Abstract
Bouveret's syndrome is a rare cause of gastric outlet obstruction. Its diagnosis is often delayed or overlooked. It is characterized by the passage of a large gall bladder stone through a bilio-duodenal fistula, which becomes lodged in the duodenum causing duodenal obstruction. We report the case of a 70-year-old male with a history suggestive of gall bladder disease over a 1-year period. The diagnosis was confirmed by ultrasound, which showed a single large gall bladder stone and the patient was planned for elective laparoscopic cholecystectomy. One week prior to the elective surgery he presented with upper gastrointestinal bleeding for which he was admitted, diagnosed by a gastroenterologist as bleeding duodenal ulcer and treated by local epinephrine injection and blood transfusion. One week later he presented with a picture of acute gastric outlet obstruction, which proved by endoscopy to be due to a large stone impacted in the duodenum. Endoscopic management failed and the stone was managed by open surgery. The patient made a good postoperative recovery and for the last year he has remained free of symptoms.
Key words: Gallstone ileus, Bouveret's syndrome, Gastric outlet obstruction
Bouveret's syndrome describes gastric outlet obstruction caused by large gallstones that reach the duodenal bulb and get lodged there through a biliodigestive fistula. It is a rare and atypical variant of gallstone ileus that typically occurs in elderly patients with multiple medical comorbidities. Because of its rarity and atypical nature the diagnosis of Bouveret's syndrome is often delayed or overlooked.1,2 Being an overlooked diagnosis in a population of elderly individuals with comorbidities is the main reason behind the considerable morbidity and mortality associated with Bouveret's syndrome. The aim of reporting this case and following it by a brief overview of current diagnostic and therapeutic modalities is to heighten awareness of this overlooked clinical entity as a timely diagnosis and management. This heightened awareness is the key to improving prognosis.
Case Presentation
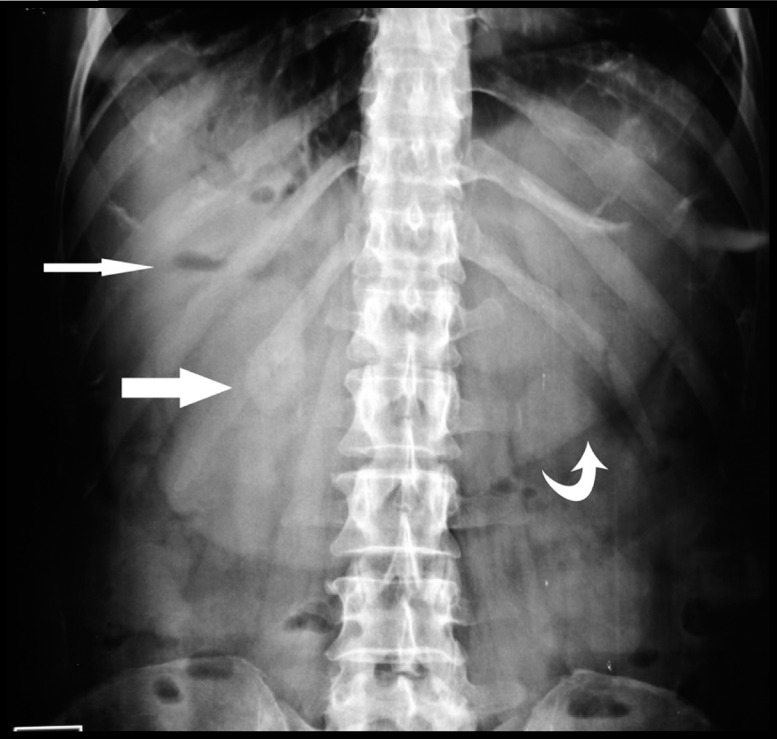
A 70-year-old male patient who is a known case of diabetes mellitus and hypertension presented to the outpatient surgical clinic complaining of recurrent attacks of biliary colic of 1-year duration. The diagnosis of cholelithiasis was confirmed by abdominal ultrasound that revealed a single large gallstone. The patient was then planned for elective laparoscopic cholecystectomy. A week prior to the date of his scheduled surgery he presented to the accident and emergency department with upper gastrointestinal bleeding and was in shock. He was promptly resuscitated with fluids and 2 units of packed red blood cells and admitted to the intensive care unit. Upper endoscopy was performed and the source of bleeding was identified as a duodenal ulcer that was managed by local epinephrine injection. Following successful management the patient was