Abstract
Background:
To date, the management of common bile duct stones (CBDs) is still controversial. If laparoscopic exploration is performed and biliary decompression is needed after stone removal, the placement of a laparoscopic transpapillary stent shows promising results in avoiding T-tube–related complications.
Methods:
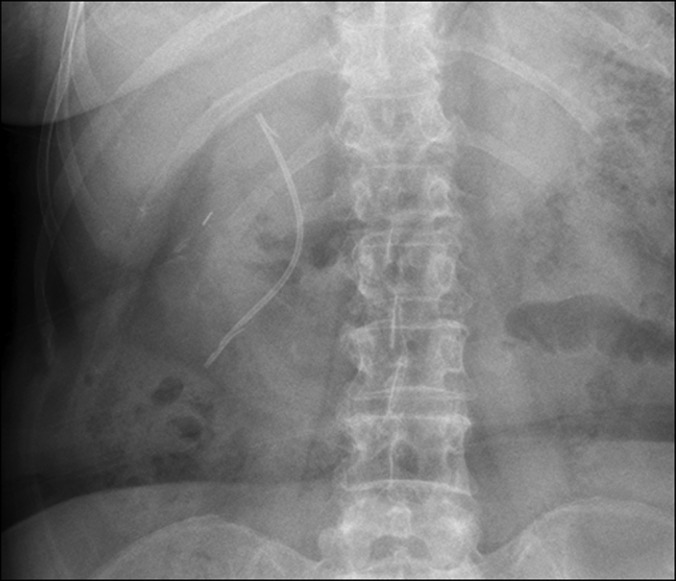
Between January 2007 and May 2012, a series of 48 patients who underwent biliary decompression after laparoscopic common bile duct exploration (LCBDE) to treat choledocholithiasis was retrospectively analyzed. The results in patients with transpapillary stent placement (TS=35) were compared with those who had an external biliary drainage (EBD=13).
Results:
LCBDE and TS placement was achieved either by a choledochotomy or through the cystic duct. There was no mortality in our series. Patients with an external biliary drainage (EBD) had more surgery-related complications (P<.0001) and a longer hospital stay (P=.03). Postoperative ERCP to remove the TS was successful in all cases.
Conclusion:
Laparoscopic TS is a safe method in the treatment of selected patients with CBD stones that can be achieved without having to perform a choledochotomy. Because of the lower morbidity and the shorter hospital stay compared with EBD, it should be considered as a first approach whenever biliary decompression is needed after LCBDE.
Keywords: Common bile duct stones, Biliary drainage, Laparoscopy, Choledocholithiasis
INTRODUCTION
To date, the management of concomitant gallbladder and common bile duct (CBD) stones is still controversial. There are several approaches to the treatment of biliary lithiasis, including laparoscopic common bile duct exploration (LCBDE) and pre-, intra-, or postoperative endoscopic retrograde cholangiopancreatography (ERCP). Despite these multiple options and the improvement of minimally invasive techniques, many surgeons still perform an open CBD exploration with external biliary drainage (EBD).
The simultaneous laparoscopic treatment of CBD stones during laparoscopic cholecystectomy (LC) has demonstrated advantages when compared with other surgical approaches.1–3 However, the laparoscopic exploration of the bile ducts requires the proper equipment as well as expertise in advanced surgical skills, such as bile duct suturing and stones extraction. The removal of biliary stones can be achieved either through the cystic duct or by choledochotomy. Although both approaches are useful and have precise indications, the transcholedochal route has been associated with a higher morbidity rate, mainly related to the frequent use of a T-tube for biliary decompression.4 Regarding this particular issue, the use of a transpapillary stent (TS) appears to be a valuable and safe alternative to avoid these complications with satisfactory outcomes.5
The aim of this study was to analyze the morbidity, mortality, and outcomes between patients with biliary lithiasis who underwent LCBDE and biliary stenting versus external biliary drainage.
METHODS
The current report presents a single-institution retrospective analysis of a prospectively maintained database. Between January 2007 and May 2012, a total of 3700 consecutive patients underwent an LC to treat gallbladder lithiasis at the Hospital Italiano de Buenos Aires. In 356 (9.6%) patients, choledocholithiasis was diagnosed or confirmed by routine intraoperative cholangiography (IOC) and were treated by an LCBDE. In all of these patients, stone extraction was attempted, either transcystically or with transcholedochal exploration. In 48 (13%) patients, either TS or EBD was required for biliary decompression as a result of residual stones or reduced flow of contrast material into the duodenal lumen. This group was included is this study analysis.
