Abstract
Background
Treatment of acute heart failure in the emergency department (ED) or observation unit is an alternative to hospitalization. Both ED and observation unit management have been associated with reduced costs and may be used to avoid penalties related to rehospitalizations. The purpose of this study was to examine trends in ED visits for heart failure and disposition following such visits.
Methods
We used the National Hospital Ambulatory Medical Care Survey, a representative sample of ED visits in the United States, to estimate rates and characteristics of ED visits for heart failure between 2002 and 2010. The primary outcome was the discharge disposition from the ED. Regression models were fit to estimate trends and predictors of hospitalization and admission to an observation unit.
Results
The number of ED visits for heart failure remained stable over the period, from 914,739 in 2002 to 848,634 in 2010 (annual change −0.7%; 95% CI −3.7% – +2.5%). Of these visits, 74.2% led to hospitalization while 3.1% led to observation unit admission. The likelihood of hospitalization did not change during the period (adjusted prevalence ratio 1.00; 95% CI 0.99–1.01 for each additional year) while admission to the observation unit increased annually (adjusted prevalence ratio 1.12; 95% CI 1.01–1.25). We observed significant regional differences in likelihood of hospitalization and observation admission.
Conclusions
The number of ED visits for heart failure and high proportion of ED visits with subsequent inpatient hospitalization have not changed in the last decade. Opportunities may exist to reduce hospitalizations by increasing short term management of heart failure in the ED or observation unit.
Keywords: heart failure, emergency department, hospitalization, observation unit
Acute heart failure accounts for over 1 million hospitalizations annually and is one of the most common causes of 30 day rehospitalization in the United States.1, 2 To reduce the morbidity and costs associated with these hospitalizations, policy makers and hospitals have implemented various strategies to improve quality of care and reduce rehospitalizations in heart failure. 3, 4 The Centers for Medicare and Medicaid Services (CMS) began publicly reporting heart failure rehospitalization rates in 2009 and subsequently established financial penalties for hospitals with high rates of rehospitalization within 30 days of the index hospitalization.4
One potential hospital strategy to reduce heart failure hospitalizations and rehospitalizations is to reduce the percentage of patients who are admitted to the hospital after an emergency department (ED) visit for heart failure. Although the majority of hospitalizations for heart failure begin in the ED,5 some patients with acute heart failure may be adequately treated and discharged from the ED.6 Accordingly, short term treatment of heart failure patients in the ED, with close outpatient follow up management, has been proposed as a viable strategy to reduce hospitalizations.6, 7
The observation unit has been used as an alternative to hospitalization for short term monitoring and management of heart failure.8–10 Observation unit stays are considered outpatient encounters, and, therefore, avoid penalties for rehospitalizations.11 Observation units are also associated with significant cost saving to hospitals and payers when compared to hospitalizations.8 As a result, admissions to observation units may be increasingly serving as substitutes for hospitalizations.
The purpose of this study was to examine trends in the number and disposition of ED visits for heart failure between 2002 and 2010. Given increasing policy pressure to reduce rehospitalizations for heart failure, we hypothesized that ED providers would be less likely to hospitalize patients with heart failure over time, with some of the decrease attributable to a concurrent increase in admissions to the observation unit. We further hypothesized that the overall number of ED visits for heart failure would decrease due to improvements in treatments and care for patients with heart failure in the last two decades. 12–15
Methods
We studied trends in ED visits between 2002 and 2010 using the National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS represents an annual, national probability sample of ED visits to non-federal, short-stay hospitals in the United States and is conducted annually by the National Center for Health Statistics (NCHS). 16
For the current study, we included ED visits of patients 18 years and older for heart failure. In NHAMCS, surveyors abstract diagnoses from the chart, which are later mapped to International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes by NCHS staff. We considered an ED visit to be for heart failure if an appropriate ICD-9-CM code (402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, and 4282, 17) was either 1) the first listed diagnosis or 2) the second or third listed diagnosis if the first diagnosis was related to a symptom of heart failure, such as shortness of breath or edema (appendix table). Only the first three ED diagnoses are recorded in NHAMCS, despite the possibility that some visits had additional diagnosis codes.
