Abstract
Background and Objectives:
Assessment of ergonomic strain during robotic surgery indicates there is a need for intervention. However, limited data exist detailing the feasibility and acceptance of ergonomic training (ET) for robotic surgeons. This prospective, observational pilot study evaluates the implementation of an evidence-based ET module.
Methods:
A two-part survey was conducted. The first survey assessed robotic strain using the Nordic Musculoskeletal Questionnaire (NMQ). Participants were given the option to participate in either an online or an in-person ET session. The ET was derived from Occupational Safety and Health Administration guidelines and developed by a human factors engineer experienced with health care ergonomics. After ET, a follow-up survey including the NMQ and an assessment of the ET were completed.
Results:
The survey was sent to 67 robotic surgeons. Forty-two (62.7%) responded, including 18 residents, 8 fellows, and 16 attending physicians. Forty-five percent experienced strain resulting from performing robotic surgery and 26.3% reported persistent strain. Only 16.6% of surgeons reported prior ET in robotic surgery. Thirty-five (78%) surgeons elected to have in-person ET, which was successfully arranged for 32 surgeons (91.4%). Thirty-seven surgeons (88.1%) completed the follow-up survey. All surgeons participating in the in-person ET found it helpful and felt formal ET should be standard, 88% changed their practice as a result of the training, and 74% of those reporting strain noticed a decrease after their ET.
Conclusion:
Thus, at a high-volume robotics center, evidence-based ET was easily implemented, well-received, changed some surgeons' practice, and decreased self-reported strain related to robotic surgery.
Keywords: Ergonomic strain, Robotic surgery, Ergonomic training, Strain
INTRODUCTION
The da Vinci Surgical System (Intuitive Surgical Inc., Sunnyvale, California), a robotic surgical system, has experienced widespread acceptance and growth over the past decade.1–4 Several studies have suggested that robotic surgery is more ergonomically favorable and potentially less mentally stressful than conventional laparoscopic surgery.5,6 However, the literature evaluating these reported ergonomic benefits remains sparse. Despite patient benefits of minimally invasive surgery (MIS) overall, surgeon strain is a prominent issue, with recent reports of strain related to MIS being as high as 87% to 88%.7,8 Although robotic surgery is often thought of as a tool to alleviate strain related to MIS,9,10 there are still high levels of strain involved with robotic surgery, and effective interventions are needed to prevent and reduce strain to prevent work-related injury.11
Craven et al have reported specifically on the ergonomic deficits in robotic surgery. Using the Rapid Upper Limb Assessment (RULA) survey and the Strain Index (SI), a detailed assessment of 17 hours of video recording was undertaken. Ergonomic evaluation of surgeon activity resulted in a mean RULA score of 6.46 (maximum possible RULA score, 7), indicating a need for further investigation. The mean SI grand score was 24.34. SI scores >10 suggest a potential for hazard to the operator.11 Thus the current use of the surgical robot merits further investigation into interventions, which can improve ergonomic use.
MIS strain is exacerbated by the lack of knowledge and training regarding proper ergonomic techniques among surgeons.7,8,12 Indeed, there is little available literature specific to robotic surgery ergonomics. What information is available has been based on recommendations from the US Department of Labor's Occupational Safety and Health Administration's (OSHA's) guidelines for working positions at workstations and on the available body of literature on the ergonomics of microscopy, which have been adapted for robotics.13 These include a comfortable headrest and adjustable ocular height aimed at relieving neck, shoulder, and upper back strain; and armrests aimed at minimizing the arm and upper back strain caused by static load forces.14
Given the increasing prevalence of robotic surgery in the setting of strain levels that are potentially hazardous and could predispose to work-related injury, there is a need to assess ergonomic training methods for robotic surgeons. To date, there are limited data on the implementation of ergonomic training modules in terms of their feasibility, acceptance, and perceived effectiveness. For this reason, we sought to evaluate robotic surgeons' perception of strain in robotic surgery, their need for training, and their willingness to participate in and acceptance of a standardized and evidence-based ergonomic training session. In addition, we wanted to evaluate whether the training provided led to self-reported change in practice and improvements in surgeon-related strain as reported by the surgeons choosing to participate.