Surgical Technique
The American technique of LC was used with the patient in the prone position. Four trocars were used (one 10-mm umbilical, one 5-mm epigastric, two 5-mm in the right flank). IOC was routinely used and performed through a cholangiography catheter into the cystic duct. Once the presence of biliary stones was confirmed, LCBDE under fluoroscopic control was performed with the use of a Web–2×4 extraction basket (Cook Medical, Bloomington, Indiana) either through the cystic duct or by choledochotomy. The presence of multiple or intrahepatic stones and low cystic duct–CBD junction were indications to perform a choledochotomy.
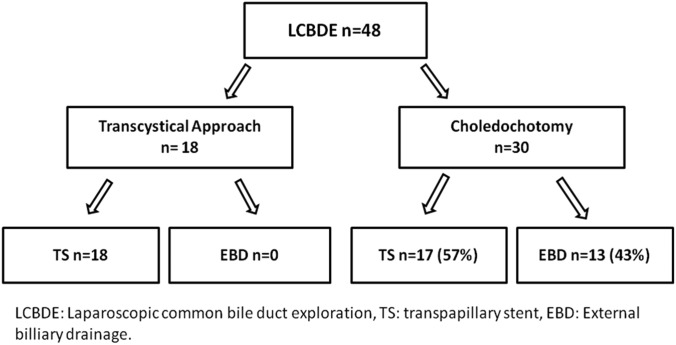
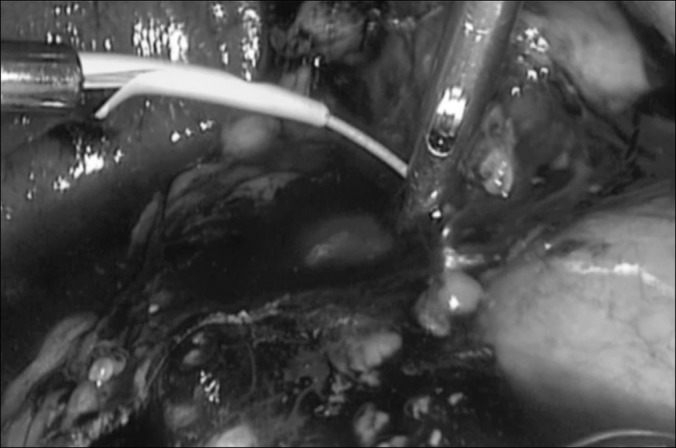
For biliary decompression either TS or EBD was considered depending on the operating surgeon's experience, the availability of the material, the possibility of cannulating the ampulla with a wire guide, and the presence of residual stones. For transpapillary stenting, a 7-Fr plastic biliary stent was placed (Cotton-Leung 7–9, Cook Medical) (Figure 1). If a choledochotomy had been performed, primary biliary closure consisted of interrupted 5-0 polydioxanone stitches (PDS II, Ethicon, Somerville, New Jersey) with the intracorporeal knot-suturing technique. For EBD, a T-tube was placed using the same surgical technique as the open approach. At the end of the procedure, an IOC was performed to certify a proper repair, ensure an appropriate positioning of the stent or the T-tube, and confirm the free flow of contrast into the duodenum (Figure 2). Once a proper biliary decompression was certified, an LC was performed.
Figure 1.
LCBDE and TS placement using the transcystic approach.
Figure 2.
IOC showing the correct placement of the TS.
Follow-Up.
During patients' hospital stay, daily clinical evaluation and laboratory tests were performed. After discharge, the patients were controlled every 3 months during the first year and annually thereafter (with clinical evaluation and liver function tests done). According to the findings, additional imaging studies were used to rule out biliary stenosis. The Dindo-Clavien classification6 was used to stratify the severity of complications.
Statistical Analysis
For comparison between treatment modality, the χ2 test was used for categorical variables and the Student t test was used for continuous variables. Analyses were performed using NCSS software (version 2007, NCSS Kaysville, Utah). All statistical tests were two-sided and statistical significance was defined as P<.05.
RESULTS
Of the 48 patients who comprised the study population, all underwent an LCBDE without conversion to open surgery. The successful clearance of stones was achieved in 41 (85%) patients.
Eighteen patients (37%) underwent a transcystic stone extraction, and 30 patients (63%) required a choledochotomy. TS and EBD were placed in 35 (73%) and 13 (27%) patients, respectively (Figure 3).
Figure 3.
Study population.