Patient characteristics included age, gender, race, ethnicity, insurance, initial systolic blood pressure, initial heart rate, comorbid conditions, hospital ownership, and hospital region. Race was categorized as Black/African-American and other, ethnicity was categorized as Hispanic/Latino and other, and insurance was categorized as Medicaid and other. Initial systolic blood pressure was categorized as <115,115–160, and >160 based on published risk classification for heart failure patients in the ED. 18 Initial heart rate was categorized as <100 and ≥100. Comorbid conditions were based on the Agency for Healthcare Research and Quality (AHRQ) Clinical Classification Software definitions. As NHAMCS records only three diagnosis codes and inclusion in this study required at least one code be for heart failure, patients could have at most two comorbid conditions. Hospital region was defined by NHAMCS as Northeast, Midwest, South, and West and was based on those used by the US Census Bureau. 16
The primary outcome was the discharge disposition made by ED providers. In NHAMCS, patients can receive multiple discharge dispositions. To reflect immediate ED disposition, we a priori categorized disposition in mutually exclusive groups according to the following hierarchy: dead on arrival or died in ED, admit to observation, admit to hospital, transfer to another facility, routine discharge, left before being seen or left against medical advice (AMA), and other or missing disposition. For the principal analysis of discharge disposition, we excluded visits with categories of died, left AMA, and other as these categories do not reflect provider decision making options for disposition; these three categories accounted for 1.6% of all ED visits in our cohort. In NHAMCS, the description for admit to observation unit changed slightly across years: “admit for 24 hour observation” (2002), “admit to the ED for observation” (2003–2004), “admit to observation unit” (2005–2008), and both “admit to observation unit, then hospitalized” and “admit to observation unit, then discharged” (2009–2010). The description for hospital admission remained consistent throughout the period. Routine discharge included options such as “no follow up given”, “return if needed”, and “return or follow up with physician”.
This study was supported by the National Center for Advancing Translational Sciences (NCATS) grant KL2 TR000053 and the National Heart Lung and Blood Institute grant K23 HL116787.
Statistical Analysis
All analyses accounted for the complex sampling design of the NHAMCS. Descriptive statistics for ED visits were presented across three year periods. We used chi-squared and analysis of variance (ANOVA) tests to evaluate differences in categorical and continuous variables across year categories.
To estimate the annual change in number of ED visits across years, we developed a simulation model to account for the variance in yearly estimates.19 First, we defined a normal distribution of visits for each year, with mean and variance based on the estimates from NHAMCS. Next, we randomly sampled from each year’s distribution to generate a number of visits for each year. A Poisson regression was then fit with the generated values as the dependent variable and year as the independent variable. These two steps were repeated 2,500 times. The mean and standard deviation of the 2,500 beta coefficients for year were used to provide a point estimate and standard error for the annual change in number of ED visits. A similar procedure was performed to estimate the census adjusted change in ED visits, with the addition of an offset of the log of the United States population age 18 or over in the Poisson model. Annual population estimates were obtained from the U.S. Census Bureau.20, 21 We examined age and sex adjusted change in ED visits by determining the distribution of ED visits and population for three age and two sex categories across years. We fit a Poisson regression with the dependent variable as a sample from the distribution of ED visits for each age and gender category, the independent variables as year, age category, and sex, and an offset of the log of the US population for the age/sex category. As above, this procedure was repeated 2,500 times to obtain estimates for annual change in visits. We noted an interaction between sex and year, so results were similarly presented for each age/sex category.
We developed univariate and multivariate regression models to estimate the change in the likelihood of decision for hospitalization during the study period. Given the high frequency of the disposition of hospitalization, Poisson regression was used to estimate a prevalence ratio.22 We reported on the association between all covariates in the model and likelihood of hospitalization. These covariates included: age, gender, race, ethnicity, insurance, systolic blood pressure, heart rate, diabetes, acute myocardial infarction (MI), cardiac dysrhythmias, pneumonia, chronic obstructive pulmonary disease (COPD), asthma, acute or chronic kidney disease, dementia, hospital ownership, and hospital region. A similar procedure was used to estimate the change in likelihood of admission to observation unit during the study period. Analyses were performed using Stata version 12 (College Station, Texas).
