Abstract
Study Design
Prospective observational cohort study
Objective
To determine if postoperative cervical sagittal balance is an independent predictor of HR-QOL outcome following surgery for CSM.
Summary of Background Data
Both ventral and dorsal fusion procedures for cervical spondylotic myelopathy (CSM) are effective at reducing the symptoms of myelopathy. The importance of cervical sagittal balance in predicting overall HR-QOL outcome following ventral versus dorsal surgery for CSM has not been previously explored.
Methods
A prospective, nonrandomized cohort of 49 patients undergoing dorsal and ventral fusion surgery for CSM was examined. Preoperative and postoperative C2-C7 sagittal vertical axis (SVA) was measured on standing lateral cervical spine radiographs. Outcome was assessed with two disease-specific measures – the mJOA scale and the Oswestry NDI- and two generalized outcome measures – the SF-36 PCS and EQ-5D. Assessments were performed preoperatively, and at 3 months, 6 months, and 1 year postoperatively. Statistical analyses were performed using SAS v.9.3 (Cary, NC).
Results
Most patients experienced improvement in all outcome measures regardless of approach. Both preoperative and postoperative C2-C7 SVA measurements were independent predictors of clinically significant improvement in SF-36 PCS scores (p=0.03 and p=0.02). The majority of patients with C2-C7 SVA values greater than 40mm did not improve from an overall HR-QOL perspective (SF-36 PCS) despite improvement in myelopathy. The postoperative sagittal balance value was inversely correlated with a clinically significant improvement of SF-36 PCS scores in patients undergoing dorsal surgery but not ventral surgery (p=0.03 vs. p=0.93).
Conclusions
Preoperative and postoperative sagittal balance measurements independently predict clinical outcomes following surgery for CSM.
Keywords: Cervical spondylotic myelopathy, CSM, sagittal balance, sagittal vertical axis, prospective study, comparative effectiveness, health-related quality of life, functional outcome, SF-36, mJOA
INTRODUCTION
Cervical spondylotic myelopathy (CSM) occurs in the setting of degenerative cervical spondylosis and is one of the most common causes of spinal cord dysfunction worldwide.1-3 Ghogawala et al previously published a prospective comparative study that found that both ventral and dorsal spine surgery are effective at treating cervical myelopathy, but that patients undergoing ventral surgery had superior health-related quality of life (HR-QOL) scores at 1 year compared to patients undergoing dorsal surgery.4
Recently, the role of sagittal balance in cervical spine disorders and on the possible role of imbalance in predicting clinical and functional outcomes has become a focus of attention. 5 Tang et al demonstrated that postoperative sagittal balance, as measured by C2-C7 sagittal vertical axis (SVA), correlated with postoperative NDI and SF-36 PCS scores in a retrospective cohort of patients undergoing posterior cervical decompression and fusion.6
The goal of this study was to determine whether postoperative cervical sagittal balance, as measured by the C2-C7 SVA measurement technique, is an independent predictor of HR-QOL outcome following surgery for CSM. Secondarily, we sought to determine whether ventral and dorsal surgery might differ with respect to postoperative cervical sagittal balance.
MATERIALS AND METHODS
Data Coordination
Institutional review board approval was obtained at 4 clinical centers. All sites had a dedicated study coordinator for data collection. Patient data was managed at the central coordinating center (Lahey Hospital and Medical Center, Burlington, MA 01805), and patient data were de-identified prior to transfer from the treating institutions to protect confidentiality.
Study Population
Patients were prospectively enrolled in a non-randomized study of dorsal and ventral fusion surgery for CSM at four centers. Patients aged 45 through 75 years with degenerative CSM (defined as having two or more of the following symptoms: clumsy hands, gait disturbance, hyperreflexia, presence of a Babinski reflex, or bladder dysfunction) and cervical spinal cord compression at 2 or more levels were eligible for inclusion. Exclusion criteria included: 1) Cobb Angle greater than 5° kyphosis (C2 - C7) measured on standing lateral cervical spine radiograph; 2) a segmental kyphotic deformity (defined as ≥3 osteophytes extending dorsal to a C2-7 dorsal-caudal line);7 3) ossification of the posterior longitudinal ligament (OPLL); 4) developmentally narrow canal (defined as a canal diameter of less than 12mm at the base of C2), 5) previous cervical spine surgery; and 6) significant active health comorbidity (defined as an American Society of Anesthesiology class 3 or higher).
The choice of ventral or dorsal surgery was at the discretion of the surgeon and patient. A multilevel discectomy with fusion and plating was performed in patients in the ventral arm. Dorsal surgery was performed using a midline cervical laminectomy with fixation with lateral mass screws and rods and a bilateral fusion technique.