Data analyzed were compared between both groups (TS vs EBD). There were no statistically significant differences in epidemiological characteristics and preoperative factors (Table 1). Regarding operative times, there were no statistically significant differences between both groups (P=0.08). However, postoperative complications were significantly higher (P<.0001) in the group with an EBD (Table 2). Overall morbidity in the EBD group was 38% (5 patients), with two patients developing acute pancreatitis, two developing cholangitis, and 1 presenting with an accidental displacement of the T-tube. Regarding the TS group, one patient presented with a biliary peritonitis in the immediate postoperative period that required reoperation. During laparoscopic exploration, an accessory duct of Luschka was diagnosed and sutured, and the patient had a favorable recovery. There were no intra- or postoperative deaths. Regarding hospital stay, the TS group presented a faster recovery than the EBD group (Table 3). This difference was also statistically significant (P=.03).
Table 1.
Epidemiological Characteristics: Preoperative Factors
| Transpapillary Stent, n (%) | External drainage, n (%) | P value | |
|---|---|---|---|
| Age (y) | 60.2 (33–83) | 64.1 (28–88) | .56 |
| M/F (sex ratio) | 2:1 | 1:1 | NS |
| Consult | |||
| Pain | 35 (100) | 12 (92) | NS |
| Jaundice | 26 (80) | 3 (23) | NS |
| Fever | 9 (25) | 4 (30) | NS |
| Dyspepsia | 5 (14) | 2 (15) | NS |
NS, not significant.
Table 2.
Postoperative Complications
| Transpapillary Stent, n (%) | External drainage, n (%) | P value | |
|---|---|---|---|
| Morbidity | 1 (2.8) | 5 (38) | .0001 |
| Mortality | 0 | 0 | |
| Type of complications (DC) | |||
| Choleperitoneum (IVa) | 1 (2.8) | 0 | .53 |
| Pancreatitis (II) | 0 | 2 (15) | .02 |
| Cholangitis (II) | 0 | 2 (15) | .02 |
| Accidental tube displacement (II) | 0 | 1 | .1 |
Table 3.
Media Time of Surgery, Hospital Stay, and Removal of Stent or Drainage
| Transpapillary Stent, n (%) | External Drainage, n (%) | P value | |
|---|---|---|---|
| Surgery time (min) | 150 (90–210) | 183 (130–250) | .08 |
| Hospital stay (d) | 3 (2–6) | 6 (4–10) | .03 |
| Removal of stent or drainage (d) | 30 (15–90) | 45 (30–70) | .08 |
Those patients in the TS group underwent a postoperative outpatient ERCP for stent removal on average 4 weeks (range, 15–90 days) after surgery, with successful cannulation and stent removal in all cases. None of these patients presented with ERCP-related complications. In addition, 7 patients (20%) in this group presented with residual biliary lithiasis that was successfully treated during the same endoscopy. In patients with an EBD, a transcatheter cholangiography was performed 6 weeks (range, 30–70 days) after surgery, which showed free contrast flow into the duodenum lumen without residual lithiasis in all patients, thus the drain was removed.
DISCUSSION
Today, LC has become the gold standard treatment for gallstone disease. Approximately 8% to 15% of the patients with symptomatic gallstones have simultaneous choledocholithiasis.4 Historically, in patients with a preoperative diagnosis of CBD stones during the early laparoscopic era, a two-stage surgical approach (ERCP followed by LC) was the preferred treatment for most surgeons.7–9 However, this approach presented several disadvantages. CBD stones often escape notice in ordinary preoperative work-up for LC such as with liver function tests or ultrasonography, making preoperative diagnosis challenging.7,10 Alternatively, ERCP has been associated with a morbidity of 7% to 15%11–13 and a cannulation failure rate ranging from 5% to 20%.11
Recent studies have demonstrated the advantages of the laparoscopic treatment of CBD stones in a single stage, with equivalent results to those of ERCP.12 Moreover, the increasing adoption of IOC has brought the laparoscopic surgeon against the potential situation of having to deal with the presence of unsuspected choledocholithiasis. Currently, LCBDE and stone extraction have become safe and valuable alternatives in the hands of skilled surgeons—either transcystically or through a choledochotomy.5 Because of a lower complication rate,14–16 laparoscopic exploration through the cystic duct remains the access location of choice.13,17,18 However, a low cystic duct–CBD junction and large (≥10 mm), multiple, or intrahepatic stones are indications to perform a choledochotomy.19 In 18 (37%) patients in our series, the CBD exploration was achieved through the cystic duct, and 30 (63%) patients underwent a choledochotomy. An EBD was used for biliary decompression in less than half of the patients who had a choledochotomy performed.
