Synopsis
Depression is among the leading causes of decreased disability-adjusted life years in the world1 and a serious public health problem.2 Older adults with DM experience greater risk for comorbid depression compared to those who do not have DM.3 Having DM increases the risk of subsequent development or recurrence of depression. Conversely, history of depression increases the risk for new onset DM.4 As an unwanted co-traveler of DM, undetected, untreated or undertreated depression impinges an individual’s ability to manage their DM successfully, hindering their adherence to treatment regime.5 It also undermines the effectiveness of provider-patient communication and decays therapeutic relationships. Thus, in the context of caring for older adults with DM, comorbid depression presents special challenges and opportunities for clinicians. Moreover, recent studies have suggested that co-occurring depression and DM may accelerate cognitive decline, highlighting the importance of treating depression and DM. Several treatment modalities are available, which can be used to treat and manage depression in primary care settings: pharmaceutical, brief psychotherapeutic, behavioral and life style interventions, and combination therapies. An evidence-based health care delivery model is also available for treating depression in primary care settings. In this article, we summarize the clinical presentation of late-life depression, potential mechanisms of comorbidity of depression and DM, importance of depression in the successful management of DM, and available best practice models for depression treatment.
Keywords: Diabetes, Depression, Mood disorders, Aging, Collaborative Care
Introduction
Diabetes mellitus (DM) is one of the most common chronic conditions among older adults. About 26.9%, or 10.9 million U.S. residents aged 65 years and older had diabetes in 2010.6 Depressive disorders are serious chronic diseases that increase morbidity and mortality,7 erode quality of life,8 and increase medical expenditure. Depression and DM often co-occur. Data from a range of settings suggest that the prognosis of both DM and depression—in terms of severity of disease, complications, treatment resistance and mortality—is worse for either disease when they are co-morbid than when they occur separately. Comorbid depression in patients with DM is strongly associated with increased burdens of DM symptoms9, poor self-management and treatment adherence10, increase in health care services utilization and medical expenditures11 and an increased risk of DM complications.12 DM complications such as myocardial infarction, amputation or loss of vision can in turn precipitate or worsen depressive episodes. Yet, few studies have extensively examined the associations between depression and DM in the older adults populations. Also, recent studies have found that combination of DM and depression may increase the risk for dementia, suggesting increased brain toxicity.13 The purpose of this review is to summarize the clinical presentation of late-life depression among older adults with DM, potential mechanisms of comorbidity of depression and DM, importance of depression in the successful management of DM, and available best practice models for depression treatment.
Disease description
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. To be diagnosed with major depression, a patient must have depressed mood or anhedonia and at least 5 of the following 9 symptoms nearly every day for at least 2 weeks:
Depressed mood
Marked diminished interest/pleasure
Sleep disturbance (increased or decreased sleep)
Appetite disturbance (increased or decreased appetite; typically with weight change)
Fatigue/loss or energy
Diminished concentration or indecisiveness
Feelings of worthlessness or excessive or inappropriate guilt
Psychomotor retardation or agitation (a change in mental and physical speed perceived by other people)
Recurrent thoughts of death or suicide (not just fear of dying)
They must also experience functional impairment related to these depressive symptoms.
Older adults, however, do not always present with the typical symptoms of depression. In particular, depressed or sad mood may be less evident or not even present. In these cases, anhedonia may be better indicator for depression.14,15 Depressed older adults may experience sleep disturbances (sleeping too much or too little) or changes in appetite (eating too much or too little). Decrease in self-efficacy, motivation, and ability to participate in self-care may also indicate underlying depressive symptoms. Signs of such symptoms can be subtle. Older adults may reply with “I don’t know” to simple questions, decline to participate in physical, speech or occupational therapy, and feeling negative or hopeless about treatments offered. Some may easily give up tasks during these therapies. Older adult who experience loss of self-worth or sense of loneliness due to depression, may complain “nobody needs me,” or “I feel I am just in everyone’s way.” The symptoms of late-life depression are often attributed to normal aging, grief, physical illness or dementia and providers and patients miss important opportunities to initiate treatment for what is an treatable health problem.16
The majority of older adults with clinically significant depressive symptoms do not meet standard diagnostic criteria for major depression or dysthymic disorder.17,18 Patients in this group fall short of meeting diagnostic criteria for major depression because of fewer or limited duration of depression symptoms. Nonetheless, studies suggest that these patients carry similar disease burden: poorer health outcomes, functional impairment, and higher health utilization and treatment costs.19-21 Moreover, these patients are at very high risk for subsequently developing major depression and may also develop suicidal ideation.22-24
Although depression can be successfully treated,25 many older adult suffer from a chronic or recurrent depression.26 In a prospective study about courses of major depression, approximately 85% of individuals who recover from depression experience recurrence within 15 years.27 Findings meta-analyses of chronic depression in primary care and community sample suggests that about one in three depressed older adults experience chronic and persist course.28,29 Depressed patients with DM are at greater risk for a chronic course of depression or less complete recovery.30 Such chronicity, in turn, makes it more difficult for older adults and their family caregivers to optimally self-manage DM.
In the older adults with DM, depressive symptoms may be overlooked because they are assumed to be due to concurrent DM and other medical illnesses. Many of the symptoms of depression such as lower energy, fatigue, loss of appetite, and sleep disturbance are also associated with DM. Thus differentiating stress related to DM self-management and depression can be challenging.31 Somatic complaints may suggest presence of depression, especially if they are out of proportion to underling physical disorders.32 Only 25-30% of primary care patients present with purely affective or cognitive symptoms of depression.33
Risk factors
Risk factors for developing depression after age 65 are similar to those in younger individuals and include being female, unmarried, low socioeconomic status, having chronic physical illness, social isolation, a history of depression, and a family history. The risk of major depression increases up to three-fold if a first-degree relative has the illness.34 Additional risk factors that are particularly important in older adults include loss and grief,35 social isolation or limited social support,36 high degrees of family conflict,37,38 and care-taking responsibilities.39 Other risk factors that increase the likelihood of depression in the medically ill elderly include presence of cognitive impairment, age greater than 75, active alcohol abuse, and lower educational attainment.40-49 Table 1 summarized the risk factors for depression in older adults.
Table 1.
Risk Factors for Depression in Older Adults
| Authors, year | Sample | Finding |
|---|---|---|
| Age | ||
| Cole et al (2003)152 | Age≥50 | Meta-analysis of epidemiological studies. Pooled OR for depression associated with age: 1.2 (95% CI: 0.9-1.7) |
| Snowden (2008)153 | Mixed age | Comprehensive review of epidemiological studies: Depression is as common in older age as in earlier life. |
|
| ||
| Being Female | ||
| Cole et al (2003)152 | Age≥50 | Meta-analysis of epidemiological studies. Pooled OR for depression associated with being female: 1.4 (95% CI: 1.2-1.8) |
| Sonnenberg et al (2001)154 |
55≤Age≤85 | A random, age and sex-stratified community sample of 3056 older Dutch people; Prevalence of depression in women was almost twice as high as in men. |
|
| ||
| Grief and Loss | ||
| Zisook et al (1991)155 | Mixed age | Major depression and anxiety disorders are common within the first year of the spouse’s death: 29-58% meet criteria for major depression at one month, 24-30% at two months, and 25% at three months. |
| Cole et al (2003)152 | Age≥50 | Meta-analysis of epidemiological studies. Pooled OR for depression associated with recent bereavement: 3.3 (95% CI: 1.7-4.9) |
| Turkey et al (1999)156 | Age≥70 | The rate of syndromal depression in the newly bereaved was nearly nine times as high as the rate for married individuals, and the rate of depressive symptoms was nearly four times as high. |
|
| ||
| Social Isolation | ||
| Cole et al (2003)152 | Age≥50 | Meta-analysis of epidemiological studies. Pooled OR for depression associated with living alone: 1.7 (95% CI: 0.6-4.7) |
| Prince et al (1998)157 | Age≥65 | Prospective epidemiological study. Lack of contact with friends was a direct risk factor but also modified the association between handicap and depression. |
| Cacioppo et al (2006)158 | Age≥55 | There is a reciprocal relationship between loneliness depressive symptomatology and over time |
|
| ||
| Cognitive impairment | ||
| Cole et al (2003)152 | Age≥50 | Meta-analysis of epidemiological studies. Pooled OR for depression associated with recent bereavement: 2.1 (95% CI: 0.6-8.6) |
Protective factors
Strong and supportive social context has been identified as a protective factor. A compelling body of evidence has shown that social support decreases the risks for depression50,51 and for depression relapse,52 increases adherence to depression treatment, 53,54 and improves treatment outcomes. Social support may have positive effects on psychological wellbeing independent of whether or not individuals are exposed to stress.55,56 Social support may also promote wellbeing through modulation of neuro-endocrine response to stress.57
Social activities, such as volunteering suggested to have positive effect on depression outcomes in older adults.58 Studies have also suggested that religion and spirituality may play an important part in many older adults’ lives and social connectedness and support are an important part of organized religion.59 Religion may allow older adults to experience life as meaningful despite losses and challenges and, thereby, reduce the risk of depression. It is also possible that the positive effect of religion on mental health is mediated by the social connectedness and the social support derived from taking part in religious activities.