Imaging Review and Assessment of Clinical Equipoise
All enrolled patients underwent MRI and CT of the cervical spine preoperatively. The images were electronically uploaded to a Web-based platform (www.csm-study.org) for imaging review and confirmation of eligibility by a surgical equipoise panel of 14 spinal experts. Equipoise was deemed to be present if a majority vote was obtained stating that the case could be performed either from a ventral or dorsal approach.4
Upright cervical spine plain radiography was performed preoperatively and at one-year postoperatively. Sagittal balance was assessed by the C2-C7 SVA measurement technique and was measured as the distance from a plumb line drawn at the mid-point at the base of C2 to the plumb line drawn at the mid-point of the base of C7 in a standing lateral cervical spine radiograph (Figure 1). Patients whose C2-C7 SVA values exceeded 40mm were deemed to have sagittal imbalance, as consistent with the threshold value reported by Tang et al., although Tang defined C2-C7 SVA slightly differently using the superior dorsal aspect of C7 as opposed to the mid-point of C7.6 This is termed herein as the sagittal balance measurement. By convention, when the C2 plumb line was ventral to the C7 level, the value was designated as positive. The C2-C7 Cobb angle and C2-C7 SVA were measured in all cases preoperatively and 1 year postoperatively.
Figure 1.
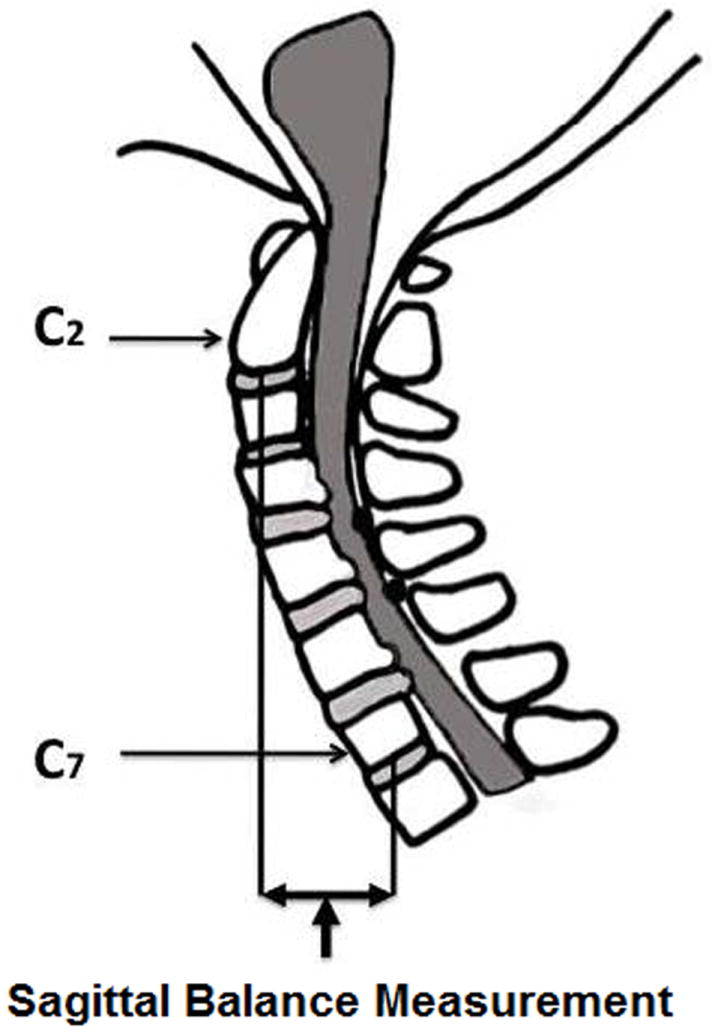
C2-C7 SVA is the distance from a plumb line drawn at the midpoint of the base of C2 to the plumb line drawn at the mid-point of the base of C7 measured on a standing lateral cervical spine radiograph.
Outcomes Assessment
Outcomes were assessed via two disease-specific measures – the modified Japanese Orthopedic Association (mJOA) scale8 and the Oswestry Neck Disability Index (NDI)9,10- and two generalized measures (HR-QOL measures) – the norm-based Short-Form 36 Physical Component Summary (SF-36 PCS) and the Euro-QOL-5D (EQ-5D). Outcome measures were obtained preoperatively and at 3 months, 6 months, and 1 year postoperatively.
Statistical Analysis
Statistical analyses were performed using SAS v.9.3 (Cary, NC). Fisher exact tests were utilized for categorical data. Shapiro-Wilk normality tests were used to assess whether a variable followed a normal distribution, and Student’s t-tests and Wilcoxon rank sum tests were used for descriptive statistics of normally and non-normally distributed continuous variables, respectively. Correlations between C2-C7 SVA measurements and HR-QOL scores were assessed using Spearman correlation coefficients due to statistically significant evidence for non-normality in observed HR-QOL scores. Furthermore, for consistency and because an assumption of linearity was not made, Spearman correlation coefficients were also calculated for change in HR-QOL scores and C2-C7 SVA measurements. Logistic regression models were generated to evaluate predictors of clinically significant improvements in HR-QOL measures with a minimal clinically important difference (MCID) for mJOA, NDI, and SF-36 PCS of 2 points, 10 points, and 5 points, respectively. 11,12 Analysis of covariance and general linear models were used to evaluate continuous outcome variables.
RESULTS
Baseline characteristics and overall outcomes
The cohort was comprised of 49 patients, 21 of whom underwent ventral fusion surgery and 28 of whom underwent dorsal surgery. Table 1 summarizes baseline demographic, radiographic, and preoperative HR-QOL measures. The two cohorts were similar with respect to age, preoperative Cobb angle, and baseline HR-QOL measurements. There were more males in the dorsal group. In addition, preoperative sagittal balance measurements were significantly more positive in the dorsal surgery group than in the ventral group (p=0.04).