Results
Between 2002 and 2010, there were 2,158 emergency department visits for heart failure in NHAMCS, representing 7,438,175 such visits in the United States. Of these visits, 84.7% had a primary diagnosis of heart failure, while 15.3% had a secondary diagnosis of heart failure with a primary diagnosis of a heart failure related symptom. The mean (SE) age of patients (71.7 (0.5) years) did not differ during the study period (Table 1). There were a greater number of total ED visits for females versus males overall (51.0% vs. 49.0%), although the proportion of males significantly increased between 2002 and 2010. There were significant increases in the documented prevalence of kidney disease and the percentage of Medicaid beneficiaries who visited the ED during the study period (Table 1).
Table 1.
Baseline characteristics of emergency department (ED) visits for heart failure in the United States.
| 2002–2004 | 2005–2007 | 2008–2010 | p | |
|---|---|---|---|---|
| ED Visits Unweighted, n | 737 | 691 | 730 | |
| ED Visits Weighted, n | 2,538,821 | 2,381,560 | 2,517,794 | |
| Age, Mean (SE) | 72.3 (0.6) | 71.8 (0.8) | 71.2 (0.7) | 0.57 |
| Age Category | 0.66 | |||
| 18–49 | 9.0 | 8.3 | 10.2 | |
| 50–64 | 19.4 | 20.3 | 23.1 | |
| 65–74 | 20.3 | 21.1 | 16.6 | |
| 75–84 | 30.4 | 29.1 | 28.1 | |
| ≥85 | 20.9 | 21.2 | 22.0 | |
| Gender | <0.01 | |||
| Female | 57.5 | 47.7 | 47.5 | |
| Male | 42.5 | 52.3 | 52.5 | |
| Black/African American Race | 20.1 | 22.6 | 25.1 | 0.28 |
| Hispanic/Latino Ethnicity | 5.8 | 5.4 | 7.0 | 0.48 |
| Medicaid Insurance | 10.5 | 20.1 | 21.0 | <0.001 |
| Heart Rate, beats/min | 0.17 | |||
| <100 | 73.5 | 71.8 | 67.6 | |
| ≥100 | 26.5 | 28.2 | 32.4 | |
| Systolic Blood Pressure, mmHG | 0.98 | |||
| <115 | 16.5 | 15.9 | 15.2 | |
| 115–160 | 52.5 | 54.0 | 54.0 | |
| >160 | 31.0 | 30.1 | 30.8 | |
| Comorbid Conditions | ||||
| Diabetes | 5.3 | 2.9 | 4.0 | 0.25 |
| Acute Myocardial Infarction | 2.6 | 2.4 | 0.9 | 0.24 |
| Cardiac Dysrhythmias | 7.1 | 4.9 | 5.4 | 0.36 |
| Pneumonia | 5.4 | 6.0 | 5.4 | 0.88 |
| COPD | 7.7 | 8.8 | 7.7 | 0.78 |
| Asthma | 0.8 | 1.1 | 0.5 | 0.45 |
| Kidney Disease | 2.6 | 3.9 | 6.4 | 0.02 |
| Dementia | 0.6 | 0.1 | 0.3 | 0.45 |
| Region | 0.72 | |||
| Northeast | 21.0 | 21.6 | 18.7 | |
| Midwest | 28.9 | 25.3 | 26.1 | |
| South | 31.7 | 34.5 | 38.8 | |
| West | 18.3 | 18.6 | 16.4 | |