Prevalence/Incidence
Depression is one of the most common mental disorders in late-life.60 About one in four U.S. resident projected to experience major depression by age 75.61 In community settings, about 5% of adults aged 65 and older meet research diagnostic criteria of major depression,62,63 with rates of subsyndromal, clinically significant depression estimated at 8% -16%.64 The rates of geriatric depression increase to 12-30% in institutional settings, and up to 50% for residents in long-term care facilities.65,66 Approximately 5-10% of older adults seen in primary care settings have clinically significant depression.67
Variations in prevalence in late-life depression across racial/ethnic group are rarely examined and existing literature present mixed findings. However, given that differences in diabetes prevalence exist by racial/ethnic group, these may be important to appreciate. Cross-sectional and longitudinal epidemiological study showed that Non-Hispanic White and Latino older adults have higher rates of depression.68-70 A longitudinal population study of community-dwelling Hispanic older adults showed approximately 9% of sample met the criteria for lifetime diagnosis of major depression, while 24% of sample reported minor depression.70 The prevalence of depression in African American is generally lower than their White counterparts.71
Minority older adults are less likely to be diagnosed with or treated for depression than their white counterparts.72,73 These health service disparities in minority populations become increasingly complicated when considering cultural beliefs and attitudes towards depression care. Culture influences how individuals experience and express depression.74,75 Minority patients from certain ethnic groups may express their depression somatically than psychologically.33,76 Such somatic presentations may reduce the recognition of depression by primary care providers or leads to the perception of a patient as ‘difficult.’77 Some minorities may also have less faith in the biological etiology of depression, be more skeptical about antidepressant use, and show stronger preferences for counseling than their White counterparts.78,79 When pharmaceutical treatment is the only available option, minority older adults may be less likely to engage in treatment and more likely to be non-adherent. The present primary care systems that focus primarily on pharmacological treatment without considering the unique barriers faced by ethnic and racial minority populations may not affect the pattern of disparities observed.80
Scant information on the cross-national prevalence of late-life depression is available. A report from a World Health Organization concluded that older adults in developed countries had relatively low average depression rates of 2.6% while those in developing countries had an average rate almost three times higher (7.5%).81 The rapid increase in diabetes across the world, particularly in developing countries,82,83 indicate that these international discrepancies are critical to understand.
Among older adults with DM, depression is highly prevalent.84 Up to 30% of individuals with DM have a significant number of depressive symptoms and 12 to 18% meet diagnostic criteria for major depression.3,85 Patients with DM experience significantly higher rates of depression compared with their age- and gender-matched counterparts.84 A meta-analysis of ten studies showed that the prevalence of depression was significantly higher in patients with DM compared with those without (17.6 vs. 9.8%).84 The prevalence of depression was higher in females with diabetes (23.8%) compared with males (12.8%); however, the odds ratio for depression in patients with Type 2 DM compared with those without was higher in males (OR = 1.9, 95% CI 1.7-2.1) than females (OR = 1.3, 95% CI 1.2-1.4).
Depression and mortality in individuals with DM
Based on several meta-analyses, depression is associated 1.5- to 2.6-fold increase of mortality among individuals with in DM.7,86,87 Few studies have examined if treating depression may decrease mortality among individuals with depression. Data from a large clinical trial of collaborative late-life depression treatment program in primary care setting (PROSPECT) showed that evidence-based treatment of depression can reduce mortality rates among those with DM (adjusted hazard ratio 0.49, 95% CI: 0.24-0.98).88 Another study of all cause mortality with same sample also found that patients with major depression in intervention practice were 24% less likely to have died, compared to depressed older adults in usual primary care practices.89
Underlying mechanisms of comorbidity of depression and DM
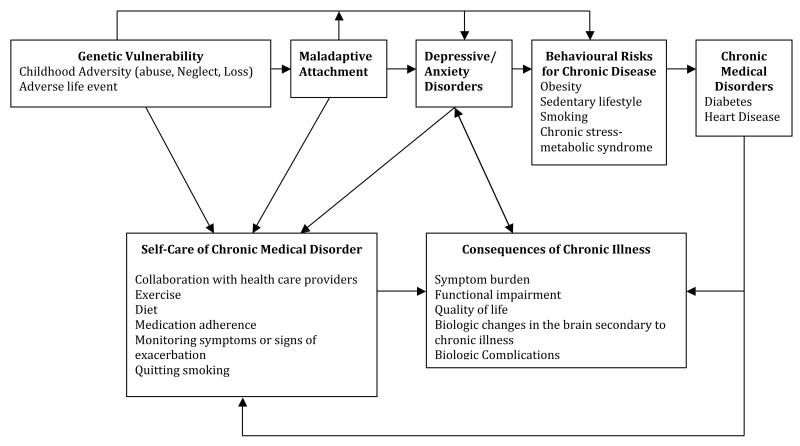
Katon90 proposed a complex bidirectional relationship between depression and type 2 DM (Figure 1). Depression early in adult life is a risk factor for subsequent development of DM.91 The increased risk of DM in patients with depression has been hypothesized to be the result of maladaptive health risk behaviors associated with depression such as smoking, obesity and lack of physical exercise90 as well as psychobiologic factors such as increased cortisol levels, increased inflammatory factors92 and insulin resistance.93
Figure 1. A conceptual model of interaction between major depression and medical illness.
Reproduced from Katon, Wayne J. "Clinical and Health Services Relationships between Major Depression, Depressive Symptoms, and General Medical Illness." Biological Psychiatry 54, no. 3 (2003): 216-26.
On the other hand, DM may increase risk of depression or worsen the depression symptoms due to increased symptom burden, DM complications causing functional impairment and decreased quality of life, as well as vascular brain changes secondary to DM. Comorbid depression has been found to impair the ability to perform self-care activities necessary to control DM by affecting memory, energy level, and executive function.94-96 Lack of self-care and the psychobiologic changes associated with comorbid depression may explain why individuals with comorbid depression experience increased risk of macro- and micro-vascular complications12 and dementia.13
While DM and depression independently associated with memory and cognitive impairment,97-99 recent clinical epidemiological studies found that concurrent DM and depression may have synergistic negative effect on brain health, posing greater risk for developing dementia and Alzheimer’s disease.13 There are several biological mechanisms that can explain such a toxic effect of the DM and depression combination on brain health. First, DM and depression are risk factors for cardiovascular and cerebrovascular diseases (e.g., vascular dementia and Alzheimer’s disease). Concurrent DM and depression may increase risk for cardiovascular and cerebrovascular events in additive fashion.13 Secondly, depression is associated with dysregulation of the hypothalamic-pituitary axis,100,101 which increases glucocorticoid production, and impairs negative feedback. Hypercortisolemia is associated with metabolic syndrome—a risk factor for vascular dementia and Alzheimer’s disease.102-104 Finally, chronic or recurrent depression is associated with hippocampal atrophy.105,106
The temporal relationship between depression and DM has not been fully established. Existing evidence suggests that the association between history of depression and subsequent development of DM is stronger than that between history DM and subsequent development of depression.107 Several prospective epidemiological studies have found that having depression increased risk for developing DM subsequent years by 1.62-to 2.52-fold: Demakakos and colleagues108 analyzed data of 6,111 individuals who reported not having doctor-diagnosed DM at baseline in 2002-2003 and concluded that, after adjusting for several demographic and clinical characteristics, individuals who had greater depressive symptomatology at baseline experienced 1.62-fold increased risk for developing DM in the subsequent 45.8 months. In another longitudinal study of community-residing adult population by Camethon et al, after adjusting for age, race, and gander, the adjusted risk of developing DM in subsequent years are 2.52-fold higher among those with greater depressive symptoms than those with low depressive symptoms.109 A prospective epidemiological study of 1,715 residents of Baltimore Catchment area showed that having major depressive disorder was associated with more than 2-fold increase in risk (adjusted odds ratio: 2.23; 95% CI 0.90-5.55) for developing DM in the subsequent 13 years.110 However, this was not statistically significant.
Having DM increases the risk for developing depression subsequently. A meta-analysis of 11 epidemiological studies concluded that individuals who had Type 2 DM without depression at baseline experienced 1.24-fold increased risk (95% CI 1.09-1.40) for subsequently developing or recurring depression in subsequent years.111 Data from the study of 5,201 multi-racial participants of Women’s Health Across the Nation (SWAN) concluded that having DM increase the odds for developing DM in the subsequent 2 years by 2.8-fold (95% CI: 1.2-6.4) among depressed African American Women.91 Therefore, older adults with diabetes should be considered at higher risk for future depression.
