensity measured on a 0-10 scale, with 0 corresponding to no pain and 10 corresponding to pain “as bad as can be”; change in worst pain intensity was determined as worst post-operative pain minus worst pre-operative pain intensity.
The signed rank test, a nonparametric analog to the paired t-test, was applied for confirmatory analyses. All results were similar and did not change the statistical significances observed (data not shown).
Analyses of post-operative worst pain intensity according to practitioner type revealed no significant differences. Mean worst pain intensity was 3.2±3.3 for GP and 2.9±3.1 for ES (p=0.13); the proportion with “severe” pain intensity was 22% for GP and 18% for ES (p=0.23) (data not shown).
Duration of Pain and Pain-related Interference
Mean (±SD) change in number of days patients experienced tooth pain, from the week pre-operative to the week post-operative, was -1.5±3.4 (p<0.0001) (Table 2). Mean (±SD) change for interference in daily activities was -0.9±2.9 (p<0.0001), indicating that tooth pain interfered significantly less with daily activities post-operatively (Table 2).
Discussion
This study sought to observe the outcome of RCT in a large group of patients receiving care from a variety of community practice dentists that reflects typical endodontic care provided. This study's patient characteristics were similar to that of other large studies, suggesting that the sampling methods used in this study successfully captured a representative group of patients (25). Furthermore, there were high levels of patients consenting to participate, low levels of attrition, a high questionnaire return rate, and a large proportion of patients completing follow up. Together this supports the concept that our data are generalizable (i.e., high external validity) and that the study was well conducted (i.e., high internal validity), thus allowing us to make broad over-arching statements about treatment outcomes (27). We focused on the effect RCT has on the patient's pain, which is a patient-centered outcome of great importance (28-30) as a complement to the large body of evidence assessing technical outcomes (3, 4). While analyses by diagnoses or practitioner type are of great interest, they were beyond the scope of this study and are intended to be addressed in future publications.
Pain Intensity
Results show that RCT decreases pain intensity, whether assessing changes in proportions of patients according to specific levels of pain (i.e., “severe” or none) or the average intensity rated on a 0-10 point scale, consistent with meta-analysis results (14). The pre-operative proportion of patients with pain and their pain intensity was nearly identical to this meta-analysis; 81% with pain compared to our 76% (worst pre-operative pain >0) and mean pain intensity of 54 on a 0-100 point intensity scale compared to our 5.3 on a 0-10 point scale. Post-operative pain differed somewhat from our findings; 40% with pain compared to our 61% (worst post-operative pain >0) and mean pain intensity of 24 on a 0-100 point scale compared to our 3.0 on a 0-10 point scale.
Knowing about the outcome of “severe” post-operative pain is important because it is a major determinant of patient satisfaction (31, 32). The proportion of patients reporting “severe” (≥7) post-operative pain (19%) was considerably higher than previous reports (6, 17, 33, 34). Our study's measure of post-treatment pain relied solely on patient recall at one week following treatment, which would likely result in a higher report than measures that required both severe pain and contact with the dental office (6, 33). While this proportion of patients with “severe” post-operative pain is high and should be further studied in an effort to improve treatment outcomes, these data should be interpreted in the context that 50% of all patients had “severe” pre-operative pain. Unfortunately, similarly designed studies assessing pain intensity one week prior and one week following the RCT are not available to compare with these results.
Subgroup Analyzes for Pain Intensity
While overall averages identified statistically and clinically significant reductions in pain intensity, subgroup analyses were used to further elucidate the nature of these changes. Patients presenting with “moderate” to “severe” pain intensities, comprising nearly two-thirds of study patients, reported reductions in their pain intensity. In contrast, patients with “mild” pre-operative pain reported no significant change in pain intensity and those with no pain reported a modest increase in pain intensity. These subgroup differences have implications for treatment decisions in that patients could be better informed about their pain-related prognosis with RCT.
One possible reason for observed differences in RCT studies assessing pain intensity is practitioner type. Technical measures of RCT quality have been reported to be higher when practitioners have advanced training (35). Subgroup analysis comparing pain outcomes according to type of practitioner revealed no difference in worst post-operative pain intensity. This is consistent with the findings of Ng et al (11), who reported that practitioner type did not influence the prevalence of post-obturation pain. This data is difficult to interpret because the patients treated by endodontists are different from those treated by general dentists due to case selection by general dentists and patient preferences.