EBD was a safe and effective method to prevent biliary leakage or to provide an effective biliary decompression in cases of incomplete stone removal after choledochotomy closure in the open cholecystectomy era. Despite these advantages, T-tube–related complications were discussed for decades, with 15% to 28% morbidity either in the open or laparoscopic approach.20,21 The most common complications described are postoperative cholangitis, accidental T-tube displacement, and biliary leakage after drainage removal.21,22 Recent literature suggests that laparoscopic endobiliary stents decrease postoperative T-tube–related complications, improving patient comfort and a promoting a faster recovery.19,23–25 In our series, the stent group had significantly fewer complications than the EBD group (2.8% vs 38%), which is consistent with the current literature. In addition, those patients in the EBD group had two times longer hospital stays than those in the TS group, with discharges 3 and 6 days after surgery, respectively.
The main drawback of placing a TS after LCBDE is the need for a second procedure (ERCP) to remove the stent. In our series, ERCP was successfully performed in all patients in whom a transpapillary stent was placed, with the removal of the stent and stones extraction as a frequent associated procedure. In this particular regard, the success rate of stone clearance after LCBDE was 85%, which is similar to that of other authors.26 The presence of residual stones is an additional reason that justifies a postoperative ERCP. The absence of cannulation failure in the ERCP, an event that has been reported in as many as 20% of patients with CBD stones, is another advantage of the stenting group that should be taken into account to decide which strategy to use whenever biliary decompression is needed after CBDE.27
Despite the results and their statistical value, our study presents some weaknesses because it is a retrospective study in a single institution. Because of this, we emphasize the need for randomized controlled trials to clarify and support our findings.
CONCLUSION
LCBDE remains a challenge even for skilled surgeons with laparoscopic training. However, the excellent results obtained make this approach a safe and useful tool to treat the CBD stones. The laparoscopic transpapillary stenting shows several advantages compared with external biliary drainage. It has lower morbidity and mortality rates, requires a shorter hospital stay, and gives the additional benefit of achieving a high rate of CBD cannulation and stone extraction with postoperative ERCP, thus avoiding repeat surgical or endoscopic procedures to treat residual lithiasis.
Contributor Information
Agustin Dietrich, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
Fernando Alvarez, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
Nicolas Resio, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
Oscar Mazza, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
Eduardo de Santibañes, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
Juan Pekolj, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
Rodrigo Sanchez Clariá, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
Martin de Santibañes, Department of General Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina..
References:
- 1. Millat B, Atger J, Deleuze A, et al. Laparoscopic treatment for choledocholithiasis: a prospective evaluation in 247 consecutive unselected patients. Hepatogastroenterology. 1997;44(13):28–34. [PubMed] [Google Scholar]
- 2. Berthou JC, Drouard F, Charbonneau P, Moussalier K. Evaluation of laparoscopic management of common bile duct stones in 220 patients. Surg Endosc. 1998;12(1):16–22. [DOI] [PubMed] [Google Scholar]
- 3. Decker G, Borie F, Millat B, et al. One hundred laparoscopic choledochotomies with primary closure of the common bile duct. Surg Endosc. 2003;17(1):12–18. [DOI] [PubMed] [Google Scholar]
- 4. Cuschieri A, Lezoche E, Morino M, et al. Multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13(10):952–957. [DOI] [PubMed] [Google Scholar]
- 5. Isla AM, Griniatsos J, Karvounis E, Arbuckle JD. Advantages of laparoscopic stented choledochorrhaphy over T-tube placement. Br J Surg. 2004;91(7):862–866. [DOI] [PubMed] [Google Scholar]
- 6. Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. [DOI] [PubMed] [Google Scholar]