Prevention and early treatment
Prevention and early treatment of depression matter to providers who treat individuals with DM for several reasons. First, as mentioned earlier, having depression may increase the risk for subsequently developing DM. Thus, prevention and early treatment of depression may lower the incidence of DM. Second, having comorbid depression decreases individuals’ ability to successfully self-manage DM and increases likelihood for poor DM outcomes. Thirdly, depression is treatable and several treatment approaches are developed for primary care settings. In a recent clinical trial with 247 older adults112 suggests that both problem solving therapy for primary care (PST-PC) and coaching in health dietary practices could effectively reduce the incidence of major depression in older adults, including in older black adults with high BMI. Despite the fact that black participants in the trial carried a greater risk for depression than did their white counterparts – including obesity –the interventions were equally effective in reducing the incidence of major depression from an expected rate of 20-25% over 2 years to only 8-9%, in both black older adults and white older adults. Thus, given the challenges of treating prevalent depression in people living with both depression an DM mellitus, especially in minority populations –where stigma represents an important barrier, it seems particularly important to develop depression prevention strategies that utilize, variously, active coping strategies and life style interventions that promote health and protective factors.
The U.S. Preventive Services Task Force found at least fair evidence that screening adults for depression improves health outcomes and that benefits outweigh harms (B rating), and recommends screening for depression if practices have systems in place to assure accurate diagnosis, effective treatment, and follow-up.113 Based on these recommendations, the Centers for Medicare & Medicaid Services recently determined to cover annual screening for depression for Medicare beneficiaries in primary care settings with staff-assisted depression care supports.
Treatment strategies
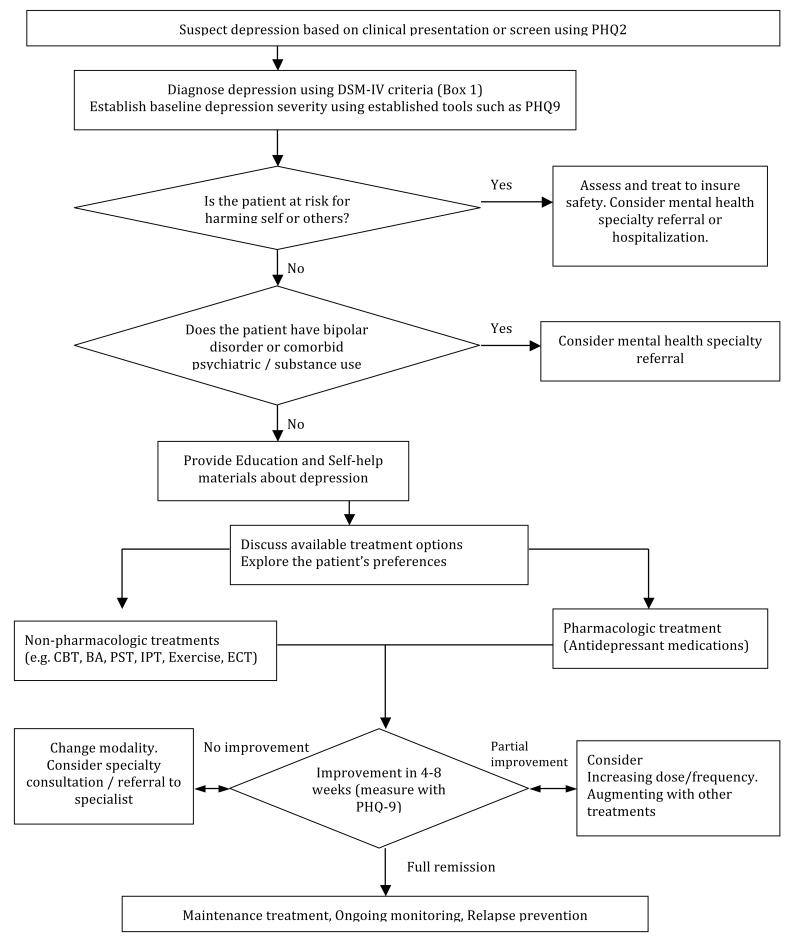
In managing DM, clinicians use several clinical data to establish a baseline and treatment goals – e.g. fasting serum glucose level and HgA1C. The same stepped, measurement-based treatment principles can be applied to treating depression: establishing a baseline; setting clinical and functional goal for depression; and assessing patient’s progress accordingly. Figure 2 illustrates one of widely used clinical guidelines for depression treatment.
Figure 2.
Algorithm for Screening and Treating Depression in Primary Care Setting
Various treatment options are available for late-life depression: antidepressant medications, psychotherapy, or a combination. Other options include exercise programs or other life-style modifying interventions and electroconvulsive therapy (ECT). Several meta-analyses showed that combination therapy is more efficacious than monotherapeutic approaches in treating and in preventing relapse.114-117 In a recent meta-analysis of 14 RCTs of intervention for depression among patient with diabetes, all treatments have shown to be effective in reduction of depressive symptoms (g=−0.51, 95% CI: −0.63, −0.39).118 The pooled effect size was large in psychotherapeutic interventions combined with diabetes self-management education (g= −0.58, 95% CI −0.77, −0.39); and pharmacological treatment showed moderate pooled effect size (g=−0.47; 95% CI −0.67 to −0.27).118 Unlike major depression, subsyndromal depressive conditions have a relatively small evidence base regarding treatments; existing data suggest that available therapies have modest effect sizes when compared to usual care or placebo.16,119,120
Targeting interventions for patients with minor and subsyndromal depression may prove useful as both primary and secondary prevention strategies and clinicians should watch such patients carefully because of the high risk of worsening depression, especially if patients have experienced prior episodes of major depression. Psychosocial treatments may be more helpful than medications for older adults with less severe forms of depression.121
Treatment delivery model for comorbid depression and DM
To date, more than 40 randomized controlled trials have established a robust evidence base for an approach called ’collaborative care models (also called integrated care models).122-125 Recently, several trials of collaborative care model have documented the effectiveness of treating comorbid depression and DM125,126 (e.g., PATHWAY126) and comorbid depression, and DM and/or coronary heart disease (TEAMcare127). In such programs, a depression care manager (usually a nurse or clinical social worker) supports medication management prescribed by PCPs through patient education, close and proactive follow-up, and brief, evidence-based psychosocial treatments such as behavioral activation or problem solving treatment in primary care. The care manager may also facilitate referrals to additional services as needed. A psychiatric consultant regularly (usually weekly) reviews all patients in the care manager’s caseload who are not improving as expected and provides focused treatment recommendations to the patient’s PCP.122,128-130
Tools for assessing and tracking depression
Several tools for assessing depression severity are available and can be easily administered by office staff or physicians during a clinic care visit. The most frequently used tool is the 9-item Patient Health Questionnaire (PHQ-9)131, which systematically explores the 9 DSM-IV132 symptoms of major depression. A score of 10 or greater on the PHQ-9 indicates an elevated level of depressive symptomatology and increased risk of clinically significant depression. PHQ-9 have good sensitivity and specificity (both about 88%) for detecting depressive disorders.133,131
Pharmacological management
Approximately 80% of antidepressant prescribed in the U.S. is prescribed in primary care settings. More than 20 antidepressant medications have been approved by the FDA for treatment of depression in older adults. Newer generations of antidepressants such as SSRIs and SNRIs have more tolerable side effect profile compared to tricyclic antidepressants (TCAs).134,135 Comparing second generation antidepressants, studies found no evidence that specific medications are more effective than others.136 Thus, physicians may discuss the choice of medication with patients and their family. Because of the changes in pharmacokinetics (e.g., decreased renal or hepatic clearance), older adults may require lower doses of medications than their younger counterparts. Furthermore, considering high rates of multimorbidity and polypharmacy among older adults, drug-drug interactions are particular concern in this population. On the other hand, medication doses should be titrated upwards to full adult doses in patients who experience partial responses without substantial side effects. Table 2 summarizes common antidepressant medications.
Table 2.
