Abstract
Objective
Report lessons learned in an RCT of Stop My Smoking (SMS) USA, an mHealth smoking cessation program for young adult smokers.
Methods
164 18-24 year olds were recruited nationally, online in 2011. Program evaluation data was provided at 12-week post-Quit Day.
Results
1) First inviting participants to complete a brief text messaging survey and then asking them to complete a longer online survey resulted in the highest response rate (89%). 2) The positive tone of program messages was the most commonly noted program strength. 3) Suggested improvements included more social connectivity and additional assistance overcoming stressful situations. 4) Half of intervention participants moved through the program linearly and half went through various paths that reflected multiple relapses. Suggestions to use pharmacotherapy resulted in 22% of heavy smokers to utilize it.
Conclusion
Participant feedback provided concrete ways in which this and other young adult-focused interventions can improve messaging and program features to be even more salient.
Practice implications
Future young adult mHealth interventions could: Integrate models that are flexible to different “paths” of behavior change; address stressful life events directly and comprehensively; integrate proactive messaging that promotes pharmacotherapy options; and use text messaging as a gateway to longer online surveys.
Keywords: mHealth, smoking cessation, hard-to-reach populations, young adults, intervention features, text messaging
1. INTRODUCTION
Public health efforts to invigorate smoking cessation rates are needed [1], particularly for young adults who have higher rates of smoking and scant availability of tailored cessation services [2, 3]. One of the ways to do so may be to use technology that has been widely adopted by young adults - in essence, going where they “are” with evidence-based messaging. An estimated 92% of 18-24 year olds in the United States use text messaging, and send and receive a median number of 50 texts per day [4]. Intervention delivery via text messaging overcomes many structural challenges and access issues (e.g., lack of services, transportation, competing life demands) of traditional programs [5]. Text messaging-based programs are cost-effective: compared to the high personnel and infrastructure costs of in-person interventions, such programs are scalable and cost <2 cents per message. In contrast with other technologies such as the Internet, text messaging-based delivery may be superior because most young adults carry their cell phones with them everywhere, making intervention messages never far from reach. Messages are received automatically and do not require one to log on, making them more convenient and accessible.
To capitalize on the potential of technology-based smoking cessation programs to invigorate cessation rates among young adults, we developed and piloted Stop My Smoking (SMS) USA, a text-messaging based smoking cessation program for young adults in the United States. The 6-week program provided 2 weeks of “pre quit” messages that helped the person understand when and why they smoked and to begin to plan for alternative strategies when smoke free. The subsequent 4 weeks were aimed at helping the person stop smoking and remain abstinent. Intervention participants were asked at Day 2 and Day 7 post-Quit Day whether they had smoked a cigarette or not. Those who indicated they were still smoking were routed to messages that helped them address their relapse and recommit to smoking. Those who were abstinent moved on to messages that helped them remain smoke free. Alternative content was developed for the control group, which talked about improving one's fitness and sleep in order to help with the quitting process. Results from the pilot randomized controlled trial (RCT) of 164 participants 18-24 years of age suggest that intervention participants (39%) were significantly more likely than attention-matched control participants (21%) to have quit at 4-weeks post-quit day [6].
Emerging evidence supports text-messaging programs (mHealth) for health behavior change [7], including smoking cessation [8-10]. While data supporting mHealth program efficacy across a variety of health behaviors is emerging [7, 11], process information that reflects respondents’ experiences and that guides refinements of program features and protocols are lacking. To this end, the current manuscript builds upon prior findings by reporting the lessons learned from the implementation of the pilot RCT of SMS USA. Results examine: 1) the mHealth research implementation experience (e.g., which retention strategy would result in the highest response rate), 2) engagement with mHealth program features (e.g., feedback about the Text Buddy, a participant with whom the person was paired during the intervention to provide quitting support), and 3) suggested mHealth program improvements. Because little mHealth cessation research has been conducted with young adults, particularly those in non-academic settings, we also report: 4) quitting experiences of young adult smokers (e.g., quitting trajectories, noted barriers to quitting). Data will inform how mHealth programs can be used to target health behavior change among difficult to reach young adults.