| Hospital Ownership | 0.76 | |||
| Voluntary, non-profit | 79.0 | 81.1 | 80.2 | |
| Government, non-Federal | 13.4 | 10.0 | 12.6 | |
| Proprietary | 7.6 | 8.9 | 7.2 | |
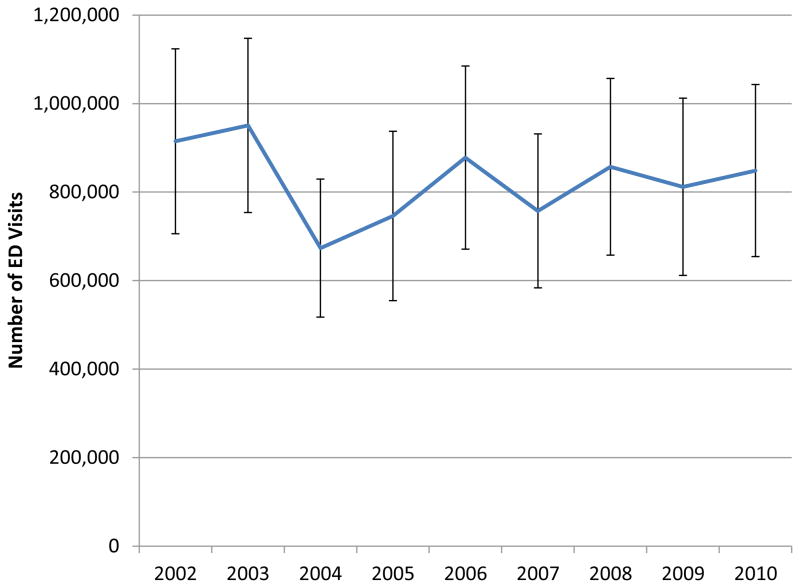
The number of ED visits for heart failure remained relatively stable over the period, from 914,739 (705,820–1,123,658) in 2002 to 848,634 (95% CI 654,255–1,043,013) in 2010 (Figure 1). The annual change in number of ED visits was −0.7% (95% CI −3.7% – +2.5%) from 2002 to 2010. The rate of ED visits for the U.S. population aged 18 and above was 42.6 (95% CI 32.9–52.3) per 10,000 people in 2002 and 36.1 (95% CI 27.8–44.3) per 10,000 people in 2010. There was a nonsignificant decrease in the rate of ED visits per population (annual change −1.7%, 95% CI −4.8% – +1.4%) as well as a decrease in age and sex-adjusted rate of ED visits that neared statistical significance (annual change −2.2%, 95% CI −4.4% – +0.1%). We found a significant interaction between year and sex. There was no change in rates of ED visits for males (annual change 0.8%, 95% CI −2.4% – +4.2%) or women below age 65 (0.1%, 95% CI −6.1% – +6.8%). However, there was an annual decrease of 6.6% (95% CI 2.4% – 10.5%) in ED visits per population of women age 65 and older.
Figure 1.
Temporal trends in the number of emergency department (ED) visits for heart failure in the United States, 2002–2010.
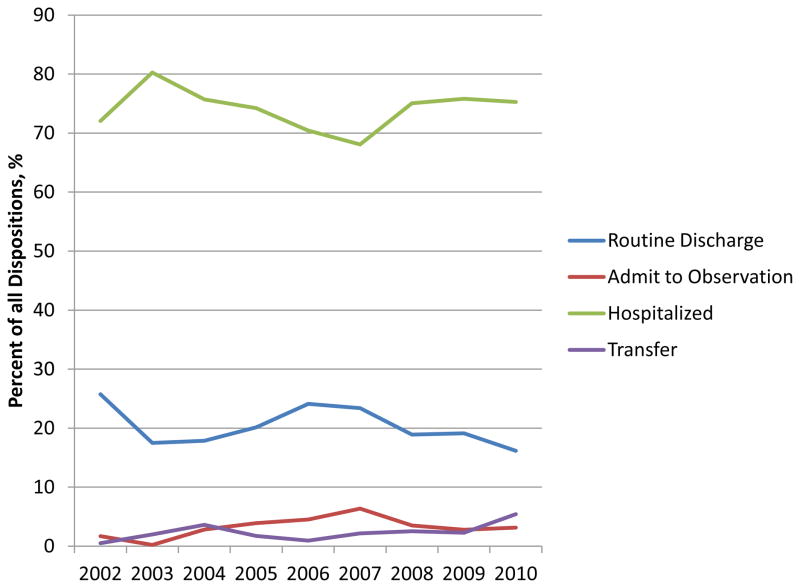
During the study period, 0.2% of patients with heart failure either died in the ED or were dead on arrival. After excluding patients who left AMA (0.5%) and/or had disposition labeled as other or missing (0.9%), ED providers made a decision regarding disposition for 98.4% of encounters, which represents 7,320,462 visits for heart failure between 2002 and 2010. Of these visits, 74.2% of patients were initially admitted to the hospital while 20.3% of patients were discharged. Admissions to the observation unit accounted for 3.1% of ED dispositions and transfer to an outside facility accounted for the remaining 2.3% of ED visits during the study period. The distribution of disposition decision making was similar across years (p=0.14, Figure 2).
Figure 2.
Temporal trends in disposition following an emergency department (ED) visit for heart failure, among 2,118 unweighted visits (7,320,462 weighted visits) which required ED provider to make a disposition decision.