discharged and his gall bladder surgery postponed allowing for adequate recovery. Surprisingly, a few days after discharge he revisited the emergency department with a picture of gastric outlet obstruction. He reported vomiting anything he ate. The vomitus was nonbilious and consisted of undigested food. He did not report hematemesis and was severely dehydrated. The patient was resuscitated and admitted to the intensive care unit again. Gastric outlet obstruction in an elderly patient with comorbidities and known cholelithiasis raised the suspicion of Bouveret's syndrome. The patient's recent history of upper gastrointestinal bleeding could also be explained by this rare and atypical clinical entity, which might have been missed on the upper endoscopy performed at that time. A plain abdominal film revealed a radio-opaque shadow in the region of the duodenum along with pneumobilia (Fig. 1). An abdominal ultrasound revealed a thickened gall bladder containing sludge but devoid of the single large stone previously detected. The ultrasound also demonstrated the pneumobilia but did not show any evidence of common bile duct stones or any biliary dilatation. Because of these ultrasonic findings and the absence of liver enzymes abnormalities in a critically ill patient with mild renal impairment, contrast tomography (CT) scan and magnetic resonance cholangiopancreatography was not performed.
Fig. 1.
Ectopic gallstone (thick arrow), pneumobilia (thin arrow) and shadow of dilated stomach (curved arrow).
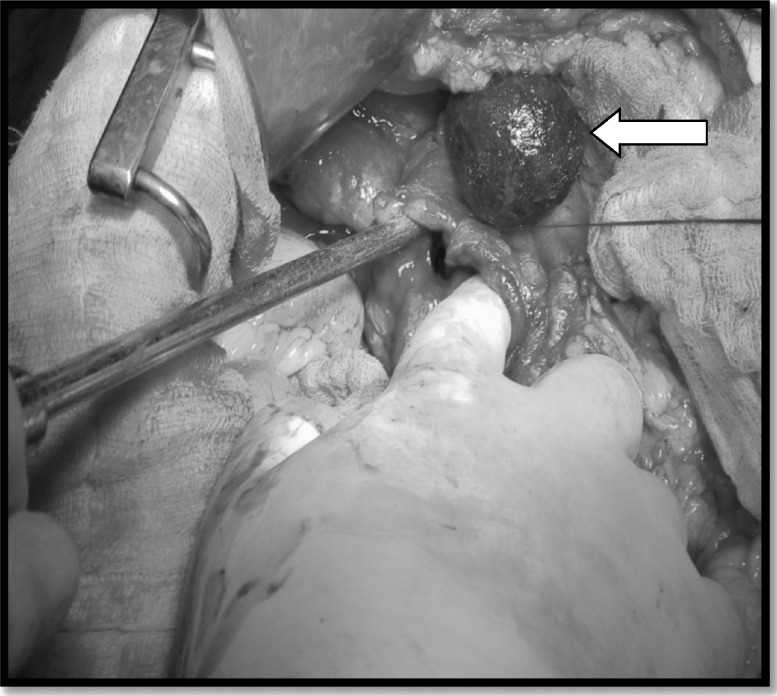
Upper endoscopy was then performed as both a diagnostic and therapeutic modality. It revealed a large, non-fleshy mass (representing the ectopic gallstone) completely obstructing the duodenum along with a dilated, fluid filled stomach. Endoscopic retrieval with mechanical lithotripsy failed and an open surgical approach was decided. Intraoperatively, the stone was found impacted in the first part of the duodenum extending to its second part and could not be milked neither proximally nor distally to be retrieved via a gastrostomy or jejunostomy respectively. It was, therefore, retrieved with difficulty through an anterior longitudinal duodenotomy (Fig. 2). The size of the extracted stone was 3.5 × 5.0 cm (Fig. 3). Inspection and palpation of the duodenum following stone extraction revealed a wide fistulous communication between the duodenum and gall bladder (Fig. 4). Taking into consideration the patient's age, comorbidities and poor functional status as well as the poor condition of local tissues in the acute inflammatory setting and the absence of additional gallstones simple stone extraction alone was performed. The postoperative course was uneventful and the patient was discharged on the seventh postoperative day. It has been a year now since his discharge and the patient has not experienced recurrent biliary symptoms. CT and contrast radiography performed 6 months after discharge both confirmed closure of the fistula.