Table 1.
Baseline demographic, radiographic, and HR-QOL scores by surgical approach.
| Dorsal | Ventral | p-value | |
|---|---|---|---|
| N | 28 | 21 | N/A |
| Age (years) | |||
| Mean | 62.2 ± 10.4 | 62.4 ± 9.5 | 0.93 |
| Range | 41-79 | 45-80 | |
| IQR | 54-68.5 | 45-80 | |
| Gender (%male) | 21/28 (75%) | 9/21 (42.9%) | 0.038 |
| Preoperative Cobb angle (°) | -7.5* ± 14.7 | -1.4 ± 16.8 | 0.27 |
| Preoperative C2-C7 SVA (mm) | 32.8 ± 16.7 | 22.6 ± 15.6 | 0.035 |
| HR-QOL measures at baseline | |||
| SF-36 PCS | 36.7 ± 12.5 | 37.5 ± 9.8 | 0.81 |
| NDI | 30.7 ± 20.4 | 37.4 ± 24.8 | 0.31 |
| mJOA | 13.1 ± 2.2 | 13.2 ± 2.5 | 0.81 |
| EQ-5D | 0.66 ± 0.21 | 0.61 ± 0.21 | 0.60 |
Negative value is lordosis
On average, patients experienced improvement in all HR-QOL measures regardless of the surgical approach. Clinically significant improvements in SF-36 PCS, NDI, and mJOA scores were observed in 62.2%, 58.7%, and 53.3% of the cohort, respectively. Outcomes measured at one-year follow up are summarized in Table 2. Patients treated with ventral surgery generally had better outcomes than patients treated with dorsal surgery. Patients treated with ventral surgery had significantly greater mean changes in NDI and EQ-5D scores over the one-year period than patients treated with dorsal surgery (p=0.02 and p=0.02) and also showed a trend for greater mean changes in SF-36 PCS scores (p=0.06).
Table 2.
Postoperative characteristics and outcomes.
| Dorsal | Ventral | p-value | |
|---|---|---|---|
| Postoperative Cobb angle(°) | -3.4* ± 16.3 | -3.1 ± 18.7 | 0.96 |
| Change from preoperative | 4.2 ± 10.8 | -1.7 ± 5.1 | 0.47 |
| Postoperative sagittal balance (mm) | 36.5 ± 16.1 | 28.0 ± 14.4 | 0.06 |
| Change from preoperative (mm) | 3.7 ± 7.3 | 5.4 ± 6.9 | 0.17 |
| Complications | 8/28 (28.6%) | 7/21 (33%) | 0.76 |
| HR-QOL measures: | |||
| SF-36 PCS | |||
| Mean value at 1 year | 42.2 ± 13.0 | 48.8 ± 9.7 | 0.11 |
| Mean change from baseline | 5.1 ± 10.8 | 10.8 ± 9.3 | 0.06 |
| % > MCID | 13/25 (52%) | 15/20 (75%) | 0.14 |
| NDI | |||
| Mean value at 1 year | 19.7 ± 17.6 | 13.5 ± 15.8 | 0.16 |
| Mean change from baseline | -9.4 ± 18.7 | -22.2 ± 16.6 | 0.02 |
| % > MCID | 13/26 (50%) | 14/20 (70%) | 0.23 |
| mJOA | |||
| Mean value at 1 year | 14.8 ± 2.1 | 15.5 ± 2.6 | 0.06 |
| Mean change from baseline | 1.6 ± 2.1 | 2 ± 2.0 | 0.48 |
| % > MCID | 12/25 (48%) | 12/20 (60%) | 0.55 |
| EQ-5D | |||
| Mean value at 1 year | 0.80 ± 0.13 | 0.87 ± 0.16 | 0.06 |
| Mean change from baseline | 0.11 ± 0.18 | 0.23 ± 0.14 | 0.016 |
Negative value is lordosis
The relationship between C2-C7 SVA measurements and absolute HR-QOL measures
Statistically significant correlations were observed between postoperative C2-C7 SVA measurements and SF-36 PCS and mJOA scores at one year (Table 3). Postoperative C2-C7 SVA measurements were observed to be negatively correlated with SF-36 PCS scores (ρ=-0.39, p=0.008) and with mJOA scores (ρ=-0.45, p=0.002) at one-year follow up. A significant correlation was not noted between postoperative C2-C7 SVA measurements and NDI scores (ρ=0.23, p=0.13) or with EQ-5D scores (ρ=-0.19, p=0.20) at one year.
Table 3.