2. METHODS
The research protocol was reviewed and approved by Chesapeake IRB and the Michigan State University IRB. Eligible participants were 18-25 years old, owned a cell phone, enrolled in an unlimited text messaging plan, smoked ≥24 cigarettes per week, seriously thinking of quitting in the next 30 days, agreed to smoking cessation status verification (e.g., by a friend), and completed the baseline survey.
Participants were recruited online, primarily through Craigslist [6]. Smokers expressed their interest by completing an online screener form. Eligible candidates were contacted via text message by the project coordinator to schedule an enrollment appointment, which occurred over the phone. On the call, eligibility was confirmed, study details were explained, and informed verbal consent was obtained. Participants then identified a quit day that was at least 15 days, but no more than 30 days from registration date. The project coordinator counseled all participants, irrespective of study arm, who smoked 10 cigarettes or more per day, to consider pharmacotherapy to assist in quitting. Participants were then randomized to the intervention (n=101) or attention-control (n=63) arm at a 2:1 ratio using a computerized adaptive randomization program that minimized the likelihood of imbalance on biological sex and level of smoking (i.e., light smokers (<20 cigs), heavy smoker (20+ cigs)).
After the enrollment call, participants were emailed a baseline survey website link and instructed to complete the online survey as soon as possible. Assessments were completed independently by participants at baseline (online), 4-weeks post-Quit Day (via text messaging), and 12-weeks post-Quit Day (online or text messaging). At 12-weeks post-Quit Day, all participants, both intervention and control, also completed a brief telephone survey with the project coordinator where they responded to open-ended questions about their program experience. Descriptive answers were typed into a data collection application. Technology functionality (e.g., pathing of participants from one stage to the next) was recorded by the software program.
Open-ended responses were compiled, sorted by study group, and summarized in Excel. The study authors independently reviewed all the responses and identified key themes for each question. Themes were counted and consistency noted across members. Study team members then discussed themes until agreement was achieved regarding the salient experiences of participants within their assigned condition (i.e., intervention or control). Descriptive statistics were used to detail the demographic characteristics of the sample. Comparisons of quantitative data were tested for statistical significance using chi-square tests.
3. RESULTS
3.1. Research implementation
Efficiency of recruitment
1,916 screeners were completed during the three-month recruitment period. For every 11 screeners completed, one person was successfully enrolled, at an average rate of 55 participants each month. Thirty-one percent of candidates who completed a screener appeared eligible (n=585), and 36% (n=211) were consented and randomized. One in five of these (n=47) failed to complete the required baseline survey and did not progress further.
A comparison of follow-up procedures to affect response rates
To test their effect on follow-up response rate, all participants (i.e., both control and intervention) were assigned to one of three data collection follow-up methods at 3-month post Quit Day (Table 1). Participants were assigned sequentially. Group 1 received: a) a text message invitation and link to complete the online survey; b) a $30 incentive; c) reminder telephone calls, texts, and emails; d) and an “early response” incentive of $10 for surveys completed within 48 hours. The same methods were employed in Groups 2 and 3. Additionally, Group 2 participants failing to complete surveys within 7-days were given a second opportunity to earn an additional $10 for surveys completed within 24 hours. Group 3 participants failing to complete surveys within 7 days were offered $10 to complete a brief, 10-item survey delivered via text messaging with the option to also complete the online survey
Table 1.