MATERIALS AND METHODS
The Institutional Review Board at the University of North Carolina (UNC#106718) approved the study protocol. An invitation to participate in the study was sent via E-mail to active robotic surgeons at UNC. UNC Surgical Services keeps an activity log for robotic surgeons, and this document was used to identify eligible surgeons. Included within the invitation was an explanation of the study and a statement that participation was voluntary and that responses to the survey would be used only for research purposes. The study participants accessed the online survey via a link included in the invitation E-mail.
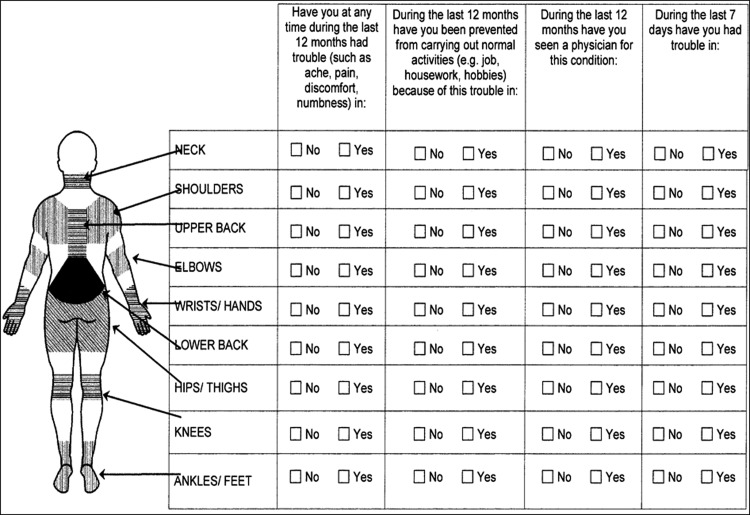
The initial survey consisted of 38 questions and focused on demographics, the surgeon's physical characteristics related to ergonomic strain, robotic surgery volume and characteristics of the operative setting, operative strain and impact on practices, and experience with ergonomic training. Responses were single-answer, multiple-choice, or numeric response. The question-and-answer structure is included in Table 1. The strain assessment was accomplished using a modified version of the Nordic Musculoskeletal Questionnaire (NMQ), a validated tool for strain in epidemiologic studies.15 The NMQ used for the survey is shown in Figure 1.
Table 1.
Initial Survey Questions
| Demographics | |
| What best described your current position (Attending, Fellow, Resident)? | SA |
| What type of residency did you or will you complete? | SA |
| Did you complete or are you currently completing a fellowship? | SA |
| What type of fellowship training did you or will you complete? | SA |
| What year did you or will you complete fellowship? | NR |
| What is your height in inches? | NR |
| What is your weight in pounds? | NR |
| What is your surgical glove size? | NR |
| What is your date of birth? | NR |
| What is your gender? | SA |
| If given a preference, how would you post a case (laparoscopic, robotic, open)? | SA |
| Robotic Surgery | |
| Do you perform robotic surgeries? | SA |
| How many years have you been performing robotic surgery? | NR |
| How many robotic cases do you perform on average in a week? | NR |
| How many robotic cases do you perform in an average year? | NR |
| How many robotic cases do you perform in an average day? | NR |
| How long is your average robotic case (minutes)? | NR |
| How long is your average robotic case? | NR |
| What is the average BMI of your robotics cases? | NR |
| Do you supervise residents and fellows during robotic surgery? | SA |
| When supervising, what percentage of time do you spend at the console? | SA |
| Ergonomic Strain | |
| Have you experienced physical discomfort directly related to robotic surgery? | SA |
| In the past 12 months I have experienced discomfort related to robotic surgery: | NMQ |
| In the past 12 months I have been prevented from carrying out normal activities: | NMQ |
| In the past 12 months I have been seen by a professional: | NMQ |
| In the past 7 days I have experienced discomfort related to robotic surgery: | NMQ |
| Is the discomfort limited to time operating or does it persist? | SA |
| Has this discomfort caused you to limit your medical practice? | SA |
| Have you reported your symptoms to Occupational Health? | SA |
| How do you attempt to minimize symptoms related to robotic surgery? | MA |
| Have you had treatment for discomfort related to robotic surgery? | SA |
| Ergonomic Training | |
| Have you been given ergonomic training specifically designed for robotic surgery? | SA |
| How did you receive your ergonomic training? | MA |
| How many years ago did you receive your ergonomic training? | NR |
| Would you be interested in a personalized, 5-mintue ergonomic training session designed for robotic surgery? | SA |
| What would be the best platform for ergonomic training? | MA |
NR, numeric response; SA, single answer; NMQ, Nordic Musculoskeletal Questionnaire; MC, multiple-choice.