Spearman correlations between C2-C7 sagittal balance radiographic measurement and HR-QOL scores (non-normally distributed variables).
| Timing of C2-C7 SVA measurement | HR-QOL score | Sample size | Correlation (Spearman rho) | p-value |
|---|---|---|---|---|
| Preoperative | EQ-5D (preoperative) | 49 | -0.164 | 0.26 |
| Preoperative | SF-36 PCS (preoperative) | 49 | -0.259 | 0.07 |
| Preoperative | mJOA (preoperative) | 48 | -0.274 | 0.06 |
| Preoperative | NDI (preoperative) | 49 | 0.069 | 0.63 |
| Postoperative | EQ-5D (1 year) | 46 | -0.193 | 0.20 |
| Postoperative | SF-36 PCS (1 year) | 46 | -0.388 | 0.008 |
| Postoperative | mJOA (1 year) | 46 | -0.448 | 0.002 |
| Postoperative | NDI (1 year) | 46 | 0.227 | 0.13 |
| Preoperative | Change in EQ-5D | 46 | -0.219 | 0.14 |
| Preoperative | Change in SF-36 PCS | 46 | -0.236 | 0.12 |
| Preoperative | Change in mJOA | 45 | -0.079 | 0.61 |
| Preoperative | Change in NDI | 46 | 0.266 | 0.07 |
| Postoperative | Change in EQ-5D | 46 | -0.158 | 0.30 |
| Postoperative | Change in SF-36 PCS | 46 | -0.327 | 0.026 |
| Postoperative | Change in mJOA | 45 | -0.080 | 0.60 |
| Postoperative | Change in NDI | 46 | 0.301 | 0.042 |
Statistically significant correlations were not observed between preoperative C2-C7 SVA measurements and preoperative HR-QOL measures, although there was a trend towards statistical significance between preoperative C2-C7 SVA measurements and preoperative SF-36 PCS scores (ρ=-0.26, p=0.07) and with preoperative mJOA scores (ρ=-0.27, p=0.06). A significant correlation was not noted between preoperative C2-C7 SVA measurements and preoperative NDI scores (ρ=0.069, p=0.63) or with preoperative EQ-5D scores (ρ=-0.16, p=0.26).
The effect of sagittal imbalance on functional status after surgery
Postoperative C2-C7 SVA measurements were significantly correlated with changes in SF-36 PCS and NDI scores from preoperative to one year follow up surveys (ρ=-0.33, p=0.03, and ρ=0.30, p=0.04, respectively) (Figure 2, Table 3). A similar correlation was not noted when comparing preoperative C2-C7 SVA measurements and any of the four HR-QOL measures.
Figure 2.
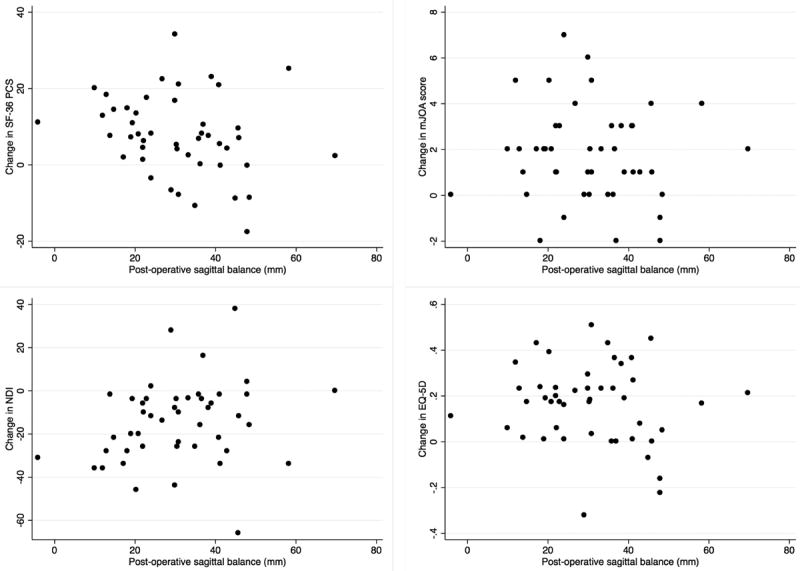
Scatter plots of postoperative C2-C7 SVA measurements and improvements in HR-QOL measures at one year.
The relationship between postoperative C2-C7 SVA measurements and change in SF-36 PCS, NDI, mJOA, and EQ-5D scores is depicted in Figure 2. Postoperative C2-C7 SVA was found to be an independent negative predictor of clinically significant improvement in SF-36 PCS (p=0.02, OR=0.49 for every 10mm increase in sagittal balance), but did not predict clinically significant improvements in NDI or mJOA scores (p=0.10 and p=0.78). Based on this simple logistic regression model, the probability of a clinically significant improvement at one year was predicted to range from 90% at a C2-C7 SVA measurement of zero to less than 50% at a sagittal balance measurement of positive 40mm (Figure 3a). Preoperative C2-C7 SVA measurements were also an independent negative predictor of clinically significant improvement in SF-36 PCS scores in the overall cohort (p=0.0315, OR=0.58 for every 10mm increase in sagittal balance), but similarly, did not predict clinically significant improvements in NDI or mJOA scores (p=0.29 and p=0.56).
Figure 3.