Different follow-up protocols and associated response rates among young adult smokers in the Stop My Smoking USA randomized controlled trial (n=164)
| Group | Sample size | Text messaging invitation | $30 incentive to complete the online survey | Reminder telephone calls, texts, emails | $10 48-hour early response incentive | 2nd $10 24-hour early response incentive in Week 2 | $10 to complete brief text messaging survey in Week 2 | Response rate |
|---|---|---|---|---|---|---|---|---|
| 1 | 54 | X | X | X | X | 74% | ||
| 2 | 55 | X | X | X | X | X | 78% | |
| 3 | 55 | X | X | X | X | X | 89% |
The program was evaluated in a randomized controlled study in 2011 with participants who were recruited online.
Group 3 had the highest survey completion rate across the three groups (89% versus 74% and 78%, respectively; p=0.12): Of the 24 people assigned to Group 2 who did not complete the survey in the first week, 2 (8%) completed the survey within 24 hours of receiving the second opportunity text. Of the 21 people assigned to Group 3 who did not complete the survey in the first week, 12 (57%) completed the brief text message survey in the second week. Ten of the 12 (83%) also went on to complete the online survey.
3.2. Engagement with program features
Preferred messages
As described elsewhere [12], eight different types of intervention messages were crafted: those that helped the person prepare to quit, described the benefits of quitting, provided coping strategies, discussed how to deal with discomforts and difficulties, provided general encouragement, encouraged NRT use, taught quitting skills, and addressed relapse. Intervention participants overwhelming shared that it was not just one message, but the encouraging, positive tone of the messages overall that was helpful. Based on intervention participant feedback, more useful messages were those that helped in preparation to quit (e.g., understanding their smoking behavior) and provided actionable suggestions on distractions from smoking (e.g., take a deep breath; drink water). Interestingly, however, a few participants shared that the supportive messages began to feel repetitive, even though no messages were actually duplicated. Unhelpful messages were those that reminded participants that they were quitting, and some participants mentioned that the program was itself a trigger: “All in all, [the] messages reminded me that I wasn't smoking, which made me want cigarettes more.”
Receiving messages in the morning and on a varied pattern throughout the day was seen as an effective way of reminding participants of their goal of quitting.
Perceived utility of the Text Buddy
Social support was encouraged with the use of a „Text Buddy’, another intervention participant that the person was paired with to provide text messaging support during the quitting process [9]. While some participants appreciated the experience, many reported problems with their buddy's availability, including being in different stages of the quitting process, different schedules, or in different time zones. Some participants were uncomfortable with the idea of a text buddy. Several suggested they already had sufficient support and, therefore, did not need a buddy.
3.3. Suggestions for program improvements
Intervention participants suggested adding more social connectivity such as: additional mechanisms for contacting telephone counselors, Facebook links, online material, voice contact with the text buddy, and chat rooms. Participants also wanted the program to be more personalized to their specific goals and issues. Some thought that the ability to pause the program (e.g., during a vacation) would be useful. Although a majority of participants wished the program was longer, equal percentages requested either more or less daily messages.
3.4. The young adult quitting experience
The quitting trajectory
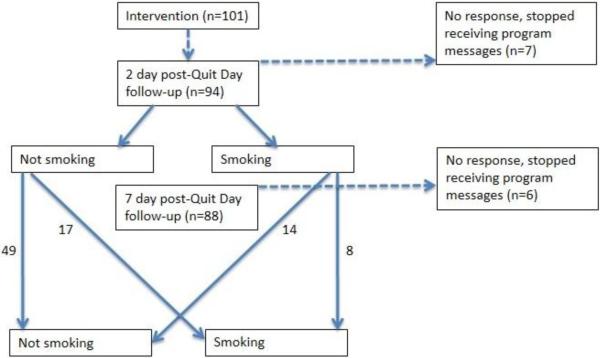
Intervention program content was tailored to meet the anticipated challenges that the person would be experiencing, based upon where the person was in the quitting process. For example, those who relapsed after their Quit Day received content focused on helping them get back on track and to recommit to quitting. To implement the tailoring, intervention participants responded to a smoking status question 2-days and again 7-days post-Quit Day (see Figure 1). Forty-nine percent reported not smoking at both assessments and were pathed first to Early and then to Late Quit messages. Fourteen percent reported smoking at 2-day post-Quit Day and not smoking at 7-day post-Quit Day. These participants were first pathed to the Relapse messages and then the Early Quit messages, followed by Late Quit messages. Seventeen percent reported not smoking at 2-day post-Quit Day but smoking at 7-day post-Quit Day, and were pathed to Early Quit, then Relapse, then Late Quit messages. Four percent reported smoking at both 2-day and 7-day post-Quit Day, and were pathed to Relapse and then the Encouragement messages that normed future quit attempts. Thirteen percent did not respond to prompts. Control content aimed to improve one's sleep and exercise habits, and was not tailored based on smoking status.