Commonly used antidepressant for late-life depression
| Medication | Starting dose |
Common Therapeutic Doses | Half-life (hour) |
Common side effects | Comments |
|---|---|---|---|---|---|
| SSRI (Selective serotonin-reuptake inhibitors): | Nausea, dyspepsia, anorexia, tremors, anxiety, insomnia, sexual dysfunction, jitteriness, hyponatremia |
Risk of serotonin syndrome if combined with certain drugs. |
|||
| Fluoxetine | 5 mg | 10 – 40 mg once daily | 70-80 | Very long acting. | |
| Sertraline | 12.5 mg | 50 – 200 mg once daily | 25-30 | Loose stools, diarrhea | |
| Citalopram | 10 mg | 20 – 40 mg once daily | 40-50 | ||
| Escitalopram | 2.5 mg | 10– 30 mg once daily | 40-50 | ||
| Paroxetine | 10 mg | 20 – 50 mg once daily | 10-20 | Dry mouth, drowsiness, fatigue, weight gain, |
More anticholinergic side effects. High risk of discontinuation syndrome if drug stopped abruptly. |
| SNRIs (Serotonin-norepinephrine reuptake inhibitors) | Nausea, drowsiness, fatigue, weight gain, hyponatremia, diastolic hypertension at higher doses |
Risk of serotonin syndrome if combined with certain drugs. High risk of discontinuation syndrome if medication stopped abruptly. |
|||
| Venlafaxine XR | 37.5 mg | 75-225g once daily | 5 – 9 | ||
| Duloxetine | 20 mg | 20-60mg once daily | 8 – 17 | ||
| Other newer antidepressants | |||||
| Mirtazapine | 15mg | 15-45mg at bedtime | 20 -40 | Sedation, increased appetite / weight gain | No sexual side effects. |
| Bupropion SR | 100mg | 100-150 mg twice daily | 15 | No sexual side effects. Contraindicated in patients with seizures. Not recommended for patients with comorbid anxiety. |
|
| TCAs (Tricyclic antidepressants) | Sedation, weight gain, dry mouth, urinary retention, constipation, blurry vision, orthostatic hypotension, impairment of cardiac conduction |
High risk in overdose: 10 days of typical daily dose may result in a fatal cardiac arrhythmia. Get baseline ECG and follow-up ECG at steady state or if new cardiac symptoms occur. |
|||
| Nortriptyline | 10mg | 50-125mg every night | 18–56 | Fatigue | Therapeutic blood levels range from 50 to 150 ng/mL |
| Desipramine | 25mg | 100-200mg once daily | 12–28 | Insomnia, agitation | |
Psychological management
Older adults patients with depression tend to prefer psychotherapy over medications.137 Several psychotherapeutic modalities are effective for late-life depression138-140: cognitive behavioral therapy (CBT),121,141 interpersonal therapy (IPT),142 problem solving treatment (PST),143 and Behavioral Activation and Pleasant Activity Scheduling (BA).144-146 A recent meta-analysis of 44 studies comparing psychotherapies and control conditions,140 concluded that the overall effect size of psychotherapy over control group were g = 0.64 (95% CI: 0.47-0.80). Although such treatments can be effectively provided to older adults in primary care,147,148 they are not widely available in most primary care settings today and we encourage clinicians to develop relationships with mental health specialists who can offer such treatments or to train a staff member in the clinic to provide evidence-based brief psychotherapies. Table 3 summarizes brief- and evidence –based psychotherapeutic approaches that can be easily administered in the primary care context and by nurses, social workers, or other licensed psychotherapists.
Table 3. Efficacious non-pharmacologic treatments for late-life depression.
| Treatment type | Studies | Level of evidence | Comments |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) |
Gould et al 2012159 | Meta-analysis of RCTs | CBT significantly more efficacious at reducing depressive symptoms |
| Combination with pharmacotherapy more efficacious than CBT alone | |||
|
|
|||
| Cuijpers et al 2014140 | Meta-analysis of RCTs | Older adults populations studies | |
|
| |||
| Behavior activation (BA) | Cuijpers et al 2007160 | Meta-analysis of RCTs | Mixed population studies Effect is weaker in older adults |
|
| |||
| Ekers et al, 2014161 | Meta-analysis of RCTs | Mixed population studies | |
|
| |||
| Samad et al162 | Meta-analysis of RCTs | Older adults populations studies | |
|
| |||
| Problem solving therapy (PST) | Bell et al 2009163 | Meta-analysis of RCTs | Mixed population studies |
|
| |||
| Interpersonal psychotherapy (IPT) | Beekman et al 2006164 | Pragmatic RCT | Older adults populations studies |
|
| |||
| Bohlmeijer et al 2003165 | Meta-analysis of RCTs | Older adults populations studies | |
|
|
|||
| Reminiscence (life review) | Pinquart & Forstmeier166 | Meta-analysis of RCTs | Efficacious for broad range of outcomes, and therapeutic as well as preventive effects are similar to those observed in other frequently used interventions. |
Electroconvulsive Treatment (ECT)
ECT is an important and viable treatment option for severely depressed older adults. ECT should be strongly considered for patients who have severe, persistent depression that does not respond to several trials of antidepressant medications or psychotherapy and/or puts patient at high risk of harm (e.g. severe weight loss, malnutrition, refusal of food, suicidal ideation). Poor tolerance or limited response to medications and a history of successful treatment with ECT are also indications for ECT. Rates of ECT use in depressed adults vary substantially.149,150 Older adults are more likely to receive ECT than younger adults, African Americans are less likely to receive ECT than Whites and individuals with poor health insurance or living in rural areas are also less likely to receive ECT.149
Summary/Discussion
DM and depression is frequently comorbid in older adult patients. Considering the negative synergistic effects on range of health outcomes resulted by comorbid depression and DM, prevention and early treatment of comorbid depression are a critical component of successful health management in older adult patients with DM.
Key Points.
Depression is highly prevalent in the general population and increases the risk for type 2 DM 2.
Comorbid depression and DM is associated negative health outcomes, such as accelerated cognitive decline and increased mortality.
Depression impinges the patient and the family caregiver’s ability to effectively manage DM, decreases adherence to treatment, and undermines successful physician-patient relationship
Effective models for treating comorbid depression and DM exists and some components of these models are implementable in individual clinics.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mijung Park, Department of Health and Community Systems, University of Pittsburgh, School of Nursing, 3500 Victoria Street, 421 Victoria building, Pittsburgh, PA 15213.
Charles F. Reynolds, III, NIMH Center of Excellence in Late Life Depression Prevention and Treatment, Hartford Center of Excellence in Geriatric Psychiatry, and Aging Institute of UPMC Senior Services and the University of Pittsburgh, 3811 O’Hara Street, Pittsburgh, PA 15213-2582, Telephone: 412-246-5991, ReynoldsCF@upmc.edu.
References
- 1.Murray CJ, Lopez AD. Measuring the global burden of disease. New England Journal of Medicine. 2013;369(5):448–457. doi: 10.1056/NEJMra1201534. [DOI] [PubMed] [Google Scholar]
- 2.Park M, Unützer J. Public Health Burden of Late-Life Mood Disorders. In: Levretsky H, Sajatovic M, Reynolds C, editors. Late-life Mood Disorders. Oxford University Press; NY: 2013. pp. 42–60. [Google Scholar]
- 3.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001 Jun;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 4.Palinkas L, Barrett-Connor E, Wingard D. Type 2 Diabetes and Depressive Symptoms in Older Adults: a Population-based Study. Diabetic medicine. 1991;8(6):532–539. doi: 10.1111/j.1464-5491.1991.tb01646.x. [DOI] [PubMed] [Google Scholar]
- 5.Kramer MK, Kriska AM, Venditti EM, et al. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. American journal of preventive medicine. 2009 Dec;37(6):505–511. doi: 10.1016/j.amepre.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control Prevention . National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2011. p. 201. [Google Scholar]
- 7.Park M, Katon WJ, Wolf FM. Depression and risk of mortality in individuals with diabetes: a meta-analysis and systematic review. General hospital psychiatry. 2013;35(3):217–225. doi: 10.1016/j.genhosppsych.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cuijpers P, Beekman AT, Reynolds CF., 3rd. Preventing depression: a global priority. JAMA: the journal of the American Medical Association. 2012 Mar 14;307(10):1033–1034. doi: 10.1001/jama.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ludman EJ, Katon W, Russo J, et al. Depression and diabetes symptom burden. General hospital psychiatry. 2004;26(6):430–436. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008 Dec;31(12):2398–2403. doi: 10.2337/dc08-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egede LE, Zheng D, Simpson K. Comorbid Depression is Associated With Increased Health Care Use and Expenditures in Individuals With Diabetes. Diabetes Care. 2002 Mar;25(3):464–470. doi: 10.2337/diacare.25.3.464. 2002. [DOI] [PubMed] [Google Scholar]