Figure 1.
Strain assessment based on the Nordic Musculoskeletal Questionnaire.
At the completion of the survey, participants were linked to a slideshow-based training session consisting of instructions on how to ergonomically set up their robotic console. All instructions included images depicting the correct and incorrect ergonomic setup at each major flexion/extension point, including knees, hips, low back, neck, shoulder, elbows, and wrists. In addition, surgeons were asked whether they wanted to participate in a 5-minute, personalized robotic ergonomic training session. Surgeons who indicated they were interested took the session at a time convenient to them over the subsequent 6 weeks.
The ergonomic training was a standardized series of instructions on setting up the robotic console based on ergonomic principles and was tailored to each surgeon. Two study personnel familiar with robotic surgery, and who had themselves completed ergonomic training, conducted the sessions. The surgeons were instructed on how to set up and save their neutral posture settings and then were given tips on how to maintain ergonomically correct postures while operating. Recommendations were based on the Occupational Safety and Health Administration (OSHA) workstation guidelines and microscope ergonomic guidelines and were reviewed by a human factors engineer experienced with health care ergonomics.13–16 All instructions provided were associated with a visual aid indicating correct and incorrect positioning. Specific instructions provided are included in Table 2.
Table 2.
Ergonomic Instructions Provided During In-Person Training
| Positioning Instructions |
| 1. Chair positioning: The chair should be on lockable castors for ease of mobility and have an adjustable height, depth, and lumbar support. |
| 2. Optic viewer height: Chair and robotic console height should be adjusted so that the optics are at a comfortable position for viewing. When adjusting, the feet should rest on the ground in front of the pedals and the knees should be at a 90° angle or greater. |
| 3. Upper arm rest: The upper arms should be perpendicular to the floor. The elbows should form a 90° angle with the forearms resting on the armrest. Elbows should remain close to the torso. |
| 4. Neck/Back: With the forearms resting comfortably on the armrest, the surgeon should be able to look through the optics without arching/straightening the back or neck to gain height. The angle of the neck should be approximately 20°. Avoid excessive bending of the neck and upper back to look downward. |
| 5. Headrest: The surgeon should avoid placing undue force on the forehead and should not press too firmly into the headrest. Too much force results in undue forehead pain and neck strain. |
| 6. Neutral position: This position should be attained at the onset of the case, with periodic revaluation if discomfort occurs later. |
| Key Reminders |
| 1. Improper positioning occurs when the arms are brought out away from the torso, often when operating at the limit of the surgical field. Returning the forearms to the rest with the elbows at the torso should be accomplished with frequent clutching. |
| 2. If strain is noted, take time to stretch intermittently during instrument/suture changes. Reevaluate neutral position as well as chair/console height to reduce excessive back and neck strain. |
The follow-up survey was sent 6 months after the original study was initiated. This follow-up consisted of 13 questions related to robotic strain over the previous months and qualitative assessments of the training modules. Answers were yes or no, multiple choice, or numeric response. The question-and-answer structure is included in Table 3. Two reminder e-mails were sent after the initial and follow-up surveys, and the survey was closed two weeks after the final reminder E-mail was sent. The results from the survey were imported from the online platform into Microsoft Excel and then analyzed.