Figure 1.
Pathing of SMS USA intervention participants based upon smoking status at 2 day and 7 day post-Quit Day
Note. The 2-day and 7-day post-Quit day smoking status for the four participants who were pathed contrary to their response due to technology issues at the 7-day post-Quit day follow-up are included.
The program was evaluated in a randomized controlled study in 2011 with participants who were recruited online.
Content focus based on pathing based on smoking status:
Early Quit: content discussed the common difficulties and discomforts associated with quitting, and emphasized the use of coping strategies.
Late Quit: content encouraged participants to recognize relapse in a different way (e.g., situations, confidence, etc.) and provided actionable information about how to deal with issues that arise as a non-smoker (e.g., stress, moods).
Relapse: content focused on helping the participants get back on track and to recommit to quitting
Encouragement (if participant smoking at both 2-day and 7-day post-Quit Day): content focused on norms for quitting and suggested that the participant attempt to quit at later time when they were ready to try again.
Triggers for relapse
Stressful situations were voiced as a major barrier to quitting by both intervention and control group participants. Examples included relationship issues, job transitions, situations with alcohol use, and social pressures. While support received from others made it less difficult to quit, those who were unsuccessful in quitting also experienced peer pressure to continue smoking.
Pharmacotherapy uptake
One in three (66%) participants in the study (i.e., in either the intervention or control group) reported heavy smoking (±10 cigarettes/day) and were encouraged at enrollment to use pharmacotherapy to help them quit. Intervention messages also spoke to the utility of nicotine replacement therapy (NRT) when trying to quit. At the 4-week post-Quit Day assessment, one in five (22%) heavy smokers reported having used pharmacotherapy in the past month compared to 9% of non-heavy smoking participants.
4. DISCUSSION AND CONCLUSION
4.1. Discussion
Invigorating smoking cessation rates among young adults is critical in order to reduce tobacco-related morbidity and mortality. The efficient pace of recruitment demonstrates the demand for this type of programming by this hard to reach population. Feedback suggests that positive messaging combined with opportunities for social support maybe particularly well received by young adult smokers who are trying to quit.
SMS USA participants suggested that stressful situations made it particularly difficult to successfully quit smoking. As acknowledged by tobacco marketing [13], young adults have many life transitions that may put them at risk for smoking initiation [14], as well as make quitting more difficult, including: moving out of their parent's house into an independent living situation; entering a full time job and/or tertiary education environment; relationship issues (e.g., having the first live-in relationship); and peer pressure in social situations, particularly when using alcohol. Most young adult participants were unable to predict the stress that these life events would evoke, and therefore were unprepared to identify alternative coping strategies. Although SMS USA includes messages that address stress, the process evaluation suggests that the content needs to be strengthened with a wider variety of possible scenarios and a greater emphasis on associated coping techniques. It may be too that a hybrid approach that includes both real people and automated messaging, such as access to coaching from cessation counselors, is warranted for some smokers in their quitting process – particularly as they try to navigate stressful situations.