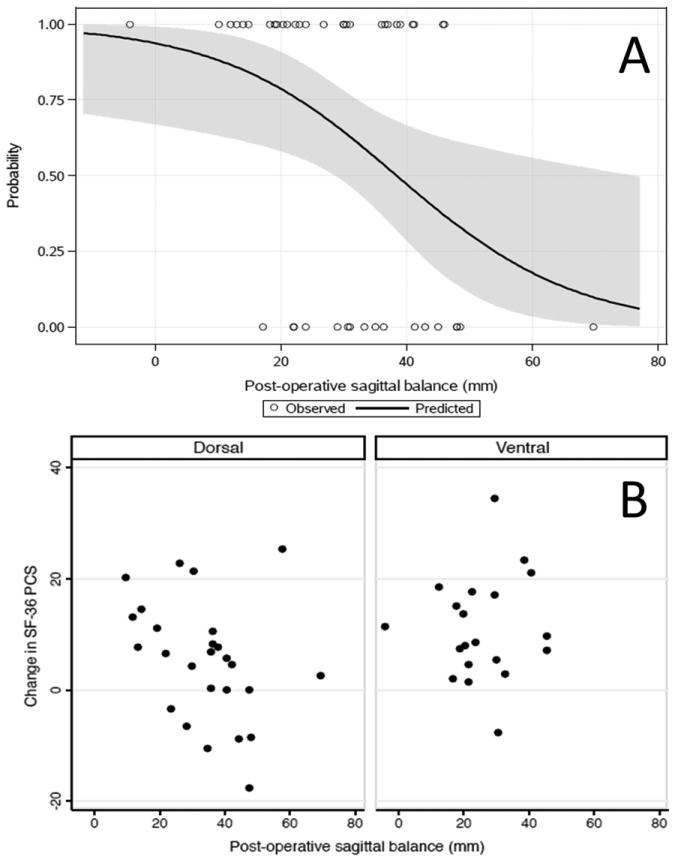
(A) Predicted probability of clinically significant improvement in SF-36 PCS scores by postoperative C2-C7 SVA measurements. Fewer than 50% of patients with postoperative sagittal balance of greater than 40mm are predicted to experience clinically significant improvement after surgery for CSM. (B) Two-way scatter plots of change in SF-36 PCS scores from baseline to one year postoperatively stratified by dorsal and ventral approach demonstrating that patients who were treated with dorsal approaches and who had positive sagittal imbalance tended to have less improvement in SF-36 PCS score.
The role of sagittal imbalance in dorsal and ventral surgery groups
The effect of sagittal imbalance was concentrated in the group of patients undergoing dorsal surgery. In a stratified logistic regression model, postoperative C2-C7 SVA measurements were an independent negative predictor of improvement in SF-36 PCS scores in the dorsal surgery group only, but did not predict improvement in the ventral group (p=0.04 vs. p=0.79) (figure 3b). The Spearman correlation coefficients of postoperative C2-C7 SVA measurements and SF-36 PCS scores differed in dorsal and ventral groups (ρ=-0.42, p=0.03, and ρ=0.02, p=0.93, respectively).
Of note, postoperative C2-C7 SVA measurements in the dorsal surgery group trended higher than in the ventral surgery group (36.5mm vs. 28mm, p=0.06); however, preoperative measurements were also significantly greater in the dorsal group (32.8mm vs. 22.6 mm, p=0.03). Given these differences, we were interested in determining whether either surgical approach resulted in greater postoperative sagittal imbalance. Surgical approach did not independently predict worse postoperative C2-C7 SVA scores in an ANCOVA model that was adjusted for preoperative measurements (p=0.92). As expected, preoperative sagittal balance measurements strongly predicted postoperative measurements (p<0.01) (Figure 4).
Figure 4.
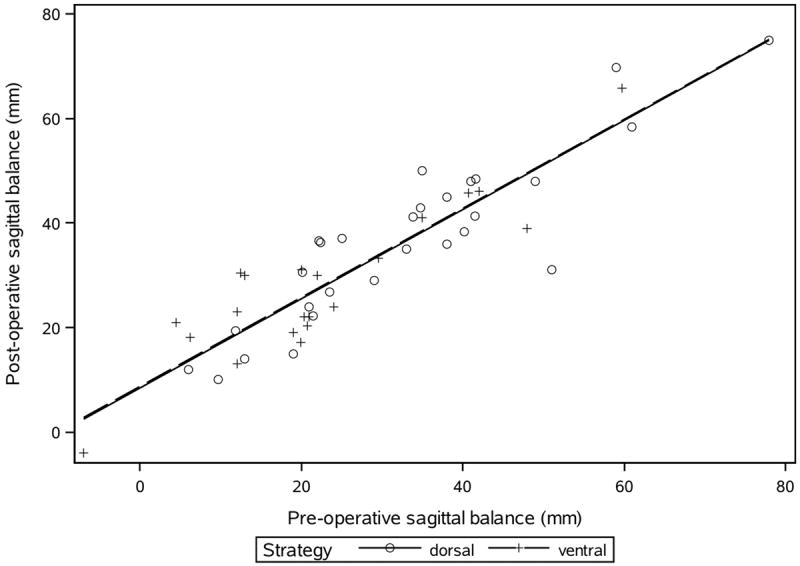
ANCOVA model of postoperative sagittal balance with preoperative sagittal balance and surgical approach.