Fig. 2.
Stone in the opened duodenum (arrow head) and gallbladder (arrow).
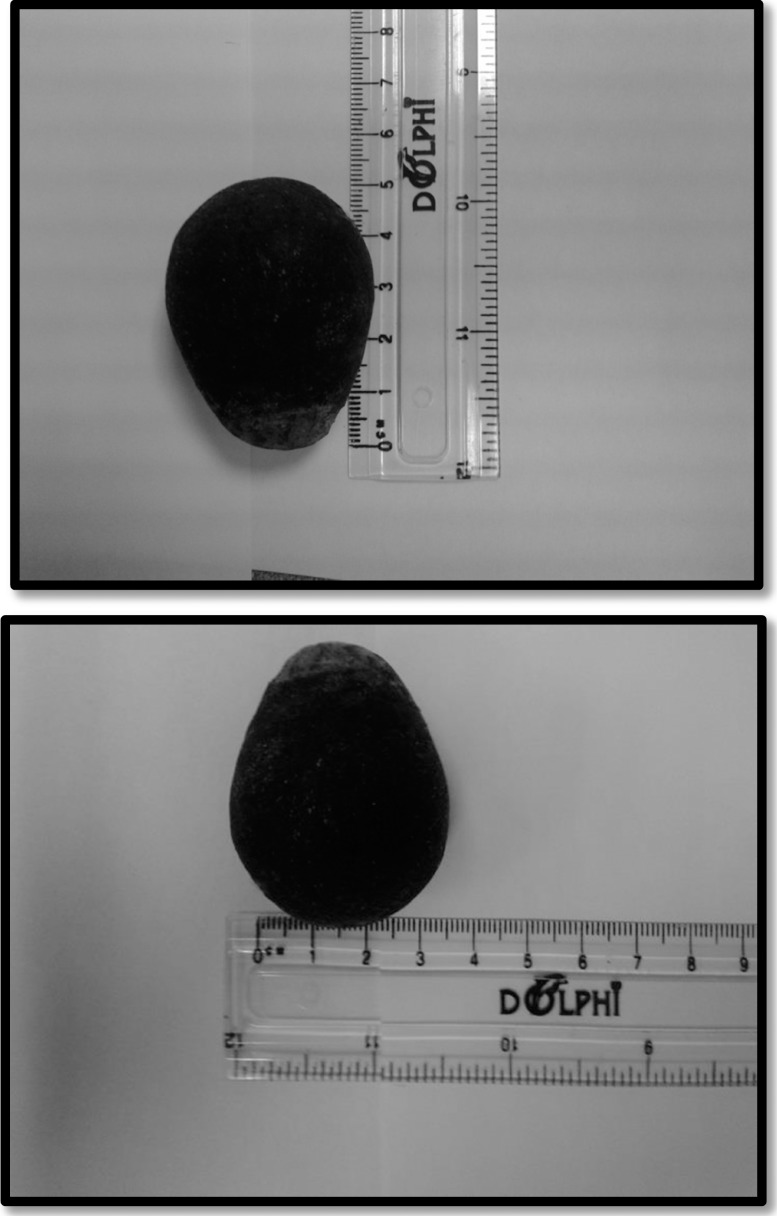
Fig. 3.