- 12.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001 Jul-Aug;63(4):619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Katon W, Lyles CR, Parker MM, Karter AJ, Huang ES, Whitmer RA. Association of depression with increased risk of dementia in patients with type 2 diabetes: the Diabetes and Aging Study. Arch Gen Psychiatry. 2012 Apr;69(4):410–417. doi: 10.1001/archgenpsychiatry.2011.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blazer DG. Psychiatry and the Oldest Old. Am J Psychiatry. 2000 Dec 1;157(12):1915–1924. doi: 10.1176/appi.ajp.157.12.1915. 2000. [DOI] [PubMed] [Google Scholar]
- 15.Evans DL, Charney DS, Lewis L, et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005 Aug 1;58(3):175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 16.Unutzer J. Diagnosis and treatment of older adults with depression in primary care. Biol Psychiatry. 2002 Aug 1;52(3):285–292. doi: 10.1016/s0006-3223(02)01338-0. [DOI] [PubMed] [Google Scholar]
- 17.Lyness JM, Kim J, Tang W, et al. The Clinical Significance of Subsyndromal Depression in Older Primary Care Patients. American Journal of Geriatric Psych. 2007;15(3):214–223. doi: 10.1097/01.JGP.0000235763.50230.83. 210.1097/1001.JGP.0000235763.0000250230.0000235783. [DOI] [PubMed] [Google Scholar]
- 18.Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in “a minor” can “b major”: A review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. Journal of Affective Disorders. 2011;129(1-3):126–142. doi: 10.1016/j.jad.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Judd LL, Akiskal HS. The Clinical and Public Health Relevance of Current Research on Subthreshold Depressive Symptoms to Elderly Patients. American Journal of Geriatric Psych. 2002;10(3):233–238. [PubMed] [Google Scholar]
- 20.Lavretsky H, Kumar A. Clinically Significant Non-Major Depression: Old Concepts, New Insights. American Journal of Geriatric Psych. 2002;10(3):239–255. [PubMed] [Google Scholar]
- 21.Lyness J, King D, Cox C, Yoediono Z, Caine E. The importance of subsyndromal depression in older primary care patients: prevalence and associated functional disability. J Am Geriatr Soc. 1999;47(6):647–652. doi: 10.1111/j.1532-5415.1999.tb01584.x. [DOI] [PubMed] [Google Scholar]
- 22.Remick RA. Diagnosis and management of depression in primary care: a clinical update and review. CMAJ. 2002 Nov 26;167(11):1253–1260. 2002. [PMC free article] [PubMed] [Google Scholar]
- 23.Lyness JM, Yu Q, Tang W, Tu X, Conwell Y. Risks for Depression Onset in Primary Care Elderly Patients: Potential Targets for Preventive Interventions. Am J Psychiatry. 2009 Dec 1;166(12):1375–1383. doi: 10.1176/appi.ajp.2009.08101489. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grabovich A, Lu N, Tang W, Tu X, Lyness JM. Outcomes of subsyndromal depression in older primary care patients. Am J Geriatr Psychiatry. 2010 Mar;18(3):227–235. doi: 10.1097/JGP.0b013e3181cb87d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Unutzer J. Clinical practice. Late-life depression. N Engl J Med. 2007 Nov 29;357(22):2269–2276. doi: 10.1056/NEJMcp073754. [DOI] [PubMed] [Google Scholar]
- 26.Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. Am J Psychiatry. 2006 May;163(5):872–880. doi: 10.1176/ajp.2006.163.5.872. [DOI] [PubMed] [Google Scholar]
- 27.Mueller TI, Leon AC, Keller MB, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am.J.Psychiatry. 1999;156(7):1000–1006. doi: 10.1176/ajp.156.7.1000. [DOI] [PubMed] [Google Scholar]
- 28.Licht-Strunk E, van der Windt DlA, van Marwijk HW, de Haan M, Beekman AT. The prognosis of depression in older patients in general practice and the community. A systematic review. Family Practice. 2007;24(2):168–180. doi: 10.1093/fampra/cml071. [DOI] [PubMed] [Google Scholar]
- 29.Cole MG, Bellavance F, Mansour A. Prognosis of depression in elderly community and primary care populations: a systematic review and meta-analysis. Am J Psychiatry. 1999 Aug;156(8):1182–1189. doi: 10.1176/ajp.156.8.1182. [DOI] [PubMed] [Google Scholar]
- 30.Iosifescu DV, Nierenberg AA, Alpert JE, et al. Comorbid Medical Illness and Relapse of Major Depressive Disorder in the Continuation Phase of Treatment. Psychosomatics. 2004;45(5):419–425. doi: 10.1176/appi.psy.45.5.419. [DOI] [PubMed] [Google Scholar]
- 31.Fisher L, Skaff MM, Mullan JT, et al. Clinical depression versus distress among patients with type 2 diabetes not just a question of semantics. Diabetes Care. 2007;30(3):542–548. doi: 10.2337/dc06-1614. [DOI] [PubMed] [Google Scholar]
- 32.Drayer RA, Mulsant BH, Lenze EJ, et al. Somatic symptoms of depression in elderly patients with medical comorbidities. International Journal of Geriatric Psychiatry. 2005;20(10):973–982. doi: 10.1002/gps.1389. [DOI] [PubMed] [Google Scholar]
- 33.Kirmayer LJ, Young A. Culture and somatization: clinical, epidemiological, and ethnographic perspectives. Psychosom Med. 1998 Jul 1;60(4):420–430. doi: 10.1097/00006842-199807000-00006. 1998. [DOI] [PubMed] [Google Scholar]
- 34.Sadovnick AD, Remick RA, Lam R, et al. Mood disorder service genetic database: Morbidity risks for mood disorders in 3,942 first-degree relatives of 671 index cases with single depression, recurrent depression, bipolar I, or bipolar II. American Journal of Medical Genetics. 1994;54(2):132–140. doi: 10.1002/ajmg.1320540208. [DOI] [PubMed] [Google Scholar]
- 35.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. The Lancet. 2007 Dec 14;370(9603):1960–1973. doi: 10.1016/S0140-6736(07)61816-9. 2007. [DOI] [PubMed] [Google Scholar]
- 36.Pinquart M, Sorensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychol Aging. 2000 Jun;15(2):187–224. doi: 10.1037//0882-7974.15.2.187. [DOI] [PubMed] [Google Scholar]
- 37.Park M, Unützer J, Grembowski D. Ethnic and Gender Variations in The Associations between Family Cohesion, Family Conflict, and Depression in Older Asian and Latino Adults. Journal of Immigrant and Minority Health. 2013:1–8. doi: 10.1007/s10903-013-9926-1. [e-pub ahead of time] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park M, Unutzer J. Hundred forty eight more days with depression: the association between marital conflict and depression-free days. Int J Geriatr Psychiatry. 2014 Apr 4; doi: 10.1002/gps.4107. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thompson A, Fan MY, Unutzer J, Katon W. One extra month of depression: the effects of caregiving on depression outcomes in the IMPACT trial. Int J Geriatr Psychiatry. 2008 May;23(5):511–516. doi: 10.1002/gps.1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abe-Kim J, Takeuchi DT, Hong S, et al. Use of mental health-related services among immigrant and US-born Asian Americans: results from the National Latino and Asian American Study. Am J Public Health. 2007 Jan;97(1):91–98. doi: 10.2105/AJPH.2006.098541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abe-Kim JS, Takeuchi DT. Cultural Competence and Quality of Care: Issues for Mental Health Service Delivery in Managed Care. Clinical Psychology: Science and Practice. 1996;3(4):273–295. [Google Scholar]
- 42.Aber JL, Bennett NG, Conley DC, Li J. The effects of poverty on child health and development. Annu Rev Public Health. 1997;18:463–483. doi: 10.1146/annurev.publhealth.18.1.463. [DOI] [PubMed] [Google Scholar]
- 43.Abueg FR, Chun KM. Traumatized Asian and Asian American populations. In: Marsella A, Friedman M, Gerrity E, Scurfield R, editors. Ethnocultural approaches to understanding posttraumatic stress disorder: Issues, research, and clinical applications. American Psychology Association; Washington D.C.: 1996. [Google Scholar]
- 44.Abueg FR, Chun KM. Traumatization stress among Asians and Asian Americans. In: Marsella AJEF, Matthew J, et al., editors. Ethnocultural aspects of posttraumatic stress disorder: Issues, research, and clinical applications. American Psychological Association; Washington, DC: 1996. pp. 285–299. [Google Scholar]
- 45.Ackerman DL, Unutzer J, Greenland S, Gitlin M. Inpatient treatment of depression and associated hospital charges. Pharmacoepidemiol Drug Saf. 2002 Apr-May;11(3):219–227. doi: 10.1002/pds.694. [DOI] [PubMed] [Google Scholar]
- 46.Adler N, Boyce W, Chesney M, Folkman S, Syme S. Socioeconomic inequalities in health: no easy solution. JAMA: the journal of the American Medical Association. 1993;269:3140. [PubMed] [Google Scholar]