The likelihood of hospitalization did not change during the period, with a prevalence ratio of hospitalization of 1.00 (95% CI 0.99–1.01) for each additional year. In multiple regression analysis, year of study was not associated with likelihood of hospitalization (adjusted prevalence ratio 1.00; 95% CI 0.99–1.01). Characteristics associated with the decision for hospitalization included female gender, Hispanic/Latino ethnicity, tachycardia, diabetes, and acute MI (Table 2). Hospitals located in the Northeast region of the country and hospitals that were voluntary and non-profit were also associated with increased likelihood of hospitalization (Table 2).
Table 2.
Association of patient and emergency department (ED) characteristics with likelihood of hospitalization and likelihood of admission for observation.
| Adjusted* Prevalence Ratio for Hospitalization | Adjusted* Prevalence Ratio for Observation | |
|---|---|---|
| Year | 1.00 (0.99,1.01) | 1.12 (1.01,1.25)† |
| Age Category | ||
| 18–49 | 1 [ref] | 1 [ref] |
| 50–64 | 1.11 (0.97,1.28) | 0.82 (0.22,3.01) |
| 65–74 | 1.01 (0.87,1.17) | 1.56 (0.41,5.98) |
| 75–84 | 1.06 (0.92,1.22) | 1.51 (0.41,5.59) |
| ≥85 | 1.06 (0.91,1.24) | 0.68 (0.18,2.53) |
| Gender | ||
| Male | 1 [ref] | 1 [ref] |
| Female | 1.08 (1.01,1.15)† | 0.70 (0.37,1.31) |
| Black/African American Race | 0.94 (0.86,1.02) | 0.82 (0.37,1.81) |
| Hispanic/Latino Ethnicity | 1.12 (1.01,1.25)† | 0.45 (0.06,3.39) |
| Medicaid Insurance | 1.03 (0.95,1.12) | 0.70 (0.31,1.57) |
| Heart Rate, beats/min | ||
| <100 | 1 [ref] | 1 [ref] |
| ≥100 | 1.11 (1.04,1.19)‡ | 1.64 (0.85,3.13) |
| Systolic Blood Pressure, mmHg | ||
| <115 | 1 [ref] | 1 [ref] |
| 115–160 | 0.99 (0.91,1.08) | 0.87 (0.40,1.91) |
| >160 | 0.98 (0.88,1.09) | 0.89 (0.31,2.57) |
| Comorbid Conditions | ||
| Diabetes | 1.15 (1.04,1.28)‡ | 0.13 (0.02,1.03) |
| Acute Myocardial | ||
| Infarction | 1.20 (1.10,1.31)§ | 1.11 (0.23,5.36) |
| Cardiac Dysrhythmias | 1.01 (0.88,1.16) | 0.21 (0.05,0.95)† |
| Pneumonia | 1.10 (0.98,1.25) | 0.31 (0.09,1.11) |
| COPD | 0.98 (0.87,1.11) | 0.67 (0.23,1.96) |
| Asthma | 1.07 (0.87,1.32) | 1.78 (0.37,8.59) |
| Kidney Disease | 1.10 (0.93,1.29) | 0.35 (0.09,1.31) |
| Dementia | 0.53 (0.28,1.02) | 6.88 (0.73,64.50) |
| Region | ||
| Northeast | 1 [ref] | 1 [ref] |
| Midwest | 0.91 (0.84,0.98)† | 2.90 (1.20,7.01)† |
| South | 0.84 (0.77,0.92)§ | 1.20 (0.39,3.70) |
| West | 0.86 (0.79,0.95)‡ | 3.21 (1.06,9.72)† |
| Hospital Ownership | ||
| Voluntary, non-profit | 1 [ref] | 1 [ref] |
| Government, non-Federal | 0.84 (0.74,0.95)‡ | 1.02 (0.47,2.22) |
| Proprietary | 0.87 (0.73,1.04) | 1.13 (0.34,3.71) |
Adjusted for other variables in the table,
p<0.05,
p<0.01,
p<0.001
In unadjusted analysis, each year was associated with a 10% (95% CI 0–21%) increase in the likelihood of admission to the observation unit; results were similar after adjustment for covariates (adjusted prevalence ratio 1.12; 95% CI 1.01–1.25). The only other characteristics associated with observation unit admission were cardiac dysrhythmias and region of the country. In comparison to hospitals from the Northeast region, hospitals from other regions were associated with an increased likelihood of admission to an observation unit (Table 2). Between 2002 and 2010, 35.9% of the patients who were initially categorized as observation were subsequently hospitalized.