Table 3.
Follow-up Survey Questions
| Ergonomic Strain | |
| In the past 6 months have you experienced physical discomfort/strain directly related to robotic surgery? | SA |
| In the past 6 months I have experienced discomfort related to robotic surgery: | NMQ |
| In the past 6 months I have been prevented from carrying out normal activities: | NMQ |
| In the past 6 months I have been seen by a professional: | NMQ |
| In the past 7 days I have experienced discomfort related to robotic surgery: | NMQ |
| Is the discomfort limited to time operating or does it persist? | SA |
| Ergonomic Training | |
| What form of ergonomic training did you receive? | MC |
| Did you find the training helpful? | SA |
| Have you changed your practice since receiving the first survey? | SA |
| What changes did you incorporate into your practice? | MC |
| Have you noticed a decrease in strain since the training session? | SA |
| Should evidence-based ergonomic training be a standard part of robotic orientation? | SA |
| What improvements could be made in the ergonomic training session? | MC |
NR, numeric response; SA, single answer; NMQ, Nordic Musculoskeletal Questionnaire; MC, multiple choice.
RESULTS
Demographics
The survey was sent to 67 eligible robotic surgeons identified from the robotic surgery activity log kept by surgical services at the institution, and the 42 (62.7%) who responded comprised the study cohort. The initial responses included 18 residents (43%), 8 fellows (19%), and 16 attending physicians (38%). The average year of graduation from residency was 2008 (range, 1982–2015). Surgeons were currently placed in or had graduated from various residency programs including Ear, Nose and Throat (n = 3, 7.1%), Urology (n = 7, 16.7%), and Obstetrics and Gynecology (n = 32, 76.2%). Twenty-one (50.0%) participants had been or were involved in fellowship training including Urogynecology (n = 3, 14.3%), Advanced Laparoscopy and Pelvic Pain (n = 5, 23.8%), and Gynecologic Oncology (n = 13, 61.9%). The average year of fellowship completion was 2008 (range, 1985–2015). The training demographics are included in Table 4.
Table 4.
Demographics of Surveyed Surgeons
| Physician Training Level | |
| Attending | 16 (38%) |
| Fellow | 8 (19%) |
| Resident | 18 (43%) |
| Residency Program Training | |
| Ear, Nose and Throat | 3 (7.1%) |
| Urology | 7 (16.7%) |
| Obstetrics and Gynecology | 32 (76.2%). |
| Fellowship Program Training | |
| Urogynecology | 3 (14.3%) |
| Advanced Laparoscopy and Pelvic Pain | 5 (23.8%) |
| Gynecologic Oncology | 13 (61.9%) |
On average, participants had 3 years of experience with robotic surgery (range, 1–8). The average height for surgeons was 67.1 inches (range, 61–72) and the average weight was 153.9 pounds (range, 105–250). Nineteen (45%) surgeons were male and 23 (55%) were female.
Robotic Surgery
When asked for their surgical posting preference, 4 (10%) preferred laparotomy, 11 (26%) preferred laparoscopic, and 27 (64%) preferred the robotic platform. The mean number of robotic surgery cases reported per week and per year were 2 (range, 0–6) and 50 (range, 3–200), respectively. When asked how many cases per day would be performed on a “robotic surgery” day, the mean was 2 (range, 1–3). Twenty-two surgeons (52.3%) reported supervising residents during robotic surgery and estimated they sat at the console for 25% of the surgical case (n = 12), 50% of the case (n = 7), and 75% of the case (n = 2). The average self-reported case time in minutes for all surgeons was 161.5 (range, 60–240), and the average patient body mass index according to surgeon recall was 34.4 kg/m2 (range, 24–45).