Half of intervention participants moved through the program linearly, going from pre-quit to early-quit to late-quit messages. The other half went through various different paths that included relapse and encouragement messages. This variation in quitting experience highlights the need for programs to have a flexible structure. At the same time, the more complex the program, the more expensive it is to develop. Increasing features and flexibility also risks degrading usability for participants. In fact, some of the features suggested by participants to be added in the future (e.g., online discussion board) were available, just not utilized in SMS USA. Future research is needed to balance tailoring, usability, and impact on cessation rates.
Only one in five heavy smokers used pharmacotherapy during the RCT, despite being encouraged to do so by the project coordinator during enrollment. Rates were twice as high for heavy smokers than non-heavy smokers, who did not receive the counseling, however. Furthermore, the rate was twice as high as what was noted among young adult smokers in the Current Population Survey [15]. It seems, then, that the advice invigorates uptake, just not to the degree desired. Formative research that informed the development of SMS USA found that young adult smokers have mixed feelings about utilizing pharmacotherapy [16]. Many voiced concerns about the cost and a lack of clarity about the various cessation options. Although intervention messages were crafted to address these potential barriers, program content could be augmented with adherence reminders and a more comprehensive battery of messages aimed at norming the use of pharmacotherapy for heavy smokers to increase pharmacotherapy use.
Although more research is needed in this area, our experiences suggest that the reinforcement of the small effort required by completing the assessment via text messaging gives researchers a “foot in the door” that increases the likelihood of completion of the more comprehensive online survey. Text messaging may be a useful gateway perhaps by reminding participants that the data collection is a relatively simple process. Even when both text messaging and the Internet are accessible from one's phone, there appears to be a real ease of interaction with text messaging that is greater than solely online content. Future research could explore whether smoking cessation programming delivered via smartphones and/or applications (“apps”) has equal or greater interest; and whether it affects greater immersion with the program, thereby resulting in higher quit rates. The effect of the incentive could also be explored. While the amount was minimal and only proffered if surveys were completed, incentives may have affected the feasibility data such that if an incentive were not provided, fewer people would have completed the program.
4.2.Conclusion
Participant feedback points to concrete ways in which this and other young adult-focused interventions can improve messaging and other program features to be even more salient for this hard to reach population.
4.3.Practice Implications
As new technologies emerge as a means of encouraging and sustaining health behavior change, researchers should share their experiences with the development, implementation, and evaluation of these interventions. Text messaging-based behavior change programs for young adults could consider a model that is flexible to different “paths” of behavior change; address concrete actionable suggestions for coping with stressful life events that may interfere with change efforts; and proactively uses messaging to both norm use of evidence-based practices and promote effective use to increase chances of success (e.g. pharmacotherapy for cessation). Researchers developing and evaluating mHealth interventions may benefit from the use of text messaging as a gateway to longer online surveys, to increase expected participation and completion rates, and to improve levels of engagement with various aspects of the intervention. Through this pilot work, we obtained clear feedback from participants that shaped our thinking about mHealth intervention content and observed useful methods to improve the internal validity of our mHealth outcomes research.
Highlights.
We analyze process data from an RCT of young adult smokers ready to quit
Programs need to be flexible to different “paths” of behavior change
Common youth stressful life events need to be addressed directly and comprehensively
Proactive messaging that promotes pharmacotherapy options are needed
Text messaging surveys can be used as a gateway to longer online surveys in RCTs
Acknowledgements
We thank Dr. Amanda Graham for her consultation. We also thank the entire Study team from Center for Innovative Public Health, Michigan State University, and the University of Texas Health Science Center at Houston (UTHealth), who contributed to the planning and implementation of the study. We thank the study participants for their time and willingness to participate in this study.
Role of Funding
This work was supported by Award Number R21CA135669 from the National Cancer Institute at the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funder had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
The authors have no conflicts to declare.
Contributor Information
Michele L Ybarra, Center for Innovative Public Health Research San Clemente, CA 92672 USA.
Jodi Summers Holtrop, Department of Family Medicine University of Colorado Denver School of Medicine Aurora, CO 80045 USA.