- 47.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002 Mar-Apr;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 48.Adler NE, Newman K. Socioeconomic Disparities In Health: Pathways And Policies. Health Aff. 2002 Mar 1;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. 2002. [DOI] [PubMed] [Google Scholar]
- 49.Park M. The Variations in Associations between Family Contexts and Late-Life Depression Outcomes [Thesis]: Health Services. University of Washington; 2013. [Google Scholar]
- 50.Martire LM, Schulz R. Involving Family in Psychosocial Interventions for Chronic Illness. current directions in psychological science. 2007;16(2):90–94. [Google Scholar]
- 51.Lee MS, Crittenden KS, Yu E. Social support and depression among elderly Korean immigrants in the United States. International Journal of Aging and Human Development. 1996;42(4):313–327. doi: 10.2190/2VHH-JLXY-EBVG-Y8JB. [DOI] [PubMed] [Google Scholar]
- 52.George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. Br J Psychiatry. 1989 Apr;154(4):478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- 53.Smith F, Francis S-A, Gray N, Denham M, Graffy J. A multi-centre survey among informal carers who manage medication for older care recipients: problems experienced and development of services. Health & Social Care in the Community. 2003;11(2):138–145. doi: 10.1046/j.1365-2524.2003.00415.x. [DOI] [PubMed] [Google Scholar]
- 54.Voils CI, Steffens DC, Flint EP, Bosworth HB. Social Support and Locus of Control as Predictors of Adherence to Antidepressant Medication in an Elderly Population. American Journal of Geriatric Psych. 2005;13(2):157–165. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- 55.Agency for Healthcare Research and Quality . 2004 National Healthcare Disparities Report. Rockville, MD2004: [Google Scholar]
- 56.Agency for Healthcare Research and Quality . National Healthcare Disparities Report. Rockville, MD2007: 2007. [Google Scholar]
- 57.Kawachi I, Berkman L. Social ties and mental health. Journal of Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hong S-I, Hasche L, Bowland S. Structural Relationships Between Social Activities and Longitudinal Trajectories of Depression Among Older Adults. The Gerontologist. 2009 Feb 1;49(1):1–11. doi: 10.1093/geront/gnp006. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Unutzer J, Katon W, Sullivan M, Miranda J. Treating depressed older adults in primary care: narrowing the gap between efficacy and effectiveness. Milbank Q. 1999;77(2):225–256. 174. doi: 10.1111/1468-0009.00132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Centers for Disease Control and Prevention and National Association of Chronic Disease Directors . In: The State of Mental Health and Aging in America Issue Brief 2: Addressing Depression in Older Adults: Selected Evidence-Based Programs. National Association of Chronic Disease Directors, editor. Atlanta, GA: 2009. [Google Scholar]
- 61.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 Jun 1;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. 2005. [DOI] [PubMed] [Google Scholar]
- 62.Mojtabai R, Olfson M. Major depression in community-dwelling middle-aged and older adults: prevalence and 2- and 4-year follow-up symptoms. Psychological Medicine. 2004;34(04):623–634. doi: 10.1017/S0033291703001764. [DOI] [PubMed] [Google Scholar]
- 63.Byers AL, Yaffe K, Covinsky KE, Friedman MB, Bruce ML. High occurrence of mood and anxiety disorders among older adults: The National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010 May;67(5):489–496. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Blazer DG. Depression in Late Life: Review and Commentary. Focus. 2009 Jan 1;7(1):118–136. 2009. [Google Scholar]
- 65.Teresi J, Abrams R, Holmes D, Ramirez M, Eimicke J. Prevalence of depression and depression recognition in nursing homes. Social Psychiatry and Psychiatric Epidemiology. 2001;36(12):613–620. doi: 10.1007/s127-001-8202-7. [DOI] [PubMed] [Google Scholar]
- 66.Hoover DR, Siegel M, Lucas J, et al. Depression in the first year of stay for elderly long-term nursing home residents in the U.S.A. International Psychogeriatrics. 2010:1–11. doi: 10.1017/S1041610210000578. First View. [DOI] [PubMed] [Google Scholar]
- 67.Lyness JM, Caine ED, King DA, Cox C, Yoediono Z. Psychiatric Disorders in Older Primary Care Patients. Journal of General Internal Medicine. 1999;14(4):249–254. doi: 10.1046/j.1525-1497.1999.00326.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kuo BCH, Chong V, Joseph J. Depression and Its Psychosocial Correlates Among Older Asian Immigrants in North America. Journal of Aging and Health. 2008;20(6):615–652. doi: 10.1177/0898264308321001. [DOI] [PubMed] [Google Scholar]
- 69.Simpson S, Krishnan L, Kunik M, Ruiz P. Racial Disparities in Diagnosis and Treatment of Depression: A Literature Review. Psychiatric Quarterly. 2007;78(1):3–14. doi: 10.1007/s11126-006-9022-y. [DOI] [PubMed] [Google Scholar]
- 70.Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003 Oct;26(10):2822–2828. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- 71.Steffens DC, Fisher GG, Langa KM, Potter GG, Plassman BL. Prevalence of depression among older Americans: the Aging, Demographics and Memory Study. Int Psychogeriatr. 2009 Oct;21(5):879–888. doi: 10.1017/S1041610209990044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Strothers HS, Rust G, Minor P, Fresh E, Druss B, Satcher D. Disparities in Antidepressant Treatment in Medicaid Elderly Diagnosed with Depression. Journal of the American Geriatrics Society. 2005;53(3):456–461. doi: 10.1111/j.1532-5415.2005.53164.x. [DOI] [PubMed] [Google Scholar]
- 73.Crystal S, Sambamoorthi U, Walkup JT, Akincigil A. Diagnosis and treatment of depression in the elderly medicare population: predictors, disparities, and trends. Journal of the American Geriatrics Society. 2003 Dec;51(12):1718–1728. doi: 10.1046/j.1532-5415.2003.51555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kleinman A. Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. University of California Press; Berkeley and Los Angeles, California: 1981. [Google Scholar]
- 75.Kleinman A. Culture and Depression. N Engl J Med. 2004 Sep 2;351(10):951–953. doi: 10.1056/NEJMp048078. 2004. [DOI] [PubMed] [Google Scholar]
- 76.Pang KYC. Symptom expression and somatization among elderly Korean immigrants. ournal of Clinical Geropsychology. 2000;6(3):199–212. [Google Scholar]
- 77.Jackson JL, Kroenke K. Difficult Patient Encounters in the Ambulatory Clinic: Clinical Predictors and Outcomes. Arch Intern Med. 1999 May 24;159(10):1069–1075. doi: 10.1001/archinte.159.10.1069. 1999. [DOI] [PubMed] [Google Scholar]
- 78.Cooper LA, Gonzales JJ, Gallo JJ, et al. The Acceptability of Treatment for Depression among African-American, Hispanic, and White Primary Care Patients. Medical care. 2003;41(4):479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 79.Givens JL, Houston TK, Van Voorhees BW, Ford DE, Cooper LA. Ethnicity and preferences for depression treatment. General hospital psychiatry. 2007 May-Jun;29(3):182–191. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 80.Alegria M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008 Nov;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kessler RC, Birnbaum HG, Shahly V, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depression and Anxiety. 2010;27(4):351–364. doi: 10.1002/da.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives. Nat Rev Endocrinol. 2012 Apr;8(4):228–236. doi: 10.1038/nrendo.2011.183. [DOI] [PubMed] [Google Scholar]
- 83.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004 May;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 84.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006 Nov;23(11):1165–1173. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 85.Li C, Ford E, Strine T, Mokdad A. Prevalence of depression among U.S. adults with diabetes: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabetes Care. 2008;31:105. doi: 10.2337/dc07-1154. [DOI] [PubMed] [Google Scholar]
- 86.Hofmann M, Köhler B, Leichsenring F, Kruse J. Depression as a risk factor for mortality in individuals with diabetes: a meta-analysis of prospective studies. PloS one. 2013;8(11):e79809. doi: 10.1371/journal.pone.0079809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.van Dooren FE, Nefs G, Schram MT, Verhey FR, Denollet J, Pouwer F. Depression and risk of mortality in people with diabetes mellitus: a systematic review and meta-analysis. PloS one. 2013;8(3):e57058. doi: 10.1371/journal.pone.0057058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bogner HR, Morales KH, Post EP, Bruce ML. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT) Diabetes Care. 2007;30(12):3005–3010. doi: 10.2337/dc07-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gallo JJ, Morales KH, Bogner HR, et al. Long term effect of depression care management on mortality in older adults: follow-up of cluster randomized clinical trial in primary care. BMJ. 2013;346:f2570. doi: 10.1136/bmj.f2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry. 2003;54(3):216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 91.Golden S, Lazo M, Carnethon M, Bertoni A, Schreiner P. Examining a bidirectional association between depressive symptoms and diabetes. JAMA: the journal of the American Medical Association. 2008;299:2751. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Stuart MJ, Baune BT. Depression and type 2 diabetes: Inflammatory mechanisms of a psychoneuroendocrine co-morbidity. Neuroscience & Biobehavioral Reviews. 2012;36(1):658–676. doi: 10.1016/j.neubiorev.2011.10.001. 1// [DOI] [PubMed] [Google Scholar]