Conclusion
Between 2002 and 2010, there were over 800,000 annual ED visits for heart failure in the United States. We found no appreciable change in the number of annual ED visits for heart failure during this period, despite both improvements in treatments for heart failure patients12–15 and a concurrent reduction in the number of hospitalizations for acute heart failure over the last decade. 2, 23 For comparison, ED visits for heart failure had been increasing between 1992 and 2001;24 we are unaware of studies examining trends in ED visits for heart failure in other countries.
In addition to finding no change in the number of ED visits for heart failure, we found no change in the rate of hospitalization following ED visits for heart failure. These findings suggest that the number of heart failure hospitalizations originating from the ED has remained stable. While these findings seem surprising given the trend of reduced number of hospitalizations for heart failure,2, 23 they complement a recent report from the RAND Corporation.25 In that report, an increase in ED visits for ambulatory sensitive conditions between 2000 and 2009 was offset by a decrease in direct hospitalizations from other outpatient settings, resulting in no change in the total number of hospitalizations for these conditions. Based on physician interviews, the authors of the report hypothesized that these trends were related to outpatient physicians increasingly referring patients to the ED rather than directly to the inpatient hospital setting. While we are unable to determine trends in referrals from an outpatient physician to the ED, it is notable that most demographic and clinical characteristics of patients did not change over time. These finding may suggest that the acuity of ED visits for heart failure has not changed over time and, thus, would not account for the trends in number of patients hospitalized following an ED visit for heart failure. We did observe a substantial reduction in the population adjusted rates of ED visits among older women; further investigation is warranted to understand why this subgroup experienced improvements in ED related outcomes in heart failure.
ED providers play an increasing role in the decision making process related to hospitalization5 and thus may have the opportunity to reduce utilization of hospital resources. 26 Improved tools for risk stratification and enhanced systems for post discharge transition of care may increase the number of patients who are safe either for discharge to home or for brief stay in an observation unit.26, 27 While we found no change in the number of patients discharged to home in our study, the likelihood of admission to an observation unit increased by 12% annually between 2002 and 2010 after adjustment for covariates. Due to the relatively small number of admissions to the observation unit, this increase did not significantly change the number of patients with heart failure who were hospitalized from the ED.
Despite the significant growth in utilization of the observation unit in our study, the overall number of admissions to observation was low and represented just 3.1% of all ED visits in which a provider made a disposition decision for heart failure. It has been estimated that 50% of patients seen in the ED for heart failure can be managed in the observation unit.28 Small studies have suggested that admission to an observation unit is safe and effective for most patients with heart failure, although larger randomized trials are needed.7, 28 Admission to the observation unit has been associated with a significant reduction in costs related to heart failure.9 Our findings suggest that there is substantial opportunity to increase the use of observation unit for heart failure patients and thus reduce significant heart failure related hospital morbidity and cost.
We found region of the country to be one of the strongest predictors of likelihood of hospitalization following an ED visit for heart failure. Specifically, patients seen in the Northeast region were 10–20% more likely to be hospitalized in comparison to patients from other regions of the country. Concurrently, ED visits in the Midwest and West were associated with three times the likelihood of observation admission when compared to Northeast, suggesting that one component of regional differences in hospital disposition may be related to use of the observation unit. Chen and colleagues previously reported regional differences in heart failure hospitalizations rates among Medicare patients. 23 Although the causes of regional differences in hospitalization rates are likely to be multifactorial, our study suggests that one component may be differences in ED practice related to the decision for hospitalization.
In our study, 3.1% of ED visits led to an observation unit admission. We were unable to evaluate the prevalence of patients who were admitted, more broadly, to observation services. Observation services reflect outpatient care delivered in a hospital setting, including care both within and outside of a dedicated observation unit;29 of note, the financial benefits of observation services have primarily been demonstrated in dedicated units. 8, 9, 29 While NHAMCS specifically surveys for admission to the observation unit, one study suggested that the observation disposition in NHAMCS may include admissions outside of a dedicated unit.30 Such potential misclassification would have led us to overestimate the percent of visits that resulted in an observation unit admission. This potential misclassification would, therefore, imply that there is even greater opportunity to manage patients in an observation unit than our findings suggest.