DISCUSSION
Ghogawala et al have previously shown that both ventral and dorsal surgery are associated with improvements in myelopathy following surgery for CSM, but that ventral surgery might be associated with greater improvement in HR-QOL at 1 year following surgery.4 In this current study, we found that patients with a postoperative C2-C7 SVA measurement greater than 40 mm were unlikely to benefit from surgery from an overall HR-QOL perspective. We demonstrated that C2-C7 SVA measurement is an independent risk factor for poorer HR-QOL outcomes following dorsal surgery for CSM. To our knowledge, this is the first study to report a statistically significant correlation between postoperative C2-C7 measurements and changes in SF-36 PCS and NDI scores and to identify preoperative and postoperative sagittal balance measurements as independent predictors of clinically significant improvements of SF-36 PCS. This study underscores the importance of considering C2-C7 SVA measurements when performing surgery for CSM.
The effect of cervical spine alignment on the severity of myelopathy and functional impairment is gathering more attention. Several authors have correlated global positive sagittal imbalance, defined as a C7 plumb line greater than 50mm anterior to the posterior superior sacral margin, with worse functional outcomes in thoracolumbar disorders.13-16 In general, cervical sagittal alignment is comprised of two separate parameters: lordosis and sagittal plane translation. Lordosis is generally measured using Cobb angles, the Harrison posterior tangent method, and Jackson physiologic stress lines.17 Sagittal plane translation is assessed via the sagittal vertical axis and represents a distinct biomechanical entity which is different than cervical lordosis. The assessment of cervical sagittal balance has been accomplished by measuring the distance between a plumb line dropped from the base of C2 and the posterior superior aspect of C7.18 In addition, sagittal balance can also be measured from the center of gravity of the head, which is approximately the distance between the plumb line dropped from the external auditory meatus to C7.18-21 It can also be estimated via other measurements, such as the chin-brow vertical angle, thoracic inlet angle, and T1 endplate slope.22 However, despite the plethora of available measurement techniques, the C2 plumb line method used in this study is of significant value because it has been previously correlated with NDI and SF-36 PCS.6
Many of the previously published series investigating the role of sagittal alignment and functional outcomes focus on the role of cervical kyphosis rather than C2-C7 sagittal imbalance. Uchida et al reported better postoperative JOA scores in patients treated with ventral surgery than in patients treated with laminoplasty; they also noted that patients treated with an anterior approach had a lower mean postoperative kyphotic angle than patients treated with laminoplasty and suggested that the kyphosis may be related to myelopathy severity.23 Naderi et al observed that an abnormal cervical curvature was associated with a lower probability of improvement in mJOA score after cervical laminectomy,24 and similar findings relating sagittal balance to HR-QOL measures have also been reported by other investigators.25,26 Not all published studies have reported correlations between cervical lordotic angle and functional outcomes, but rather, some found correlations between sagittal alignment and functional outcomes.27,28
Tang et al reported a statistically significant association between postoperative C2-C7 SVA and postoperative NDI and SF-36 PCS scores in a retrospective cohort study of 108 patients undergoing posterior cervical fusion.6 We similarly report a correlation between postoperative C2-C7 SVA and postoperative SF-36 PCS scores, and the magnitude of correlation closely matches that reported by Tang et al. We also report the additional correlation of postoperative C2-C7 SVA and postoperative mJOA scores (p=0.0018). Although the correlation of postoperative C2-C7 SVA and NDI in the current study did not reach statistical significance (p=0.13), the magnitude of correlation approximates that found by Tang at al. Thus, our study builds on the foundation laid by Tang et al and provides additional insights into the relationship of postoperative cervical sagittal balance and HR-QOL.
In a post-hoc analysis of the prospective, multicenter AOSpine North America CSM study, Smith et al reported a correlation of preoperative severity of myelopathy, as measured by mJOA scores, with C2-C7 SVA.29 We also report statistically significant correlations between preoperative C2-C7 SVA measurements and HR-QOL scores. The observed magnitude of correlation between preoperative C2-C7 SVA measurements and mJOA scores is similar to the correlation of -0.282 reported by Smith et al (p=0.06).
Cervical sagittal alignment may be linked to HR-QOL and disease-specific functional measures through various mechanisms. First, kyphotic deformity may induce anterior spinal cord pathology through direct compression against the posterior vertebral body and may increase longitudinal spinal cord tension due to tethering by the dentate ligaments and cervical nerve roots.18,30,31 Sagittal imbalance may itself result in neck pain, muscle fatigue, dysphagia, and alterations in visual horizon.5,23 Compensation for global or regional sagittal imbalance places stress on the surrounding ligaments, muscles, and soft tissues and may result in increased pain and fatigue.
Although this study offers several novel findings, it does have some limitations. First, although study information was gathered prospectively, the patient groups were not randomized, and, thus, our effect estimates are prone to bias from confounding and selection bias. In addition, it is probable that the current study is underpowered to detect a clinically significant change in NDI scores. Our study evaluated C2-C7 SVA only. It is likely that global sagittal balance is also relevant and further studies should include complete sagittal alignment assessments when examining outcomes from surgery for CSM.
Despite these limitations, our conclusions are consistent with other reports in the literature and provide useful new insights into the role of sagittal balance and improvements in HR-QOL scores after surgery. Surgeons might consider sagittal balance correction in selected CSM cases depending upon the degree of cervical sagittal imbalance (e.g. C2-C7 CVA >40 mm) present pre-operatively. A prospective randomized Patient-Centered Outcome Research Institute (PCORI) sponsored trial (PCORI identifier: CE-1304-6173; www.ClinicalTrials.gov identifier: NCT02076113) is currently underway to evaluate cervical and global sagittal imbalance as a predictor of outcome following surgery for CSM.32
CONCLUSIONS
Preoperative and postoperative sagittal balance measurements independently predict clinically significant improvements in CSM patients undergoing decompressive surgery. Postoperative C2-C7 SVA measurements were inversely related to clinical improvement in SF-36 PCS scores in patients treated with dorsal surgery. Surgeons must carefully consider cervical sagittal imbalance during the surgical decision making process.