- 93.Silva N, Atlantis E, Ismail K. A review of the association between depression and insulin resistance: pitfalls of secondary analyses or a promising new approach to prevention of type 2 diabetes? Curr Psychiatry Rep. 2012 Feb;14(1):8–14. doi: 10.1007/s11920-011-0245-8. [DOI] [PubMed] [Google Scholar]
- 94.Kuo H-K. Cognitive dysfunction and depression in older adults with diabetes. Geriatric Diabetes. 2007:63–84. [Google Scholar]
- 95.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. General hospital psychiatry. 2003 Jul-Aug;25(4):246–252. doi: 10.1016/s0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 96.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000 Nov 27;160(21):3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 97.McDermott LM, Ebmeier KP. A meta-analysis of depression severity and cognitive function. J Affect Disord. 2009 Dec;119(1-3):1–8. doi: 10.1016/j.jad.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 98.Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011 Jun;7(6):323–331. doi: 10.1038/nrneurol.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rapp MA, Schnaider-Beeri M, Wysocki M, et al. Cognitive decline in patients with dementia as a function of depression. The American Journal of Geriatric Psychiatry. 2011;19(4):357–363. doi: 10.1097/JGP.0b013e3181e898d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Stetler C, Miller GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med. 2011 Feb-Mar;73(2):114–126. doi: 10.1097/PSY.0b013e31820ad12b. [DOI] [PubMed] [Google Scholar]
- 101.Lok A, Mocking RJ, Ruhe HG, et al. Longitudinal hypothalamic-pituitary-adrenal axis trait and state effects in recurrent depression. Psychoneuroendocrinology. 2012 Jul;37(7):892–902. doi: 10.1016/j.psyneuen.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 102.Vanhanen M, Koivisto K, Moilanen L, et al. Association of metabolic syndrome with Alzheimer disease A population-based study. Neurology. 2006;67(5):843–847. doi: 10.1212/01.wnl.0000234037.91185.99. [DOI] [PubMed] [Google Scholar]
- 103.Craft S. The role of metabolic disorders in Alzheimer disease and vascular dementia: two roads converged. Arch Neurol. 2009 Mar;66(3):300–305. doi: 10.1001/archneurol.2009.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Notarianni E. Hypercortisolemia and glucocorticoid receptor-signaling insufficiency in Alzheimer’s disease initiation and development. Curr Alzheimer Res. 2013 Sep;10(7):714–731. doi: 10.2174/15672050113109990137. [DOI] [PubMed] [Google Scholar]
- 105.Cole J, Costafreda SG, McGuffin P, Fu CH. Hippocampal atrophy in first episode depression: a meta-analysis of magnetic resonance imaging studies. J Affect Disord. 2011 Nov;134(1-3):483–487. doi: 10.1016/j.jad.2011.05.057. [DOI] [PubMed] [Google Scholar]
- 106.Taylor WD, McQuoid DR, Payne ME, Zannas AS, Macfall JR, Steffens DC. Hippocampus Atrophy and the Longitudinal Course of Late-life Depression. Am J Geriatr Psychiatry. 2013 Nov 22; doi: 10.1016/j.jagp.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008 Dec;31(12):2383–2390. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Demakakos P, Pierce MB, Hardy R. Depressive Symptoms and Risk of Type 2 Diabetes in a National Sample of Middle-Aged and Older Adults. Diabetes Care. 2010 Apr 1;33(4):792–797. doi: 10.2337/dc09-1663. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Carnethon MR, Kinder LS, Fair JM, Stafford RS, Fortmann SP. Symptoms of depression as a risk factor for incident diabetes: findings from the National Health and Nutrition Examination Epidemiologic Follow-up Study, 1971-1992. American journal of epidemiology. 2003;158(5):416–423. doi: 10.1093/aje/kwg172. [DOI] [PubMed] [Google Scholar]
- 110.Eaton W, Pratt L, Armenian H, Ford D, Gallo J. Depression and risk for onset of type II diabetes: a prospective populationbased study. Diabetes Care. 1996;19:1097–1102. doi: 10.2337/diacare.19.10.1097. [DOI] [PubMed] [Google Scholar]
- 111.Nouwen A, Winkley K, Twisk J, et al. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53(12):2480–2486. doi: 10.1007/s00125-010-1874-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Reynolds CF, Thomas SB, Morse JQ, et al. Early Intervention to Preempt Major Depression Among Older Black and White Adults. Psychiatric Services. 2014 doi: 10.1176/appi.ps.201300216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.U.S. Preventive Services Task Force [Accessed October 30, 2011];Screening for Depression: Recommendations and Rationale. 2002 http://www.uspreventiveservicestaskforce.org/3rduspstf/depression/depressrr.htm.
- 114.Cuijpers P, van Straten A, Hollon SD, Andersson G. The contribution of active medication to combined treatments of psychotherapy and pharmacotherapy for adult depression: a meta-analysis. Acta Psychiatr Scand. 2010 Jun;121(6):415–423. doi: 10.1111/j.1600-0447.2009.01513.x. [DOI] [PubMed] [Google Scholar]
- 115.Kohler S, Hoffmann S, Unger T, Steinacher B, Dierstein N, Fydrich T. Effectiveness of cognitive-behavioural therapy plus pharmacotherapy in inpatient treatment of depressive disorders. Clin Psychol Psychother. 2013 Mar-Apr;20(2):97–106. doi: 10.1002/cpp.795. [DOI] [PubMed] [Google Scholar]
- 116.Rocha FL, Fuzikawa C, Riera R, Hara C. Combination of antidepressants in the treatment of major depressive disorder: a systematic review and meta-analysis. J Clin Psychopharmacol. 2012 Apr;32(2):278–281. doi: 10.1097/JCP.0b013e318248581b. [DOI] [PubMed] [Google Scholar]
- 117.Reynolds CF, Frank E, Perel JM, et al. Nortriptyline and Interpersonal Psychotherapy as Maintenance Therapies for Recurrent Major Depression. JAMA: The Journal of the American Medical Association. 1999;281(1):39–45. doi: 10.1001/jama.281.1.39. [DOI] [PubMed] [Google Scholar]
- 118.van der Feltz-Cornelis CM, Nuyen J, Stoop C, et al. Effect of interventions for major depressive disorder and significant depressive symptoms in patients with diabetes mellitus: a systematic review and meta-analysis. General hospital psychiatry. 2010;32(4):380–395. doi: 10.1016/j.genhosppsych.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 119.Bruce ML, Ten Have TR, Reynolds CF, III, et al. Reducing Suicidal Ideation and Depressive Symptoms in Depressed Older Primary Care Patients: A Randomized Controlled Trial. JAMA: the journal of the American Medical Association. 2004;291(9):1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 120.Oxman TE, Sengupta A. Treatment of Minor Depression. American Journal of Geriatric Psych. 2002;10(3):256–264. [PubMed] [Google Scholar]
- 121.Pinquart M, Duberstein PR, Lyness JM. Treatments for Later-Life Depressive Conditions: A Meta-Analytic Comparison of Pharmacotherapy and Psychotherapy. Am J Psychiatry. 2006 Sep 1;163(9):1493–1501. doi: 10.1176/ajp.2006.163.9.1493. 2006. [DOI] [PubMed] [Google Scholar]
- 122.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: A cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 123.Simon G. Collaborative care for depression. BMJ. 2006 Feb 4;332(7536):249–250. doi: 10.1136/bmj.332.7536.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Simon G. Collaborative care for mood disorders. Curr Opin Psychiatry. 2009 Jan;22(1):37–41. doi: 10.1097/YCO.0b013e328313e3f0. [DOI] [PubMed] [Google Scholar]
- 125.Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. The Annals of Family Medicine. 2012;10(1):15–22. doi: 10.1370/afm.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Katon W, Von Korff M, LE B, al e. The pathways study: A randomized trial of collaborative care in patients with diabetesand depression. Archives of General Psychiatry. 2004;61(10):1042–1049. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 127.Katon W, Lin EHB, Von Korff M, et al. Integrating depression and chronic disease care among patients with diabetes and/or coronary heart disease: The design of the TEAMcare study. Contemporary Clinical Trials. 2010;31(4):312–322. doi: 10.1016/j.cct.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Katon W, Unutzer J. Collaborative Care Models for Depression: Time to Move From Evidence to Practice. Arch Intern Med. 2006 Nov 27;166(21):2304–2306. doi: 10.1001/archinte.166.21.2304. 2006. [DOI] [PubMed] [Google Scholar]