- 7. Hauer-Jensen M, Kåresen R, Nygaard K, et al. Predictive ability of choledocholithiasis indicators. A prospective evaluation. Ann Surg. 1985;202:64–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Neuhaus H, Feussner H, Ungeheuer A, Hoffmann W, Siewert JR, Classen M. Prospective evaluation of the use of endoscopic retrograde cholangiography prior to laparoscopic cholecystectomy. Endoscopy. 1992;24(9):745–749. [DOI] [PubMed] [Google Scholar]
- 9. Liu TH, Consorti ET, Kawashima A, et al. Patient evaluation and management with selective use of magnetic resonance cholangiography and endoscopic retrograde cholangiopancreatography before laparoscopic cholecystectomy. Ann Surg. 2001;234(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barkun AN, Barkun JS, Fried GM, et al. Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. Ann Surg. 1994;220:32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morino M, Baracchi F, Miglietta C, Furlan N, Ragona R, Garbarini A. Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients with gallbladder and bile duct stones. Ann Surg. 2006;244(6):889–893; discussion 893–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lu J, Cheng Y, Xiong XZ, Lin YX, Wu SJ, Cheng NS. Two-stage vs single-stage management for concomitant gallstones and common bile duct stones. World J Gastroenterol. 2012;18(24):3156–3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Martin IG, Curley P, McMahon MJ. Minimally invasive treatment for common bile duct stones. Br J Surg. 1993;80(1):103–106. [DOI] [PubMed] [Google Scholar]
- 14. Phillips EH, Liberman M, Carroll BJ, Fallas MJ, Rosenthal RJ, Hiatt JR. Bile duct stones in the laparoscopic era Is preoperative sphincterotomy necessary? Arch Surg. 1995;130(8):880–886. [DOI] [PubMed] [Google Scholar]
- 15. Cuschieri A, Croce E, Faggioni A, et al. EAES ductal stone study. Preliminary findings of multi-center prospective randomized trial comparing two-stage vs single-stage management. Surg Endosc. 1996;10(12):1130–1135. [DOI] [PubMed] [Google Scholar]
- 16. Fanelli RD, Gersin KS. Laparoscopic endobiliary stenting: a simplified approach to the management of occult common bile duct stones. J Gastrointest Surg. 2001;5(1):74–80. [DOI] [PubMed] [Google Scholar]
- 17. Petelin JB. Laparoscopic approach to common duct pathology. Am J Surg. 1993;165(4):487–491. [DOI] [PubMed] [Google Scholar]
- 18. Memon MA, Hassaballa H, Memon MI. Laparoscopic common bile duct exploration: the past, the present, and the future. Am J Surg. 2000;179(4):309–315. [DOI] [PubMed] [Google Scholar]
- 19. DePaula AL, Hashiba K, Bafutto M, Machado C, Ferrari A, Machado MM. Results of the routine use of a modified endoprosthesis to drain the common bile duct after laparoscopic choledochotomy. Surg Endosc. 1998;12(7):933–935. [DOI] [PubMed] [Google Scholar]
- 20. Leida Z, Ping B, Shuguang W, Yu H. A randomized comparison of primary closure and T-tube drainage of the common bile duct after laparoscopic choledochotomy. Surg Endosc. 2008;22(7):1595–1600. [DOI] [PubMed] [Google Scholar]
- 21. Wills VL, Gibson K, Karihaloot C, Jorgensen JO. Complications of biliary T-tubes after choledochotomy. ANZ J Surg. 2002;72(3):177–180. [DOI] [PubMed] [Google Scholar]
- 22. Bernstein DE, Goldberg RI, Unger SW. Common bile duct obstruction following T-tube placement at laparoscopic cholecystectomy. Gastrointest Endosc. 1994;40(3):362–365. [DOI] [PubMed] [Google Scholar]
- 23. Gersin KS, Fanelli RD. Laparoscopic endobiliary stenting as an adjunct to common bile duct exploration. Surg Endosc. 1998;12(4):301–304. [DOI] [PubMed] [Google Scholar]
- 24. Berci G, Morganstern L. Laparoscopic management of common bile duct stones. A multi-institutional SAGES study. Surg Endosc. 1998;1168–l174. [DOI] [PubMed] [Google Scholar]
- 25. Cuschieri A. Ductal stones: pathology, clinical manifestations, laparoscopic extraction techniques, and complications. Semin Laparosc Surg. 2000;7(4):246–261. [PubMed] [Google Scholar]
- 26. Fanelli RD, Gersin KS, Mainella MT. Laparoscopic endobiliary stenting significantly improves success of postoperative endoscopic retrograde cholangiopancreatography in low-volume centers. Surg Endosc. 2002;16(3):487–491. [DOI] [PubMed] [Google Scholar]
- 27. Mangla V, Chander J, Vindal A, Lal P, Ramteke VK. A randomized trial comparing the use of endobiliary stent and T-tube for biliary decompression after laparoscopic common bile duct exploration. Surg Laparosc Endosc Percutan Tech. 2012;22(4):345–348. [DOI] [PubMed] [Google Scholar]