The extracted ectopic gallstone (5 × 3.5 cm).
Fig. 4.
The extracted stone (arrow). Index finger in the duodenum and the tip of suction pointing to the fistula between the duodenum and gall bladder.
Discussion
Bouveret's syndrome describes gastric outlet obstruction caused by large gallstones that reach the duodenal bulb and get lodged there through a biliodigestive fistula. Though the condition was first described in 2 patients at autopsy by Bonnet in 1841, it was not until 1896 that Leon August Bouveret made the first preoperative diagnosis of the condition, which, since then, bears his name.1
Mechanical obstruction of the gastrointestinal tract caused by gallstones that enter it via an acquired cholecystoenteric fistula (gallstone ileus) complicates 0.3%–0.5% of cholelithiasis cases. It usually follows an attack of acute cholecystitis that leads to the formation of adhesions between the gallbladder and the digestive tract which, in turn, allow pressure necrosis from large calculi to form a cholecystoenteric fistula.2
The vast majority of these stones pass spontaneously without producing obstruction. Stones that get stuck in the digestive tract are usually greater than 2–2.5 cm in diameter. Obstruction mostly occurs in the terminal ileum. Stones may also obstruct the proximal ileum, distal jejunum, colon and the duodenum or gastric outlet (Bouveret's syndrome) in decreasing order of frequency.2,3 Stones associated with Bouveret's syndrome are typically greater than 2.5 cm in size following the general rule that states: the larger the stone, the more proximal the obstruction.4
Bouveret's syndrome is a rare variant of gallstone ileus, accounting for 1–3% of cases. It is typically a disease of elderly females with a nonspecific clinical presentation, not limited to gastric outlet obstruction. There have been reports of patients presenting with acute pancreatitis, upper gastrointestinal bleeding, duodenal perforation, Borehaave's syndrome and gastric bezoars formation.5–11
The nonspecific presentation and rarity of Bouveret's syndrome are responsible for it often being labeled as an overlooked or delayed diagnosis. However, with a high index of clinical suspicion and the aid of appropriate imaging studies, the diagnosis is easier made. In about one-third of cases the diagnosis can be made by a plain abdominal film that demonstrates the classical Rigler's triad of a dilated stomach, pneumobilia, and a radio-opaque shadow in the region of the duodenum representing the ectopic gallstone.5,12 Rigler's triad was shown clearly in our case (Fig. 1). Serial plain films can also be useful, demonstrating a relative shift in the position of the shadow. This helps confirm the ectopic location of the gallstone. When such a change in position is demonstrated on serial X-rays of the abdomen, Rigler's triad becomes Rigler's tetrad.2 Ultrasonography can assess the condition of the gallbladder; demonstrate Rigler's triad and occasionally the biliodigestive fistula.2 Rigler's triad is clearly picked up on contrast-enhanced CT of the abdomen with the ectopic stone appearing as a filling defect in the duodenum. CT can also demonstrate the condition of the gallbladder and at times reveal the biliodigestive fistula. The identification of oral contrast in the gallbladder indirectly indicates the presence of a biliodigestive fistula.4 Contrast radiography, no longer used as a routine means of diagnosis being largely replaced by CT, can identify the level of obstruction and may also depict the biliodigestive fistula. However, it is still useful when CT is not available or contraindicated.2 Esophagogastroduodenoscopy (EGD) allows visualization of the impacted stone that appears as a hard non-fleshy mass along with a dilated stomach. The duodenal ostium of the biliodigestive fistula may also be seen.2,4 The importance of EGD in Bouveret's syndrome is related to it being of both diagnostic and therapeutic significance.13