Additional limitations of our study design deserve consideration in the interpretation of our findings. First, the descriptions of some variables in NHAMCS were modified over time. In particular, the language related to admit to observation unit changed twice during the period. It is unlikely that these changes substantially contributed to our findings as similar growth in observation admissions was observed in NHAMCS in the years when the description remained stable.10 Given changes in the definition and the small number of observation unit admissions in NHAMCS, additional information is needed to better characterize these admissions for heart failure. Second, the dataset lacked a number of important variables that are likely related to clinical decision making in the ED, including ejection fraction, comorbidities, creatinine, troponin, and social support. Third, we were unable to assess the effect of disposition on clinically important outcomes such as rehospitalization and mortality. Fourth, because NHAMCS does not include individual identifiers, we were unable to evaluate trends in the number of unique patients who visited an ED for heart failure or trends in repeat ED visits for heart failure. Fifth, although the NHAMCS survey represents a national probability sample of ED visits in the United States, the dataset is a sample and may not fully reflect all ED visits. Sixth, although demographic and clinical characteristics were stable during the study period, we were unable to determine whether patient acuity, a presumed contributor to discharged disposition, changed over time. Seventh, the NHAMCS dataset only describes location within one of four United States regions. While our findings of regional differences likely speak to local difference in health care delivery, such as local provider practice and regional variations in patient preferences, we were unable to describe these differences within a more specific region, such as hospital referral region. Finally, this study did not account for the ongoing effects of policy changes, including public reporting and financial penalties for heart failure rehospitalizations,4 on ED disposition as NHAMCS data was only available through 2010.
Despite the recent trend of a reduction in the number of acute heart failure hospitalizations, the number of heart failure related ED visits has remained unchanged in the United States. Additionally, the proportion of patients admitted to the hospital from the ED has not changed in the last decade, suggesting that an increasing number of hospitalizations for acute heart failure originate in the ED. Opportunities may exist to reduce the substantial morbidity and costs related to heart failure hospitalizations by increasing the number of patients acutely managed in the ED and discharged to home or admitted for short term observation. Further research is needed to assist with risk stratification for appropriate disposition and to compare the outcomes of ED patients who are admitted to an observation unit versus those who are hospitalized.
Acknowledgments
Funding Sources
Dr. Blecker was supported by the National Center for Advancing Translational Sciences (NCATS) grant KL2 TR000053. Dr. Ladapo was supported by the National Heart Lung and Blood Institute grant K23 HL116787.
Footnotes
Disclosures
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure-associated hospitalizations in the United States. Journal of the American College of Cardiology. 2013;61(12):1259–67. doi: 10.1016/j.jacc.2012.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley EH, Curry L, Horwitz LI, Sipsma H, Thompson JW, Elma M, et al. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. Journal of the American College of Cardiology. 2012;60(7):607–14. doi: 10.1016/j.jacc.2012.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent? Circulation. 2012;126(4):501–6. doi: 10.1161/CIRCULATIONAHA.112.125435. [DOI] [PubMed] [Google Scholar]
- 5.Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. The New England journal of medicine. 2012;367(5):391–3. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 6.Weintraub NL, Collins SP, Pang PS, Levy PD, Anderson AS, Arslanian-Engoren C, et al. Acute heart failure syndromes: emergency department presentation, treatment, and disposition: current approaches and future aims: a scientific statement from the American Heart Association. Circulation. 2010;122(19):1975–96. doi: 10.1161/CIR.0b013e3181f9a223. [DOI] [PubMed] [Google Scholar]
- 7.Peacock WFt, Remer EE, Aponte J, Moffa DA, Emerman CE, Albert NM. Effective observation unit treatment of decompensated heart failure. Congest Heart Fail. 2002;8(2):68–73. doi: 10.1111/j.1527-5299.2002.01519.x. [DOI] [PubMed] [Google Scholar]
- 8.Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3. 1 billion a year. Health Aff (Millwood) 2012;31(10):2314–23. doi: 10.1377/hlthaff.2011.0926. [DOI] [PubMed] [Google Scholar]
- 9.Peacock WF. Using the emergency department clinical decision unit for acute decompensated heart failure. Cardiol Clin. 2005;23(4):569–88. viii. doi: 10.1016/j.ccl.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Venkatesh AK, Geisler BP, Gibson Chambers JJ, Baugh CW, Bohan JS, Schuur JD. Use of observation care in US emergency departments, 2001 to 2008. PloS one. 2011;6(9):e24326. doi: 10.1371/journal.pone.0024326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feng Z, Wright B, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood) 2012;31(6):1251–9. doi: 10.1377/hlthaff.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. The New England journal of medicine. 2004;350(21):2140–50. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 13.Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA. 1995;273(18):1450–6. [PubMed] [Google Scholar]
- 14.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. The New England journal of medicine. 1999;341(10):709–17. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 15.Fonarow GC, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF) Circulation. 2010;122(6):585–96. doi: 10.1161/CIRCULATIONAHA.109.934471. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. [Accessed July 20, 2014];About the Ambulatory Health Care Surveys. Available at: http://www.cdc.gov/nchs/ahcd/about_ahcd.htm.