Initial Ergonomic Strain
When asked whether they experienced strain specifically caused by robotic surgery, 45.2% (19/42) responded “yes.” The group of 19 responding “yes” comprised 7 of the 18 residents responding (39%), 4 of the 8 fellows responding (50%), and 8 of the 16 attending physicians responding (50%). Using the NMQ assessment for those who experienced strain in the prior 12 months, surgeons experienced discomfort (aches, pains, or numbness) related to robotic surgery in the following areas: head (n = 5, 26.3%), neck (n = 14, 73.7%), shoulders (n = 10, 52.6%), upper back (n = 3, 15.8%), wrist/hands (n = 7, 36.8%), lower back (n = 8, 42.1%), hips/thighs (n = 1, 5.3%), and knees (n = 1, 5.3%). The numbers tallied are >19 because several surgeons commented on experiencing discomfort in more than one location. There were no reports of pain in the elbows or ankles and feet. Again using the NMQ scale, three surgeons indicated they had experienced strain related to robotic surgery in the prior 7 days. Areas of strain indicated included the head, neck, upper and lower back, and wrists and hands.
Two surgeons reported that they had been prevented from carrying out normal daily activities in the prior 12 months from strain related to robotic surgery, one because of neck strain and the other because of hand/wrist strain. Three surgeons reported seeking professional medical care for strain attributed to robotic surgery, one for neck/shoulder/upper back strain, one for head/neck/shoulder/upper and lower back strain, and one for lower back strain. Of those surgeons reporting strain, 26.3% (5/19) had persistent strain related to robotic surgery. No surgeon reported limiting their practice because of strain, and no surgeon reported strain related to robotic surgery to occupational health.
Sixteen surgeons reported that they attempted to minimize ergonomic strain. The majority (n = 14) did so by adjusting the ergonomic controls at the robotic console. No surgeon reported limiting their surgical case volume or taking time off.
Ergonomic Training
Only 16.6% (7/42) of surgeons reported prior formal ergonomic training in robotic surgery. Of those who received training, two had been trained by an industry representative, two by using the robotic simulator, and three by having another surgeon show them how to set up the console. Thirty-five surgeons (83.3%) elected to have an in-person training session, and this was successfully arranged for 32 surgeons (91.4%) based on their availability during the study time frame. Of the seven surgeons not interested in the in-person session, 80% (n = 4) were interested in online training and only one indicated they were uninterested in any form of training. Two surgeons did not reply to this question.
Follow-up Survey
The follow-up survey was completed by 37 (88.1%) of the original 42 surgeons who responded to the first survey. All of the surgeons who participated in the in-person training (n = 32) found it to be helpful, and 88% (28/32) changed their practice as a result of the training. Of those indicating changes to practice, 21.4% (n = 6) paid closer attention to chair selection and position, 75% (n = 21) ensured their chair was positioned so they had 90 degrees of flexion at the knee, 67.9% (n = 19) adjusted the armrest to allow for forearm placement parallel to the floor with elbows tucked at their sides, 67.9% (n = 19) adjusted head tilt to ensure no more than 20 degrees of flexion at the neck, 50% (n = 14) took care not to place pressure on their foreheads while using the headrest, 35.7% (n = 10) adjusted the finger straps, and 42.8% (n = 12) increased the frequency of clutching.
Of the 19 surgeons who reported strain in the original survey, all underwent ergonomic training and 14 (74%) noted a decrease in strain after training. All of the surgeons surveyed felt that formal ergonomic training should be standard practice for robotic surgeons.
DISCUSSION
Our findings reveal that a brief, standardized ergonomic training program for robotic surgery is feasible and perceived to be effective in terms of meeting the needs of the surgeons. Our study represents the first evaluation of an ergonomic training session for robotic surgeons published in the literature. With reported rates of strain related to MIS being as high as 87% to 88%7,8 and strain related to robotic surgery reported by surgeons surveyed in this study being 45%, there is a great need for this type of intervention. These results not only demonstrate a desire on the part of surgeons for ergonomic education, but also the ability to implement a succinct program that is effectively integrated into the busy routines of surgeons.