The main therapeutic goal in dealing with Bouveret's syndrome is to remove the obstructing gallstone. Therapeutic options include both nonsurgical (endoscopic) and surgical (open or laparoscopic) approaches.14 Endoscopic retrieval of the obstructing gallstone with or without lithotripsy is an appealing option in a high risk population of elderly patients with comorbidities. Reported methods of lithotripsy include mechanical lithotripsy, laser lithotripsy, extracorporeal shockwave lithotripsy, and intracorporeal electrohydraulic lithotripsy. An important drawback of lithotripsy is that stone fragments may migrate and impact distally converting Bouveret's syndrome into distal gallstone ileus. Despite its low success rate (<10%), interventional endoscopy should always be attempted as a first line of management.15
The low success rate of endoscopic retrieval makes surgery the mainstay therapeutic option for Bouveret's syndrome. But the surgical strategy itself remains a controversial matter.14,15 Enterolithotomy or gastrostomy combined with cholecystectomy and closure of the fistula as a definitive 1- or 2-stage procedure is weighed against simple enterolithotomy or gastrostomy alone with cholecystectomy and fistula closure performed only if patients experience future symptoms. Advocates of the former fear the potential complications of a non-definitive biliary procedure. These include cholangitis, cholecystitis, recurrent ileus, gastrointestinal bleeding, and gallbladder carcinoma.12 Advocates of the latter argue that the need for a definitive biliary procedure may not arise due to the high likelihood of spontaneous closure of the fistula in the presence of a patent cystic duct and the absence of residual stones in the gallbladder. The literature has demonstrated that only 10% of patients require additional surgery for persistent biliary symptoms and has failed to provide evidence supporting the theoretical risk of developing carcinoma of the gallbladder with a persistent biliodigestive fistula.15 Furthermore, advocates of simple stone extraction consider a lengthy and/or possibly unnecessary procedure an invitation to additional “unnecessary” morbidity and mortality. The reported mortality rate associated with simple stone extraction is 12% whereas that associated with a definitive one stage procedure is 20% to 30%.14,16 On the other hand, proponents of a definitive biliary procedure do not attribute the considerable morbidity and mortality associated with Bouveret's syndrome to extended operative time but to 2 other main reasons: first is the elderly population with multiple medical comorbidities in which it typically occurs; second is the detrimental impact of the delay in diagnosing this rare and atypical clinical entity on the patient's general well-being.16
To date the literature does not favor a particular operative strategy for the management of Bouveret's syndrome. The operative strategy should be planned based on both patient-related factors and operative findings. The former includes the patient's age, comorbidities and general well-being. The latter includes the local inflammatory status (condition of the local tissue) and whether additional gallstones are present or not. A tailored surgical approach is, therefore, the key to successful management of Bouveret's syndrome.14–16
Our case clearly shows the atypical nature of Bouveret's syndrome and how easily it could be missed. Our patient first presented with upper gastrointestinal bleeding and the diagnosis of Bouveret's syndrome was overlooked. It seems that the profuse bleeding in the first endoscopy obscured the field and prevented the endoscopist from visualizing the stone and the biliodigestive fistula. Our experience with this case also supports adopting a tailored surgical strategy for the successful management of Bouveret's syndrome. We chose to perform simple stone extraction, which was followed by prompt symptomatic relief and an uneventful hospital stay. It has been 1 year since our patient was discharged and he has not experienced biliary symptoms. We believe that our operative strategy in this case of Bouveret's syndrome was appropriate.
Conclusion
Bouveret's syndrome is a rare and atypical clinical entity that continues to pose a great challenge for surgeons because of the considerable morbidity and mortality associated with it. The key to improving its prognosis is a timely diagnosis (based on a high index of suspicion) and a tailored management strategy.