Pain Duration
We could not locate any articles assessing change in pain duration with RCT. Given that pain duration contributes to orofacial pain (36) and impacts patient reporting of other outcome measures (37), as well as serving as a measure of chronicity (38), its importance should not be overlooked. These results show a reduction in the number of days in pain from the week prior to RCT compared to the week after, which includes procedure-related inflammation. Duration of pain can also be seen as a measure of patient burden, in that pain may inhibit the ability to engage in daily activities, including work. Thus, it is not unexpected that, along with the decrease in the duration of post-treatment pain, we also found a decrease in pain-related burden.
Pain-related Interference
Interference on Patient's Activities
Pain-related interference with activities due to tooth pain has infrequently been studied (31, 39), which is surprising since it is considered a major contributor to quality of life and has been determined to be an important outcome to measure (40). Significant reductions in pain interference with daily activities, whether measured using a numerical scale or numbers of days, was observed. While an overall mean reduction of 0.2 days of interference does not appear large, it represents approximately five hours less interference above and beyond the recovery time experienced post-treatment. This is consistent with an earlier report showing improvement on quality of life measures (31).
Limitations
Pain intensity ratings were based on recall, which is subject to potential bias as a result of selective recall of past events. However, this is unlikely to have negatively impacted our results because the recall period was short, used the same length for both time periods (pre-operative and post-operative), and worst pain intensity is often best remembered (37). Furthermore, our study used post-operative minus pre-operative pain intensity as the outcome, an approach thought to be less sensitive to treatment effects when compared to measuring self-reported pain relief (37). Given that significant reductions in pain were consistently observed with different measures of pain intensity also suggests the results represent true treatment effects.
Daily post-operative pain intensity ratings were not obtained. Such data are important because of temporal changes in post-operative pain intensity, with the highest pain levels occurring 2 to 3 days after treatment (14). Such data would allow for comparison with existing literature.
Another limitation is not having standardized diagnoses for each patient, which have been observed to influence post-operative pain intensity (41). Feasibility constraints prohibited using radiographs or reliability training of practitioners. Therefore, pulpal and apical diagnoses were derived from clinical signs as reported by practitioners (Table 1).
Conclusions
The results demonstrated an overall therapeutic effect of reducing patient's pain intensity, duration, and related burden when receiving RCT in this practice-based research network, thus supporting RCT for the treatment of odontogenic pain in general clinical settings. In addition, the results demonstrated that 73% of patients with moderate pain, 83% of the patients with severe pain, and 92% of the patients with “pain as bad as it could be” had decreased pain following RCT, while 47% of the patients with no pain and 35% of the patients with mild pain had an increase in pain following RCT. Future publications exploring factors known to influence the outcome of RCT and investigating the relationships in subsets of the patients are planned.
Acknowledgments
Supported by National Institutes of Health grants K12-RR023247, U01-DE016746, U01-DE016747, and U19-DE022516. The second author thanks his thesis committee members Drs. Mike John, Eric Schiffman, and Jim Hodges for their mentoring, as well as Dr. John Look for his invaluable guidance. The authors declare that there are no conflicts of interest. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. Clinical Trial Number: NCT01201681
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Dental Association Survey Center. 2005-06 survey of dental services rendered. Chicago: American Dental Association; 2007. [Google Scholar]
- 2.Wolcott J, Rossman LE, Hasselgren G. Management of endodontic emergencies. In: Hargreaves KM, Cohen S, editors. Cohen's pathways of the pulp. 10th. St Louis: Mosby Elsevier; 2011. pp. 40–8. [Google Scholar]