Additional areas of ergonomic focus can be gleaned from this study. According to the NMQ assessment, the areas of greatest strain were the neck, shoulders, and wrists and hands. Much of the strain related to neck and shoulder strain is likely caused by a failure to maintain “neutral posture” during robotic surgery. Wrist and hand pain is likely caused by a combination of improper adjustment of the finger straps, which causes unnecessary tension on the intrinsic hand muscles, in addition to failure to maintain a neutral position with frequent clutching. Although that combination may seem quite obvious, it is something that is observed frequently during robotic surgery11 and needs to be incorporated into ergonomic training.
Interestingly, only 16% of surgeons reported having any ergonomic training, and the most frequent form of training involved informal discussion with other surgeons or simply using other surgeons' settings. This was a common theme among surgeons and highlights a potential cause for strain exacerbation. When individuals used another surgeon's settings, they often adjusted them, and the system automatically saves these settings. Thus, when the original surgeon sat to perform surgery, their settings had been altered and required adjustment. In addition, at the study institution, there are not dedicated chairs for the robotic consoles; the chairs can be moved from room to room. This can also lead to subtle changes in the ergonomic settings that may not be immediately noticed by the surgeon but can lead to progressive strain.
Overall, very few surgeons indicated that they would not be interested in the in-person training. Of those who did, most indicated they would be willing to perform online training. It is the opinion of the authors that in-person training is more effective because it causes the participant to immediately put into practice the components of the training; however, this needs to be confirmed with a prospective intervention trial. Nevertheless, it is apparent that in-person training is widely accepted by surgeons because >80% of respondents elected to participate in the training program. The online and in-person training sessions were easy to accomplish and, more importantly, they were perceived to be highly effective, leading surgeons to make changes in their practice, as well as noting a perceived decrease in robotic strain in 74% of surgeons who originally reported robotic strain.
Despite these important findings, there are several limitations that must be acknowledged. There is a selection bias introduced given that participation in the training session was voluntary. However, this bias is tempered somewhat by the high rate of participation, with >80% of those responding indicating a desire to take part in ergonomic training. In addition, given the subjective nature of strain, studying its effects is challenging. A standardized strain assessment in the NMQ was used, but the reporting of strain is inherently subjective because strain is subjective. In addition, we asked participants to recall levels of strain over a 12-month period of time. This was done in an effort to capture the surgeons (residents) who may have been intermittently rotating on services that perform robotic surgery. This increases the generalizability of our study because surgeons with various levels of experience and volume were targeted. However, asking for recall over a long period of time may affect recall. Finally, there was a great range of both user experience level, from residents to attending physicians, as well as case volume, from 3 to 200 cases during the prior year. The primary purpose of this study was to explore the feasibility and acceptance of a robotic ergonomic training program. Although an intervention study using this training session may show varied levels of impact across surgeon experience and volume, it is important that a training session be available for all robotic surgeons.
There were some important findings in this study, which could be useful in planning a larger intervention study. Although the generalizability might be compromised somewhat, it would be important to consider the level of experience and surgical volume of participants in the intervention study. Although this pilot study evaluated acceptance and feasibility for all levels of experience and volume, in an intervention study the surgeons with limited robotic surgery experience (ie, residents and fellows) are not likely to show meaningful change in their strain scores compared with more experienced surgeons and those who perform a higher volume of procedures. In surgeons with a high volume of procedures, information on volume of conventional laparoscopic and open surgery would need to be collected and controlled for statistically. In addition, the method of assessment of strain might also be altered. In addition to the validated but subjective NMQ, it is possible that the addition of more objective measures such as the RULA and SI would be useful. This would require the assistance of an individual trained in assessing and scoring these indices.