Tonya L Prescott, Center for Innovative Public Health Research San Clemente, CA 92672 USA.
David Strong, Department of Family and Preventive Medicine University of California, San Diego La Jolla, CA 92093 USA.
References
- 1.Hammond D. Smoking behaviour among young adults: beyond youth prevention. Tob Control. 2005;14:181–5. doi: 10.1136/tc.2004.009621. doi: 10.1136/tc.2004.009621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration . Results from the 2010 National Survey on Drug Use and Health: Summary of national findings. H-41 ed. US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2011. [June 1, 2014]. (NSDUH Series). Available at: http://www.samhsa.gov/data/NSDUH/2k10NSDUH/2k10Results.htm. [Google Scholar]
- 3.U.S. Department of Health and Human Services . Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2012. [June 1, 2014]. Available at: http://www.surgeongeneral.gov/library/reports/preventing-youth-tobacco-use/full-report.pdf. [Google Scholar]
- 4.Smith A. How American Use Text Messaging. Pew Internet & American Life Project; Washington, DC: 2011. [June 1, 2014]. Available at: http://www.pewinternet.org/2011/09/19/how-americans-use-text-messaging/. [Google Scholar]
- 5.Ybarra ML, Bull S. Current trends in internet- and cell phone-based HIV prevention and intervention programs. Curr HIV/AIDS Rep. 2007;4:201–7. doi: 10.1007/s11904-007-0029-2. doi: 10.1007/s11904-007-0029-2. [DOI] [PubMed] [Google Scholar]
- 6.Ybarra ML, Holtrop JS, Prescott TL, Rahbar MH, Strong D. Pilot RCT results of Stop My Smoking USA: a text messaging-based smoking cessation program for young adults. Nicotine Tob Res. 2013;15:1388–99. doi: 10.1093/ntr/nts339. doi: 10.1093/ntr/nts339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wei J, Hollin I, Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. J Telemed Telecare. 2011;17:41–8. doi: 10.1258/jtt.2010.100322. doi: 10.1258/jtt.2010.100322. [DOI] [PubMed] [Google Scholar]
- 8.Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2012:CD006611. doi: 10.1002/14651858.CD006611.pub3. doi: 10.1002/14651858.CD006611.pub3. [DOI] [PubMed] [Google Scholar]
- 9.Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14:255–61. doi: 10.1136/tc.2005.011577. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet. 2011;378:49–55. doi: 10.1016/S0140-6736(11)60701-0. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010;32:56–69. doi: 10.1093/epirev/mxq004. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ybarra ML, Holtrop JS, Bagcı Bosi T, Emri S. Design considerations in developing a text messaging program aimed at smoking cessation. J Med Internet Res. 2012;14:e103. doi: 10.2196/jmir.2061. doi: 10.2196/jmir.2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ling PM, Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: evidence from industry documents. Am J Public Health. 2002;92:908–16. doi: 10.2105/ajph.92.6.908. doi: 10.2105/AJPH.92.6.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allem J-P, Soto DW, Baezconde-Garbanati L, Unger JB. Role transitions in emerging adulthood are associated with smoking among hispanics in southern California. Nicotine Tob Res. 2013;15:1948–51. doi: 10.1093/ntr/ntt080. doi: 10.1093/ntr/ntt080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Messer K, Trinidad DR, Al-Delaimy WK, Pierce JP. Smoking cessation rates in the United States: A comparison of young adult and older smokers. Am J Public Health. 2008;98:317–22. doi: 10.2105/AJPH.2007.112060. doi: 10.2105/AJPH.2007.112060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ybarra ML, Prescott TL, Holtrop JS. Steps in tailoring a text messaging-based smoking cessation program for young adults. J Health Commun. 2014 doi: 10.1080/10810730.2014.901441. doi: 10.1080/10810730.2014.901441. [DOI] [PubMed] [Google Scholar]