- 129.Katon W, Unutzer J, Wells K, Jones L. Collaborative depression care: history, evolution and ways to enhance dissemination and sustainability. Gen Hosp Psychiatry. 2010 Sep-Oct;32(5):456–464. doi: 10.1016/j.genhosppsych.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Katon W, Von Korff M, Lin E, Simon G. Rethinking practitioner roles in chronic illness: the specialist, primary care physician, and the practice nurse. General Hospital Psychiatry. 2001 May-Jun;23(3):138–144. doi: 10.1016/s0163-8343(01)00136-0. [DOI] [PubMed] [Google Scholar]
- 131.Kroenke K, Spitzer RL, Williams JBW, L√∂we B. The PaTent Health QuesTonnaire SomaTc, Anxiety, and Depressive Symptom Scales: a systematic review. General hospital psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 132.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 4th ed. Washington, DC2000: [Google Scholar]
- 133.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: Validity of a Two-Item Depression Screener. Medical care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 134.Kok RM, Heeren TJ, Nolen WA. Continuing Treatment of Depression in the Elderly: A Systematic Review and Meta-Analysis of Double-Blinded Randomized Controlled Trials With Antidepressants. American Journal of Geriatric Psych. 2011;19(3):249–255. doi: 10.1097/jgp.0b013e3181ec8085. 210.1097/JGP.1090b1013e3181ec8085. [DOI] [PubMed] [Google Scholar]
- 135.Nelson JC, Delucchi K, Schneider L. Efficacy of Second Generation Antidepressants in Late-Life Depression: A Meta-Analysis of the Evidence. American Journal of Geriatric Psychiatry. 2008;16(7):558–567. doi: 10.1097/JGP.0b013e3181693288. [DOI] [PubMed] [Google Scholar]
- 136.Gartlehner G, Gaynes BN, Hansen RA, et al. Comparative benefits and harms of second-generation antidepressants: background paper for the American College of Physicians. Ann Intern Med. 2008 Nov 18;149(10):734–750. doi: 10.7326/0003-4819-149-10-200811180-00008. [DOI] [PubMed] [Google Scholar]
- 137.Gum AM, Arean PA, Hunkeler E, et al. Depression treatment preferences in older primary care patients. Gerontologist. 2006 Feb;46(1):14–22. doi: 10.1093/geront/46.1.14. [DOI] [PubMed] [Google Scholar]
- 138.Cuijpers P, van Straten A, Smit F. Psychological treatment of late-life depression: a meta-analysis of randomized controlled trials. Int J Geriatr Psychiatry. 2006 Dec;21(12):1139–1149. doi: 10.1002/gps.1620. [DOI] [PubMed] [Google Scholar]
- 139.Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: A meta-analysis. Aging and Mental Health. 2007;11(6):645–657. doi: 10.1080/13607860701529635. [DOI] [PubMed] [Google Scholar]
- 140.Cuijpers P, Karyotaki E, Pot AM, Park M, Reynolds CF., III Managing depression in older age: psychological interventions. Maturitas. 2014 doi: 10.1016/j.maturitas.2014.05.027. [Epub ahead of time] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wilson KC, Mottram PG, Vassilas CA. Psychotherapeutic treatments for older depressed people. Cochrane Database Syst Rev. 2008;1(1):CD004853. doi: 10.1002/14651858.CD004853.pub2. [DOI] [PubMed] [Google Scholar]
- 142.de Mello MF, de Jesus Mari J, Bacaltchuk J, Verdeli H, Neugebauer R. A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. Eur Arch Psychiatry Clin Neurosci. 2005 Apr;255(2):75–82. doi: 10.1007/s00406-004-0542-x. [DOI] [PubMed] [Google Scholar]
- 143.Bell AC, D’Zurilla TJ. Problem-solving therapy for depression: a meta-analysis. Clin Psychol Rev. 2009 Jun;29(4):348–353. doi: 10.1016/j.cpr.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 144.Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: a meta-analysis. Clin Psychol Rev. 2007 Apr;27(3):318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 145.Mazzucchelli T, Kane R, Rees C. Behavioral Activation Treatments for Depression in Adults: A Meta-analysis and Review. Clinical Psychology: Science and Practice. 2009;16(4):383–411. [Google Scholar]
- 146.Ekers D, Richards D, Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychol Med. 2008 May;38(5):611–623. doi: 10.1017/S0033291707001614. [DOI] [PubMed] [Google Scholar]
- 147.Arean P, Hegel M, Vannoy S, Fan MY, Unuzter J. Effectiveness of problem-solving therapy for older, primary care patients with depression: results from the IMPACT project. Gerontologist. 2008 Jun;48(3):311–323. doi: 10.1093/geront/48.3.311. [DOI] [PubMed] [Google Scholar]
- 148.Schulberg HC, Post EP, Raue PJ, Have TT, Miller M, Bruce ML. Treating late-life depression with interpersonal psychotherapy in the primary care sector. International Journal of Geriatric Psychiatry. 2007;22(2):106–114. doi: 10.1002/gps.1700. [DOI] [PubMed] [Google Scholar]
- 149.Olfson M, Marcus S, Sackeim HA, Thompson J, Pincus HA. Use of ECT for the Inpatient Treatment of Recurrent Major Depression. Am J Psychiatry. 1998;155:22–29. doi: 10.1176/ajp.155.1.22. [DOI] [PubMed] [Google Scholar]
- 150.Case BG, Bertollo DN, Laska EM, Siegel CE, Wanderling JA, Olfson M. Racial differences in the availability and use of electroconvulsive therapy for recurrent major depression. Journal of Affective Disorders. 2012;136(3):359–365. doi: 10.1016/j.jad.2011.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Association AP. Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- 152.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am.J.Psychiatry. 2003;160(6):1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 153.Snowdon J. Is depression more prevalent in old age? Australian and New Zealand Journal of Psychiatry. 2001;35(6):782–787. doi: 10.1046/j.1440-1614.2001.00968.x. [DOI] [PubMed] [Google Scholar]
- 154.Sonnenberg CM, Beekman AT, Deeg DJ, van Tilburg W. Sex differences in late-life depression. Acta Psychiatr Scand. 2000 Apr;101(4):286–292. [PubMed] [Google Scholar]
- 155.Zisook S, Shuchter SR. Depression through the first year after the death of a spouse. Am J Psychiatry. 1991 Oct;148(10):1346–1352. doi: 10.1176/ajp.148.10.1346. [DOI] [PubMed] [Google Scholar]
- 156.Turvey CL, Carney C, Arndt S, Wallace RB, Herzog R. Conjugal loss and syndromal depression in a sample of elders aged 70 years or older. Am J Psychiatry. 1999 Oct;156(10):1596–1601. doi: 10.1176/ajp.156.10.1596. [DOI] [PubMed] [Google Scholar]
- 157.Prince MJ, Harwood RH, Thomas A, Mann AH, The Gospel Oak Project VII A prospective population-based cohort study of the effects of disablement and social milieu on the onset and maintenance of late-life depression. Psychol Med. 1998 Mar;28(2):337–350. doi: 10.1017/s0033291797006478. [DOI] [PubMed] [Google Scholar]
- 158.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and aging. 2006;21(1):140. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- 159.Gould RL, Coulson MC, Howard RJ. Cognitive behavioral therapy for depression in older people: a meta-analysis and meta-regression of randomized controlled trials. Journal of the American Geriatrics Society. 2012 Oct;60(10):1817–1830. doi: 10.1111/j.1532-5415.2012.04166.x. [DOI] [PubMed] [Google Scholar]
- 160.Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007;27(3):318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 161.Ekers D, Webster L, Van Straten A, Cuijpers P, Richards D, Gilbody S. Behavioural activation for depression; an update of meta-analysis of effectiveness and sub group analysis. PLoS One. 2014;9(6):e100100. doi: 10.1371/journal.pone.0100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Samad Z, Brealey S, Gilbody S. The effectiveness of behavioural therapy for the treatment of depression in older adults: a meta-analysis. Int J Geriatr Psychiatry. 2011 Dec;26(12):1211–1220. doi: 10.1002/gps.2680. [DOI] [PubMed] [Google Scholar]
- 163.Bell AC, D’Zurilla TJ. Problem-solving therapy for depression: A meta-analysis. Clinical Psychology Review. 2009;29(4):348–353. doi: 10.1016/j.cpr.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 164.Beekman A, van Schaik A, van Marwijk H, et al. Interpersonal Psychotherapy for Elderly Patients in Primary Care. American Journal of Geriatric Psych. 2006;14(9):777–786. doi: 10.1097/01.JGP.0000199341.25431.4b. 710.1097/1001.JGP.0000199341.0000125431.0000199344b. [DOI] [PubMed] [Google Scholar]
- 165.Bohlmeijer E, Smit F, Cuijpers P. Effects of reminiscence and life review on late-life depression: a meta-analysis. International Journal of Geriatric Psychiatry. 2003;18(12):1088–1094. doi: 10.1002/gps.1018. [DOI] [PubMed] [Google Scholar]
- 166.Pinquart M, Forstmeier S. Effects of reminiscence interventions on psychosocial outcomes: a meta-analysis. Aging mental healh t. 2012;16(5):541–558. doi: 10.1080/13607863.2011.651434. [DOI] [PubMed] [Google Scholar]