Acknowledgments
Funding: Jean and David Wallace Foundation (GH382)
Dr. Ghogawala reports receiving private research funding from the Wallace Foundation (GH-382) and received federal grants from PCORI (CE-1304-6173) and NIH (1R13AR065834-01) that are related to the material presented in this manuscript. Dr. Benzel reports receiving royalties from DePuy and being inventor and developer of an arthroplasty device for AxioMed. He is a board member for OrthoMEMS, has an ongoing grant with Stryker, and owns stock options in OrthoMEMS and AxioMed. Dr. Bisson reports consultancy with nView Medical Company and an ongoing grant with PCORI. Dr. Butler reports a grant, travel support, consultancy, employment, and patent from Life Force Informatics. Dr. Heary reports an ongoing grant with PCORI and royalties with Zimmer Spine, DePuy Spine, and Thieme Medical Publishers. Dr. Steinmetz reports consultancy with Biomet Spine, Stryker Spine, and Depuy Synthes.
Footnotes
Benzel: Board, consultancy, grants pending, patents, royalties, stock
Bisson: Grant, consultancy, expert testimony
Ghogawala: Grant, grants pending
Heary: Grant, board, consultancy
Krishnany: None
Curran: Grant
Butler: Patents, consultancy, employment
Steinmetz: Consultancy
Roguski: Grant
Magge: Expert testimony, employment
Potential Conflicts of Interest: For the remaining authors, none were declared.
Level of Evidence: 2
References
- 1.Kalsi-Ryan S, Karadimas SK, Fehlings MG. Cervical spondylotic myelopathy: the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. The Neuroscientist : a review journal bringing neurobiology, neurology and psychiatry. 2013 Aug;19(4):409–421. doi: 10.1177/1073858412467377. [DOI] [PubMed] [Google Scholar]
- 2.Tracy JA, Bartleson JD. Cervical spondylotic myelopathy. The neurologist. 2010 May;16(3):176–187. doi: 10.1097/NRL.0b013e3181da3a29. [DOI] [PubMed] [Google Scholar]
- 3.Young WF. Cervical spondylotic myelopathy: a common cause of spinal cord dysfunction in older persons. American family physician. 2000 Sep 1;62(5):1064–1070. 1073. [PubMed] [Google Scholar]
- 4.Ghogawala Z, Martin B, Benzel EC, et al. Comparative effectiveness of ventral vs dorsal surgery for cervical spondylotic myelopathy. Neurosurgery. 2011 Mar;68(3):622–630. doi: 10.1227/NEU.0b013e31820777cf. discussion 630-621. [DOI] [PubMed] [Google Scholar]
- 5.Fehlings MG, Gray R. Importance of sagittal balance in determining the outcome of anterior versus posterior surgery for cervical spondylotic myelopathy. Journal of neurosurgery Spine. 2009 Nov;11(5):518–519. doi: 10.3171/2009.5.SPINE09182. discussion 519-520. [DOI] [PubMed] [Google Scholar]
- 6.Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2012 Sep;71(3):662–669. doi: 10.1227/NEU.0b013e31826100c9. discussion 669. [DOI] [PubMed] [Google Scholar]
- 7.Ghogawala Z, Coumans JV, Benzel EC, Stabile LM, Barker FG., 2nd Ventral versus dorsal decompression for cervical spondylotic myelopathy: surgeons’ assessment of eligibility for randomization in a proposed randomized controlled trial: results of a survey of the Cervical Spine Research Society. Spine. 2007 Feb 15;32(4):429–436. doi: 10.1097/01.brs.0000255068.94058.8a. [DOI] [PubMed] [Google Scholar]
- 8.Chiles BW, 3rd, Leonard MA, Choudhri HF, Cooper PR. Cervical spondylotic myelopathy: patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery. 1999 Apr;44(4):762–769. doi: 10.1097/00006123-199904000-00041. discussion 769-770. [DOI] [PubMed] [Google Scholar]
- 9.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. Journal of manipulative and physiological therapeutics. 1991 Sep;14(7):409–415. [PubMed] [Google Scholar]
- 10.Vernon H. The Neck Disability Index: state-of-the-art, 1991-2008. Journal of manipulative and physiological therapeutics. 2008 Sep;31(7):491–502. doi: 10.1016/j.jmpt.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. The spine journal : official journal of the North American Spine Society. 2010 Jun;10(6):469–474. doi: 10.1016/j.spinee.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Auffinger B, Lam S, Shen J, Thaci B, Roitberg BZ. Usefulness of minimum clinically important difference for assessing patients with subaxial degenerative cervical spine disease: statistical versus substantial clinical benefit. Acta neurochirurgica. 2013 Dec;155(12):2345–2354. doi: 10.1007/s00701-013-1909-4. discussion 2355. [DOI] [PubMed] [Google Scholar]