- 3.Kojima K, Inamoto K, Nagamatsu K, Hara A, Nakata K, Morita I, et al. Success rate of endodontic treatment of teeth with vital and nonvital pulps. A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004 Jan;97(1):95–9. doi: 10.1016/j.tripleo.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int Endod J. 2011 Jul;44(7):583–609. doi: 10.1111/j.1365-2591.2011.01872.x. [DOI] [PubMed] [Google Scholar]
- 5.Sathorn C, Parashos P, Messer H. The prevalence of postoperative pain and flare-up in single-and multiple-visit endodontic treatment: A systematic review. Int Endod J. 2008 Feb;41(2):91–9. doi: 10.1111/j.1365-2591.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 6.Walton R, Fouad A. Endodontic interappointment flare-ups: A prospective study of incidence and related factors. J Endod. 1992 Apr;18(4):172–7. doi: 10.1016/S0099-2399(06)81413-5. [DOI] [PubMed] [Google Scholar]
- 7.Hujoel PP. Endpoints in periodontal trials: The need for an evidence-based research approach. Periodontol 2000. 2004;36:196–204. doi: 10.1111/j.1600-0757.2004.03681.x. [DOI] [PubMed] [Google Scholar]
- 8.Turk DC, Dworkin RH, Burke LB, Gershon R, Rothman M, Scott J, et al. Developing patient-reported outcome measures for pain clinical trials: IMMPACT recommendations. Pain. 2006 Dec 5;125(3):208–15. doi: 10.1016/j.pain.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 9.Genet JM, Wesselink PR, Thoden van Velzen SK. The incidence of preoperative and postoperative pain in endodontic therapy. Int Endod J. 1986 Sep;19(5):221–9. doi: 10.1111/j.1365-2591.1986.tb00482.x. [DOI] [PubMed] [Google Scholar]
- 10.DiRenzo A, Gresla T, Johnson BR, Rogers M, Tucker D, BeGole EA. Postoperative pain after 1- and 2-visit root canal therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002 May;93(5):605–10. doi: 10.1067/moe.2002.121900. [DOI] [PubMed] [Google Scholar]
- 11.Ng YL, Glennon JP, Setchell DJ, Gulabivala K. Prevalence of and factors affecting post-obturation pain in patients undergoing root canal treatment. Int Endod J. 2004 Jun;37(6):381–91. doi: 10.1111/j.1365-2591.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- 12.Torabinejad M, Shabahang S, Bahjri K. Effect of MTAD on postoperative discomfort: A randomized clinical trial. J Endod. 2005 Mar;31(3):171–6. doi: 10.1097/01.don.0000137642.50944.a2. [DOI] [PubMed] [Google Scholar]
- 13.Attar S, Bowles WR, Baisden MK, Hodges JS, McClanahan SB. Evaluation of pretreatment analgesia and endodontic treatment for postoperative endodontic pain. J Endod. 2008 Jun;34(6):652–5. doi: 10.1016/j.joen.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 14.Pak JG, White SN. Pain prevalence and severity before, during, and after root canal treatment: A systematic review. J Endod. 2011 Apr;37(4):429–38. doi: 10.1016/j.joen.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 15.Henry M, Reader A, Beck M. Effect of penicillin on postoperative endodontic pain and swelling in symptomatic necrotic teeth. J Endod. 2001 Feb;27(2):117–23. doi: 10.1097/00004770-200102000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Nusstein JM, Reader A, Beck M. Effect of drainage upon access on postoperative endodontic pain and swelling in symptomatic necrotic teeth. J Endod. 2002 Aug;28(8):584–8. doi: 10.1097/00004770-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Fava LR. Acute apical periodontitis: Incidence of post-operative pain using two different root canal dressings. Int Endod J. 1998 Sep;31(5):343–7. doi: 10.1046/j.1365-2591.1998.00159.x. [DOI] [PubMed] [Google Scholar]
- 18.Harrison JW, Baumgartner JC, Svec TA. Incidence of pain associated with clinical factors during and after root canal therapy. part 2. postobturation pain. J Endod. 1983 Oct;9(10):434–8. doi: 10.1016/S0099-2399(83)80259-3. [DOI] [PubMed] [Google Scholar]
- 19.Arslan H, Topcuoglu HS, Aladag H. Effectiveness of tenoxicam and ibuprofen for pain prevention following endodontic therapy in comparison to placebo: A randomized double-blind clinical trial. J Oral Sci. 2011 Jun;53(2):157–61. doi: 10.2334/josnusd.53.157. [DOI] [PubMed] [Google Scholar]
- 20.Savitz DA. Interpreting epidemiological evidence: Strategies for study design and analysis. New York, NY: Oxford University Press; 2003. Integration of evidence across studies; pp. 261–83. [Google Scholar]