References
- 1.Lawther RE, Diamond T. Bouveret's syndrome: gallstone ileus causing gastric outlet obstruction. Ulster Med J. 2000;69(1):69–70. [PMC free article] [PubMed] [Google Scholar]
- 2.Beuran M, Venter MD, Ivanov I, Smarandache R, Iftimie-Nastase I, Venter DP. Gallstone ileus–still a problem with heart. Annals of Academy of Romanian Scientists: Medical sciences. 2012;3(1):5–28. [Google Scholar]
- 3.Nuno-Guzman CM, Arroniz-Jauregui J, Moreno-Perez PA, Chavez-Solis EA, Esparza-Arias N, Hernandez-Gonzalez CI. Gallstone ileus: one-stage surgery in a patient with intermittent obstruction. World J Gastrointest Surg. 2010;2(5):172–176. doi: 10.4240/wjgs.v2.i5.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koulaouzidis A, Moschos J. Bouveret's syndrome. Narrative review. Ann Hepatol. 2007;6(2):89–91. [PubMed] [Google Scholar]
- 5.Rehman A, Hasan Z, Saeed A, Jamil K, Azeem Q, Zaidi A, et al. Bouveret's syndrome. J Coll Physicians Surg Pak. 2008;18(7):435–437. [PubMed] [Google Scholar]
- 6.Zafar A, Ingham G, Jameel JK. “Bouveret's syndrome” presenting with acute pancreatitis: a very rare and challenging variant of gallstone ileus. Int. J Surg Case Rep. 2013;4(5):528–530. doi: 10.1016/j.ijscr.2013.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mengual-Ballester M, Guillen-Paredes MP, Cases-Baldo MJ, Garcia-Garcia ML, Aguayo-Albasini JL. Gastrointestinal bleeding and bowel obstruction as a presentation of Bouveret' syndrome. Cir Cir. 2011;79(6):557–559. [PubMed] [Google Scholar]
- 8.Wonaga A, Fritz V, D'Alessandro M, Waldbaum C. Bouveret's syndrome: unusual cause of gastrointestinal bleeding. Acta Gastroenterol Latinoam. 2010;40(2):159–161. [PubMed] [Google Scholar]
- 9.Harthun NL, Long SM, Wilson W, Choudhury A. An unusual case of Bouveret's syndrome. Laparoendosc Adv Surg Tech A. 2002;12(1):69–72. doi: 10.1089/109264202753486975. [DOI] [PubMed] [Google Scholar]
- 10.Modi BP, Owens C, Ashley SW, Colson YL. Bouveret meets Boerhaave. Ann Thorac Surg. 2006;81(4):1493–1495. doi: 10.1016/j.athoracsur.2005.04.049. [DOI] [PubMed] [Google Scholar]
- 11.Tadros GM, Draganescu JM, Clarke LE, Alboronz MA. Intragastric gallstone-induced bezoar: an unusual cause of acute gastric outlet obstruction. South Med J. 2002;95(2):261–264. [PubMed] [Google Scholar]
- 12.Liew V, Layani L, Speakman D. Bouveret's syndrome in Melbourne. ANZ J Surg. 2002;72(2):161–163. doi: 10.1046/j.1445-2197.2002.02319.x. [DOI] [PubMed] [Google Scholar]
- 13.Trubek S, Bhama JK, Lamki N. Radiological findings in Bouveret's syndrome. Emergency Radiology. 2001;8(6):335–337. [Google Scholar]
- 14.Mavroeidis VK, Matthioudakis DI, Economou NK, Karanikas ID. Bouveret syndrome—the rarest variant of gallstone ileus: a case report and literature review. Case Rep Surg. 2013;2013:839370. doi: 10.1155/2013/839370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nickel F, Muller-Eschner MM, Chu J, Von Tengg-Kobligk H, Muller-Stich BP. Bouveret's syndrome: presentation of two cases with review of the literature and development of a surgical treatment strategy. BMC Surg. 2013;13(33ub) doi: 10.1186/1471-2482-13-33. 2013 Jun 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sica GS, Sileri P, Gaspari AL. Laparoscopic treatment of Bouveret's syndrome presenting as acute pancreatitis. JSLS. 2005;9(4):472–475. [PMC free article] [PubMed] [Google Scholar]