In summary, at a high-volume robotics center, reported strain rates are high and require immediate intervention. Here, we highlight robotic surgeons' desire to participate in ergonomic training. Subsequently, implementation of an evidence-based training session was well-received, changed practice, and decreased reported strain related to robotic surgery. To allow for an assessment of the true effectiveness of this program to decrease strain, a prospective, randomized trial assessing this training program is the next step.
Contributor Information
Jason Franasiak, Department of Obstetrics, Gynecology and Reproductive Science, Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ. USA..
Renatta Craven, University of North Carolina School of Medicine, Chapel Hill, NC, USA..
Prithima Mosaly, University of North Carolina School of Medicine, Chapel Hill, NC, USA..
Paola A. Gehrig, Department of Obstetrics and Gynecology, University of North Carolina, Chapel Hill, NC, USA..
References:
- 1. Wexner SD, Bergamaschi R, Lacy A, et al. The current status of robotic pelvic surgery: results of a multinational interdisciplinary consensus conference. Surg Endosc. 2009;23:438–443. [DOI] [PubMed] [Google Scholar]
- 2. Challacombe BJ, Khan MS, Murphy D, Dasgupta P. The history of robotics in urology. World J Urol. 2006;24:120–127. [DOI] [PubMed] [Google Scholar]
- 3. Ballantyne GH, Moll F. The da Vinci telerobotic surgical system: the virtual operative field and telepresence surgery. Surg Clin North Am 2003;83:1293–1304. [DOI] [PubMed] [Google Scholar]
- 4. Ruurda JP, van Vroonhoven TJ, Broeders IA. Robot-assisted surgical systems: a new era in laparoscopic surgery. Ann Royal Coll Surg Engl. 2002;84:223–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mohr CJ, Nadzam GS, Curet MJ. Totally robotic Roux-en-Y gastric bypass. Arch Surg. 2005;140:779–786. [DOI] [PubMed] [Google Scholar]
- 6. Talamini MA, Chapman S, Horgan S, Melvin WS, Academic Robotics G. A prospective analysis of 211 robotic-assisted surgical procedures. Surg. Endosc. 2003;17:1521–1524. [DOI] [PubMed] [Google Scholar]
- 7. Park A, Lee G, Seagull FJ, et al. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. 2010;210(3):306–313. [DOI] [PubMed] [Google Scholar]
- 8. Franasiak J, Ko EM, Kidd J, et al. Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol. 2012;126(3):437–442. [DOI] [PubMed] [Google Scholar]
- 9. Mucksavage P, Kerbl DC, Lee JY. The da Vinci (R) Surgical System overcomes innate hand dominance. J Endourol. 2011;25:1385–1388. [DOI] [PubMed] [Google Scholar]
- 10. Schreuder HW, Verheijen RH. Robotic surgery. Br J Obstet Gynecol. 2009;116:198–213. [DOI] [PubMed] [Google Scholar]
- 11. Craven R, Franasiak J, Mosaly P, Gehrig PA. Ergonomic deficits in robotic gynecologic oncology surgery: a need for intervention. J Minim Invasive Gynecol. 2013;20(5):648–655. [DOI] [PubMed] [Google Scholar]
- 12. Stone R, McCloy R. Ergonomics in medicine and surgery. BMJ. 2004;328:1115–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lux MM, Marshall M, Erturk E, Joseph JV. Ergonomic evaluation and guidelines for use of the DaVinci Robot system. J Endourol. 2010;24:371–375. [DOI] [PubMed] [Google Scholar]
- 14. McAtamney L, Corlett EN. Ergonomic workplace assessment in a health care context. Ergonomics. 1992;35:965–978. [DOI] [PubMed] [Google Scholar]
- 15. Sillanpaa J, Nyberg M, Laippala P. A new table for work with a microscope, a solution to ergonomic problems. Appl Ergon. 2003;34:621–628. [DOI] [PubMed] [Google Scholar]
- 16. Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237. [DOI] [PubMed] [Google Scholar]