- 21.Spangberg LSW. Systematic reviews in endodontics - examples of GIGO? Oral Surg Oral Med Oral Path Oral Rad and Endod. 2007;103(6):723–4. doi: 10.1016/j.tripleo.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 22.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Gilbert GH, Williams OD, Rindal DB, Pihlstrom DJ, Benjamin PL, Wallace MC, et al. The creation and development of the dental practice-based research network. J Am Dent Assoc. 2008 Jan;139(1):74–81. doi: 10.14219/jada.archive.2008.0024. [DOI] [PubMed] [Google Scholar]
- 24.Gilbert GH, Williams OD, Korelitz JJ, Fellows JL, Gordan VV, Makhija SK, et al. Purpose, structure, and function of the united states national dental practice-based research network. J Dent. 2013 Nov;41(11):1051–9. doi: 10.1016/j.jdent.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nixdorf DR, Law AS, Look JO, Rindal DB, Durand EU, Kang W, et al. Large-scale clinical endodontic research in the national dental practice-based research network: Study overview and methods. J Endod. 2012 Nov;38(11):1470–8. doi: 10.1016/j.joen.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992 Aug;50(2):133–49. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 27.Hulley SB, Newman TB, Cummings SR. Choosing the study subjects: Specification, sampling and recruitment. In: Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB, editors. Designing Clinical Research. 3rd. Philadelphia, PA: Lippincott, Williams & Wilkins; 2007. pp. 27pp. 27–36. [Google Scholar]
- 28.Cohen LA, Harris SL, Bonito AJ, Manski RJ, Macek MD, Edwards RR, et al. Coping with toothache pain: A qualitative study of low-income persons and minorities. J Public Health Dent. 2007;67:28–35. doi: 10.1111/j.1752-7325.2007.00005.x. [DOI] [PubMed] [Google Scholar]
- 29.Woolfolk MW, Lang WP, Borgnakke WS, Taylor GW, Ronis DL, Nyquist LV. Determining dental checkup frequency. J Am Dent Assoc. 1999 May;130(5):715–23. doi: 10.14219/jada.archive.1999.0282. [DOI] [PubMed] [Google Scholar]
- 30.Anderson R, Thomas DW. ‘Toothache stories’: A qualitative investigation of why and how people seek emergency dental care. Community Dent Health. 2003;20(2):106–11. [PubMed] [Google Scholar]
- 31.Dugas NN, Lawrence HP, Teplitsky P, Friedman S. Quality of life and satisfaction outcomes of endodontic treatment. J Endod. 2002 Dec;28(12):819–27. doi: 10.1097/00004770-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Gedney JJ, Logan H. Pain related recall predicts future pain report. Pain. 2006 Mar;121(1-2):69–76. doi: 10.1016/j.pain.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 33.Imura N, Zuolo ML. Factors associated with endodontic flare-ups: A prospective study. Int Endod J. 1995 Sep;28(5):261–5. doi: 10.1111/j.1365-2591.1995.tb00311.x. [DOI] [PubMed] [Google Scholar]
- 34.Eleazer PD, Eleazer KR. Flare-up rate in pulpally necrotic molars in one-visit versus two-visit endodontic treatment. J Endod. 1998 Sep;24(9):614–6. doi: 10.1016/S0099-2399(98)80122-2. [DOI] [PubMed] [Google Scholar]
- 35.Dugas NN, Lawrence HP, Teplitsky PE, Pharoah MJ, Friedman S. Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J. 2003 Mar;36(3):181–92. doi: 10.1046/j.1365-2591.2003.00640.x. [DOI] [PubMed] [Google Scholar]
- 36.Nixdorf DR, John MT, Wall MM, Fricton JR, Schiffman EL. Psychometric properties of the modified symptom severity index (SSI) J Oral Rehabil. 2010 Jan;37(1):11–20. doi: 10.1111/j.1365-2842.2009.02017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Haythornthwaite JA, Fauerbach JA. Assessment of acute pain, pain relief, and patient satisfaction. In: Turk DC, Melzack R, editors. Handbook of pain assessment. 2nd. New York: The Guilford Press; 2001. pp. 417–30. [Google Scholar]
- 38.Nixdorf DR, Drangsholt MT, Ettlin DA, Gaul C, De Leeuw R, Svensson P, et al. Classifying orofacial pains: A new proposal of taxonomy based on ontology. J Oral Rehabil. 2012 Mar;39(3):161–9. doi: 10.1111/j.1365-2842.2011.02247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gatten DL, Riedy CA, Hong SK, Johnson JD, Cohenca N. Quality of life of endodontically treated versus implant treated patients: A university-based qualitative research study. J Endod. 2011 Jul;37(7):903–9. doi: 10.1016/j.joen.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 40.Turk DC, Dworkin RH, McDermott MP, Bellamy N, Burke LB, Chandler JM, et al. Analyzing multiple endpoints in clinical trials of pain treatments: IMMPACT recommendations. initiative on methods, measurement, and pain assessment in clinical trials. Pain. 2008 Oct 31;139(3):485–93. doi: 10.1016/j.pain.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 41.Keiser K, Byrne BE. Endodontic pharmacology. In: Hargreaves KM, Cohen S, editors. Cohen's pathways of the pulp. 10th. St Louis: Mosby Elsevier; 2011. pp. 671–90. [Google Scholar]