- 13.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005 Mar 15;30(6):682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 14.Mac-Thiong JM, Transfeldt EE, Mehbod AA, et al. Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine. 2009 Jul 1;34(15):E519–527. doi: 10.1097/BRS.0b013e3181a9c7ad. [DOI] [PubMed] [Google Scholar]
- 15.Videbaek TS, Bunger CE, Henriksen M, Neils E, Christensen FB. Sagittal spinal balance after lumbar spinal fusion: the impact of anterior column support results from a randomized clinical trial with an eight- to thirteen-year radiographic follow-up. Spine. 2011 Feb 1;36(3):183–191. doi: 10.1097/BRS.0b013e3181cc8fce. [DOI] [PubMed] [Google Scholar]
- 16.Lamartina C, Berjano P, Petruzzi M, et al. Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012 May;21(Suppl 1):S27–31. doi: 10.1007/s00586-012-2236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine. 2000 Aug 15;25(16):2072–2078. doi: 10.1097/00007632-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 18.Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine. 2013 Oct 15;38(22 Suppl 1):S149–160. doi: 10.1097/BRS.0b013e3182a7f449. [DOI] [PubMed] [Google Scholar]
- 19.Gangnet N, Pomero V, Dumas R, Skalli W, Vital JM. Variability of the spine and pelvis location with respect to the gravity line: a three-dimensional stereoradiographic study using a force platform. Surgical and radiologic anatomy : SRA. 2003 Nov-Dec;25(5-6):424–433. doi: 10.1007/s00276-003-0154-6. [DOI] [PubMed] [Google Scholar]
- 20.Lafon M, Megret F, Meuth SG, et al. Detrimental contribution of the immuno-inhibitor B7-H1 to rabies virus encephalitis. Journal of immunology. 2008 Jun 1;180(11):7506–7515. doi: 10.4049/jimmunol.180.11.7506. [DOI] [PubMed] [Google Scholar]
- 21.Lafage V, Schwab F, Skalli W, et al. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine. 2008 Jun 15;33(14):1572–1578. doi: 10.1097/BRS.0b013e31817886a2. [DOI] [PubMed] [Google Scholar]
- 22.Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. Journal of spinal disorders & techniques. 2012 Apr;25(2):E41–47. doi: 10.1097/BSD.0b013e3182396301. [DOI] [PubMed] [Google Scholar]
- 23.Uchida K, Nakajima H, Sato R, et al. Cervical spondylotic myelopathy associated with kyphosis or sagittal sigmoid alignment: outcome after anterior or posterior decompression. Journal of neurosurgery Spine. 2009 Nov;11(5):521–528. doi: 10.3171/2009.2.SPINE08385. [DOI] [PubMed] [Google Scholar]
- 24.Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C. Cervical spondylotic myelopathy: surgical results and factors affecting prognosis. Neurosurgery. 1998 Jul;43(1):43–49. doi: 10.1097/00006123-199807000-00028. discussion 49-50. [DOI] [PubMed] [Google Scholar]
- 25.Cabraja M, Abbushi A, Koeppen D, Kroppenstedt S, Woiciechowsky C. Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: sagittal alignment and clinical outcome. Neurosurgical focus. 2010 Mar;28(3):E15. doi: 10.3171/2010.1.FOCUS09253. [DOI] [PubMed] [Google Scholar]
- 26.Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ. Anterior correction of cervical kyphotic deformity: effects on myelopathy, neck pain, and sagittal alignment. Journal of neurosurgery. 2004 Jan;100(1 Suppl Spine):13–19. doi: 10.3171/spi.2004.100.1.0013. [DOI] [PubMed] [Google Scholar]
- 27.Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery. 2011 May;68(5):1309–1316. doi: 10.1227/NEU.0b013e31820b51f3. discussion 1316. [DOI] [PubMed] [Google Scholar]
- 28.Guerin P, Obeid I, Gille O, et al. Sagittal alignment after single cervical disc arthroplasty. Journal of spinal disorders & techniques. 2012 Feb;25(1):10–16. doi: 10.1097/BSD.0b013e31820f916c. [DOI] [PubMed] [Google Scholar]
- 29.Smith JS, Lafage V, Ryan DJ, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine. 2013 Oct 15;38(22 Suppl 1):S161–170. doi: 10.1097/BRS.0b013e3182a7eb9e. [DOI] [PubMed] [Google Scholar]
- 30.Albert TJ, Vacarro A. Postlaminectomy kyphosis. Spine. 1998 Dec 15;23(24):2738–2745. doi: 10.1097/00007632-199812150-00014. [DOI] [PubMed] [Google Scholar]
- 31.Farley CW, Curt BA, Pettigrew DB, Holtz JR, Dollin N, Kuntz Ct. Spinal cord intramedullary pressure in thoracic kyphotic deformity: a cadaveric study. Spine. 2012 Feb 15;37(4):E224–230. doi: 10.1097/BRS.0b013e31822dd69b. [DOI] [PubMed] [Google Scholar]
- 32.Cervical Spondylotic Myelopathy Surgical (CSM-S) Trial: Randomized Controlled Trial Design and Rationale. Neurosurgery. doi: 10.1227/NEU.0000000000000479. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]