- 17.Bonow RO, Ganiats TG, Beam CT, Blake K, Casey DE, Jr, Goodlin SJ, et al. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. Circulation. 2012;125(19):2382–401. doi: 10.1161/CIR.0b013e3182507bec. [DOI] [PubMed] [Google Scholar]
- 18.Peacock WF, Braunwald E, Abraham W, Albert N, Burnett J, Christenson R, et al. National Heart, Lung, and Blood Institute working group on emergency department management of acute heart failure: research challenges and opportunities. Journal of the American College of Cardiology. 2010;56(5):343–51. doi: 10.1016/j.jacc.2010.03.051. [DOI] [PubMed] [Google Scholar]
- 19.Robert CP, Casella G. Monte Carlo statistical methods. New York: Springer; 1999. [Google Scholar]
- 20.US Census Bureau. [Accessed July 20, 2014];Annual Estimates of the Resident Population by Sex and Selected Age Groups for the United States: April 1, 2000 to July 1, 2009. Available at: http://www.census.gov/popest/data/historical/2000s/vintage_2009/index.html.
- 21.US Census Bureau. [Accessed July 20, 2014];Annual Estimates of the Resident Population for Selected Age Groups by Sex: April 1, 2010 to July 1, 2012. Available at: http://www.census.gov/popest/data/national/asrh/2012/index.html.
- 22.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157(10):940–3. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 23.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306(15):1669–78. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hugli O, Braun JE, Kim S, Pelletier AJ, Camargo CA., Jr United States emergency department visits for acute decompensated heart failure, 1992 to 2001. Am J Cardiol. 2005;96(11):1537–42. doi: 10.1016/j.amjcard.2005.07.064. [DOI] [PubMed] [Google Scholar]
- 25.Gonzalez Morganti K, Bauhoff S, Blanchard JC, Abir M, Iyer N, Smith A, et al. The Evolving Role of Emergency Departments in the United States: RAND Corporation. 2013 [PMC free article] [PubMed] [Google Scholar]
- 26.Collins S, Storrow AB, Kirk JD, Pang PS, Diercks DB, Gheorghiade M. Beyond pulmonary edema: diagnostic, risk stratification, and treatment challenges of acute heart failure management in the emergency department. Ann Emerg Med. 2008;51(1):45–57. doi: 10.1016/j.annemergmed.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Dunnion ME, Kelly B. From the emergency department to home. J Clin Nurs. 2005;14(6):776–85. doi: 10.1111/j.1365-2702.2005.01129.x. [DOI] [PubMed] [Google Scholar]
- 28.Collins SP, Pang PS, Fonarow GC, Yancy CW, Bonow RO, Gheorghiade M. Is hospital admission for heart failure really necessary?: the role of the emergency department and observation unit in preventing hospitalization and rehospitalization. Journal of the American College of Cardiology. 2013;61(2):121–6. doi: 10.1016/j.jacc.2012.08.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ross MA, Hockenberry JM, Mutter R, Barrett M, Wheatley M, Pitts SR. Protocol-driven emergency department observation units offer savings, shorter stays, and reduced admissions. Health Aff (Millwood) 2013;32(12):2149–56. doi: 10.1377/hlthaff.2013.0662. [DOI] [PubMed] [Google Scholar]
- 30.Wiler JL, Ross MA, Ginde AA. National study of emergency department observation services. Acad Emerg Med. 2011;18(9):959–65. doi: 10.1111/j.1553-2712.2011.01151.x. [DOI] [PubMed] [Google Scholar]